No Difference in Failure Rates Between Hybrid Grafts Compared with Hamstring Autografts Following ACL Reconstruction
Article Information
Andrew Jimenez*, Rafael Kakazu, Barton Branam, Angelo Colosimo, Brian Grawe
Department of Orthopaedics Surgery, University of Cincinnati College of Medicine, Ohio, USA
*Corresponding Author: Andrew Jimenez, Department of Orthopaedics Surgery, University of Cincinnati College of Medicine, Ohio, USA
Received: 29 April 2019; Accepted: 10 May 2019; Published: 14 May 2019
Citation: Andrew Jimenez, Rafael Kakazu, Barton Branam, Angelo Colosimo, Brian Grawe. No Difference in Failure Rates Between Hybrid Grafts Compared with Hamstring Autografts Following ACL Reconstruction. Journal of Orthopaedics and Sports Medicine 1 (2019): 028-036.
View / Download Pdf Share at FacebookAbstract
Background: Hamstring tendon autografts, for ACL (anterior cruciate ligament) reconstruction, have demonstrated a higher re-rupture rates when graft diameter of <8 mm is chosen. In the event that an autograft yield a graft diameter <8 mm, augmentation with allograft creates a hybrid graft with increased diameter. Clinical outcomes of this hybrid graft have yet to be established.
Purpose: To assess clinical outcomes and failure rates of an adult population who undergo augmentation with allograft compared to patients with hamstring autograft alone.
Methods: A retrospective chart review of primary ACL reconstructions performed by 4 sports fellowship trained surgeons at a single institution between 2010-2016 identified 23 patients with hamstring autografts and allograft augmentation. A comparison group of 23 patients consisted of patients who underwent ACL reconstruction with hamstring autograft of >8 mm diameter was then selected. The comparison group was matched based on age within 3 years. Graft failure was defined as revision ACL reconstruction or evidence of graft failure on clinical exam (no end point on lachman or pivot shift) or MRI evidence of retear. International Knee Documentation Committee (IKDC), Marx Activity, and Knee injury Osteoarthritis and Outcome (KOOS) scores were obtained. Patients were contacted to obtain information regarding outcome scores, revision procedures, return to sport, and complications. A minimum follow up time was set at 12 months.
Results: Forty-six patients met criteria for inclusion in this study and had follow up data. The hybrid group had a total of 23 patients consisting of 7 men and 16 women with an average age of 31 years (Range 17-51 years). The autograft group had a total of 23 patients con
Keywords
ACL, Allograft, Autograft, Knee, Arthroscopy, Hybrid graft
Orthopaedics surgery articles Orthopaedics surgery Research articles Orthopaedics surgery review articles Orthopaedics surgery PubMed articles Orthopaedics surgery PubMed Central articles Orthopaedics surgery 2023 articles Orthopaedics surgery 2024 articles Orthopaedics surgery Scopus articles Orthopaedics surgery impact factor journals Orthopaedics surgery Scopus journals Orthopaedics surgery PubMed journals Orthopaedics surgery medical journals Orthopaedics surgery free journals Orthopaedics surgery best journals Orthopaedics surgery top journals Orthopaedics surgery free medical journals Orthopaedics surgery famous journals Orthopaedics surgery Google Scholar indexed journals ACL reconstruction articles ACL reconstruction Research articles ACL reconstruction review articles ACL reconstruction PubMed articles ACL reconstruction PubMed Central articles ACL reconstruction 2023 articles ACL reconstruction 2024 articles ACL reconstruction Scopus articles ACL reconstruction impact factor journals ACL reconstruction Scopus journals ACL reconstruction PubMed journals ACL reconstruction medical journals ACL reconstruction free journals ACL reconstruction best journals ACL reconstruction top journals ACL reconstruction free medical journals ACL reconstruction famous journals ACL reconstruction Google Scholar indexed journals Bone patella articles Bone patella Research articles Bone patella review articles Bone patella PubMed articles Bone patella PubMed Central articles Bone patella 2023 articles Bone patella 2024 articles Bone patella Scopus articles Bone patella impact factor journals Bone patella Scopus journals Bone patella PubMed journals Bone patella medical journals Bone patella free journals Bone patella best journals Bone patella top journals Bone patella free medical journals Bone patella famous journals Bone patella Google Scholar indexed journals ACL injuries articles ACL injuries Research articles ACL injuries review articles ACL injuries PubMed articles ACL injuries PubMed Central articles ACL injuries 2023 articles ACL injuries 2024 articles ACL injuries Scopus articles ACL injuries impact factor journals ACL injuries Scopus journals ACL injuries PubMed journals ACL injuries medical journals ACL injuries free journals ACL injuries best journals ACL injuries top