Functional Outcome of Modified Open Bankart Surgery in Military Personnel for Traumatic, Recurrent, Anterior Glenohumeral Dislocations
Article Information
Zafar Israil1 *, Pankaj Poswal2, Prasenjeet Singh2, Ravindra Chauhan3
1Orthopaedic surgeon, practising in the Army Medical Corps, Indian Army, India
2Orthopaedic surgeon, Military Hospital, Agra, Delhi, India
3Orthopaedic surgeon, Base Hospital, Delhi Cantt, India
*Corresponding Author: Zafar Israil, Orthopaedic surgeon, practising in the Army Medical Corps, Indian Army, India
Received: 24 May 2021; Accepted: 02 June 2021; Published: 17 June 2021
Citation: Zafar Israil, Pankaj Poswal, Prasenjeet Singh, Ravindra Chauhan. Functional Outcome of Modified Open Bankart Surgery in Military Personnel for Traumatic, Recurrent, Anterior Glenohumeral Dislocations. Journal of Orthopaedics and Sports Medicine 3 (2021): 088-101.
View / Download Pdf Share at FacebookAbstract
Introduction: This study evaluates the functional outcome of modified open Bankart surgery in military personnel for traumatic, recurrent, anterior glenohumeral dislocations. With the arthroscope unavailable, there was no selection bias and 5 military orthopedic surgeons used modification of the Bankart procedure. Metallic suture anchors were used for repair of avulsed labrum along with capsular repair.
Materials and methods: This Case series was done in 30 male soldiers (30 shoulders) over a span of 4 years (2011-2014). Only recurrent (>2 dislocations), traumatic, anterior and unilateral glenohumeral dislocations were included. Hill Sach’s lesion >20 %, glenoid bone loss >10 %, atraumatic MDI, associated SLAP/Rotator cuff lesions were excluded. Pre op MRI and CT was done in all cases. All patients were followed up for a minimum of 2 years, with patients reporting regularly to the center as per existing defence medical regulations.
Results: The mean pre op Rowe score was 40.6 and mean post op Rowe score was 86.6. The mean loss of external rotation was 4.3 degrees (0 to 15 degrees) and 40 % of the study group had no loss of external rotation.76.6% of the patients (n=23) had excellent or good post op Rowe scores and were upgraded to join/continued to serve in armed forces. 23.3% of patients (n=7) had fair and poor post op Rowe scores (<75) at 2 year follow up. The failure rate was 6% with 2 patients having complications. One patient had backing out of suture anchors requiring re-surgery and the other having persistent feeling of subluxation. We conclude that modified Bankart surgery is a suitable option for military personnel.
Keywords
Modified open bankart; Anterior shoulder instability; Military; Functional outcomes; Rowe scores
Open bankart surgery articles Open bankart surgery Research articles Open bankart surgery review articles Open bankart surgery PubMed articles Open bankart surgery PubMed Central articles Open bankart surgery 2023 articles Open bankart surgery 2024 articles Open bankart surgery Scopus articles Open bankart surgery impact factor journals Open bankart surgery Scopus journals Open bankart surgery PubMed journals Open bankart surgery medical journals Open bankart surgery free journals Open bankart surgery best journals Open bankart surgery top journals Open bankart surgery free medical journals Open bankart surgery famous journals Open bankart surgery Google Scholar indexed journals Climbing vertical rope articles Climbing vertical rope Research articles Climbing vertical rope review articles Climbing vertical rope PubMed articles Climbing vertical rope PubMed Central articles Climbing vertical rope 2023 articles Climbing vertical rope 2024 articles Climbing vertical rope Scopus articles Climbing vertical rope impact factor journals Climbing vertical rope Scopus journals Climbing vertical rope PubMed journals Climbing vertical rope medical journals Climbing vertical rope free journals Climbing vertical rope best journals Climbing vertical rope top journals Climbing vertical rope free medical journals Climbing vertical rope famous journals Climbing vertical rope Google Scholar indexed journals Orthopaedic surgeon articles Orthopaedic surgeon Research articles Orthopaedic surgeon review articles Orthopaedic surgeon PubMed articles Orthopaedic surgeon PubMed Central articles Orthopaedic surgeon 2023 articles Orthopaedic surgeon 2024 articles Orthopaedic surgeon Scopus articles Orthopaedic surgeon impact factor journals Orthopaedic surgeon Scopus journals Orthopaedic