An Insight to Illness Narrated by A Patient with Right Hemisphere Damage Associated with Frontal Blood Flow Changes: An Implication for Self-Treatment of Lifestyle-Related Diseases
Article Information
Junko Takada MSc1,2, Kenichi Meguro MD, PhD1,2,3,4*, Shigeo Kinomura MD, PhD5, Satoshi Yamaguchi MD, PhD1,2
1Geriatric Behavioral Neurology Project, Tohoku University New Industry Creation Hatchery Center (NICHe), Sendai, Japan
2The Osaki-Tajiri SKIP Center, Osaki, Japan
3Tohoku University CYRIC, Sendai, Japan
4Tohoku University Graduate School of Medicine, Sendai, Japan
5Clinic of Imaging Medicine and Brain Health, Sendai, Japan
*Corresponding Author: Kenichi Meguro, MD, PhD, Geriatric Behavioral Neurology Project, Tohoku University New Industry Creation Hatchery Center (NICHe), 4-1, Seiryo-machi, Aoba-ku, IDAC, 980-8575 Sendai, Japan
Received: 07 October 2020; Accepted: 19 October 2020; Published: 20 November 2020
Citation: Junko Takada, Kenichi Meguro, Shigeo Kinomura, Satoshi Yamaguchi. An Insight to Illness Narrated by A Patient with Right Hemisphere Damage Associated with Frontal Blood Flow Changes: An Implication for Self-Treatment of Lifestyle-Related Diseases. Archives of Clinical and Medical Case Reports 4 (2020): 1096-1107.
View / Download Pdf Share at FacebookAbstract
The authors experienced a case (Mr. T) with right hemisphere infarction. After he came to understand his disease, he changed his behavior; he reflected on his past conduct, had the consciousness to face his disease, improved his daily life. He talked about his past behavior as the cause of cognitive impairment. Mr. T reviewed his past behaviors before the hospital visit, saying “I can fully understand the way I am by considering my disease and myself separately.” Furthermore, as his living activities changed, the right frontal cerebral blood flow also improved. Early diagnosis is not necessarily accepted negatively by patients and their family. When an early diagnosis is made with an explanation of the disease, the patient may reflect on their past conduct, leading to changes in their living activities. In our case, it was fortunate that there were no problems.
Keywords
Right hemisphere; Cerebral infarction; Vascular cognitive impairment; Self-treatment
Right hemisphere articles; Cerebral infarction articles; Vascular cognitive impairment articles; Self-treatment articles
Right hemisphere articles Right hemisphere Research articles Right hemisphere review articles Right hemisphere PubMed articles Right hemisphere PubMed Central articles Right hemisphere 2023 articles Right hemisphere 2024 articles Right hemisphere Scopus articles Right hemisphere impact factor journals Right hemisphere Scopus journals Right hemisphere PubMed journals Right hemisphere medical journals Right hemisphere free journals Right hemisphere best journals Right hemisphere top journals Right hemisphere free medical journals Right hemisphere famous journals Right hemisphere Google Scholar indexed journals Cerebral infarction articles Cerebral infarction Research articles Cerebral infarction review articles Cerebral infarction PubMed articles Cerebral infarction PubMed Central articles Cerebral infarction 2023 articles Cerebral infarction 2024 articles Cerebral infarction Scopus articles Cerebral infarction impact factor journals Cerebral infarction Scopus journals Cerebral infarction PubMed journals Cerebral infarction medical journals Cerebral infarction free journals Cerebral infarction best journals Cerebral infarction top journals Cerebral infarction free medical journals Cerebral infarction famous journals Cerebral infarction Google Scholar indexed journals Vascular cognitive impairment articles Vascular cognitive impairment Research articles Vascular cognitive impairment review articles Vascular cognitive impairment PubMed articles Vascular cognitive impairment PubMed Central articles Vascular cognitive impairment 2023 articles Vascular cognitive impairment 2024 articles Vascular cognitive impairment Scopus articles Vascular cognitive impairment impact factor journals Vascular cognitive impairment Scopus journals Vascular cognitive impairment PubMed journals Vascular cognitive impairment medical journals Vascular cognitive impairment free journals Vascular cognitive impairment best journals Vascular cognitive impairment top journals Vascular cognitive impairment free medical journals Vascular cognitive impairment famous journals Vascular cognitive impairment Google Scholar indexed journals cognitive impairment articles cognitive impairment Research articles cognitive impairment review articles cognitive impairment PubMed articles cognitive impairment PubMed Central articles cognitive impairment 2023 articles cognitive impairment 2024 articles cognitive impairment Scopus articles cognitive impairment impact factor journals cognitive impairment Scopus journals cognitive impairment PubMed journals cognitive impairment medical journals cognitive impairment free journals cognitive impairment best journals cognitive impairment top journals cognitive impairment free medical