Best Palliation for Malignant Bowel Obstruction- A Retrospective study
Article Information
Laxmidhara Padhy*1, Saroj Kumar Barma2, Pranay Kumar Patro3
1Department of General Surgery, Govt. Medical College & Hospital, Sundargarh, Odisha, India
2Department of Paediatrics, Govt. Medical College & Hospital, Sundargarh, Odisha, India
3Department of General Medicine, Govt. Medical College & Hospital, Sundargarh, Odisha, India
*Corresponding Author: Laxmidhara Padhy, Department of General Surgery, Govt. Medical College & Hospital, Sundargarh, Odisha, India
Received: 01 March 2023; Accepted: 09 March 2023; Published: 18 April 2023
Citation: Laxmidhara Padhy, Saroj Kumar Barma, Pranay Kumar Patro. Best Palliation for Malignant Bowel Obstruction, A Retrospective study. Journal of Surgery and Research. 6 (2023): 143-149.
View / Download Pdf Share at FacebookAbstract
Objective: To determine the best palliative procedures undergone surgery and non-surgical procedures such as Chemotherapy/Stenting.
Background: Malignancy of Gastrointestinal tract starting from Oesophgus to Anus may cause acute or sub-acute obstruction which requires emergency relief from the symptoms. Surgery with diversion, colostomy or ileostomy, Nutritional Management with feeding gastrostomy/ jejunostomy and further chemoradiotherapy were required according to the different pathological variants at different site of G.I. tract to reduce the mortality rate and prolonging the survival time. Previous studies have been compared for the outcome of success rate,hospital stay,mean long term survival for different palliative interventions. None of them had proved to be most efficient for prolonged survival as most of cases were in the advanced stage of cancer.
Method: A retrospective study of Seventy patients of malignant bowel obstruction was done with statistical analysis.
Observation: Among the Seventy patients 49 were male and 21 were female and mean age of the patient was 49.57. The overall symptoms improve rate was 75.71%. Among them symptom improve rate 96% in surgical group,42.80% in stenting group and 15.38% are in chemotherapy group. Median survival time was 270 days in surgery group.
Conclusion: Malignant obstruction is an emergency condition in most of times needs urgent symptom relief by any mean of palliation. Complete and unresectable malignant obstruction needs diversion colostomy or any by-pass surgeries. Among all type of surgeries resection and anastomosis with or without diversion of loop is best palliation.
Keywords
MBO: Malignant Bowel Obstruction; GJ: Gastrojejunostomy; TPN: Total Parental Nutrition; Chemo-radio (Chemoradiotherapy).
MBO articles: Malignant Bowel Obstruction articles; GJ articles: Gastrojejunostomy articles; TPN articles: Total Parental Nutrition articles; Chemo-radio articles(Chemoradiotherapy) articles.
Malignant Bowel Obstruction articles Malignant Bowel Obstruction Research articles Malignant Bowel Obstruction review articles Malignant Bowel Obstruction PubMed articles Malignant Bowel Obstruction PubMed Central articles Malignant Bowel Obstruction 2023 articles Malignant Bowel Obstruction 2024 articles Malignant Bowel Obstruction Scopus articles Malignant Bowel Obstruction impact factor journals Malignant Bowel Obstruction Scopus journals Malignant Bowel Obstruction PubMed journals Malignant Bowel Obstruction medical journals Malignant Bowel Obstruction free journals Malignant Bowel Obstruction best journals Malignant Bowel Obstruction top journals Malignant Bowel Obstruction free medical journals Malignant Bowel Obstruction famous journals Malignant Bowel Obstruction Google Scholar indexed journals Gastrojejunostomy articles Gastrojejunostomy Research articles Gastrojejunostomy review articles Gastrojejunostomy PubMed articles Gastrojejunostomy PubMed Central articles Gastrojejunostomy 2023 articles Gastrojejunostomy 2024 articles Gastrojejunostomy Scopus articles Gastrojejunostomy impact factor journals Gastrojejunostomy Scopus journals Gastrojejunostomy PubMed journals Gastrojejunostomy medical journals Gastrojejunostomy free journals Gastrojejunostomy best journals Gastrojejunostomy top journals Gastrojejunostomy free medical journals Gastrojejunostomy famous journals Gastrojejunostomy Google Scholar indexed journals Total Parental Nutrition articles Total Parental Nutrition Research articles Total Parental Nutrition review articles Total Parental Nutrition PubMed articles Total Parental Nutrition PubMed Central articles Total Parental Nutrition 2023 articles Total Parental Nutrition 2024 articles Total Parental Nutrition