surgeon PubMed journals Orthopaedic surgeon medical journals Orthopaedic surgeon free journals Orthopaedic surgeon best journals Orthopaedic surgeon top journals Orthopaedic surgeon free medical journals Orthopaedic surgeon famous journals Orthopaedic surgeon Google Scholar indexed journals Shoulder dislocation articles Shoulder dislocation Research articles Shoulder dislocation review articles Shoulder dislocation PubMed articles Shoulder dislocation PubMed Central articles Shoulder dislocation 2023 articles Shoulder dislocation 2024 articles Shoulder dislocation Scopus articles Shoulder dislocation impact factor journals Shoulder dislocation Scopus journals Shoulder dislocation PubMed journals Shoulder dislocation medical journals Shoulder dislocation free journals Shoulder dislocation best journals Shoulder dislocation top journals Shoulder dislocation free medical journals Shoulder dislocation famous journals Shoulder dislocation Google Scholar indexed journals Sports and games articles Sports and games Research articles Sports and games review articles Sports and games PubMed articles Sports and games PubMed Central articles Sports and games 2023 articles Sports and games 2024 articles Sports and games Scopus articles Sports and games impact factor journals Sports and games Scopus journals Sports and games PubMed journals Sports and games medical journals Sports and games free journals Sports and games best journals Sports and games top journals Sports and games free medical journals Sports and games famous journals Sports and games Google Scholar indexed journals Physical training articles Physical training Research articles Physical training review articles Physical training PubMed articles Physical training PubMed Central articles Physical training 2023 articles Physical training 2024 articles Physical training Scopus articles Physical training impact factor journals Physical training Scopus journals Physical training PubMed journals Physical training medical journals Physical training free journals Physical training best journals Physical training top journals Physical training free medical journals Physical training famous journals Physical training Google Scholar indexed journals Sportsmen articles Sportsmen Research articles Sportsmen review articles Sportsmen PubMed articles Sportsmen PubMed Central articles Sportsmen 2023 articles Sportsmen 2024 articles Sportsmen Scopus articles Sportsmen impact factor journals Sportsmen Scopus journals Sportsmen PubMed journals Sportsmen medical journals Sportsmen free journals Sportsmen best journals Sportsmen top journals Sportsmen free medical journals Sportsmen famous journals Sportsmen Google Scholar indexed journals Arthroscopic shoulder surgery articles Arthroscopic shoulder surgery Research articles Arthroscopic shoulder surgery review articles Arthroscopic shoulder surgery PubMed articles Arthroscopic shoulder surgery PubMed Central articles Arthroscopic shoulder surgery 2023 articles Arthroscopic shoulder surgery 2024 articles Arthroscopic shoulder surgery Scopus articles Arthroscopic shoulder surgery impact factor journals Arthroscopic shoulder surgery Scopus journals Arthroscopic shoulder surgery PubMed journals Arthroscopic shoulder surgery medical journals Arthroscopic shoulder surgery free journals Arthroscopic shoulder surgery best journals Arthroscopic shoulder surgery top journals Arthroscopic shoulder surgery free medical journals Arthroscopic shoulder surgery famous journals Arthroscopic shoulder surgery Google Scholar indexed journals Shoulder surgeons articles Shoulder surgeons Research articles Shoulder surgeons review articles Shoulder surgeons PubMed articles Shoulder surgeons PubMed Central articles Shoulder surgeons 2023 articles Shoulder surgeons 2024 articles Shoulder surgeons Scopus articles Shoulder surgeons impact factor journals Shoulder surgeons Scopus journals Shoulder surgeons PubMed journals Shoulder surgeons medical journals Shoulder surgeons free journals Shoulder surgeons best journals Shoulder surgeons top journals Shoulder surgeons free medical journals Shoulder surgeons famous journals Shoulder surgeons Google Scholar indexed journals Rehabilitation articles Rehabilitation Research articles Rehabilitation review articles Rehabilitation PubMed articles Rehabilitation PubMed Central articles Rehabilitation 2023 articles Rehabilitation 2024 articles Rehabilitation Scopus articles Rehabilitation impact