journals ACL injuries free medical journals ACL injuries famous journals ACL injuries Google Scholar indexed journals Allograft tissue articles Allograft tissue Research articles Allograft tissue review articles Allograft tissue PubMed articles Allograft tissue PubMed Central articles Allograft tissue 2023 articles Allograft tissue 2024 articles Allograft tissue Scopus articles Allograft tissue impact factor journals Allograft tissue Scopus journals Allograft tissue PubMed journals Allograft tissue medical journals Allograft tissue free journals Allograft tissue best journals Allograft tissue top journals Allograft tissue free medical journals Allograft tissue famous journals Allograft tissue Google Scholar indexed journals Skeletal immaturity articles Skeletal immaturity Research articles Skeletal immaturity review articles Skeletal immaturity PubMed articles Skeletal immaturity PubMed Central articles Skeletal immaturity 2023 articles Skeletal immaturity 2024 articles Skeletal immaturity Scopus articles Skeletal immaturity impact factor journals Skeletal immaturity Scopus journals Skeletal immaturity PubMed journals Skeletal immaturity medical journals Skeletal immaturity free journals Skeletal immaturity best journals Skeletal immaturity top journals Skeletal immaturity free medical journals Skeletal immaturity famous journals Skeletal immaturity Google Scholar indexed journals Multiligamentous knee reconstruction articles Multiligamentous knee reconstruction Research articles Multiligamentous knee reconstruction review articles Multiligamentous knee reconstruction PubMed articles Multiligamentous knee reconstruction PubMed Central articles Multiligamentous knee reconstruction 2023 articles Multiligamentous knee reconstruction 2024 articles Multiligamentous knee reconstruction Scopus articles Multiligamentous knee reconstruction impact factor journals Multiligamentous knee reconstruction Scopus journals Multiligamentous knee reconstruction PubMed journals Multiligamentous knee reconstruction medical journals Multiligamentous knee reconstruction free journals Multiligamentous knee reconstruction best journals Multiligamentous knee reconstruction top journals Multiligamentous knee reconstruction free medical journals Multiligamentous knee reconstruction famous journals Multiligamentous knee reconstruction Google Scholar indexed journals Knee injury articles Knee injury Research articles Knee injury review articles Knee injury PubMed articles Knee injury PubMed Central articles Knee injury 2023 articles Knee injury 2024 articles Knee injury Scopus articles Knee injury impact factor journals Knee injury Scopus journals Knee injury PubMed journals Knee injury medical journals Knee injury free journals Knee injury best journals Knee injury top journals Knee injury free medical journals Knee injury famous journals Knee injury Google Scholar indexed journals Osteoarthritis articles Osteoarthritis Research articles Osteoarthritis review articles Osteoarthritis PubMed articles Osteoarthritis PubMed Central articles Osteoarthritis 2023 articles Osteoarthritis 2024 articles Osteoarthritis Scopus articles Osteoarthritis impact factor journals Osteoarthritis Scopus journals Osteoarthritis PubMed journals Osteoarthritis medical journals Osteoarthritis free journals Osteoarthritis best journals Osteoarthritis top journals Osteoarthritis free medical journals Osteoarthritis famous journals Osteoarthritis Google Scholar indexed journals MRI scans articles MRI scans Research articles MRI scans review articles MRI scans PubMed articles MRI scans PubMed Central articles MRI scans 2023 articles MRI scans 2024 articles MRI scans Scopus articles MRI scans impact factor journals MRI scans Scopus journals MRI scans PubMed journals MRI scans medical journals MRI scans free journals MRI scans best journals MRI scans top journals MRI scans free medical journals MRI scans famous journals MRI scans Google Scholar indexed journals Gracilis tendons articles Gracilis tendons Research articles Gracilis tendons review articles Gracilis tendons PubMed articles Gracilis tendons PubMed Central articles Gracilis tendons 2023 articles Gracilis tendons 2024 articles Gracilis tendons Scopus articles Gracilis tendons impact factor journals Gracilis tendons Scopus journals Gracilis tendons PubMed journals Gracilis tendons medical journals Gracilis tendons free journals Gracilis tendons best journals Gracilis tendons top journals Gracilis tendons free medical journals Gracilis tendons famous journals Gracilis tendons Google Scholar indexed journals Semitendinosus articles Semitendinosus Research articles Semitendinosus review articles Semitendinosus PubMed articles Semitendinosus PubMed Central articles Semitendinosus 2023 articles Semitendinosus 2024 articles Semitendinosus Scopus articles Semitendinosus impact factor journals Semitendinosus Scopus journals Semitendinosus PubMed journals Semitendinosus medical