Urgent Appendectomy Performed Along with Hematopoietic Cell Transplantation (HCT) for a Patient with Severe Aplastic Anaemia – A Case Report
Article Information
Sondus Alsharidah1*, Samar Ousia2, Elshazly Abdelhafez1, Brigitta Antoun1, Dalal Alshemmeri1, Hassan Khalil3, Medhat Askar4, 5, 6
1Paediatric Stem Cell Transplant Unit, Department of Paediatric Haematology oncology, NBK children’s specialized hospital, Kuwait
2Stem Cell Transplant Unit, Department of hematology and bone marrow transplant, Kuwait Cancer Centre, Kuwait
3Surgical department, Sabah Hospital, Kuwait
4Department of pathology and laboratory medicine, Texas health science Center, college of medicine, Texas, USA
5Cell processing laboratory, Baylor University Medical Center, Texas, USA
6Director of Clinical Services, The National Marrow Donor Program (NMDP)/BeTheMatch, MN, USA
*Corresponding Author: Sondus Alsharidah, Paediatric Stem Cell Transplant Unit, Paediatric Haematology oncology department, NBK children’s specialized hospital, Kuwait
Received: 01 April 2022; Accepted: 23 April 2022; Published: 29 April 2022
Citation: Sondus Alsharidah, Samar Ousia, Elshazly Abdelhafez, Brigitta Antoun, Dalal Alshemmeri, Hassan Khalil, Medhat Askar. Urgent Appendectomy Performed Along with Hematopoietic Cell Transplantation (HCT) for a Patient with Severe Aplastic Anaemia – A Case Report. Archives of Clinical and Medical Case Reports 6 (2022): 324-330.
View / Download Pdf Share at FacebookAbstract
A 14-year-old male was waiting for hematopoietic cell transplantation for severe aplastic anaemia. The night prior to the transplant he unexpectedly developed acute appendicitis. A couple of hours earlier to the emergency laparoscopic appendectomy, he had peripheral blood stem cell (PBSC) transplant with no complications.
Keywords
Acute Appendicitis; HCT; Aplastic Anaemia; Pancytopenia; Appendectomy; Case Report
Acute Appendicitis articles; HCT articles; Aplastic Anaemia articles; Pancytopenia articles; Appendectomy articles; Case Report articles
Acute Appendicitis articles Acute Appendicitis Research articles Acute Appendicitis review articles Acute Appendicitis PubMed articles Acute Appendicitis PubMed Central articles Acute Appendicitis 2023 articles Acute Appendicitis 2024 articles Acute Appendicitis Scopus articles Acute Appendicitis impact factor journals Acute Appendicitis Scopus journals Acute Appendicitis PubMed journals Acute Appendicitis medical journals Acute Appendicitis free journals Acute Appendicitis best journals Acute Appendicitis top journals Acute Appendicitis free medical journals Acute Appendicitis famous journals Acute Appendicitis Google Scholar indexed journals COVID-19 articles COVID-19 Research articles COVID-19 review articles COVID-19 PubMed articles COVID-19 PubMed Central articles COVID-19 2023 articles COVID-19 2024 articles COVID-19 Scopus articles COVID-19 impact factor journals COVID-19 Scopus journals COVID-19 PubMed journals COVID-19 medical journals COVID-19 free journals COVID-19 best journals COVID-19 top journals COVID-19 free medical journals COVID-19 famous journals COVID-19 Google Scholar indexed journals HCT articles HCT Research articles HCT review articles HCT PubMed articles HCT PubMed Central articles HCT 2023 articles HCT 2024 articles HCT Scopus articles HCT impact factor journals HCT Scopus journals HCT PubMed journals HCT medical journals HCT free journals HCT best journals HCT top journals HCT free medical journals HCT famous journals HCT Google Scholar indexed journals Aplastic Anaemia articles Aplastic Anaemia Research articles Aplastic Anaemia review articles Aplastic Anaemia PubMed articles Aplastic Anaemia PubMed Central articles Aplastic Anaemia 2023 articles Aplastic Anaemia 2024 articles Aplastic Anaemia Scopus articles Aplastic Anaemia impact factor journals Aplastic Anaemia Scopus journals Aplastic Anaemia PubMed journals Aplastic Anaemia medical journals Aplastic Anaemia free journals Aplastic Anaemia best journals Aplastic Anaemia top journals Aplastic Anaemia free