factor journals Rehabilitation Scopus journals Rehabilitation PubMed journals Rehabilitation medical journals Rehabilitation free journals Rehabilitation best journals Rehabilitation top journals Rehabilitation free medical journals Rehabilitation famous journals Rehabilitation Google Scholar indexed journals Glenohumeral instability articles Glenohumeral instability Research articles Glenohumeral instability review articles Glenohumeral instability PubMed articles Glenohumeral instability PubMed Central articles Glenohumeral instability 2023 articles Glenohumeral instability 2024 articles Glenohumeral instability Scopus articles Glenohumeral instability impact factor journals Glenohumeral instability Scopus journals Glenohumeral instability PubMed journals Glenohumeral instability medical journals Glenohumeral instability free journals Glenohumeral instability best journals Glenohumeral instability top journals Glenohumeral instability free medical journals Glenohumeral instability famous journals Glenohumeral instability Google Scholar indexed journals Rotator cuff articles Rotator cuff Research articles Rotator cuff review articles Rotator cuff PubMed articles Rotator cuff PubMed Central articles Rotator cuff 2023 articles Rotator cuff 2024 articles Rotator cuff Scopus articles Rotator cuff impact factor journals Rotator cuff Scopus journals Rotator cuff PubMed journals Rotator cuff medical journals Rotator cuff free journals Rotator cuff best journals Rotator cuff top journals Rotator cuff free medical journals Rotator cuff famous journals Rotator cuff Google Scholar indexed journals Glenoid bone articles Glenoid bone Research articles Glenoid bone review articles Glenoid bone PubMed articles Glenoid bone PubMed Central articles Glenoid bone 2023 articles Glenoid bone 2024 articles Glenoid bone Scopus articles Glenoid bone impact factor journals Glenoid bone Scopus journals Glenoid bone PubMed journals Glenoid bone medical journals Glenoid bone free journals Glenoid bone best journals Glenoid bone top journals Glenoid bone free medical journals Glenoid bone famous journals Glenoid bone Google Scholar indexed journals Cephalic vein articles Cephalic vein Research articles Cephalic vein review articles Cephalic vein PubMed articles Cephalic vein PubMed Central articles Cephalic vein 2023 articles Cephalic vein 2024 articles Cephalic vein Scopus articles Cephalic vein impact factor journals Cephalic vein Scopus journals Cephalic vein PubMed journals Cephalic vein medical journals Cephalic vein free journals Cephalic vein best journals Cephalic vein top journals Cephalic vein free medical journals Cephalic vein famous journals Cephalic vein Google Scholar indexed journals Swimming articles Swimming Research articles Swimming review articles Swimming PubMed articles Swimming PubMed Central articles Swimming 2023 articles Swimming 2024 articles Swimming Scopus articles Swimming impact factor journals Swimming Scopus journals Swimming PubMed journals Swimming medical journals Swimming free journals Swimming best journals Swimming top journals Swimming free medical journals Swimming famous journals Swimming Google Scholar indexed journals
Article Details
1. Introduction
Recurrent anterior dislocation of the shoulder in military personnel is a serious problem. The arduous training involves difficult upper body exercises e.g. climbing vertical rope, horizontal rope and jumping from 10 meters high dive board. Also these personnel have to participate in contact sports as well as overhead activities, which predispose them to injuries and accidents leading to shoulder dislocation. Sports and games are an integral part of soldierly life. In addition many arms and services involve physical training and hard labour during routine activites, due to which it is necessary to consider them in the same set as sportsmen.
After a shoulder dislocation, it is expected that a paramedic or coach tries to relocate the shoulder using any known method. The process may or may not be successful and the patient is brought to a military doctor who attempts close reduction or then refers to an Orthopaedic set up. After the emergency reduction of shoulder by either the Regimental medical officer or Surgeon/Orthopaedic surgeon the patient is analysed by x -rays to confirm the relocation. The particular patient’s recurrent instability is thoroughly analysed and he is given a choice for open/arthroscopic shoulder surgery.