journals Semitendinosus free journals Semitendinosus best journals Semitendinosus top journals Semitendinosus free medical journals Semitendinosus famous journals Semitendinosus Google Scholar indexed journals Femoral articles Femoral Research articles Femoral review articles Femoral PubMed articles Femoral PubMed Central articles Femoral 2023 articles Femoral 2024 articles Femoral Scopus articles Femoral impact factor journals Femoral Scopus journals Femoral PubMed journals Femoral medical journals Femoral free journals Femoral best journals Femoral top journals Femoral free medical journals Femoral famous journals Femoral Google Scholar indexed journals Physical therapy articles Physical therapy Research articles Physical therapy review articles Physical therapy PubMed articles Physical therapy PubMed Central articles Physical therapy 2023 articles Physical therapy 2024 articles Physical therapy Scopus articles Physical therapy impact factor journals Physical therapy Scopus journals Physical therapy PubMed journals Physical therapy medical journals Physical therapy free journals Physical therapy best journals Physical therapy top journals Physical therapy free medical journals Physical therapy famous journals Physical therapy Google Scholar indexed journals Sport articles Sport Research articles Sport review articles Sport PubMed articles Sport PubMed Central articles Sport 2023 articles Sport 2024 articles Sport Scopus articles Sport impact factor journals Sport Scopus journals Sport PubMed journals Sport medical journals Sport free journals Sport best journals Sport top journals Sport free medical journals Sport famous journals Sport Google Scholar indexed journals
Article Details
1. Introduction
ACL injuries are common, affecting 200,000 persons in the United States each year [1]. Most of these patients elect to receive treatment with ACL reconstruction due to symptoms of instability or a desire to continue participation in activities that involve twisting and cutting motions. ACL reconstruction has been very successful; however, graft failure can still occur. Studies to improve the outcomes following ACL reconstructive surgery have focused on many aspects, such as fixation methods, graft type, and graft size. Bone patella bone has been considered the gold standard for reconstruction, but recently quadrupled hamstring tendon has been shown to be biomechanically equivalent in strength, at time zero, and can result in less donor site morbidity when compared to BTB (bone patella tendon bone) [2-4]. Several well-designed studies have confirmed that 8 mm serves as an important predictor of re-tear following ACL surgery [5]. Additionally, smaller hamstring autograft size is a predictor of poorer KOOS sport/recreation subscores 2 years after primary ACL reconstruction [6]. It is often difficult to predict whether or not a patient’s hamstring tendons will be of sufficient size for ACL reconstruction. If the autograft is insufficient, options include a tripling of the semitendinosus graft or augmenting the repair by harvesting the hamstring tendon from the unaffected extremity or by adding allograft tissue.
The purpose of this study is to compare the rates of failure and patient reported outcome scores of patients undergoing ACL reconstruction with a hamstring autograft compared with an autograft-allograft hybrid ACL reconstruction. Our hypothesis is that patients with hybrid ACL graft reconstruction would have similar rates of failure and patient reported outcome scores when compared to a group of matched patients undergoing ACL hamstring autograft reconstruction.
2. Methods
2.1 Study population
This study was approved by the institutional review board for the study of human participants. A retrospective chart review was performed for patients undergoing ACL reconstruction at our institution from January 1, 2011 to December 31, 2015. A total of 697 consecutive patients were identified. Patients were included in the study based upon the graft that was chosen for reconstruction, either those with hamstring autograft alone and those with hamstring autograft augmented with allograft. The exclusion criteria included the revision ACL setting, skeletal immaturity, and multiligamentous knee reconstruction. Application of inclusion and exclusion criteria yielded a total of 23 patients in the hybrid group with complete follow up data. Once the hybrid group was identified, matched controls were obtained from the same database. Controls were matched based on age within 3 years. All control patients underwent primary ACL reconstruction using hamstring autograft. Collected data included graft size, patient demographics, intraoperative findings, and patient reported outcome scores. Outcomes scores obtained were the International Knee Documentation Committee (IKDC), Knee injury and Osteoarthritis Outcome Score (KOOS), and Marx activity score. A minimum follow up time of 12 months was used.
