Dieulafoy’s Lesion of Ileum; Report of A Rare Case
Article Information
Dimitrios Paikos1*#, John Moschos2#, Georgios Sofianidis1, Christos Zavos1, Georgios Tikos1, Konstantinos Theodoridis4, Aikaterini Dimakopoulou4, Antonios Mpakas4, Dimitrios Raptis3##, Basilios Papaziogas3##
#Aurhors equally contributed as first authors
##Aurhors equally contributed as last authors
1Department of Gastrenterology, “G. Gennimatas” Hospital, 41. Eth. Aminis Str., 54635, Thessaloniki, Greece
2 International University of Hellas, Thessaloniki, Greece
32nd Surgical Department, Aristotle University of Thessaloniki, “G. Gennimatas” Hospital, 41. Eth. Aminis Str., 54635, Thessaloniki, Greece
4Department of Internal Medicine, “G. Gennimatas” Hospital, 41. Eth. Aminis Str., 54635, Thessaloniki, Greece
*Corresponding Author: Dimitrios Raptis, 2nd Surgical Department, Aristotle University of Thessaloniki, “G. Gennimatas” Hospital, 41. Eth. Aminis Str., 54635, Thessaloniki, Greece
Received: 16 October 2020; Accepted: 02 November 2020; Published: 01 December 2020
Citation: Dimitrios Paikos, John Moschos, Georgios Sofianidis, Christos Zavos, Georgios Tikos, Konstantinos Theodoridis, Aikaterini Dimakopoulou, Antonios Mpakas, Dimitrios Raptis, Basilios Papaziogas. Dieulafoy’s Lesion of Ileum; Report of A Rare Case. Archives of Clinical and Medical Case Reports 4 (2020): 1140-1145.
View / Download Pdf Share at FacebookAbstract
Dieulafoy’s lesions (DLs) are dilated aberrant submucosal vessels, otherwise histologically normal, that erode the overlying epithelium in the absence of a primary ulcer, thereby causing a massive gastrointestinal (GI) bleeding. DLs are usually located in the proximal stomach along the lesser curvature, near the esophagogastric junction (typically within 5-6 cm). However, other locations throughout the GI tract have also been reported, such the esophagus, duodenum and colon. DL located in the ileum is extremely rare.
Thus, we report a rare case of DL located 10 cm from the ileocecal valve, which treated endoscopically with hemoclips. On the fifth day post-endoscopic intervention, there were no signs of recurrent bleeding and the patient was discharged from our hospital.
Most of the ileal DL cases reported in the literature were treated surgically. However, we believe that endoscopic treatment with thermal, mechanical (hemoclip or band ligation), or combination therapy (adrenaline injection combined with thermal or mechanical therapy) should be considered as the first-line management of bleeding DLs. Surgical resection should be reserved for: a. selected cases that cannot be treated with endoscopic or angiographic methods.
Keywords
Dieulafoy; Gastrointestinal bleeding; Ileum; Hematochezia
Dieulafoy articles; Gastrointestinal bleeding articles; Ileum articles; Hematochezia articles
Dieulafoy articles Dieulafoy Research articles Dieulafoy review articles Dieulafoy PubMed articles Dieulafoy PubMed Central articles Dieulafoy 2023 articles Dieulafoy 2024 articles Dieulafoy Scopus articles Dieulafoy impact factor journals Dieulafoy Scopus journals Dieulafoy PubMed journals Dieulafoy medical journals Dieulafoy free journals Dieulafoy best journals Dieulafoy top journals Dieulafoy free medical journals Dieulafoy famous journals Dieulafoy Google Scholar indexed journals Gastrointestinal bleeding articles Gastrointestinal bleeding Research articles Gastrointestinal bleeding review articles Gastrointestinal bleeding PubMed articles Gastrointestinal bleeding PubMed Central articles Gastrointestinal bleeding 2023 articles Gastrointestinal bleeding 2024 articles Gastrointestinal bleeding Scopus articles Gastrointestinal bleeding impact factor journals Gastrointestinal bleeding Scopus journals Gastrointestinal bleeding PubMed journals Gastrointestinal bleeding medical journals Gastrointestinal bleeding free journals Gastrointestinal bleeding best journals Gastrointestinal bleeding top journals Gastrointestinal bleeding free medical journals Gastrointestinal bleeding famous journals Gastrointestinal bleeding Google Scholar indexed journals Ileum articles Ileum Research articles Ileum review articles Ileum PubMed articles Ileum PubMed Central articles Ileum 2023 articles Ileum 2024 articles Ileum Scopus articles