The patient has full liberty to choose the timing of his surgery and is put in ‘Low Medical Category’ classification till he functionally improves, with or without surgery. As per defence medical regulations, he is followed up at 6 to 8 weeks followed by 6 monthly and later, every 2 years, till the end of his service. In a series of US Army soldiers, Bottoni et al [1] reported that 75% of patients managed non operatively had recurrent instability and 67% underwent surgery for the same. Wheeler et al [2] found that in US Military Academy, the cadets had a 92% instability rate after non operative treatment.
This study was carried out from 2011 to 2014 at a tertiary orthopaedic center with 5 military orthopaedic surgeons out of which none of them were exclusive Shoulder surgeons. The limitations of breakdown of arthroscope or its accessories, along with steep learning curve made it imperative to take up patients for open bankart surgery. The open Bankart surgery has been modified by Altchek [3] using a T plasty modification which theoretically allowed both a capsulolabral reattachment using suture anchors and capsular repair followed by scarring which should decrease antero-inferior capsular redundancy. Neer and Foster [4] have also described a inferior capsular shift for Multi directional instability to decrease capsular volume. However the premise that capsular tightening would cause loss of external rotation needed to be analyzed in this sub group of population.
To standardize the procedure, capsular reinforcement at the time of closure was done at 30degrees of abduction and 30 degrees of external rotation [5]. The aim of the study was to find the 1) functional outcomes using Rowe scores and 2) loss of external rotation at 2 year follow up, 3) epidemiological survey of events leading to first dislocation in this cohort.
2. Materials and Methods
This case series was done in a tertiary military hospital which has a teaching and Orthopaedic referral unit. After approval of Institutional Review Board and Ethics Committee, the study was designed to include only military personnel from 2011 to 2014, suffering from recurrent anterior shoulder dislocation and choosing to undergo elective shoulder surgery. Only recurrent (>2 dislocations), traumatic anterior unilateral glenohumeral dislocations were included. Hill Sach’s lesion > 20 % or glenoid bone loss>10% were excluded. Subjects with MDI, Revision cases and associated rotator cuff lesion cases were not included in this study design.
First time dislocators are generally unwilling for surgery in this group of patients and were excluded. The patients were given to sign an informed consent and the surgical technique was modified open Bankart repair, albeit with slight variations in capsular closure due to 5 different surgeons operating. The age distribution was 18 to 45 yrs (mean age 30 yrs) and included recruits and cadets (age>19 years). This subset of the cohort were training to join armed forces and formed 16.7 % (n=5) of the total subjects being studied. However, they had only 6 months for post op rehabilitation and return to training level fitness before they see a medical board. Rest of them comprised of military personnel who were given ‘Low medical category’ depending on their performance and ability to come back to preinjury levels, notwithstanding any threat to their job.
Pre op clinical evaluation was done for glenohumeral instability, capsular laxity and rotator cuff functioning. All patients were evaluated with Rowe scores, and ROM was measured and tabulated. Pre op MRI was done for confirmation of bankart lesion as well as to exclude any other associated pathology. (See Image A). CT scan for bilateral shoulders was done in all cases to find bipolar bone loss. Using 3D CT, enface view of glenoid with humeral subtraction, glenoid bone loss was calculated. It was then compared with contralateral glenoid using linear measurement [6]. Also Glenoid track width [7] was calculated and compared to Hill Sach’s interval using 3D CT [6]. All bipolar bone loss cases which were on track [6] Hill Sach’s lesion were selected for modified open bankart surgery.
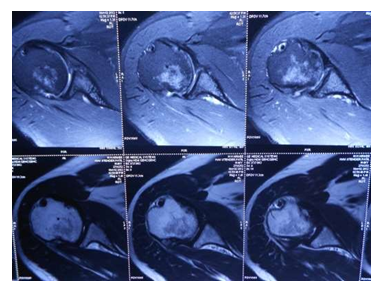
Image A: MRI Shoulder: axial views showing fibrocartilaginous bankart lesion.