2.2 Data collection
A retrospective chart review was performed on all hybrid and control patients. Data was obtained from preoperative clinic notes, preoperative MRI scans, operative reports, postoperative clinic notes, and postoperative MRI scans. Patients were contacted by phone and completed IKDC, KOOS, Marx Activity surveys. They were also asked to report any additional procedures performed on their leg, return to sport, and Likert pain and satisfaction scores.
2.3 Surgical technique
The semitendinosus and gracilis tendons were harvested via a standard anterior approach, stripped of muscle, whipstitched on both ends, and folded over to form a 4-stranded graft. This graft was then measured to determine diameter. Grafts with a diameter of less than 8 mm were augmented with a semitendinosus tendon allograft (Figure 1). An arthroscopic assisted technique was then used to complete the ACL reconstruction. Femoral tunnels were drilled through a transtibial method or the anterior medial portal per the preference of the attending surgeon. The femoral tunnel was drilled to the same diameter as the prepared graft. Femoral fixation was performed with suspensory fixation in all cases using the EndoButton (Smith and Nephew, London, England). Tibial fixation was achieved with an interference screw and backed up with either a staple, a suture to a post or a knotless suture anchor (Figure 2, 3). Unless a concomitant meniscal repair was performed, all patients underwent a standard rehabilitation protocol. At our institution, this included full weight bearing and a successive physical therapy program. Strength training was slowly begun, with open chain quadriceps activity beginning at 6 weeks. The patient is typically able to job at around 3 months with an expected return to sport and cutting activities between 6-8 months.
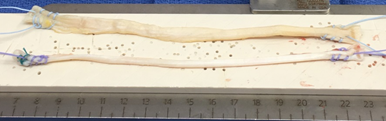
Figure 1: Clinical Image of semitendinosus allograft (top) and hamstring autograft (bottom).

Figure 2: AP radiograph of ACL reconstruction with hybrid graft.
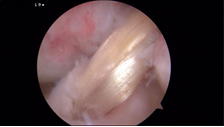
Figure 3: Arthroscopic image of hybrid graft after ACL Reconstruction.
2.4 Data analysis
SPSS for Windows (version 22; SPSS, Chicago, IL) was used for statistical analysis. An independent t-test was used for comparing continuous variables. A chi square test was used for categorical variables. The significance level was set at p<0.05. Any patients in the hybrid group who were lost to follow up were not included in the final statistical analysis.
3. Results
3.1 Demographics
The hybrid group had a total of 23 patients consisting of 7 men and 16 women with an average age of 31 years (CI 26.6-35.5 years). The autograft group had a total of 23 patients consisting of 17 men and 6 women with an average age of 33.3 years (CI 29.9-36.7). Average BMI in the autograft group was 26.1 compared to 30.5 in the hybrid group (p=0.064) The mean overall graft size was 9.1 mm (range 8-11 mm) in the autograft group and 10 mm (range 9-11mm) in the hybrid group. The average follow-up between both groups was 31.5 months (range 12-63 months), with 36 months (30.8-42.2) and 26 months (22.7-30.1) for autograft and hybrid groups respectively (p=0.0038). In terms of concomitant procedures performed during the ACL reconstruction, 52.1% (12 of 23 patients) underwent the medial meniscus procedure in the autograft group compared to 39.1% (9 of 23 patients) in the hybrid group (p=0.37453). Eleven patients in the autograft group (47.8%) underwent a lateral meniscus procedure compared to 5 in the hybrid group (21.7%) (p=0.063). Additionally, 21.7% (5 of 23 patients) underwent treatment for cartilage injury in the autograft group compared to 17.4% (4 of 23 patients) in the hybrid group. In each group this treatment was limited to either microfracture or chondroplasty. The data is summarized in Table 1.