Ileum impact factor journals Ileum Scopus journals Ileum PubMed journals Ileum medical journals Ileum free journals Ileum best journals Ileum top journals Ileum free medical journals Ileum famous journals Ileum Google Scholar indexed journals Hematochezia articles Hematochezia Research articles Hematochezia review articles Hematochezia PubMed articles Hematochezia PubMed Central articles Hematochezia 2023 articles Hematochezia 2024 articles Hematochezia Scopus articles Hematochezia impact factor journals Hematochezia Scopus journals Hematochezia PubMed journals Hematochezia medical journals Hematochezia free journals Hematochezia best journals Hematochezia top journals Hematochezia free medical journals Hematochezia famous journals Hematochezia Google Scholar indexed journals DLs articles DLs Research articles DLs review articles DLs PubMed articles DLs PubMed Central articles DLs 2023 articles DLs 2024 articles DLs Scopus articles DLs impact factor journals DLs Scopus journals DLs PubMed journals DLs medical journals DLs free journals DLs best journals DLs top journals DLs free medical journals DLs famous journals DLs Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Cardioverter articles Cardioverter Research articles Cardioverter review articles Cardioverter PubMed articles Cardioverter PubMed Central articles Cardioverter 2023 articles Cardioverter 2024 articles Cardioverter Scopus articles Cardioverter impact factor journals Cardioverter Scopus journals Cardioverter PubMed journals Cardioverter medical journals Cardioverter free journals Cardioverter best journals Cardioverter top journals Cardioverter free medical journals Cardioverter famous journals Cardioverter Google Scholar indexed journals enterectomy articles enterectomy Research articles enterectomy review articles enterectomy PubMed articles enterectomy PubMed Central articles enterectomy 2023 articles enterectomy 2024 articles enterectomy Scopus articles enterectomy impact factor journals enterectomy Scopus journals enterectomy PubMed journals enterectomy medical journals enterectomy free journals enterectomy best journals enterectomy top journals enterectomy free medical journals enterectomy famous journals enterectomy Google Scholar indexed journals
Article Details
1. Introduction
Dieulafoy’s lesions (DLs) are dilated aberrant submucosal vessels, otherwise histologically normal, that erode the overlying epithelium in the absence of a primary ulcer, thereby causing a massive gastrointestinal (GI) bleeding [1]. Despite being initially described by Dr. M.T. Gallard in 1884 as gastric aneurysm, the nomenclature for this lesion is attributed to Georges Dieulafoy in 1898, who considered it to be the initial stage of a common gastric ulcer [2]. We herein describe the rare case of an elderly patient with severe hematochezia, dizziness, and instability of vitals due to a DL located in the ileum.
2. Case Report
An 85-year-old man was transferred to the Accident and Emergency Unit of our hospital after he collapsed due to several episodes of voluminous fresh hematochezia. On admission, the patient felt dizzy, his blood pressure was 90/56 mmHg, and his pulse rate was 108 beats/min. On general physical examination, he looked pale and dehydrated. Blood hemoglobin level was 6.5 g/dL. He had a history of heart failure, mitral regurgitation, hypertension, paroxysmal atrial flutter, and was receiving treatment with acenocoumarol. The patient did not report any use of aspirin or nonsteroidal anti-inflammatory drugs (NSAIDs) in the previous 7 days. Family history was negative for any GI disease.
Initially the patient was treated with a transfusion of 3 units of packed red blood cells, and thereafter he underwent an urgent esophagogastroduodenoscopy (EGD), which was unrevealing for a bleeding site. After he became hemodynamically stable, a colonoscopy was performed, which revealed fresh blood throughout the entire colon and terminal ileum. A DL on the distal ileum, approximately 10 cm from the ileocecal valve, was found (Figure 1 and 2), and immediate hemostasis was successful using hemoclips (Figure 3). On the fifth day post-endoscopic intervention, there were no signs of recurrent bleeding and the patient was discharged from our hospital.