Scopus articles Total Parental Nutrition impact factor journals Total Parental Nutrition Scopus journals Total Parental Nutrition PubMed journals Total Parental Nutrition medical journals Total Parental Nutrition free journals Total Parental Nutrition best journals Total Parental Nutrition top journals Total Parental Nutrition free medical journals Total Parental Nutrition famous journals Total Parental Nutrition Google Scholar indexed journals Chemoradiotherapy articles Chemoradiotherapy Research articles Chemoradiotherapy review articles Chemoradiotherapy PubMed articles Chemoradiotherapy PubMed Central articles Chemoradiotherapy 2023 articles Chemoradiotherapy 2024 articles Chemoradiotherapy Scopus articles Chemoradiotherapy impact factor journals Chemoradiotherapy Scopus journals Chemoradiotherapy PubMed journals Chemoradiotherapy medical journals Chemoradiotherapy free journals Chemoradiotherapy best journals Chemoradiotherapy top journals Chemoradiotherapy free medical journals Chemoradiotherapy famous journals Chemoradiotherapy Google Scholar indexed journals colostomy articles colostomy Research articles colostomy review articles colostomy PubMed articles colostomy PubMed Central articles colostomy 2023 articles colostomy 2024 articles colostomy Scopus articles colostomy impact factor journals colostomy Scopus journals colostomy PubMed journals colostomy medical journals colostomy free journals colostomy best journals colostomy top journals colostomy free medical journals colostomy famous journals colostomy Google Scholar indexed journals by-pass surgeries articles by-pass surgeries Research articles by-pass surgeries review articles by-pass surgeries PubMed articles by-pass surgeries PubMed Central articles by-pass surgeries 2023 articles by-pass surgeries 2024 articles by-pass surgeries Scopus articles by-pass surgeries impact factor journals by-pass surgeries Scopus journals by-pass surgeries PubMed journals by-pass surgeries medical journals by-pass surgeries free journals by-pass surgeries best journals by-pass surgeries top journals by-pass surgeries free medical journals by-pass surgeries famous journals by-pass surgeries Google Scholar indexed journals carcinomamatosis articles carcinomamatosis Research articles carcinomamatosis review articles carcinomamatosis PubMed articles carcinomamatosis PubMed Central articles carcinomamatosis 2023 articles carcinomamatosis 2024 articles carcinomamatosis Scopus articles carcinomamatosis impact factor journals carcinomamatosis Scopus journals carcinomamatosis PubMed journals carcinomamatosis medical journals carcinomamatosis free journals carcinomamatosis best journals carcinomamatosis top journals carcinomamatosis free medical journals carcinomamatosis famous journals carcinomamatosis Google Scholar indexed journals hospital stay articles hospital stay Research articles hospital stay review articles hospital stay PubMed articles hospital stay PubMed Central articles hospital stay 2023 articles hospital stay 2024 articles hospital stay Scopus articles hospital stay impact factor journals hospital stay Scopus journals hospital stay PubMed journals hospital stay medical journals hospital stay free journals hospital stay best journals hospital stay top journals hospital stay free medical journals hospital stay famous journals hospital stay Google Scholar indexed journals Geriatric patients articles Geriatric patients Research articles Geriatric patients review articles Geriatric patients PubMed articles Geriatric patients PubMed Central articles Geriatric patients 2023 articles Geriatric patients 2024 articles Geriatric patients Scopus articles Geriatric patients impact factor journals Geriatric patients Scopus journals Geriatric patients PubMed journals Geriatric patients medical journals Geriatric patients free journals Geriatric patients best journals Geriatric patients top journals Geriatric patients free medical journals Geriatric patients famous journals Geriatric patients Google Scholar indexed journals
Article Details
Introduction