medical journals Aplastic Anaemia famous journals Aplastic Anaemia Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Radiology articles Radiology Research articles Radiology review articles Radiology PubMed articles Radiology PubMed Central articles Radiology 2023 articles Radiology 2024 articles Radiology Scopus articles Radiology impact factor journals Radiology Scopus journals Radiology PubMed journals Radiology medical journals Radiology free journals Radiology best journals Radiology top journals Radiology free medical journals Radiology famous journals Radiology Google Scholar indexed journals Pancytopenia articles Pancytopenia Research articles Pancytopenia review articles Pancytopenia PubMed articles Pancytopenia PubMed Central articles Pancytopenia 2023 articles Pancytopenia 2024 articles Pancytopenia Scopus articles Pancytopenia impact factor journals Pancytopenia Scopus journals Pancytopenia PubMed journals Pancytopenia medical journals Pancytopenia free journals Pancytopenia best journals Pancytopenia top journals Pancytopenia free medical journals Pancytopenia famous journals Pancytopenia Google Scholar indexed journals Appendectomy articles Appendectomy Research articles Appendectomy review articles Appendectomy PubMed articles Appendectomy PubMed Central articles Appendectomy 2023 articles Appendectomy 2024 articles Appendectomy Scopus articles Appendectomy impact factor journals Appendectomy Scopus journals Appendectomy PubMed journals Appendectomy medical journals Appendectomy free journals Appendectomy best journals Appendectomy top journals Appendectomy free medical journals Appendectomy famous journals Appendectomy Google Scholar indexed journals
Article Details
Introduction
Aplastic anaemia is a syndrome of hematopoietic failure resulting from injury leading to diminished or absent hematopoietic precursors or hypocellularity in the bone marrow and associated pancytopenia [1]. It is a rare, life-threatening haematological disorder that occurs across all age groups [2]. The most common complications of aplastic anaemia include bleeding, infections, or transformation to lymphoproliferative disorders [1]. The prognosis for patients with aplastic anaemia has markedly improved recently because of better treatment and supportive measures. For idiopathic severe aplastic anaemia (SAA), a matched sibling donor (MSD) hematopoietic cell transplant (HCT) is the treatment of choice [3].
Pancytopenia and bone marrow suppression, due to aplastic anemia increase the susceptibility to infections, particularly infections of the abdomen [4]. Neutropenic Enterocolitis (NE) and acute appendicitis are life-threatening conditions, that develop in children with severe or prolonged neutropenia and are often hard to diagnose [5]. Hematopoietic cell transplantation (HCT) for patients with active infections generally has poor outcomes, because of high infection- related and transplant-related mortality. Appendicitis is an uncommon complication of SAA; it is an inflammation of the appendix, which leads to an increased diameter of the organ to ≥ 0.6 cm and corresponding clinical signs [6]. Here, we report a case of severe aplastic anaemia complicated by the development of acute appendicitis on the night of stem cell transplantation.
2. Case Presentation
A 14-year-old male presented with ecchymotic skin patches, pallor, lethargy, investigated and diagnosed with severe aplastic anaemia (bone marrow aspiration: cellularity <10% and no blast cells, no evidence of PNH, depressed all precursors) 2 weeks later he had COVID-19 that required hospitalisation for 2 weeks. During all this period he was blood products transfusion dependent everyother day, then started on oral eltrombopag (thrombopoietin receptor agonist) 50 mcg, twice a day on increment doses with poor response over 6 weeks. The patient serum ferritin was 3400 mg/L then started on iron chelation therapy (IV deferoxamine infusion 50 mg/kg) 4 times a week while being inpatient due to the high demand of blood products trans-fusions.