journals cognitive impairment famous journals cognitive impairment Google Scholar indexed journals Chronic kidney disease articles Chronic kidney disease Research articles Chronic kidney disease review articles Chronic kidney disease PubMed articles Chronic kidney disease PubMed Central articles Chronic kidney disease 2023 articles Chronic kidney disease 2024 articles Chronic kidney disease Scopus articles Chronic kidney disease impact factor journals Chronic kidney disease Scopus journals Chronic kidney disease PubMed journals Chronic kidney disease medical journals Chronic kidney disease free journals Chronic kidney disease best journals Chronic kidney disease top journals Chronic kidney disease free medical journals Chronic kidney disease famous journals Chronic kidney disease Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Self-treatment articles Self-treatment Research articles Self-treatment review articles Self-treatment PubMed articles Self-treatment PubMed Central articles Self-treatment 2023 articles Self-treatment 2024 articles Self-treatment Scopus articles Self-treatment impact factor journals Self-treatment Scopus journals Self-treatment PubMed journals Self-treatment medical journals Self-treatment free journals Self-treatment best journals Self-treatment top journals Self-treatment free medical journals Self-treatment famous journals Self-treatment Google Scholar indexed journals kidney articles kidney Research articles kidney review articles kidney PubMed articles kidney PubMed Central articles kidney 2023 articles kidney 2024 articles kidney Scopus articles kidney impact factor journals kidney Scopus journals kidney PubMed journals kidney medical journals kidney free journals kidney best journals kidney top journals kidney free medical journals kidney famous journals kidney Google Scholar indexed journals
Article Details
Article Summary
Strengths and limitations of this study
- It is important to provide effective explanation on illness based on an understanding the difference between the right and left hemispheres.
- In our case, it was fortunate that there were no problems in the left hemisphere, and memory and language comprehension were preserved.
- After the case came to understand his disease, he changed his behavior; he reflected on his past conduct, had the consciousness to face his disease, improved his daily life, and talked about the importance of early diagnosis and received an explanation about the disease.
- Limitation is one case report.
1. Introduction
Long-term Care Insurance (LTCI) provides medical and care services as a legal contract, based on the free will of individuals. However, being understood by the people surrounding them is essential for dementia patients to be able to continue to live in a familiar surrounding (the Orange Plan). In addition to early detection and intervention of dementia, the Community General Support Center (CGSC) plays a role in understanding dementia as the base for self-help as self-care, and complementary or mutual assistance for the self-help.
The 1st author have experience in working at a CGSC as a care manager [1]. Many people whom the author met at the Center did not agree to visit a hospital, even if special medication was objectively considered to be necessary, or rather inevitable. Self-care, that is, self-help to face one’s own disease with one’s own will, is limited due to impaired judgement. Therefore, it is fortunate that a patient can visit an outpatient department to commence treatment for dementia. The patients, who have anxiety about changes in themselves, must have immeasurable bravery and preparation to face their disease to relieve the anxiety of people surrounding them. The process is very long and difficult, and thus, I have been distressed by the gap between the ideal world and reality every day.
At present, the 1st author works as a psychologist at a memory clinic. In the daily work, after medical consultation by a specialist, Magnetic Resonance Imaging (MRI) and/or Single Photon Emission Computed Tomography (SPECT) neuroimaging, and neuropsychological examinations for each new patient, the author explains the policies of the treatment or care to the patient and family, possibly in the presence of a care manager, in order to discuss the policies. In the clinic, we consider it important to explain the disease state, and when necessary, we focus on the explanation of dementing diseases, such as Alzheimer disease (AD) and vascular dementia (VaD), as an underlying disease, rather than the name of symptoms, dementia, which tends to be considered as a social label.
Although the notification of the diagnosis of dementia is recommended by the Medical Service Act, there are still mixed reactions to such an announcement. According to the report by Mizutani [2], 13 out of the 16 persons, who were informed that they had the diagnosis of dementia, responded that the diagnosis was eventually good, in the interview. Firstly, there have been very few reports on how dementia patients accept the explanation of the disease from a physician.
