Subacute Constrictive Pericarditis after mRNA Covid-19 Vaccination
Article Information
Ilir Hysi1*, Olivier Rebet1, Bruno Vaquette2, Olivier Fabre1
1Departement of Cardiac Surgery of Artois, Centre Hospitalier de Lens et Hôpital privé de Bois Bernard, Ramsay Santé, France
2Departement of Cardiology, Hôpital privé de Bois Bernard, Ramsay Santé, France
*Corresponding Author: Ilir Hysi, Departement of Cardiac Surgery of Artois, Centre Hospitalier de Lens et Hôpital privé de Bois Bernard, Ramsay Santé, France.
Received: 23 February 2022; Accepted: 04 March 2022; Published: 09 March 2022
Citation: Ilir Hysi, Olivier Rebet, Bruno Vaquette, Olivier Fabre. Subacute Constrictive Pericarditis after mRNA Covid-19 Vaccination. Archives of Clinical and Medical Case Reports 6 (2022): 189-192.
View / Download Pdf Share at FacebookAbstract
Relation between mRNA Covid-19 vaccine and acute pericarditis has been advocated. However, we have with no further information about the mid-term evolution of this complication. Here we present the possibility of a rapid evolution towards a constrictive pericarditis. Physicians should know this possibility and closely follow-up these patients.
Keywords
Covid-19; Acute pericarditis; mRNA Covid-19 vaccines; Myocarditis
Covid-19 articles; Acute pericarditis articles; mRNA Covid-19 vaccines articles; Myocarditis articles
Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Acute pericarditis articles Acute pericarditis Research articles Acute pericarditis review articles Acute pericarditis PubMed articles Acute pericarditis PubMed Central articles Acute pericarditis 2023 articles Acute pericarditis 2024 articles Acute pericarditis Scopus articles Acute pericarditis impact factor journals Acute pericarditis Scopus journals Acute pericarditis PubMed journals Acute pericarditis medical journals Acute pericarditis free journals Acute pericarditis best journals Acute pericarditis top journals Acute pericarditis free medical journals Acute pericarditis famous journals Acute pericarditis Google Scholar indexed journals cancer articles cancer Research articles cancer review articles cancer PubMed articles cancer PubMed Central articles cancer 2023 articles cancer 2024 articles cancer Scopus articles cancer impact factor journals cancer Scopus journals cancer PubMed journals cancer medical journals cancer free journals cancer best journals cancer top journals cancer free medical journals cancer famous journals cancer Google Scholar indexed journals mRNA articles mRNA Research articles mRNA review articles mRNA PubMed articles mRNA PubMed Central articles mRNA 2023 articles mRNA 2024 articles mRNA Scopus articles mRNA impact factor journals mRNA Scopus journals mRNA PubMed journals mRNA medical journals mRNA free journals mRNA best journals mRNA top journals mRNA free medical journals mRNA famous journals mRNA Google Scholar indexed journals Ultra Sound articles Ultra Sound Research articles Ultra Sound review articles Ultra Sound PubMed articles Ultra Sound PubMed Central articles Ultra Sound 2023 articles Ultra Sound 2024 articles Ultra Sound Scopus articles Ultra Sound impact factor journals Ultra Sound Scopus journals Ultra Sound PubMed journals Ultra Sound medical journals Ultra Sound free journals Ultra Sound best journals Ultra Sound top journals Ultra Sound free medical journals Ultra Sound famous journals Ultra Sound Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals Radiology articles Radiology Research articles Radiology review articles Radiology PubMed articles Radiology PubMed Central articles Radiology 2023 articles Radiology 2024 articles Radiology Scopus articles Radiology impact factor journals Radiology Scopus journals Radiology PubMed journals Radiology medical journals Radiology free journals Radiology best journals Radiology top journals Radiology free medical journals Radiology famous journals Radiology Google Scholar indexed journals Covid-19 articles Covid-19 Research articles Covid-19 review articles Covid-19 PubMed articles Covid-19 PubMed Central articles Covid-19 2023 articles Covid-19 2024 articles Covid-19 Scopus articles Covid-19 impact factor journals Covid-19 Scopus journals Covid-19 PubMed journals Covid-19 medical journals Covid-19 free journals Covid-19 best journals Covid-19 top journals Covid-19 free medical journals Covid-19 famous journals Covid-19 Google Scholar indexed journals Myocarditis articles Myocarditis Research articles Myocarditis review articles Myocarditis PubMed articles Myocarditis PubMed Central articles Myocarditis 2023 articles Myocarditis 2024 articles Myocarditis Scopus articles Myocarditis impact factor journals Myocarditis Scopus journals Myocarditis PubMed journals Myocarditis medical journals Myocarditis free journals Myocarditis best journals Myocarditis top journals Myocarditis free medical journals Myocarditis famous journals Myocarditis Google Scholar indexed journals
Article Details
1. Background
During the recent Covid-19 pandemic, while vaccination rates are growing worldwide, there has been debate about potential cardiac manifestations of the anti-Covid-19 vaccination and the viral infection itself. Although recent studies have demonstrated the safety of the mRNA Covid-19 vaccines [1], some authors have evoked the possibility of rare acute myocarditis/pericarditis following vaccines [2]. Here we describe for the first time the case of a rapidly evolving constrictive pericarditis after a mRNA Covid-19 Pfizer vaccination.