Furthermore, he was prepared for hematopoietic cell transplantation with matched related sibling donor (his brother) and conditioned with Flu, Cy, ATG and GVHD prophylaxis cyclosporin and methotrexate. Although the patient was booked for fresh bone marrow stem cell transplant, we cryopreserved peripheral blood stem cell (PBSC) prior to the chemotherapy conditioning following EBMT recommend-dations for all patients during the COVID-19 pandemic [7].
On day -1 the patient developed severe acute abdominal pain on the right iliac fossa associated with constipation and vomiting, x-ray abdomen and ultrasound abdomen showed no abnormalities ,but abdominal pain persisted, so he was evaluated by the surgeon and wanted to rule out appendicitis by CT abdomen with contrast, that showed later the appendix with retrocaecal position presented as tubular dilated blind end structure measuring about 8 mm in calibre fluid filled showing unilateral mural thickness reaching 3 mm with mucosal hyperenhancement associated with minimal pelvic fluid collection surrounding fat stranding and few mildly enlarged sub mesenteric regional lymph nodes, this is suggestive of acute appendicitis, the ascending colon and ileocecal junction and to a lesser extent the ascending colon showed diffuse mural thickening with fat halo sign likely indicating neutropenic colitis, his complete blood count WBC 0.01X109/L, Haemoglobin (HB) 75 g/L platelets 8X109/L.
After diagnosing the patient clinically and radiologically with acute appendicitis and neutropenic colitis he was kept nil per oral, on IV metronidazole IV 7.5 mg/kg /TDS and Amikacin IV 15 mg/kg/d and piperacillin tazobactam IV 4.5 g/QDS, then he was prepared for the surgical procedure as he was anaemic and thrombocytopenic. Here the decision of stem cell transplant was taken to be done prior to the surgical procedure, so the patient had PBSC transplantation with CD34 cell dose 4.4 × 106 /KG, viability 85%. The SCT started after pre-medications (steroids, paracetamol, antihistamine) given to the patient with the vitals were stable throughout with no immediate complications. The parents were consented with high-risk consent for an urgent laparoscopic appendectomy that was performed 2 hours after the HCT. The patient was continued on antibiotics for 7-10 days post- laparoscopic appendectomy surgery, and pain was controlled with opioids and paracetamol, we noticed hypokalaemia that was corrected with potassium supplements. The histopathology of the appendix resected revealed acute suppurative appendicitis (Figure 1).
The patient was cared for post HCT. and post-surgical procedure, so the oral fluids were resumed within 2-3 days with good tolerance. Regarding the HCT care: he engrafted platelets on day 12 and neutrophils within day 16. We noticed the patient had anxiety attacks and aggressive behaviour that required psychiatric management, he was started temporarily on anxiolytics for 2 weeks. The patient remained in the hospital for management and close monitoring. Then was discharged home on day +26 post SCT, day+26 Post endoscopic appendectomy, follow up is scheduled twice a week. Day + 28 Chimerism: 94.4% donor cells. The patient continued on regular follow up, and occasionally requiring hydration at the day care, the follow up was every 4 weeks in the clinic. with good outcome of his Chimerism day +90 and +360 is 93, 4%, 97.9% respectively.
Immunoreconstitution was within 5 months of transplant CD 4 absolute count 335 cells/ ul. There was iron overload, serum ferritin (1884 ng/ml) venesection was started for him, last serum ferritin 584 ng/ml, last CBC: WBC 7.4 × 109/L neutrophil 3.7 × 109/L, HB 139 g/L platelets 223 × 109/L. Patient is off immunosuppression medication after 1 year of transplant and the chimerism is stable all through.

