Non-traumatic Low Back Pain: Five Case Reports and Al Wakra Recommendations
Article Information
Islam Hussam Elrobaa*, Hani Hamad Aldulimi, Muayad Kasim Khalid, Elfadel Hamad Dafalla, Abdulhadi Haider Khan, Bassam Adel Fathi, Mohamed Abu Elgasem Mgaram, Helmy Gouda Elhag, Nashat Nabil Ali, Hisham Mohammed Khader, Maria Jennifer Del Castillo
Department of Adult Emergency, Al Wakra Hospital, Hamad Medical Corporation, Al Wakrah, Qatar
*Corresponding Author: Dr. Islam Hussam Elrobaa, Emergency Medicine Specialist, Department of Al Wakra Emergency, Al Wakra Hospital, Hamad Medical Corporation, Doha, Qatar
Received: 28 September 2020; Accepted: 19 October 2020; Published: 20 November 2020
Citation: Islam Hussam Elrobaa, Hani Hamad Aldulimi, Muayad Kasim Khalid, Elfadel Hamad Dafalla, Abdulhadi Haider Khan, Bassam Adel Fathi, Mohamed Abu Elgasem Mgaram, Helmy Gouda Elhag, Nashat Nabil Ali, Hisham Mohammed Khader, Maria Jennifer Del Castillo. Non-traumatic Low Back Pain: Five Case Reports and Al Wakra Recommendations. Archives of Clinical and Medical Case Reports 4 (2020): 1084-1095.
View / Download Pdf Share at FacebookAbstract
Low back pain (LBP) is the fifth most common reason for visiting a physician [1, 2]. Although non-traumatic LBP is benign, and self-limited in most cases, it occasionally indicates a serious disease. Emergency physician must able to distinguish between patients with benign non-traumatic LBP requiring merely history taking and physical examination and identify those with LBP indicative of a serious illness. In this article, we have discussed five such cases and have proposed some clinical recommendations to manage nontraumatic LBP to avoid missing the loss of diagnosis of a serious disease.
Keywords
Non traumatic low back pain; Serious disease; Emergency medicine
Non traumatic low back pain articles; Serious disease articles; Emergency medicine articles
Non traumatic low back pain articles Non traumatic low back pain Research articles Non traumatic low back pain review articles Non traumatic low back pain PubMed articles Non traumatic low back pain PubMed Central articles Non traumatic low back pain 2023 articles Non traumatic low back pain 2024 articles Non traumatic low back pain Scopus articles Non traumatic low back pain impact factor journals Non traumatic low back pain Scopus journals Non traumatic low back pain PubMed journals Non traumatic low back pain medical journals Non traumatic low back pain free journals Non traumatic low back pain best journals Non traumatic low back pain top journals Non traumatic low back pain free medical journals Non traumatic low back pain famous journals Non traumatic low back pain Google Scholar indexed journals Serious disease articles Serious disease Research articles Serious disease review articles Serious disease PubMed articles Serious disease PubMed Central articles Serious disease 2023 articles Serious disease 2024 articles Serious disease Scopus articles Serious disease impact factor journals Serious disease Scopus journals Serious disease PubMed journals Serious disease medical journals Serious disease free journals Serious disease best journals Serious disease top journals Serious disease free medical journals Serious disease famous journals Serious disease Google Scholar indexed journals Emergency medicine articles Emergency medicine Research articles Emergency medicine review articles Emergency medicine PubMed articles Emergency medicine PubMed Central articles Emergency medicine 2023 articles Emergency medicine 2024 articles Emergency medicine Scopus articles Emergency medicine impact factor journals Emergency medicine Scopus journals Emergency medicine PubMed journals Emergency medicine medical journals Emergency medicine free journals Emergency medicine best journals Emergency medicine top journals Emergency medicine free medical journals Emergency medicine famous journals Emergency medicine Google Scholar indexed journals LBP articles LBP Research articles LBP review articles LBP PubMed articles LBP PubMed Central articles LBP 2023 articles LBP 2024 