Malignant bowel obstruction is acute or sub-acute presentation of intestinal obstruction in the emergency OPD with features of distention, vomiting, pain abdomen and nutritional disorders due to malignant involvement of bowel. The various methods including their efficacy and safety, indication and appropriate timing of intervention are required for relive of symptoms to improve the quality of life [1]. Neoadjuvant chemotherapy, immediate surgery can improve the symptoms but don’t have overall survival among patients with epidermoid cancer or adenocarcinoma of oesophagus [2]. Metastasis to distant organs including carcinomamatosis peritonei may be presented with intestinal obstruction. The treatment is considered purely palliative. However, for sub-group of patients multimodal treatment can be provided with curative intent. Cytoprotective surgery systemic chemotherapy can improve the symptoms and survival time [3]. The decision on a surgical versus on endoscopic stentinig procedure for palliation depends on the tumour stage and degree of obstruction [4]. The goal of different methods of interventions concern life expectancy, nutritional status and intestinal function. Enteral feeding with feeding gastrostomy or jejonostomy should be considered as fast choice, if definite surgery or endoscopic stenting are not feasible [5]. Colonic stening was first performed in the countees of Chester Hospital 2001. Combined endoscopy and radiological approach of stenting for large bowel malignant obstruction help for, palliation and as a ‘Bridge to Surgery’. Thus reduces morbidity and mortality, avoidance of stomach and shorter hospital stay [6].
Periampullary cancer often present with duodenal obstruction, obstructive jaundice. Both surgical and non-surgical palliative procedure relief obstruction. Stenting and by-pass surgical treatment are required for longer life expectancy [7]. Surgery is associated with a better overall survival compared to other basic supportive care treatment for patient of malignant bowel obstruction with peritoneal metastasis [8]. One stage primary resection and anastomosis is the preferred choice for law risk patients. Colostomy has a role for colonic obstruction of patients with very ill patients. Colonic stenting is the best option either for palliation or as a bridge to surgery as it reduces morbidity and mortality rate and also reduces colostomy formation [9]. Self Expendable Metal Stents (SEMS) may be used for both palliative measure and as a pre-operative bridge to facilitate a one stage surgical resection of primary colonic tumours. SEMS can be placed endoscopically or radiologically. The indications, methods of insertion and outcomes following the procedure are most important for comparative study [10]. Geriatric patients, patients with anaemia, hypoproteinemia, ascites, jaundice, any cardio respiratory morbidity and distant metastasis, influence the outcomes in three areas like oncological prognosis, morbidity and mortality risk and long term function loss. Occurrence of complication is the strongest predictor of multiorgan failure and death. Post operative care plays a major role to optimize outcomes. The third of coloreatal cancers are diagnosed in an emergency setting, mostly among geriatre patients [11].
Patients with duodenal obstruction due to tumour growth duodenal stenting is best pallation considered for better survival time [12]. In patients with locally advanced gastric cancer with symptomatic can be managed with radiotherapy extends survival time [13]. Gynecological malignancies like Overy / uterus also invade adjacent intestine causing malignant bowel obstruction. Inappropriate management may result in uncontrolled (Faeculant) vomiting, pain at distress management of the symptoms can include palliative surgery, nasogestric suction therapy together with IV fluids and pharmacological means such as Corticosteroids [14]. Management of these patients is difficult due to patients deteriorating mobility and performance status. The lack of further chemotherapeutic options and higher mortality and morbidity associated with palliative surgery. In order to compare the outcomes of time to recurrence, time of hospital stay, time of survival and time of reintervention, study of complication of surgery, chemoradiotherapy and stenting there needs to be greater degree standardized management [15]. Stent placement for palliation are beneficial as a bridge to surgery, but the selection of patients are most essential for colorectal malignancy [16]. Several options are available to palliate malignant bowel obstruction but none of them have established consensus among surgery [17]. Self expending metal stents are for palliation of malignant billiary and duodenal obstruction may provide a safe and less invasive attentative to surgical palliation with acceptable clinical outcomes [18]. Malignant bowel obstruction is complication of different gynocological malignancy particularly ovarian cancer. Only small subset of patients with MBO appears to benefit from surgical intervention with controversy to use of chemotherapy and TPN [19].