Figure 1: features the removed appendix from the patient’s abdomen.
|
Complete Blood Count |
WBCs |
0.01 × 109 |
|
Hemoglobin concentration |
75 g/L |
|
|
Platelet count |
8 × 109 |
|
|
Absolute Neutrophil Count |
0 |
|
|
Liver Function Tests |
Bilirubin |
15.4 umol/L |
|
AST |
9.1 U/L |
|
|
ALT |
9 U/L |
|
|
Renal Function Tests |
Sodium (Na) |
139 mmol/L |
|
Potassium (K) |
3.92 mmol/L |
|
|
Urea (U) |
3.4 mmol/L |
|
|
Creatinine (Cr) |
37 umol/L |
|
|
Magnesium (Mg) |
0.77 mmol/L |
|
|
Serum Calcium (Ca) |
2.12 mmol/L |
|
|
Phosphorus (Ph) |
0.74 mmol/L |
|
|
Coagulation Profile |
Prothrombin Time (PT) |
21.6 Secs high |
|
INR |
1.42 |
|
|
Partial thromboplastin time (PTT) |
49.2 Secs high |
|
|
D.Dimer |
414 ng/ml high |
|
|
CRP |
153 mg/L high |
|
Table 1: Shows the blood test results during the diagnosis of appendicitis.
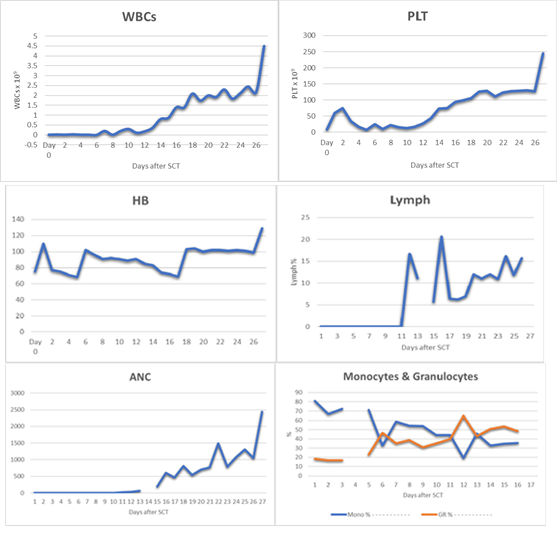
Chart 1: CBC showing engraftment following the SCT up to discharge.
3. Discussion
Appendicitis is a life-threatening, rare complication that is reported during hematopoietic cell transplantation (HCT) with no set standard of care [8, 9]. Severe prolonged neutropenia secondary to aplastic anaemia, chemotherapy and immunosuppressant is probably the culprit as they increase the risk of gastrointestinal infections [5]. Gastrointestinal infections observed in this patient population represent approximately 30% of neutropenic infections [10]. Owing to the rarity of this condition, there is not enough data on the incidence of acute appendicitis in HCT patients, nor there is enough evidence to support optimal management. There is limited literature on acute appendicitis in the setting of hematopoietic cell transplant [10-12]. Most data published in the literature comes from case reports or case series [8].
Even though appendicitis in stem cell transplant HSCT is uncommon, it is a challenging complication, both in diagnosis and management. The Alvarado Scoring System (the MANTRELS acronym stands for ‘Migration, Anorexia-acetone, Nausea-vomiting, Tenderness in the right quadrant, Rebound pain, Elevation of temperature, Leukocytosis, Shift to the left), which is shortened to ASSMANTRELS, has been used to diagnose acute appendicitis [3]. However, acute appendicitis occurred in HSCT patients during the neutropenic phase. The indexes of leukocytosis and shift to the left (LS) of the ASS-MANTRELS did not apply to these patients. A new scoring system named ASS-MANTREU includes symptoms, signs, and the ultrasound examination result [13]. There is still a debate whether surgical intervention or conservative antibiotic therapy is the best approach in such a population.