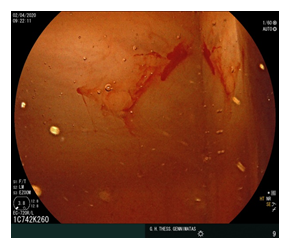
Figure 1: A DL on the distal ileum.
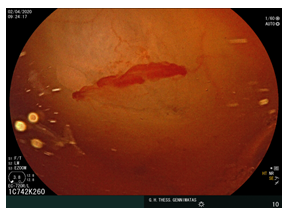
Figure 2: A DL on the distal ileum, approximately 10 cm from the ileocecal valve.
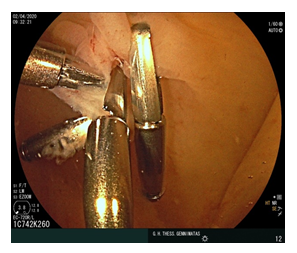
Figure 3: Immediate hemostasis using hemoclips.
3. Discussion
DLs can affect any age group but present more commonly in the elderly, as in our patient presented herein, with an average age ranging from the fifth to the seventh decade of life. The etiology is not entirely known, but it seems that the submucosal artery does not undergo normal branching within the wall of the GI tract. As a result, the caliber of the artery is in the range of 1-3 mm, approximately 10-fold that of the normal caliber of mucosal capillaries. No causal link has been established between the formation of DLs and (a). the use of NSAIDs, alcohol and tobacco; (b). the presence of peptic ulcer disease; or (c). Helicobacter pylori infection [3]. However, patients who bleed from DLs are mostly men with comorbidities including cardiovascular disease, hypertension (as in our patient), chronic kidney disease, diabetes mellitus, and/or chronic alcohol abuse [4].
DLs are usually (70%) located in the proximal stomach along the lesser curvature, near the esophagogastric junction (typically within 5-6 cm). However, other locations throughout the GI tract have also been reported, such the esophagus, duodenum, and colon, uncommonly causing GI symptoms, especially abdominal pain, usually indicating an alternative diagnosis such as peptic ulcer disease or complications from bleeding such as mesenteric ischemia secondary to hemorrhagic shock [5]. A high proportion of DLs are found at intestinal anastomoses, predominantly Billroth II, after gastrectomy [6].
Our patient was diagnosed endoscopically with a bleeding DL located in the ileum, an extremely rare site, with only 6 cases reported in the literature thus far [7-10]. Endoscopic detection is the diagnostic modality of choice, although endoscopic identification of the bleeding source may be extremely difficult, as bleeding is typically intermittent and surrounding mucosa is typically normal or demonstrates only a tiny ulcer. Computed tomographic angiography may be a diagnostic strategy in the setting of acute bleeding, which may facilitate interventional radiology and arterial embolization [11]. In the absence of active bleeding, common endoscopic findings include a small, usually less than 3 mm, protruding pulsatile lesion surrounded by normal mucosa, with or without active bleeding [12]. Endoscopic criteria for the diagnosis of a DL are: a. active arterial spurting or micropulsatile streaming from a minute (less than 3 mm) mucosal defect or through normal-surrounding mucosa; b. visualization of a protruding vessel with or without active bleeding within a minute mucosal defect or through normal-surrounding mucosa; or c. a fresh, densely adherent clot with a narrow point of attachment to a minute mucosal defect or to normal-appearing mucosa [13]. Although in our patient the endoscopic features could not be proven to be a true DL by histology, the endoscopic finding remains convincing for DL [14]. Histologic evaluation is usually unavailable in most cases, because recently, most vascular lesions have been treated by nonsurgical modalities. Finally, endoscopic ultrasonography may be useful in confirming the diagnosis if the DL is not actively bleeding.