Regarding our case (Mr. T) who visited the specialty dementia outpatient clinic, he was able to commence the treatment after overcoming the first hurdle with support from his family. Since Mr. T could logically accept the explanation of the disease state from a physician (K.M) and reflected on his past thoughts and conduct, he was able to show improvement of the psychobehavioral symptoms and living habits as if he could regain his former self.
This case was a new experience, even for a specialist (K.M), and discussions could be made based on the cerebral disease state. Herein, we report the case because it is important in providing a “suggestion of the methods for brain disease state-based care and mund therapie.” Prior to preparation of this report, we obtained approval and written informed consent from the patient and his family. The Ethical Committee of the Osaki-Tajiri SKIP Center approved this report (#2017-0526).
2. Case Report
Mr. T, an 81-year-old right-handed man
2.1 Education
16 years (educational background: university)
2.2 Chief complaints
(Patient) Memory loss, (His wife) Memory loss and short temper
2.3 Family history
Nothing of interest
2.4 Past medical history
Diabetes mellitus, hypertension, atrial fibrillation, and gastric ulcer after a stent surgery. When he was a company worker, he liked to smoke and consume alcohol.
2.5 Personality before suffering from the disease
He was gentle and peaceful. He was sometimes short tempered with his wife, as he was an overbearing husband. He was energetic at work, and an intelligent person with much knowledge about social conditions.
2.6 Life history
He was born as the oldest son and had 4 brothers. After graduating from university, he worked for an insurance company for 35 years until retirement as a director. After retirement, he worked as a security officer. When he was a company worker, he never cooked under the policy, “A real man stays away from the kitchen.” However, his wife had great regard for his dedicated care for his parents, i.e., help with eating and bathing, for about 20 years while working for the company. As a hobby, he loved to read books about international politics and economics.
Present illness
- Around year X-3: He began to frequently experience memory loss and suddenly shout angrily at his wife. In addition, he began to break chopsticks by biting the tip.
- Around year X-2: The memory loss and short temper gradually became aggravated, and he sometimes appeared spaced-out, exhibiting unstable feelings. Although his family booked an appointment for examination at a brain health check center for dementia, he cancelled it by phone without notifying his family.
- Around year X-1: He was not able to return home on two occasions after visiting the next city by motorbike. At that time, Mr. T said, “My mind became a complete blank.” Furthermore, his unstable feelings became aggravated, and he fell down frequently. In addition, changes were observed in his behaviors, such as eating with his elbow on the table, although he was usually strict about good manners.
- Around June in the year of X: He began to walk slowly with slouch and shuffle. The memory loss was further aggravated, and he could not remember the story of a TV drama or a book. He experienced anxiety since he had to read the same book repeatedly.
- In July in the year of X: After talking by phone with his grandchild who recommended he visit a hospital, he made up his mind to visit the specialty outpatient department of our clinic.
2.8 Present symptoms
- General internal medicine/examination findings: Blood pressure, pulse, blood test, and electrocardiogram are normal.
- Neurological findings: No disorder in the field of view or paralysis were confirmed.
- Daily life: In the basic activities of daily living (ADL), there were no problems, and the patient lived independently. Barthel Index was 100/100.
Neuroimaging image findings
(see Figure 1).
MRI [3]
These are the T1 weighted images (TR: 564, TE: 11, FA: 80) and the T2 weighted images (TR: 4450, TE: 80, FA: 180) from a 1.5T MRI (Toshiba), and the FLAIR images (TR: 8000, TE: 82, FA: 150, TI: 2400). Diagnosis was made by a neurologist, using the axial and coronal images. In the MRI images, right parietal damage was confirmed.
SPECT [4]
After an intravenous line was ensured, 600 MBq of 99mTc-ethyl cysteinate dimer (99mTc- ECD) was administered at a dorsal position with complete rest and closed eyes. Ten minutes after administration, images were taken using a γ-camera (Multispect, Siemens Medical Systems, Inc.). The projection data were saved in 128*128 format. For image reconstruction (0.7 cycle/cm) and attenuation correction, Shepp Logan Hanning filter and the Chang method were used, respectively. In SPECT images, due to the remote effect of the right parietal lobe damage, a decrease in blood flow was confirmed in the medial frontal lobe.