|
Data |
Autograft |
Hybrid |
p |
|
Female |
6 |
16 |
*0.0031 |
|
Age (years, mean, CI) |
33.3 (29.9-36.7) |
31 (26.6-35.5) |
0.41 |
|
BMI (kg/m2, mean, CI) |
26.1 (23.7-28.4) |
30.5 (26.4-34.6) |
0.064 |
|
Graft Diameter (mm) |
9.13 (8.81-9.45) |
10.1 ( 9.77-10.4) |
*0.00006 |
|
Followup Time (months, mean, CI) |
36.5 (30.8-42.2) |
26.4 (22.7-30.1) |
*0.0038 |
|
Return to Sport |
20 (87%) |
15 (65.2%) |
0.083 |
|
Associated Procedure |
|||
|
Medial meniscus |
12 (52.1%) |
9 (39.1%) |
0.37 |
|
Lateral meniscus |
11 (47.8%) |
5 (21.7%) |
0.063 |
|
Cartilage Procedure |
5 (21.7%) |
4 (17.4%) |
0.71 |
Table 1: Summary of demographic data for the study population.
|
Data |
Autograft |
Hybrid |
p |
|
Failure Rate |
1 (4.3%) |
2 (8.7%) |
0.49 |
|
Reoperation Rate |
4 (17.4%) |
3 (13.0%) |
0.68 |
|
IKDC |
73.8 (66.6-80.9) |
67.8 (59.8-75.9) |
0.26 |
|
KOOS |
86.5 (81.4-91.7) a |
75.8 (67.5-84.1) |
*0.03 |
|
Pain |
89.5 (82.6-96.4) b |
81.4 (73.6-89.3) c |
0.08 |
|
Symptoms |
82.4 (74.7-90.0) b |
79.3 (71.9-86.6) c |
0.32 |
|
Activity |
93.4 (88.5-98.4) b |
88.8 (80.5-97.2) c |
0.32 |
|
Sports |
75.3 (63.1-87.4) b |
69 (55.5-82.5) c |
0.44 |
|
Quality of Life |
68.7 (55.7-81.7) b |
57.8 (44.9-70.7) c |
0.27 |
|
Return to Sport |
20 (87%) |
15 (65.2%) |
0.083 |
|
Marx |
7.8 (5.63-9.94) |
5.9 (4.00-7.8) |
0.18 |
Table 2: Summary of results for the study population. All are n=23 unless noted. 95% CI in parenthesis a: n=21; b: n=19; c: n=20.
3.2 Failure rate
The graft failure rate in the hybrid group was 8.7% (2 of 23 patients), while the autograft group demonstrated a graft failure rate of 4.3% (1 of 23 patients) (p=0.49). For both groups, graft failure was determined by physical examination with a pivot shift in 1 patient and arthroscopically confirmed during revision surgery in 2 patients. One patient from each group underwent revision ACL reconstruction after failure of their initial procedure. One patient with a failed hybrid reconstruction elected not to undergo revision surgery (Figure 4).
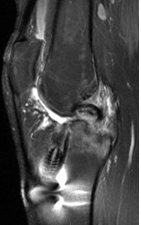
Figure 4: MRI of a failed hybrid ACL reconstruction.
3.3 Reoperation rate
In the autograft ACL group there were a total of 4 patients who underwent another procedure on their reconstructed knee after their index reconstruction procedure. One underwent a revision ACL reconstruction, another for a manipulation under anesthesia due to stiffness, a third patient underwent a partial meniscectomy on a meniscus that was repaired during their primary ligament reconstruction, and a final patient underwent irrigation and debridement of a suture abscess four weeks post operatively from their ACL reconstruction. The hybrid group had 3 patients undergo surgery on their operative extremity after their index ACL reconstruction. One was for a revision ACL reconstruction and 2 for irrigation and debridement for surgical site infection 6 months post-operatively. The overall rates of reoperation for any reason were 17.4% (4 of 23) of the autograft group and 13.0% of those in the hybrid group [(3 of 23) (p=0.068)].
3.4 Functional outcomes
In the hybrid ACL group, the mean IKDC was 67.8 (CI 59.8-75.9) compared to 73.8 (CI 66.6-80.9) in the autograft group (p=0.26). The average KOOS scores for the hybrid group was 75.8 (CI 67.5-84.1) compared to 86.5 (CI 81.4-91.7) in the autograft group (p=0.03). KOOS subsection scores were available for 20 in the hybrid group and 19 in the autograft group. The subsections of the KOOS score displayed an average of 89.5 compared to 81.4 (p=0.08) for “pain”, 82.4 vs 79.27 (p=0.55) for “symptoms”, 93.44 vs 88.84 (p=0.32) for “activity, 75.3 vs 69.0 (p=0.44) for “sports”, and 68.7 vs 57.8 (p=0.27) for “quality of life” in the autograft and hybrid groups, respectively. In terms of return to sport, 65% (15 of 23 patients) in the hybrid group and 87% (20 of 23 patients) in the autograft group returned to their sport (p=0.08). Lastly, the Marx activity score of patients in the autograft group was 7.8 opposed to 5.9 in the hybrid group (p=0.18). Outcome scores are summarized in Table 2.