articles LBP Scopus articles LBP impact factor journals LBP Scopus journals LBP PubMed journals LBP medical journals LBP free journals LBP best journals LBP top journals LBP free medical journals LBP famous journals LBP Google Scholar indexed journals Chronic kidney disease articles Chronic kidney disease Research articles Chronic kidney disease review articles Chronic kidney disease PubMed articles Chronic kidney disease PubMed Central articles Chronic kidney disease 2023 articles Chronic kidney disease 2024 articles Chronic kidney disease Scopus articles Chronic kidney disease impact factor journals Chronic kidney disease Scopus journals Chronic kidney disease PubMed journals Chronic kidney disease medical journals Chronic kidney disease free journals Chronic kidney disease best journals Chronic kidney disease top journals Chronic kidney disease free medical journals Chronic kidney disease famous journals Chronic kidney disease Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals pancreas, articles pancreas, Research articles pancreas, review articles pancreas, PubMed articles pancreas, PubMed Central articles pancreas, 2023 articles pancreas, 2024 articles pancreas, Scopus articles pancreas, impact factor journals pancreas, Scopus journals pancreas, PubMed journals pancreas, medical journals pancreas, free journals pancreas, best journals pancreas, top journals pancreas, free medical journals pancreas, famous journals pancreas, Google Scholar indexed journals kidney articles kidney Research articles kidney review articles kidney PubMed articles kidney PubMed Central articles kidney 2023 articles kidney 2024 articles kidney Scopus articles kidney impact factor journals kidney Scopus journals kidney PubMed journals kidney medical journals kidney free journals kidney best journals kidney top journals kidney free medical journals kidney famous journals kidney Google Scholar indexed journals
Article Details
What is already known about non traumatic low back pain?
- Non traumatic Low back pain [LBP] is one of most case presented in emergency department [ED ]
- Almost non traumatic LBP is simple issue and self-limited
- Some studies suggested no need to any image in LBP until after 6 to 8 weeks from the onset.
What is this study adds?
- Some of serious disease could be presented as non-traumatic LBP and may be fatal if not diagnosed early.
- Second visit may need further investigation and image even if the onset less than 6 weeks.
- We collect the learning points together and put it as clinical recommendations and we made low back pain management algorithm to help Emergency physicians to avoid any misdiagnosis of serious disease that presented as non-traumatic low back pain.
1. Introduction
Non-traumatic low back pain (LBP) is one of the most common complaints in the emergency department. Most of these cases require easy treatment and are manageable, but occasionally, non-traumatic LBP is an indication of a serious disease. Although simple LBP is most commonly encountered, detecting such diseases represents a challenge to emergency physicians. Several studies have been conducted on non-traumatic LBP, but some of them may have presented serious diseases as non-traumatic LBP. In fact, some of these studies have suggested that imaging is not needed for non-traumatic LBP until 6 to 8 weeks after its onset [1]. Unfortunately, we found some patients with serious diseases presenting as non-traumatic LBP who died 1-2 weeks after pain onset. In this article, we have discussed five such cases and have proposed some clinical recommendations to manage non-traumatic LBP and avoid missing the diagnosis of serious diseases.
2. Methods
This is a descriptive study, for five case reports that presented with non-traumatic LBP and each one diagnosed as serious disease. We described each case and we put the learning points together as clinical recommendations. Also we made algorithm for non-traumatic low back pain management to help the Emergency physician to avoid any miss diagnosis for any serious disease presented as non-traumatic LBP.