Aim
To determine the best palliative procedure undergone surgery and non-surgical procedure such as Chemotherapy / stenting from 2017 to 2022 at M.K.C.G. MCH, Brahmapur.
Methods
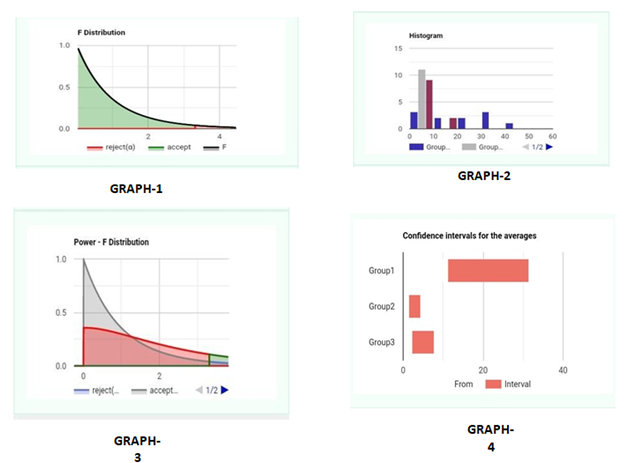
A retrospective study of patients admitted to the M.K.C.G. Hospital for intestinal obstruction and diagnosed as a cause of malignancy preoperatively and postoperatively. It may be partial or complete obstruction of any part of G.I. track. The patients conditions clinical characteristics and their follow ups with diagnostic evaluation and interventions were recorded from the registry of the Department and O.T. records from the period May 2017 to May 2022. No ethical committee clearance was required as it was a retrospective study. Patient were selected from the age group 16 to 85 admitted for intestinal obstruction who were required immediate surgery or other interventional modalities. Intestinal obstruction due to any other benign conditions like Foreign Body, adhesions, bands and herniations were excluded from this study. Any growth causing obstruction and proved to be malignancy perioperative or postoperative with histopathological evidence were included in this study (Figure 1,2,3). The clinical and different diagnosis were made by diagnostic procedures such as X-ray, Ultrasonography, CECT and MRI were done for diagnosis of intestinal obstruction as needed. Accordingly the palliative interventions surgically such as diversion of bowel, feeding gastrostomy / jejunostomy, Gastrojejunostomy, Diversion colostomy or Ileostomy were done for the relief of symptoms or signs in case of acute intestinal obstruction. Those were relieved conservatively and diagnosed to be in sub-acute condition were thoroughly investigated by different investigating procedure such as CECT, MRI and Serum markers for malignancy such as CEA, CA-19.9 and CA-125. Those patients required chemotherapy or elective surgery after staging of the malignancy. The patients were categorized in to 3 groups : (1) Surgical Palliation (2) Stenting (3) Chemotherapy First. The significance of different factors and outcomes of long survival were compared to conclude the one of the procedures undergone for malignant intestinal obstruction and that procedure was considered the best palliation.
Statistical analysis
The different groups of interventions for the patients were compared with their clinical characteristics by one way Anova and posthoc analysis for the significant groups and outcomes. The associated factors influence the outcome of survival were detected by multivariable analysis. Time and events were noted from hospital admission of the patients, hospital stay, recurrence, interventions and death were recorded for the survival analysis. Cox regression analysis and hazard ratios along with Kaplan Meir survival analysis were done by the help of SPSS - 22.
Result
A total of 70 patients proved with G.I. malignancy causing intestinal obstruction were enrolled in this study. Among the 70 patients 49 were male and 21 were female. Patient’s age ranged from 16 years to 85 years with mean age of 49.57 and median age of 53 years. Median survival time was 270 days in surgery group. The clinical and pathological data of all patients in this study were as follows in the table 1.