4. Discussion
In our series, allograft-autograft hybrid hamstring graft failure had no statistically significant difference compared to that of the hamstring autograft group. Failure rate of the hybrid graft was 8.7% (2 of 23 patients) compared to 4.3% (1 of 23 patients) in the autograft group (p=0.49). Our study did not demonstrate a statistically significant difference in the IKDC patient reported outcome score, but it did show a difference in the overall KOOS score [86.5 (CI 81.4-91.7) in the autograft group, 75.8 (CI 67.5-84.1) In the hybrid group (p=0.03)]. Despite this difference, there was no statistically significant difference in the subsections of the KOOS between the two groups; in each subsection the scores were lower in the hybrid group compared to the autograft group. Hybrid grafts have been a commonly used solution for a patient with a small hamstring autograft diameter. It allows the surgeon to augment the overall graft size to create an overall graft diameter of 8mm or greater [5-7]. It has been hypothesized that supplementation of the undersized autograft with allograft could diminish the risk of rerupture associated with critically small graft diameters.
There have been several studies in recent years examining failure rates of hybrid graft constructs compared to autograft only constructs in an adult population with somewhat varied results. Burrus et al. [8] published on their series in 2015, which demonstrated a statistically significant increased rate of graft rupture or graft compromise in hybrid graft patients as compared to a control group of autograft patients. In their series, they showed a rate of hybrid graft rupture or graft compromise in 38% of knees compared to 7% of their control autograft group (p=0.005) [8]. Additionally, they showed a significantly worse IKDC score in the hybrid compared to the autograft group, 71.3 and 85.7 respectively (p=0.012). In contrast to these results, Darnley et al. published data on autograft ACL reconstructions compared to hybrid graft reconstructions using MOON registry data in 2016 [9]. In their study, they demonstrated no statistically significant difference with regards to patient outcome scores or revision surgery. In their series, revision surgery was performed in 18.5% of hybrid patients and 7.4% of autograft reconstruction patients (p=0.26). Both of these studies were underpowered to detect a difference in failure risk between hybrid and autograft, but they both showed higher rates of failure in the hybrid graft. The results from our study are in agreement with the MOON study demonstrating no difference of failure rate between the two groups, but similar to the study by Burrus et al. [8] in that we showed a statistically significantly worse patient reported outcome score. Their study demonstrated a lower IKDC score in the hybrid group, whereas our study has demonstrated a lower KOOS score. It is unclear the exact cause of our lower KOOS score. We theorize that it may be due to an overall higher level of athlete in our autograft population, compared to our hybrid population, which is in turn a direct result of the selection bias that is associated with the retrospective nature of the study. In our autograft cohort, we had 11 patients who participated in a sport at a competitive level, whereas only 6 were marked that they participated in competitive athletics in the hybrid group. Although this difference did not reach statistical significance in our study, it may contribute the disparity in KOOS scores. It is possible that a higher quality athlete may be more likely to inherently have a more robust tissue compared to an equally active, but less athletic counterpart based upon previously reported studies regarding demographics and hamstring diameter [10].
Despite the larger number of competitive athletes in the autograft group, there was an equal number of patients participating in high risk sports for ACL injury. We defined high risk sports as football, soccer, rugby, basketball, skiing. In each group there were 5 patients participating in these higher risk sports. The most common sports response for sports participation and level was recreational running between the two groups. Our study population differed with regard to proportion of females and follow-up time. The autograft group had a significantly longer follow-up time (36.5 months vs 26.4 months, p=0.0038), which would potentially capture more graft failures. As such, it is possible that our study underestimates the graft failures in the hybrid group. Several animal studies and human MRI studies have shown slow revascularization and ligamentization in allografts tissue [11, 12]. As a result, it has been proposed that return to activity and sport should be slower in a hybrid graft construct compared to a purely autograft reconstruction. The mean time to hybrid graft revision was 11.3 months in the Darnley et al. series. In the series reported by Burrus and colleagues all hybrid failures occurred within 9.3 months. Failures that we have reported in our study all occurred within 13 months. Allograft processing has also been shown to have an impact on mechanical properties and consideration should be given to allograft processing methods [11, 13]. In our series, which involved all sports fellowship trained surgeons, no high dose terminal irradiation was used similar to the studies by Burrus, et al. [8] and Darnley, et al. [9]. The use of low dose irradiation techniques in allograft processing has been shown to have a minimal effect on the graft’s mechanical properties [14].