3. Case Descriptions
3.1 Case 1
A 41-year-old South-Asian male patient presented with non-traumatic LBP for 2 weeks with inability to walk well for the last 3 days. Investigations revealed normal muscle tone in both lower limbs with no pain or sign of cord compression. He reported controlled defecation, no urinary incontinence, and no numbness or tingling sensation in either lower limb. Although he appeared sick, his vital signs were stable with no history of fever or cough. A previous X-ray examination at a private clinic had revealed osteolytic lesions L3-L5, and repeat X-ray examination in our emergency department [ED] showed the same results (Figure 1). A computed tomography [CT] scan demonstrated osteolytic lesions at T12 and L3-L5, suggesting tuberculosis [TB] or metastasis to the vertebrae. The patient was then admitted after orthopedic consultation. Magnetic resonance imaging [MRI] showed extensive pathological bone marrow infiltration of the vertebrae with suspicion of metastases (Figure 2). Pathological investigation revealed moderately differentiated metastatic adenocarcinoma, possibly of the lung, although that of the thyroid, pancreas, and biliary tract could not be excluded. The patient was being managed by the orthopedic and oncology teams. His file review revealed bronchial asthma 2 years ago and no history of any other comorbidity. He was diagnosed with non-small cell lung cancer.
3.2 Case 2
A 37-year-old Asian male patient visited the ED with nontraumatic LBP and no other complaint or history of comorbidity. His vital signs were stable with no sign of cord compression. He received a pain killer and was discharged. After 2 days, the man returned with the same complaint and was administered a pain killer. The pain was radiating to the right leg, but he experienced no weakness in the leg and showed stable vital signs. The next day, he visited the ED with severe hypotension and appeared sick. He was admitted to the intensive care unit [ICU] and was diagnosed with septic shock. Chest X-ray examination revealed miliary TB (Figure 3). The following day, the patient died in the ICU. The physicians suspected Pott's disease, which had presented as LBP in the first and second visits. The patient had visited the hospital on Monday, followed by Wednesday and Thursday, and on Friday, he expired.
3.3 Case 3
A 64-year-old Arab male patient presented with LBP. He had fever in the last 3 days and a history of hypertension but not diabetes. His vital signs were stable. The physician recommended abdominal ultrasound to rule out abdominal aortic aneurysm [AAA] as well as blood investigation. Lumbar X-ray examination revealed spondylosis in L5 (Figure 4), and though the patient had no history of epilepsy, he suffered a sudden seizure with status epilepticus in the ED. He was then intubated and transferred to the ICU. The blood reports were unremarkable, abdominal ultrasound ruled out AAA and CT scan of the head was normal. Echocardiography revealed a left ventricular ejection fraction of 63%, abdominal CT revealed spondylosis but ruled out AAA. Electrocardiography [ECG] results were unremarkable. Examination of the cerebrospinal fluid revealed meningoencephalitis. The patient was thus diagnosed with tuberculous meningitis.
3.4 Case 4
A 48-year-old Arab male patient presented with non-traumatic LBP radiating to both legs. However, the gait was normal, and no comorbidity or sign of cord compression was observed. He was alcoholic and a smoker. General examination results were unremarkable. He received a pain killer but as the pain continued, he revisited the observation room for more pain killers and investigation. The pain in his right leg increased along with weakness. A neurosurgical consultation was sought, and one more pain killer was administered which had no effect. MRI showed a bulge in the patient’s L5 and S1 but was asymptomatic. During discharge the patient felt sudden chest pain and palpitation. Reassessment revealed weakness in both the lower limbs with signs of ischemia and chest pain. ECG showed rapid atrial fibrillation (AF) and his troponin level was elevated. CT angiography of the aorta showed aortic occlusion at the distal part of aortic bifurcation and proximal part of both common iliac arteries (Figures 5).
Subsequently, patient underwent laparotomy and thrombectomy and was transferred to the ICU.
3.5 Case 5
A 27-year-old Arab male patient presented with non-traumatic LBP during the first visit for which he received a pain killer. During the second visit, he presented with non-traumatic LBP accompanied by repeated vomiting. He showed signs of dehydration and was sent to the observation room for rehydration and blood investigation. The patient experienced sudden disturbance in consciousness and was intubated. CT scan of the head showed interventricular hemorrhage (Figure 6). He then underwent ventriculostomy and was transferred to the ICU and survived.