|
Clinical Characteristics |
Surgery (x1) (no. 50) = 71.4% |
Stenting (x2) (no.7) = 10% |
Chemoradio (x3) therapy (no. 13)= 18.5% |
|
< 75 years |
48 |
4 |
13 |
|
> 75 years |
2 |
3 |
0 |
|
Male |
38 |
5 |
6 |
|
Female |
12 |
2 |
7 |
|
BMI > 35 |
4 |
3 |
3 |
|
BMI < 35 |
46 |
4 |
10 |
|
Acute intestinal obstruction |
30 |
0 |
0 |
|
Sub-acute intestinal obstruction |
20 |
7 |
13 |
|
Blood transfusion |
38 |
2 |
2 |
|
TPN |
22 |
4 |
6 |
|
Patient with sepsis |
2 |
1 |
1 |
|
History of previous surgery |
4 |
2 |
11 |
|
H/o Previous Chemoradio therapy |
6 |
0 |
5 |
|
Other comorbidity |
16 |
5 |
1 |
|
Long Hospital Stay |
13 |
4 |
11 |
|
G.I. Bleeding |
4 |
1 |
0 |
|
Recurrence |
17 |
6 |
6 |
|
Median survival time |
270 days |
180 days |
190 day |
|
Complications |
14 |
2 |
5 |
|
Hospital Death |
6 |
0 |
1 |
Table 1: Different clinicopathological characteristics and treatment modalities
The means of the following pairs are significantly different: (x1) Surgery Vs. Stenting(x2), Surgery(x1) Vs. Chemotherapy(x3) age analyzed by ANOVA and posthoc analysis as on table 2.
|
Pair |
Difference |
SE |
Q |
Lower CI |
Upper CI |
Critical Mean |
p-value |
|
x1-x2 |
18.4545 |
2.7479 |
6.7159 |
8.8742 |
28.0349 |
9.5803 |
0.0001367 |
|
x1-x3 |
16.2727 |
2.7479 |
5.9219 |
6.6924 |
25.8531 |
9.5803 |
0.0006488 |
|
x2-x3 |
2.1818 |
2.7479 |
0.794 |
-7.3985 |
11.7622 |
9.5803 |
0.8414 |
Table 2: ANOVA and posthoc analysis
Evaluation of effectiveness of different palliative procedure for survival analysis were done. The overall symptom improvement rate was 75.71%. The overall symptom improvement rate in the surgical category was significantly higher than the stenting and chemotherapy category i.e., 96% Vs. 42.80 and 96% Vs. 15.38% respectively. The means of the surgical category compared the chemotherapy and stenting were significantly different 18.45 (8.8742 - 28.0349) and 16.2727 (6.6924 - 25.8331) with 95% confidence interval and p-value 0.0001367 and 0.0006488 respectively as on the table 3. 50 patients of surgical category, 13 patients on chemoradiotherapy and 7 patients in the stenting group were analyzed. Among them 46 patients were died in 5 years of intervention for malignant bowel obstruction. The overall median survival time was nine month and one year mortality rate was 77.14% overall. Patient within surgical group had longer median survival than stenting and chemotherapy group. Patients those had transfused blood and needed total parental nutrition at the time of intervention were significantly influenced the death rate among all the groups.
|
Variables |
Death rate |
P < = 0.05 |
|
R.R. (95%C.I.) P. Value |
(Significant) |
|
|
< 75 vs > 75 years |
2.13 (0.627 – 7.258) 0.1125 |
NS |
|
BMI < 35 vs. > 35 |
2 (0.803 – 4.980) 0.068 |
NS |
|
Blood transfusion |
5.25 (2.030 – 13.580) 0.0003 |
Significant |
|
YES vs. NO |
||
|
TPN |
16.62(4.260 – 64.878) 0.00002 |
Significant |
|
YES vs. NO |
||
|
Surgery vs. Chemoradiotherapy |
0.99 (0.835 – 1.190) 0.485 |
NS |
|
Surgery vs. stenting |
1.07 (0.785 – 1.468) 0.328 |
NS |
Table 3: Multi variable analysis for outcome of survival time
Non-surgical patients were associated increase risk of mortality 0.99 (0.835 – 1.190) 0.485. The risk ratio for death for surgery compared to chemotherapy and stenting were 0.6783 (0.4973 – 0.9250) 0.0249 and 0.7826 (0.5599 – 1.0939) 0.1766 for those patients required blood transfusion. The risk ratio for death for surgery compared to chemotherapy and stenting were 0.8696 (0.5784 – 1.3072) 0.5130 and 0.7826 (0.5599 – 1.0939) 0.1766 which were non- significant for the patients required TPN. The associated factors which is highly responsible for the outcome of the survival were analyzed by Cox regression Analysis. The five-year survival rate as reported and recorded were analyzed by Cox hazard ratio and Kaplan Meir Survival Analysis with the help of recorded data and events.