Several studies and case reports advocate the benefits of conservative treatment with antibiotic therapy. However, other studies have shown that surgical management of acute appendicitis in neutropenic patients can be safely performed and is the most effective therapeutic modality despite having neutropenia [6]. The study of Mortellaro et al. suggested that timely surgical interventions within a day of diagnosis could be done safely in neutropenic patients [14]. Nevertheless; appendectomy in this patient population is not without risks. Wound infection, delayed healing, and hemorrhagic complications are all factors to be considered. Other studies recommend a multidisciplinary team assessment of each case to decide on the best approach to treat appendicitis on a case- by-case basis [8]. Surgical appendectomy remains the treatment of choice for appendicitis and in line with treatment guidelines of the American College of Surgeons and World Society of Emergency Surgery [15, 16]. In our case, the decision was made based on the patient’s clinical status and he was successfully treated for appendicitis using surgical management with no complications.
4. Conclusion
In conclusion, even though acute appendicitis in hematopoietic stem cell transplant patients is a rare occurrence, a critical complication should be addressed and managed in a timely fashion to avoid further complications. The choice to surgically remove the appendix or use conservative antibiotic therapy remains subject to each patient’s clinical scenario.
Declaration of Conflicting Interests
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent
The patient’s mother provided written informed consent for the patient information.
Acknowledgements
Funded by Gilead Sciences without any interpretation of data.
References
- Moore CA, Krishnan K. Aplastic Anemia. In: StatPearls (2022).
- DeZern AE, Guinan EC. Aplastic anaemia in adolescents and young adults. Acta Haematol 132 (2014): 331-339.
- Samarasinghe Sujith, Webb David. (2012). How I manage aplastic anaemia in children. British journal of haematology 157 (2012): 26-40.
- Ali A, Alhindi S, Alalwan A A, et al. Acute Appendicitis in a Child with Acute Leukemia and Chemotherapy-Induced Neutropenia: A Case Report and Literature Review. Cureus 12 (2020): e8858.
- Bulent Alioglu, Zekai Avci, Figen Ozcay, et al. Neutropenic Enterocolitis in Children with Acute Leukemia or Aplastic Anemia. Int J Hematol 86 (2007): 364-368.
- Von Mersi H, Benkö T, Boztug H, et al. Diagnosis and management of acute appendicitis in 21 pediatric hematology and oncology patients at a tertiary care cancer center. Scientific reports 11 (2021): 1-6.
- Coronavirus Disease Covid-19: Ebmt Recommendations Version 14 (2021)
- Wright Z, Essien F, Renshaw J, et al. Appen-diceal disease in hematopoietic cell transpla-ntation. Clin Case Rep 10 (2022): e05047.
- Wright Zachary, Wiggins Michael, Renshaw John, et al. Appendiceal Disease Peri-Transplant. Biology of Blood and Marrow Transplantation 22 (2016): S296-S297.
- Koretz MJ, Neifeld JP. Emergency surgical-ltreatmentfor patients with acute leukemia. Surg Gynecol Obstet 161 (1985): 149-151.
- Forghieri F, Luppi M, Narni F, et al. Acute appendicitis in adult neutropenic patients with hematologic malignancies. Bone Marrow Transplant 42 (2008): 701-703.
- Kontoyiannis DP, Mathur M, ChenY-B, et al. Case records of the Massachusetts General Hospital. Case 13-2014. A 41-year-old man with fever and abdominal pain after stem-cell transplantation. N Engl J Med 370 (2014): 1637-1646.
- Zhang Q, Zhou Y, Majaw J, et al. Acute appendicitis in leukaemia patients undergoing haematopoietic stem cell transplantation during the neutropaenic phase: a case series from a single BMT centre in China. Bone Marrow Transplant 53 (2018): 219-222.
- Mortellaro V, Juang D, Fike FB, et al. Treatment ofappendicitis in neutropenic children. J Surg Res 170 (2011): 14-16.
- Ruffolo C, Fiorot A, Pagura G, et al. Acute appendicitis: what is the gold standard oftreatment?. World J Gastroenterol 19 (2013): 8799- 8807.
- Sartelli M, Viale P, Catena F, et al. 2013 WSES guidelines for management of intra- abdominal infections. World J Emerg Surg 8 (2013): 3.