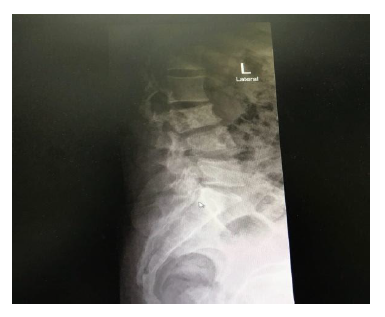
Figure 1: Case1, x ray showed osteolytic lesion L3,4.

Figure 2: Case 1, MRI: showed metastasis on lumbar vertebra.
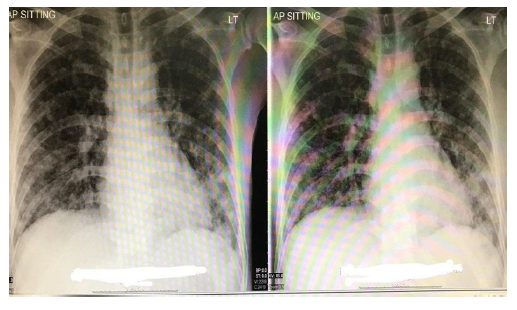
Figure 3: Case 2, x rays showed: millary TB.

Figure 4: Case 3, spondylotic change at L5/S1.
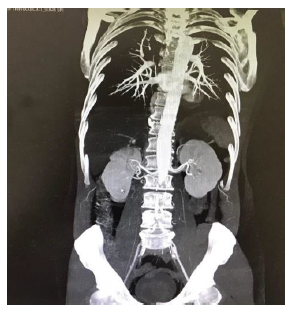
Figure 5: Case 4, C T showed distal aortic occlusion at the site of bifurcation and common iliac arteries.
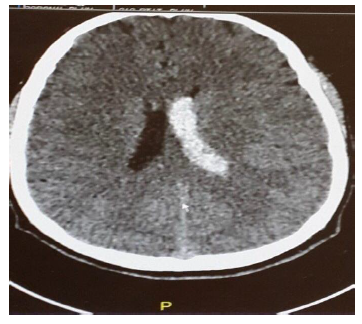
Figure 6: Case 5, CT brain showed inter ventricular hemorrhage.
4. Case Discussions
4.1 Case 1
The patient had non-traumatic LBP for 2 weeks without any neurological deficit, and he could not walk well because of the LBP for 3 days before the visit. He denied any trauma but appeared sick due to the pain. Fortunately, the lumbar radiography he had previously undergone in a private clinic could identify the disease. Based on evidence-based practice, imaging should be performed in patients with LBP 6-8 weeks after the onset even if the patient shows no neurological deficit.
4.2 Case 2
The patient had LBP for 3 days before the first visit with no history of trauma. He died of septic shock after 4 days. Although he had shown no respiratory symptoms during previous visits, chest X-ray examination after septic shock indicated miliary TB. The physicians suspected LBP due to Pott's disease. Unfortunately, he did not undergo lumbar radiography during his first or second visit, which could have detected Pott's disease and he could have been saved.
4.3 Case 3
The key diagnostic feature of this case was the sudden episode of seizure, after which the patient was sent to the observation room for investigation. The patient showed multiple red flags: old age, hypertension and a history of fever in the last 3 days. X-ray examination revealed spondylotic changes in L5/and S1, blood investigation revealed mild leukocytosis [white blood cell count: 11000/ul], abdominal ultrasound ruled out AAA, and chest X-ray findings were unremarkable. He experienced a sudden seizure attack, which led to the diagnosis of meningitis by lumbar puncture. CT scan of the head was unremarkable, and he had no fever on this visit.
4.4 Case 4
The key to diagnostic feature of this case was the persistent pain with rapid progress of the neurological symptoms. However, the patient was discharged as the MRI result could not explain the severe pain. During discharge, the patient experienced severe chest pain with rapid, indication of the vascular cause of LBP. Point-of-Care Ultrasound [POCUS] ruled out AAA, and CT angiography revealed aortic occlusion. Vascular causes of LBP should be considered, especially if MRI does not explain the patient's symptoms.