2.1 Surgical technique
All patients were administered GA supplemented with interscalene block. Both beach chair and supine position were used depending on surgeon’s preference (See Image B). Deltopectoral approach was used. Cephalic vein was identified and taken medially or laterally (See Image C). Clavipectoral was incised and Subscapularis exposed, without trying to isolate the axillary nerve. The subscapularis was incised in a L shaped incision at about 1 cm from its humeral insertion or split in line of its fibres at the junction of upper 2/3rd and lower 1/3rd, depending on surgeon preference (See Image D). A blunt gelpi’s self-retaining retractor was put to dissect anterior glenohumeral capsule. Some surgeons preferred to put stay sutures in before incising Subscapularis.

Image B: Positioning of the patient in Beach Chair with GA and interscalene block.

Image C: Approach- Deltopectoral with identification of Cephalic vein.
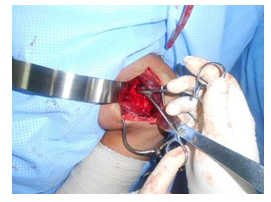
Image D: Splitting the subscapularis.

Image E: Visualization of glenoid and identification of anteroinferior labral avulsion.
A- T’ shaped capsulotomy with a humeral based vertical component was made and held by stay sutures of vicryl no. 2 and anterior glenoid rim was identified. In the absence of a Fukuda retractor at the center, a broad Hohman was improvised to depress the humeral head behind the retractor and expose the anterior glenoid rim. A useful observation was to put a rolled towel underneath the ipsilateral scapula during pre op positioning, which allowed increased excursion of the free draped arm relative to the stable and elevated scapula. The anterior glenoid rim was exposed and confirmed for the Bankart lesion [8], though it was difficult to discern in a few cases owing it to limited overall exposure which is a sincere drawback of this surgery as compared to its televised arthroscopic variant. (See image E).

Image F: Drilling of glenoid rim for suture anchors.

Image G: Repaired anteroinferior capsulolabral tissue.
The anteroinferior capsulolabrum was elevated using arthroscopic elevator and the underlying bone rasped using the arthroscopic rasp. Next, the repair was done using metallic anchors, Titanium (Biotek mini vim 2.8 mm). Three suture anchors were used at 3, 5 and 6 oclock positions (see image F) and the avulsed labrum was repaired to create a ‘bumper effect’using a suture shuttling device, Smith & Nephew 45 degree ACCUPASS. (See Image G). After the repair of labral avulsion, the improvised (Hohman) retractor is taken out and gleno humeral joint is relocated. The closure starts with T shaped inferior capsular flap which is advanced superiorly and laterally and closed with vicryl. Similarly the superior flap is advanced inferiorly and slightly medially to give a ‘pants over vest’ closure. It was imperative to standardize the closure at 30 degrees of abduction and 30 degrees of external rotation [5]. The subscapularis was repaired to its humeral component. In a L-shaped incision, it was repaired and if Subscapularis was split, it was stitched. The subscapularis repair was completed using no. 2 ethibond along with Rotator interval closure. Post operatively, patients were rehabilitated for the operated shoulder as per open bankart protocol. All patients were followed up at intervals of 2 months, 6 months , 1 year and 3 years post op as they had to come to the institute or affiliated hospitals for medical categorization.

Image H: Post op X ray with suture anchors in the anteroinferior edge of glenoid.
3. Rehabilitation Protocol and Post Op
- Shoulder immobilizer for first 7 days post op. Active wrist, finger movements and elbow movement with the shoulder immobilizer.
- External rotation upto 0 degrees and regular use of shoulder immobilizer. Also Pendulum exercises started from day 7 to day 14 post op.
- Suture removal on 14th post op day. Patients were sent home on sick leave with intermittent use of shoulder immobilizer and were advised pendulum exercises with maximum abduction up to 90 degrees. Active and gradual external rotation exercises were initiated. Full internal rotation and gradual abduction was expected at the end of sick leave of 4 wks. Overhead activities were strictly restricted.
- At the end of 4 weeks sick leave, use of shoulder immobilizer was discarded, ROM was assessed and gradual external rotation was expected to be 50% of contralateral. All military personnel were given restrictions of military activities that involved overhead activities including climbing ropes and overhead sports.