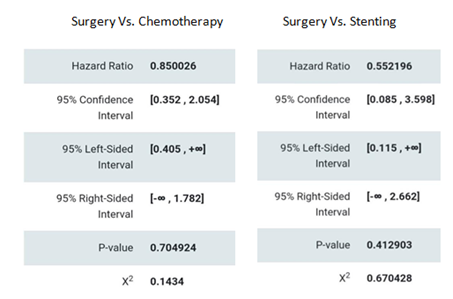
Calculation of hazard ratio
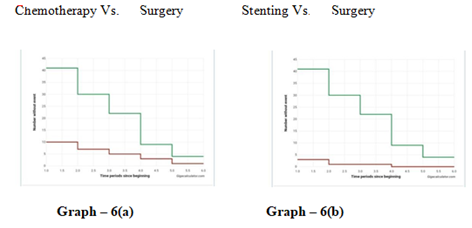
Time event graph analysis
The Hazard ratio, 95% confidence interval and p-value for the 5-year death rate for surgery compared to Chemotherapy and Stenting were 0.85 (0.352 – 2.054) 0.70 and 0.55 (0.085 – 3.598) 0.41 respectively. Mortality related to surgery and other interventions were compared and found to be non-significant. Thus, median survival time calculated among different interventional groups remain significant for survival analysis.
Discussion
Patients with malignant bowel obstruction represent a complex and heterogeneous population. Previous studies have reported on the effectiveness of palliative surgery for MBO. Most of which focused on gynecological and G.I. cancer population [20-22]. In our study we observed higher symptom relief rate and prolonged survival rate after any palliative surgery compared with non-surgical procedures such as endoscopic stenting or chemotherapy. The priority of care for inoperable patients was to control their symptoms and improve their quality of life. Medical treatment combining total parenteral nutrition, opioids, antiemetics and somatostatin drugs are usually considered to be preferred treatment [23]. The primary goal in any palliative procedures are symptom relief and restoration of oral feeding. Single site obstruction can be resolved by endoscopic stenting and diversion ostomy with chemotherapy [24,25]. However, some patients with complete obstruction may have different sites and acute presentation requires immediate surgery for relief of symptoms. The overall symptoms relief rate of all the patients included in this study was 75.71%. The surgery group achieved a higher symptoms relief rate than the others 96% Vs. 42.80% Vs. 15.38% as discussed on table 4.
|
Clinical Study |
Type of intervention |
Outcomes |
|
Jay SH et al. [24] |
GJ Vs. SEMS |
Success rate: 95.6% Vs. 96% |
|
Overall survival: 393 days Vs. 129 days |
||
|
Enrico Fiori M.D. et al. [25] |
Endoscopic placement Vs. Diverting Stoma |
Hospital stay: |
|
2.6 days Vs. 8.1 days. Mean long term survival |
||
|
297 days (125 – 612 days) Vs. 280 days (135days – 571 days) |
||
|
Vashi PG et al. [26] |
PEG |
Symptoms relief 100%. |
|
Recurrence of obstructive symptoms 5 – 129 days |
||
|
Idakikkedar P et al. [27] |
Surgery Vs. Chemotherapy |
Median survival: |
|
45 days (38 – 49) P=0.128 |
||
|
Caceres A et al. [28] |
Endoscopic Stent placement |
Median survival: 7.7 months (3.19 – 11.9 |
|
Van OOijen et al. [29] |
Surgery Vs. Non-operative |
Median survival: (109 – 191) days Vs. (33 – 78) days |
|
Thoms J Miner et al. [30] |
Palliative surgery |
Symptom relief : 46%. |
|
Post operative complication: 35% Median survival: 34 months |
||
|
Our study |
Surgery Vs. Chemo. Vs. Stenting |
Overall symptom improvement: 75.71% (96% Vs 42.80% Vs. 15.38%) |
|
Overall 1 year survival rate: 77.14% |
||
|
Median Survival rate: 270 days Vs. 180 days Vs. 190 days |
Table 4: Comparison among different studies
Conclusions