4.5 Case 5
The key diagnostic feature of this case was the sudden disturbance in consciousness in the ED. Fortunately, during the second visit, the emergency physician sent the patient for observation and blood investigation because he appeared dehydrated. The patient had stable vital signs with no fever or abdominal pain. CT scan of the head should be considered in cases of non-traumatic LBP with persistent vomiting.
5. Short Review
LBP is the fifth most common reason for visiting a physician [1, 2]. Although non-traumatic LBP is benign and self-limited in most cases, it occasionally indicates a serious disease. Emergency physicians must be able to distinguish between patients with benign non-traumatic LBP requiring merely history-taking and physical examination and those with LBP indicative of a serious illness [3]. Causes of acute non-traumatic LBP can be divided into three categories: (i) benign self-limited musculoskeletal causes, (ii) spinal pathologies that can cause severe neurological disability because of spinal cord compression or caudal equina damage, and (iii) other non-spinal causes, such as abdominal or retroperitoneal processes that may cause serious back pain [3]. History-taking and physical examination are crucial for determining the cause of non-traumatic LBP. The patient's response to pain management may also indicate the cause of non-traumatic LBP. Simple back pain may be limited to muscular origin caused by abnormal movement or be associated with degenerative spinal disease. Some authors have contraindicated imaging for LBP within the first 6 weeks after onset unless red flags are present [4]. The clinician should also offer patient education for self-care and discuss noninvasive treatment options, including pharmacological and non-pharmacological pain management therapies [5].
LBP due to spinal pathology can cause severe neurological disability because of the damage to the spinal cord or caudal equina [3]. This type of LBP usually presents with neurological findings, such as sciatica urinary incontinence, uncontrolled defecation, or weakness in the lower limbs [3]. Such cases should be examined using detailed investigations and history-taking [6]; emergency MRI is also recommended [3]. LBP due to non-spinal causes is occasionally associated with serious diseases, which can be identified by detailed history taking and careful examination [7]. In general, such patients present with red flags, such as a history of cancer, old age, immunosuppressive medicine use, IV drug use, and unexplained weight loss. Management of this type of LBP involves blood investigations, including testing of erythrocyte sedimentation rate [ESR], complete blood count [CBC], C-reactive protein [CRP] urea and electrolytes [U&E], lipase, renal function, and liver function. Ultrasound examination may be performed to rule out AAA, cholangitis, and pancreatitis. CT angiography or MRI may also be required [3]. The various red flags identifiable by history-taking and physical examination include a history of cancer, corticosteroid use, anticoagulant use, and abnormal neurological findings, such as gait ataxia [8, 9]. Patients with red flags should always be examined for an underlying systemic disease. The presence of one red flag alone, i.e., a history of cancer, substantially increases the likelihood of cancer [10]. Otherwise, In addition, investigations of inflammatory marker, e.g., ESR, can be used to determine the need for advanced imaging [11].
Most patients presenting with LBP without concerning symptoms can be considered to have nonspecific mechanical back pain. Plain radiography often leads to findings (such as degenerative joint disease, bone spurs, and spondylosis) that are unrelated to pain symptoms. Patients are not recommended radiography unless their pain fails to improve after 4-6 weeks of conservative care [12]. Advanced imaging is generally recommended only for LBP patients with red flags of potentially critical nature [13]. In such patients, further testing is required even if the pain duration is <4 weeks. A meta-analysis of 1,804 patients revealed no difference in outcomes between patients who did not undergo imaging and those who underwent at least one type of imaging, spine radiography or MRI [14]. Another study also randomized 380 back pain patients, who were recommended radiography or MRI in order to compare the outcomes of radiography with that of MRI [14]. Its results revealed that the use of MRI does not improve outcomes, but costs tend to be higher in the MRI group than in the radiography group. This may be because of the increased number of procedures based on abnormal MRI findings that are often incidental, e.g. almost 52% of asymptomatic individuals with no history of back pain have disc bulges and 27% have disc protrusions [15].