Most of the ileal DL cases reported in the literature were treated surgically [15]. However, we believe that endoscopic treatment with thermal, mechanical (hemoclip or band ligation), or combination therapy (adrenaline injection combined with thermal or mechanical therapy) should be considered as the first-line management of bleeding DLs, replacing surgery in a significant number of small bowel DL cases. These endoscopic hemostatic techniques are safe and have similar outcomes in observational studies. Transcatheter angiographic embolization should be the next option in cases that cannot be treated endoscopically [16]. Surgical resection should be reserved for: a. selected cases that cannot be treated with endoscopic or angiographic methods; and b. rebleeding or difficult-to-control with nonsurgical treatment bleeding DLs, as a last resort [9, 17].
Doppler ultrasound has been used to confirm ablation of a DL by documenting the absence of blood flow following treatment [18]. However, this approach should be based upon local experience and expertise. With proper diagnosis and treatment, the rate of mortality has decreased from 30% in the 1970s to currently 8%. Clinicians should bear in mind that the difficulty lies in the early and accurate detection, especially in rare locations, as was the case in our patient.
References
- Juler GL, Labitzke HG, Lamb R, et al. The pathogenesis of Dieulafoy's gastric erosion. Am J Gastroenterol 79 (1984): 195-200.
- Baxter M, Aly EH. Dieulafoy’s lesion: current trends in diagnosis and management. Ann R Coll Surg Engl 92 (2010): 548-554.
- Gastrointestinal bleeding from Dieulafoy’s lesion: clinical presentation, endoscopic findings, and endoscopic therapy. Nojkov B, Cappell MS. World J Gastrointest Endosc 7 (2015): 295-307.
- Lara LF, Sreenarasimhaiah J, Tang SJ, et al. Dieulafoy lesions of the GI tract: localization and therapeutic outcomes. Dig Dis Sci 55 (2010): 3436-3441.
- Baettig B, Haecki W, Lammer F, et al. Dieulafoy's disease: endoscopic treatment and follow up. Gut 34 (1993): 1418-1421.
- The evolution of Dieulafoy's lesion since 1897: then and now—a journey through the lens of a pediatric lesion with literature review. Senger JL, Kanthan R. Gastroenterol Res Pract (2012): 432-517.
- Choi YC, Park SH, Bang BW, et al. Two cases of ileal dieulafoy lesion with massive hematochezia treated by single balloon enteroscopy. Clin Endosc 45 (2012): 440-443.
- Gastric Dieulafoy lesion: a rare cause of massive haematemesis in an elderly woman Jamie Clements et. al. BMJ Case Rep (2018): bcr2017223615.
- Lee YT, Walmsley RS, Leong RW, et al. Dieulafoy's lesion. Gastrointest Endosc 58 (2003): 236-243.
- Dy NM, Gostout CJ, Balm RK. Bleeding from the endoscopically-identified Dieulafoy lesion of the proximal small intestine and colon. Am J Gastroenterol 90 (1995): 108-111.
- Young Chul Choi, Sang Hyun Park, Byoung Wook Bang, et al. Two Cases of Ileal Dieulafoy Lesion with Massive Hematochezia Treated by Single Balloon Enteroscopy. Clin Endosc 45 (2012): 440-443.
- Marangoni G, Cresswell AB, Faraj W, et al. An uncommon cause of life-threatening gastrointestinal bleeding: 2 synchronous Dieulafoy lesions. J Pediatr Surg 44 (2009): 441-443.
- Alshumrani G, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagn Interv Radiol 12 (2006): 151-154.
- Endoscopic management of massive rectal bleeding from a Dieulafoy's lesion: Case report. Pineda-De Paz MR et.al. World J Gastrointest Endosc 11 (2019): 438-442.
- Jaspersen D. Dieulafoy's disease controlled by Doppler ultrasound endoscopic treatment. Gut 34 (1993): 857-858.
- Alshumrani G, Almuaikeel M. Angiographic findings and endovascular embolization in Dieulafoy disease: a case report and literature review. Diagn Interv Radiol 12 (2006): 151-154.
- Endoscopic management of massive rectal bleeding from a Dieulafoy's lesion: Case report. Pineda-De Paz MR et.al. World J Gastrointest Endosc 11 (2019): 438-442.
- Jaspersen D. Dieulafoy's disease controlled by Doppler ultrasound endoscopic treatment. Gut 34 (1993): 857-858.