- Patient were again reviewed at 6 months when full range of motion and full external rotation was expected. Patients were again given military restrictions of overhead and throwing activities. However, they were encouraged to participate in sports judging their own recovery. Recruits and cadets, if found with good strength and recovery were upgraded and deemed fit to join the armed forces else invalidated out.The medical board was held in various academies at about 180 days following injury and telephonic follow up was taken.
- Patients were reviewed at 1 year post op and the again at 3 years post op for final assessment of ROM and any limitations in ROM were noted. ROWE scoring system was used and patients gave themselves marks on stability, function and motion. All soldiers were put through Low medical recategorization.
- All patients who had good results and volunteered to be upgraded, were relieved of military restrictions and those who were apprehensive or had fair or poor results were put in permanent LOW MEDICAL CATEGORY with restrictions with a regular 2 yearly follow up.
To repeat, all patients were followed up at intervals of 2 months, 6 months and 1 year and 3 years post op as they had to come to the institute or affiliated hospitals for medical categorization. Final functional outcome was evaluated after a period of 2 years from the date of surgery. Assessment at the end of 3 year follow up:
- Functional assessment using Rowe scores (Refer Table 1)– status of shoulder function and recovery to military and athletic levels. Preop and postop Rowe scores were compared and used to grade the recovery. Any feeling of subluxation or recurrent dislocation episodes after surgery were noted.
- Functional recovery – Range of motion was compared especially loss of external rotation (See Image J)
- Mode of Injury- An epidemiological assessment of the pattern of injury leading to the first episode of dislocation in this cohort.

Image J: Postop evaluation: comparing loss of external rotation with contralateral shoulder.
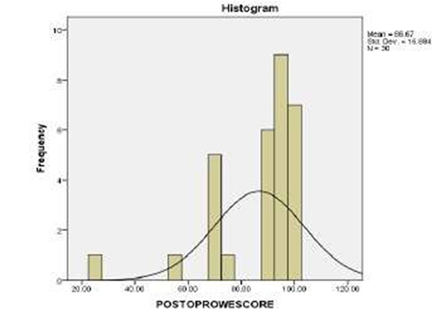
Table 1: Details of the Rowe Score
Rowe Score: 100 / 100
Section 1 – Stability
- No Recurrence, subluxation or apprehension (50)
- Apprehension when placing arm in certain positions (30)
- Subluxation (not requiring reduction) (10)
- Recurrent Dislocation (0)
Section 2 - Motion
- 100% of normal ext. rotation, int. rotation and elevation (20)
- 75% of normal ext. rotation, int. rotation and elevation (15)
- 50% of normal ext. rotation, int. rotation and elevation (5)
- 50% of normal elevation, and int. rotation, No ext rotation (0)
Section 3 - Function
- No limitation of work or sports, little or no discomfort (eg shoulder strong overhead, lifting, swimming, throwing, tennis) (30)
- Mild limitation and minimum discomfort (25)
- Moderate limitation and discomfort (10)
- Marked limitation and pain (0)
Rowe Scoring System: The scoring is done over one hundred points, with 50 points for stability, 30 points for function and 20 points for motion. Results are considered poor between 0 and 50 points, fair between 51 and 75, good between 76 and 90, and excellent between 91 and 100 points.
4. Results
Epidemiological assessment: The mean age of first dislocation was 26.5 yrs in this study group (min 17 and max 45). The commonest cause was bike accident which accounted for 16.7 %. The other common causes were basketball, kabaddi, swimming, 10 metres diving and slipping of one hand while climbing vertical rope, each measuring 10% in frequency (Refer Table2). 70% of the patients (n=21) had recurrent dislocations in their dominant arm and 30 % (n=9) had recurrent dislocation in their non-dominant arm. 46.7% (n=14) of the patients had < 5 dislocations and there were 7 patients (23.3%) who had >30 dislocations.