6. Conclusions and Recommendations
Based on our practice and evidence-based practice, we propose the following recommendations to manage non-traumatic LBP to avoid missing the diagnosis of a serious disease presenting as non-traumatic LBP:
Al Wakra recommendations for non-traumatic LBP:
- Detailed history-taking and careful physical examination should be performed to determine the cause of LBP so that the patient can receive proper medical care and management for the disease.
- X-ray examination is recommended (i) during the second visit for LBP, (ii) when the patient appears sick, (iii) in case of severe back pain, (iv) when a red flag is present, and (v) if the pain is not relieved by pain killers (persistent pain). Persistent pain can occasionally indicate the diagnosis.
- Emergency MRI should be considered for non-traumatic LBP if the patient shows neurological findings, X-ray findings, or a sign of spinal cord compression.
- The emergency MRI should be accompanied by neurosurgical consultation.
- CT angiography should be considered if the patient shows signs of lower limb ischemia or if the MRI result cannot explain the patient's symptoms.
- Abdominal ultrasound may be considered during the second visit, in case of a red flag presentation from the patient's history, or if the back pain is accompanied by abdominal pain.
- Blood investigations, including testing of CBC, ESR, CRP, U&E, lipase, D dimer, liver and renal functions may be considered in case of a red flag in the patient's history in presence of neurological findings, during the second visit, in cases of LBP accompanied by abdominal pain, and in cases of unclear cause of LBP.
- CT scan of the head may be considered if the LBP is accompanied by persistent vomiting.
- Meningitis should be considered if the patient with non-traumatic LBP has a history of recent fever for which lumbar puncture should be performed as the definitive diagnostic procedure.
- Vascular causes should be considered in sudden onset LBP with unclear cause or with a red flag in the patient's history, such as chronic AF and hypercoagulability. ECG along with vascular examination, e.g., pulse perfusion, and Doppler [imaging] should be performed for both lower limbs.
- Further investigations should be performed during the second and subsequent visits for non-traumatic LBP.
- The algorithm in LBP management may guide in managing LBP, see Figure 7.
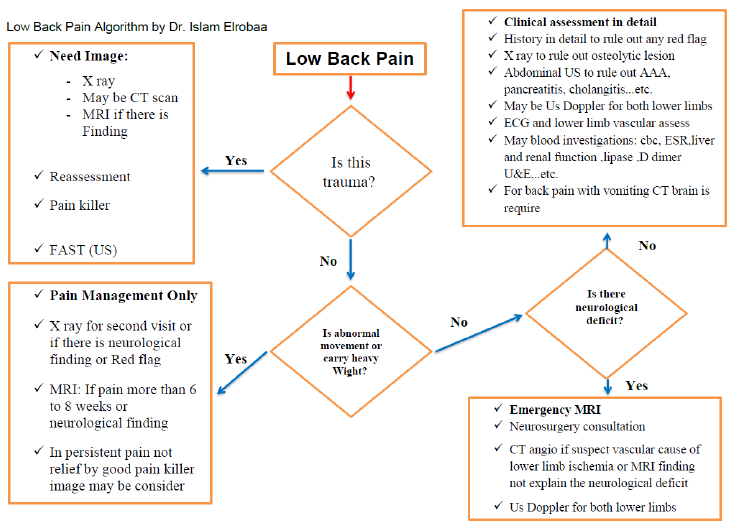
Figure 7: Low back pain management algorithm, Algorithm made by Dr. Islam Elrobaa with under the supervision of Dr. Elfadel Dafalla, Dr. Helmy Elhag and Dr. Hani Aldulimi.
Appendix
Red Flags for a Potentially Serious Underlying Cause of Low Back Pain [16, 17]:
- Age > 50 years
- Duration > 4 weeks
- Focal neurological deficit(s)
- Pain not relief by bed rest
- Thoracic pain or abdominal pain
- History of abdominal aortic aneurysm
- History of cancer Immunosuppression
- HIV
- IV drug use or abuse
- Osteoporosis, prolonged use of corticosteroids,
- Trauma
- Unexplained fever
- Systemic illness
- Unexplained weight loss
- Widespread neurological symptoms (including cauda equina syndrome)
- Structural deformity
Ethical Statement
Our data collected from patients' files without any private or personal information also no intervention. Our manuscript has been accepted for publication by the Medical Research Center, HMC, Qatar under reference number: MRC- 04- 20- 002 that include the Ethical committee approval.