2. Case Study
The patient was a 63-year-old man with a past medical history of peripheral arterial disease and pulmonary embolism in 2019. He had been receiving rivaroxaban (Xarelto) 20mg daily for two years. He was inoculated the first dose of the BNT162b2 Pfizer BioNTech vaccine on April 21st and three days later he reported to the cardiology department, resenting with shortness of breath. Transthoracic echocardiography showed a moderate pericardial effusion without signs of compression. Troponin assays were within normal range which was taken as evidence against myocarditis. A diagnosis isolated pericarditis was made and the patient was treated by oral nonsteroid anti-inflammatory drugs (Ibuprofen) and colchicine. On the May 25th the patient returned to the hospital with symptoms of tamponade. Echocardiography showed increased pericardial effusion with compression on the right chambers. The patient was transferred to the operating room where a pericardial drainage was performed through a subxiphoid incision (150ml of hemorrhagic liquid). He was discharged home three days later in stable clinical condition. The anti-inflammatory drugs were discontinued after one month of treatment. His second dose of the same vaccine of June 7th were not followed by any clinical problem. The patient presented again at the hospital in August, with a severe shortness of breath and lower limb swelling. A thickened pericardium with signs of constriction of the right side of the heart but no signs of pericardial effusion were on ultrasound. These findings were confirmed by the magnetic resonance imaging (Figure 1).
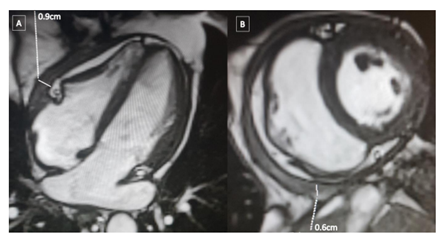
Figure 1: Magnetic resonance imaging of the heart. A) Axial view showing a thickening of the pericardium on the anterior part of the right ventricle. B) Coronal view showing a semicircular thickening of the pericardium constricting the right ventricle.
Left heart catheterization was normal and right heart catheterization did not show a dip plateau sign. The patient was referred for surgical constrictive pericarditis in order to relieve constriction on September 21st of the same year. During the procedure, the pericardium was hardened and showing obvious signs of inflammation. The surgery liberated the heart after an extended pericardiectomy, without the need for cardiopulmonary bypass. The patient’s clinical condition improved immediately after the surgery and the postoperative period was uneventful. Cytologic examination of the pericardium showed nonspecific inflammatory infiltration. Currently the patient reports being in good health and absence of any symptoms.
3. Discussion
Constrictive pericarditis is a rare but well-known heart disease that often requires cardiac surgery. It ensues any inflammatory process involving the pericardium. In industrialized countries the most common causes are idiopathic or viral, or following surgical, radiation, and inflammatory or infectious disease, while tuberculosis remain a major cause in developing countries [3]. To our knowledge, there have been only three published cases of related constrictive pericarditis in the presence of exposure to Covid-19 [3-5]. In two of these cases the patients died due to the catastrophic evolution of their pulmonary Covid-19 lesions and the third patient survived on a treatment consisting of pericardiocentesis combined with oral anti-inflammatory therapy. On the other hand, there has been concerns about the safety of Covid-19 mRNA vaccines. The European Medicines Agency reports a combined incidence rate of myocarditis and pericarditis in the order of 1.6 per million among the recipients of the 160 million doses administered [2]. Importantly myocarditis outnumbers pericarditis by 3:2. To our knowledge, there has been no description in the literature of cases of constrictive pericarditis following inoculation mRNA vaccination. Our patient experienced an initial pericardial effusion a few days after the first dose of the vaccine. Although causality cannot be established with absolute certainty, an adverse effect of the vaccine may reasonably be among the possible causes. Although anti-inflammatory oral treatment and pericardiocentesis were promptly administered, the condition rapidly deteriorated towards rapid pericarditis with three months of the onset of symptoms. There may be open questions on whether a prolonged course of initial anti-inflammatory treatment, in the space of three to six months could have avoid the secondary inflammatory infiltration and thickening of the pericardium. This case illustrates the extremely rare, but real possibility of constrictive pericarditis after mRNA anti Covid-19 vaccination. Intense follow-up of similar patients may be of particular importance, especially given that the use of these vaccines is likely to increase across the world in response to a developing pandemic.
Conflict of Interest
None to declare
Funding Statement
No funding received for this work.
References
- Barda N, Dagan N, Ben-Shlomo Y, et al. Safety of the BNT162b2 mRNA Covid-19 Vaccine in a Nationwide Setting. N Engl J Med 385 (2021): 1078-1090.
- Pepe S, Gregory AT, Denniss AR. Myocarditis, Pericarditis and Cardiomyopathy After COVID-19 Vaccination. Heart Lung Circ 30 (2021):1425-1429.
- Beckerman JK, Alarfaj M, Tracy CM, et al. Coronavirus disease 2019 (COVID-19)-associated constrictive pericarditis. BMJ Case Rep 14 (2021): 242018.
- Diaconu R, Popescu L, Voicu A, et al. Subacute effusive-constrictive pericarditis in a patient with COVID-19. BMJ Case Rep 14 (2021): 242443.
- SeyedAlinaghi S, Ghadimi M, Gharabaghi MA, et al. Constrictive Pericarditis Associated with Coronavirus Disease 2019 (COVID-19): A Case Report. Infect Disord Drug Targets 21 (2021): 160921188928.