40% of the patients (n=12) did not dislocate during sleep and 60% (n=18) had dislocations/apprehension during sleep. Dislocation during sleep was a consistent feature in patients who had greater number of dislocations. 30% (n=9) had their latest episode of relocation by a doctor in a medical institute. 16.7% (n=5) had their latest episode of relocation by a paramedic. 53.3 % (n=16) were able to relocate on their own in their latest episode. This subset of patients reported of initial dislocations which required paramedic intervention but later gained the expertise due to ease and experience.
|
Mode of injury |
Frequency |
Percent |
|
10 metres diving |
3 |
10.0 |
|
basketball |
3 |
10.0 |
|
bike accident |
5 |
16.7 |
|
boxing |
1 |
3.3 |
|
cricket |
1 |
3.3 |
|
fall from tank |
1 |
3.3 |
|
horizontal rope |
1 |
3.3 |
|
kabaddi |
3 |
10.0 |
|
rope climbing |
1 |
3.3 |
|
skydiving |
1 |
3.3 |
|
swimming |
3 |
10.0 |
|
vertical rope |
3 |
10.0 |
|
volleyball |
2 |
6.7 |
|
wrestling |
2 |
6.7 |
|
Total |
30 |
100.0 |
Table 2: Mode of injury at first episode of dislocation in this cohort.
4.1 Functional assessment
The mean pre op Rowe score was 40.6, (range 15-80). All patients underwent modified open modified bankart repair at the institute during the stipulated time period.
The mean post op Rowe score was 86.6 (range 25-100) at the end of 3 year for Refer Table3, Histogram of Post op Rowe scores.
- 22 patients had overall excellent results (73.3 %) with a post op Rowe score of greater than 90.
- One patient had good result (3%) with a post op Rowe score in between 75 and 89.
- 6 patients had fair result (20%) with a post op Rowe score between 74 and 51.
- One patient had poor result (3%) with a post op Rowe score of lesser than 50.
Table 3: Post Op Rowe Scores (histogram).
4.2 Functional recovery
At the end of 3 yrs, 40% (n=12) did not have loss of external rotation, 36.7 % (n=11) had 5 degrees loss of external rotation, 20% (n=6) had 10 degrees of loss of external rotation and only 1 patient had greater than 15 degrees of loss of external rotation. The mean loss of external rotation was 4.3 degrees with a range of 0 to 15 degrees.
4.3 Complications
There were 2 failures (6%) with one patient having backing out of suture anchors requiring a revision surgery. The other patient had persistent feeling of apprehension even after surgery, who was a sky diver. He chose ground duties later, however his post op Rowe score was greater than 50, earning him a fair result.
5. Discussion
The study is a useful projection of open Bankart surgery in absence of adequate arthroscopy equipment. In our set up, we are increasingly facing odds of setting up newer orthopaedic centers in military echelons with logistics lagging behind for years. The theoretical advantage of tightening of anterior capsule in addition to repair of avulsed labrum needed to be compared with previous open bankart studies and if possible in military population. There were few limitations in this study. Firstly, the sample size was small. Secondly the arthroscope was not fully functional for shoulder surgeries from 2011 to 2014 at the aforementioned center, eliminating selection bias. Thirdly, there were no controls for this study. Fourthly, due to the participation of 5 different surgeons, subtle variations in surgical technique is bound to creep in. Fifth, there was no investigation done in post op to study the healing of Subscapularis. Sixth, this study has a short followup of only 3 years, which is why redislocation rates cannot be properly assessed.
Rowe [9] et al has studied 145 patients with 3.5 % redislocation rate in a thirty year period (1946 to 1976). They have reported 74% excellent, 23% good and 3% poor results. Altchek [3] et al have described a medial based T- plasty modification with an average followup of 3 yrs (range 2 to 7 yrs). They reported 4 patients with instability after operation. Altchek [3] reported an average loss of external rotation of 5 degrees with arm by the side. Also satisfaction was rated at excellent for 95 % of the cases, which is comparable to our series. Coming to epidemiology, we researched for similar papers on anterior instability in military population. Brian Waterman [10] et al has reported a 10 fold greater incidence of anterior shoulder dislocation as compared to civilian population. In the US military, higher incidence is seen in men, age>30years, junior enlisted rank and Army branch of service [11]. The US military academy has higher rates of anterior shoulder instability in the military cohort with rigors of military activity [10]. Shoulder dislocations occurred in 4.35 cadets per 1000 person-years.