Malignant obstruction is an emergency condition in most of times needs urgent symptom relief by any mean of palliation. At this same time, it needs nutritional and psychological support in both pre and post-diagnostic procedures. Complete and unresectable malignant obstruction needs diversion colostomy or any by-pass surgeries. Among all type of surgeries resection and anastomosis with or without diversion of loop is best palliation in all settings of surgery. Pre-operative diagnosis of acute intestinal obstruction due to any malignancy is not completely conclusive hence laparotomy and post OP histopathological gradation is required for further treatment. In most of cases surgeries are practiced than the other modalities in acute or sub-acute conditions as patients’ needs urgent symptomatic reliefs. Overall, 5-year survival rate are insignificantly different among all the treatment modalities as the patients present in advance stage of malignant disease. But symptoms relief rate is more in surgical group than other stenting or chemotherapy group of patients. Anemia, hypoproteinemia and ascites were significant factors effect on the prognosis and survival time. For improvement of quality-of-life surgery is the priority among all type of treatment modalities in acute and sub-acute conditions.
References
- Ahmed O, Lee JH, Thompson CC, et al. AGA Clinical practice Update on the Optimal Management of the malignant alimentary tract obstruction. Expert rev
- Baron TH, Kozarek RA. Endoscopic stenting of Colonic tumours. Best Pract Res Clin. Gastroenterol. 2004, 18 (2004) : 209-229.
- Zattoni D. Christofaridis D. How best to Palliate and treat emergency conditions in geriatric patients with colorectal cancer. Eur J Surg On Col. 2020 Mar.; 46(3) : 369- 378.
- Harima S, Fujimoto Y, Amcno S, et al. Comparison of duodenal stenting and gestrojejunostomy for duodenal obstruction with billiary obstruction. J Gestro Intestinal Surg 26 (2022): 1853-1862.
- Jey J, Back MF, Shakespeare TP, et al. The role of palliative radiation therapy in Symptomatic locally advanced gastric cancer. Int J Radiat Onco Biol Phys 67 (2007): 385-388.
- FeuerDJ, Broadley KE, Corticosteroids for the resolution of Malignant bowel obstruction in advanced gynaecological and gastrointestinal cancer. Cochrane data base Syst. Rev. 2000; 2000(2). CD001219.
- Cousins SE, Tempest E, Feuer DJ. Surgery for the resolution of symptoms in malignant bowel obstruction in advanced gynaecological and gastrointestinal cancer. Cochrane Database Syst. Rev 4 2 (2016): CD002764.
- Aaadam AA, Martin JA, Enteral Stents in Malignant bowel obstruction. Gastrointest Endosc Clin N Am 23 (2013): 153-164.
- Englert ZP, White MA, Fitzgeral JL, et al. Surgical management of Malignant bowel obstruction: at what price palliation ? Am surg 78 (2012): 647-652.
- Kaw M, Sing S, Gagne Ja H. Clnical outcome of simultaneous self expendable metal stent for palliation of malignant billiary and duodenal obstruction surg. Endosc 17 (2003): 457-461.
- Yeh Chen Lee, Mazhn Jivraj, Catherine O’ Bren, et al. Malignant Bowel Obstruction in advanced gynaecological cancer : An updated Renew from multidisciplinary prospective; obstetrics and gynaecology international (2018): 18672381.
- Tran E, Spisetlard C, Sandhu NP, et al. Malignant Bowel Obstruction with recurrent ovarian cancer. Arn J Hosp Palliative Care 33 (2016): 272-275.
- Alese OB, Kim S, Cheri Z, et al. Management Patterns and Predictors of mortality among US patients with cancer hospitalize for malignant bowel obstruction cancer 121 (2015): 1772-1778.