Competing Interests
The authors declare no competing interest.
Authors’ Contributions
Case 1: Islam Hussam Elrobaa, MD; Bassam Adel Fathi, MD; Abdulhadi Haider Khan, MD; Muayad Khalid, MD and Mohamed Abu Elgasem Magram, MD
Case 2: Islam Hussam Elrobaa, MD; Nashat Nabil Ali, MD; Hisham Mohammed Khader, MD; Maria Jennifer Del Castillo, MD and Muayad kassim Khalid, MD
Case 3: Islam Hussam Elrobaa, MD; Abdulhadi Haider Khan, MD and Muayad Kassim Khalid, MD
Case 4: Helmy Gouda Elhag, MD; Islam Hussam Elrobaa, MD; Hani Hamad Aldulimi, MD and Muayad Kasim Khalid, MD
Case 5: Islam Hussam Elrobaa, MD; Hani Hamad Aldulumi, MD and Muayad Kassim Khalid, MD
The low back pain management algorithm by Dr. Islam Elrobaa with under the supervision of Dr. Elfadel Dafalla, Dr. Helmy Elhag and Dr. Hani Aldulimi
References
- Bigos S, Bowyer, Braen G, et al. Acute low back problems in adults. Clinical Practice Guideline (1994).
- Goertz M, Thorson D, Bonsell J, et al. Adult acute and subacute low back pain. Bloomington, MN: Institute for Clinical Systems Improvement (2012).
- Edlow JA. Managing nontraumaticacute back pain. Ann Emerg Med 6 (2015): 148-153.
- National Institute for Health and Clinical Excellence. Low back pain: Early management of persistent non-specific low back pain (2009).
- Chou R, Qaseem A, Snow V, et al. Clinical Efficacy Assessment Subcommittee of the American College of Physicians; American College of Physicians; American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 147 (2007): 478-491.
- Deyo RA, Diehl AK. Cancer as a cause of back pain: frequency, clinical presentation, and diagnostic strategies. J Gen Intern Med 3 (1988): 23238.
- Koes BW, Tulder M, Lin CW, et al. An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. Eur Spine J 19 (2010): 2075-2094.
- Downie A, Williams CM, Henschke N, et al. Red flags to screen for malignancy and fracture in patients with low back pain: Systematic review. BMJ 347 (2013): f7095.
- Thiruganasambandamoorthy V, Turko E, Ansell D, et al. Risk factors for serious underlying pathology in adult emergency department non traumatic low back pain patients. J Emerg Med 47 (2014): 1-11.
- Henschke N, Maher CG, Ostelo RW, et al. Red flags to screen for malignancy in patients with low back pain. Cochrane Database SystRev 2 (2013): CD008686.
- Deyo RA, Diehl AK. Cancer as a cause of back pain: frequency, clinical presentation, and diagnostic strategies. J Gen Intern Med 3 (1988): 230-238.
- Chou R, Qaseem A, Snow V, et al. Clinical Efficacy Assessment Subcommittee of the American College of Physicians, American College of Physicians, American Pain Society Low Back Pain Guidelines Panel. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med 147 (2007): 478-491.
- Jarvik JG. Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med 137 (2002): 586-597.
- Jarvik JG, Hollingworth W, Martin B, et al. Rapid magnetic resonanceimaging vs radiographs for patients with low back pain: a randomizedcontrolled trial. JAMA 289 (2003): 2810-2818.
- Jensen MC, Brant-Zawadzki MN, Obuchowski N, et al. Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331 (1994): 69-73.
- Mike Roscoe, Alyssa Nishihira. Low Back Pain Evidence-based Diagnosis and Treatment. Clinician Reviews 26 (2016): 38-45.
- Robert L Bratton. Assessment and Management of Acute Low Back Pain. Am Fam Physician 60 (1999): 2299-2306.