If subluxation is added, the instability events were nearly 3% per year and comprised of 85 percent of all instability events [12]. In a trial of 61 military patients, open and arthroscopic stabilization had comparable clinical outcomes, although open procedures had reported longer operative duration and greater losses in motion [13]. Yamamoto, Itoi [7] and colleagues in 2007, introduced the concept of glenoid track which can be measured using 3D CT scans and linear measurement. It can be compared to the contralateral unaffected shoulder to look for glenoid bone loss. Calculation of glenoid track is relevant in posterior end range of movements of abduction, external rotation when posterior humeral articular surface is in contact with glenoid.
The glenoid track is 83% of the linear width of glenoid (83%D). If there is glenoid bone loss, then the width(d) is subtracted from 83% value to get the true width of glenoid track using en face view of 3D CT glenoid (.83D-d). This measurement (.83D-d) is superimposed on 3D CT of posterior humeral head depicting the Hill Sach’s lesion. If size and location of Hill Sach’s lesion is within the glenoid track, it is called ‘On Track’ and is suitable for open or arthroscopic bankart, provided glenoid bone loss is less than 25% to the contralateral side. The relevance of this surgery lies in switching to open Latarjet for all bipolar bone loss cases with off track [6] Hill Sach’s lesion and >25% glenoid bone loss. Since the surgical approach and exposure of anteroinferior glenoid remains the same.
6. Conclusions
Military surgeons have made significant contributions in understanding of traumatic anterior shoulder instability [14] .This study gives an Indian military experience to the continuing research with excellent results with modified open bankart.
Funding
This research was not funded by any agency and authors have no conflict of interest to declare.
References
- Bottoni CR, Wilckens JH, DeBerardino TM, et al. A prospective, randomized evaluation of arthroscopic stabilization versus nonoperative treatment in patients with acute, traumatic, first-time shoulder dislocations. Am J Sports Med 30 (2002): 576-
- Wheeler JH, Ryan JB, Arciero RA, et al. Arthroscopic versus non operative treatment of acute shoulder dislocations in young athletes. Arthroscopy 5 (1989): 213-217.
- Altchek DW, Warren RF, Skyhar MJ, et al. T-plasty modification of the Bankart procedure for multidirectional instability of the anterior and inferior types. J Bone Joint Surg Am 73 (1991): 105-112.
- Neer CS 2nd, Foster CR. Inferior capsular shift for involuntary inferior and multidirectional instability of the shoulder: a preliminary report. J Bone Joint Surg Am 62 (1980): 897-908.
- Boileau P, Fourati E, Bicknell R. Neer Modification of Open Bankart Procedure: What are the Rates of Recurrent Instability, Functional Outcome, and Arthritis? Clin Orthop and Relat Res 470 (2012): 2554-2560.
- Di Giacomo G, Itoi E, Burkhart SS. Evolving concept of bipolar bone loss and the HillSach’s lesion: from engaging /non engaging, lesion to on-track/off-track lesion. Arthroscopy 30 (2014): 90-98.
- Itoi E, EFORT Open Rev 2 (2017): 343-351.
- Bankart AS. The pathology and treatment of the recurrent dislocation of the shoulder joint. Br J Surg 26 (1938): 23-39.
- Rowe C, Patel D, Southmayd W. The Bankart procedure: A long-term end result study. J Bone Joint Surg Am 60 (1978): 1-16.
- Waterman B, Owens BD, Tokish JM. Anterior Shoulder Instability in the Military Athlete. Orthopaedic Surgery (2016).
- Owens BD, Dawson L, Burks R, et al. Incidence of shoulder dislocation in the United States military: demographic considerations from a high -risk population. J Bone Joint Surg Am 91 (2009): 791-796.
- Owens BD, Duffey ML, Nelson BJ, et al. The incidence and characteristics of shoulder instability at the United States Military Academy. Am J Sports Med 35 (2007): 1168-1173.
- Bottoni CR, Smith EL, Berkowitz MJ, et al. Arthroscopic versus open shoulder stabilization for recurrent anterior instability: a prospective randomized clinical trial. Am J Sports Med 34 (2006): 1730-1737.
- Provencher MT, Mannava S, Tokish JM, et al. Traumatic anterior shoulder instability: the US military experience. Am J Orthop 46 (2017): 184-189.