- Chen JH, Huang TC, Cheng PX, et al. Malignant bowel obstruction. A Retrospective Clinical Analysis. Mol Cli. Oncol 2 (2014): 13-18.
- Currow DC, Qinn S, Ager M, et al. Double- blind, placebo - Controlled, randomized trial of Octreotide in malignant bowel obstruction. J Pain symptom manage. 49 (2015): 814-821.
- Jang SH, Lee H, Min BH, et al. Palliative Gastrojejunostomy Vs. Endoscopic stent placement for gastric outlet obstruction in patients with unresectable Gastric Cancer: a propensity score matched analysis. Surg Endosc 31 (2017): 4127-4223.
- Fiori E, Lamazza A, Schillaci A, et al. Palliative Management for Patients with sub acute obstruction and stage IV unresectable rectosigmoid cancer: Colostomy Vs. Endoscopic stenting: Final result of a prospective randomized trial. Am J Surg 204 (2012): 321-326.
- Vashi PG, Dahlk S, Vashi RP, et al. Percutaneous Endoscopic gastrostomy tube occlusion in Malignant peritoneal Carcinomatosis - Induced bowel obstruction. Eur J Gastroenterol Hospital 23 (2011): 1069-1073.
- Idaikkadar P, Georgious A, Skene S, et al. Non Surgical Management of Malignant Bowel Obstruction in advanced ovarian cancer patients. A system review and metaanlysis.Arn J Hosp. Pallative Care 39 (2022): 838-846.
- Caceres A, Zhou Q, Lasmos A,et al. Colorectal stent for Palliation of large bowel obstruction in recurrent gynaecological cancer : An updated Series. Gynacol Oncol 108 (2008): 482-485.
- Van Ooijen B, Van Der BergMEL, Planting Asth, et al. Surgical treatment or gastric drainage only for intestinal obstruction in patients with Carcinoma ovary or peritoneal Carcinometosis of other origin. Surg Gynaecol Obstet. 176151 (1993): 469-474.
- Miner TJ, Jaques DP, Shriver CD. A prospective evolution of patients undergoing surgery for the palliation of an advanced malignancy. Ann Surg Oncol 9 (2002): 696-703.
- Currow DC, Qinn S, Ager M, et al. Double - blind, placebo - Controlled, randomized trial of Octreotide in malignant bowel obstruction. J Pain symptom manage 49 (2015): 814-821.
- Jang SH, Lee H, Min BH, et al. Palliative Gastrojejunostomy Vs. Endoscopic stent placement for gastric outlet obstruction in patients with unresectable Gastric Cancer: a propensity score matched analysis. Surg Endosc 31 (2017): 4127-4223.
- Fiori E, Lamazza A, Schillaci A, et al. Palliative Management for Patients with sub acute obstruction and stage IV unresectable rectosigmoid cancer: Colostomy Vs. Endoscopic stenting : Final result of a prospective randomized trial. Am J Surg 204 (2012): 321-326.
- Vashi PG, Dahlk S, Vashi RP, et al. Percutaneous Endoscopic gastrostomy tube occlusion in Malignant peritoneal Carcinomatosis - Induced bowel obstruction. Eur J Gastroenterol Hospital 23 (2011): 1069-1073.
- Idaikkadar P, Georgious A, Skene S, et al. Non Surgical Management of Malignant Bowel Obstruction in advanced ovarian cancer patients. A system review and metaanlysis.Arn J Hosp. Pallative Care 39 (2022) : 838-846.
- Caceres A, Zhou Q, Lasmos A,et al. Colorectal stent for Palliation of large bowel obstruction in recurrent gynaecological cancer: An updated series. Gynacol Oncol 108 (2008): 482-485.
- Van Ooijen B, Van Der BergMEL, Planting Asth, et al. Surgical treatment or gastric drainage only for intestinal obstruction in patients with Carcinoma ovary or peritoneal Carcinometosis of other origin. Surg Gynaecol Obstet. 176151 (2011): 469-474.
- Miner TJ, Jaques DP, Shriver CD, A prospective evolution of patients undergoing surgery for the palliation of an advanced malignancy. Ann Surg Oncol 9 (2002): 696-703.