This study has several limitations. Similar to the other reported studies on this subject, it is underpowered to definitively determine whether there is a statistically significant difference in failure between hybrid and autograft ACL reconstructions. Additionally, the retrospective nature of the study introduces selection bias. Based on our database search, this is not a common procedure, which makes obtaining large numbers difficult. Recent studies are also demonstrating methods to predict graph size to obviate the potential need for allograft augmentation.
5. Conclusion
Patients who undergo ACL reconstruction with hybrid hamstring grafts did not have a statistically significant difference in failure rate or reoperation rate compared to an autograft control group.
References
- Timothy E Hewett, Sandra J Shultz and LYG. Understanding and Preventing Noncontact ACL injuries. Am Orthop Soc Sport Med (2007): 163-171.
- Ahldén M, Samuelsson K, Sernert N, et al. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med 40 (2012): 2230-2235.
- Hamner DL, Brown CH, Steiner ME, et al. Hamstring tendon grafts for reconstruction of the anterior cruciate ligament: biomechanical evaluation of the use of multiple strands and tensioning techniques. J Bone Joint Surg Am 81 (1999): 549-557.
- Wilson TW, Zafuta MP, Zobitz M. A biomechanical analysis of matched bone-patellar tendon-bone and double-looped semitendinosus and gracilis tendon grafts. Am J Sports Med 27 (1999): 202-207.
- Magnussen RA, Lawrence JTR, West RL, et al. Graft size and patient age are predictors of early revision after anterior cruciate ligament reconstruction with hamstring autograft. Arthroscopy 28 (2012): 526-531.
- Mariscalco MW, Flanigan DC, Mitchell J, et al. The influence of hamstring autograft size on patient-reported outcomes and risk of revision after anterior cruciate ligament reconstruction: A Multicenter Orthopaedic Outcomes Network (MOON) Cohort Study. Arthroscopy 29 (2013): 1948-1953.
- Park SY, Oh H, Park S, et al. Factors predicting hamstring tendon autograft diameters and resulting failure rates after anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc 21 (2013): 1111-1118.
- Burrus MT, Werner BC, Crow AJ, et al. Increased Failure Rates After Anterior Cruciate?? Ligament Reconstruction With Soft-Tissue Autograft-Allograft Hybrid Grafts. Arthroscopy Arthroscopy Association of North America 31 (2015): 2342-2351.
- Darnley JE, Léger-St-Jean B, Pedroza AD, et al. Anterior Cruciate Ligament Reconstruction Using a Combination of Autograft and Allograft Tendon. Orthop J Sport Med 4 (2016): 2325967116662249.
- Grawe BM, Williams PN, Burge A, et al. Anterior Cruciate Ligament Reconstruction With Autologous Hamstring: Can Preoperative Magnetic Resonance Imaging Accurately Predict Graft Diameter? Orthop J Sport Med 4 (2016): 2325967116646360.
- Fideler BM, Vangsness CT, Bin Lu B, et al. Gamma Irradiation: Effects on Biomechanical Properties of Human Bone-Patellar Tendon-Bone Allografts. Am J Sports Med 23 (1995): 643-646.
- Scheffler SU, Schmidt T, Gangéy I, et al. Fresh-frozen free-tendon allografts versus autografts in anterior cruciate ligament reconstruction: delayed remodeling and inferior mechanical function during long-term healing in sheep. Arthroscopy 24 (2008): 448-458.
- Rasmussen TJ, Feder SM, Butler DL, et al. The effects of 4 Mrad of gamma irradiation on the initial mechanical properties of bone-patellar tendon-bone grafts. Arthroscopy 10 (1994): 188-197.
- Balsly CR, Cotter AT, Williams LA, et al. Effect of low dose and moderate dose gamma irradiation on the mechanical properties of bone and soft tissue allografts. Cell Tissue Bank 9 (2008): 289-298.
- Sanders TL, Kremers HM, Bryan AJ, et al. Is Anterior Cruciate Ligament Reconstruction Effective in Preventing Secondary Meniscal Tears and Osteoarthritis? Am J Sports Med 44 (2016): 1699-1707.