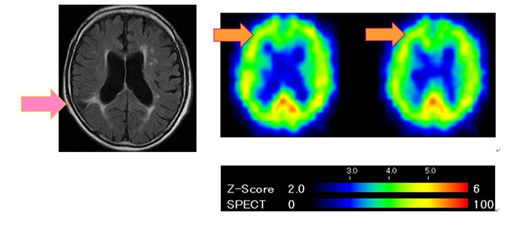
Figure 1: Neuroimaging image findings.
Neuropsychological findings
(see Table 1).
- General cognitive function was evaluated as 26 points on the MMSE [5], and points were lost for place orientation, 3-word recall, writing, and figure copying.
- Memory was evaluated with the Wechsler Memory Scale-Revised. Although general memory, verbal memory, and attention/concentration were within the normal range, visual memory and delayed recall were poor.
- Although anosognosia and hemispatial neglect were not confirmed, constructional impairment was observed in the pantomime of scissors use, imitation of finger configurations. The Necker cube copying task [6, 7] also revealed constructional impairment as illustrated by Figure 2.
|
Neuropsychological test items |
Points |
|
|
General cognitive function |
MMSE |
26/30 Items with loss points: place orientation: 4/5 3-words recall: 2/3, and writing: 0/1 |
|
Memory |
WMS-R |
General memory: 74 verbal memory: 87 attention/concentration: 99 visual memory: 57 and delayed recall: 65 |
|
Subjective memory |
Living amnesia checking |
Patient: 23 Family: 14 |
|
BPSD |
Behave-AD total points |
Total points: 4 Subordinate items: fear/horror: 2 circadian rhythm disorder: 2 |
|
Depression |
GDS15 |
6/15 |
MMSE=Mini Mental State Examination; WMS-R=Wechsler Memory Scale-Revised; BPSD=Behavioral and psychological symptoms of dementia; BEHAVE-AD=Behavioral Pathology in Alzheimer’s Disease Rating Scale; GDS=Geriatric Depression Scale
Table 1: Neuropsychological findings.

Figure 2: The Necker cube copying task.
- No dressing disability was apparent.
- In the memory checklist, awareness of memory loss was more apparent in the patient, rather than the family.
- Among the behavioral symptoms, anxiety and diurnal rhythm disturbances (large changes in sleep patterns, i.e., 8-9 hours of sleeping, but with no good sleep, waking up to go to the bathroom 3-4 times) were confirmed in the Behavioral Pathology in Alzheimer’s Disease Rating Scale (BEHAVE-AD) [8].
- Based on the Geriatric Depression Scale (GDS)-15 [9], a mild depressive mood was confirmed.
2.11 A meeting on treatment
Based on these data, a meeting was held for explanation of the disease state by the physician in charge and discussion of the therapeutic policy. In the meeting, the physician (K.M) explained the diagnosis of the disease, in which a cerebral infarction had developed in the right hemisphere, causing cognitive dysfunction, mainly visuospatial dysfunction. Although the patient met the diagnostic criteria for VaD, the disease name was not mentioned. The focus was placed particularly on the fact that his symptoms were caused by a cerebral lesion, and that it was not a fault of Mr. T because his symptoms were caused by the disease. Then, in addition to the drugs prescribed by his general physician for diabetes, hypertension, and atrial fibrillation, treatment with drugs was commenced that were thought to improve cerebral blood flow and metabolism.
2.12 Reaction to the disease and explanation of the disease state
Three months after the policy review meeting, the first author, who conducted the psychological tests, interviewed Mr. T and his wife about the visit to the specialty outpatient department.
Mr. T said, “I thought my symptoms were caused by aging, but it was good for me to visit the clinic. After the visit, I felt relieved, because the physician explained that it was not my fault and that the disease caused my symptoms. I could understand the reasons for my frequent memory losses.”
His wife also suggested the importance of the visit to the specialty clinic, saying “I felt relieved because I could rely on the physician who said that his symptoms were caused by the disease, and were not his fault. I do not have to worry about him alone.”
2.13 Self-reflection for past conduct/future changes in actions
Based on self-reflection by Mr. T of his past conduct and information obtained from his family, we indicate the items that suggested significant changes in his actions (see Table 2).
|
Before the hospital visit |
During the review by Mr. T |
After the hospital visit |
|
|
Short temper |
Easily feeling frustrated and getting angry. Having unstable feelings |
Mr. T said, “I got irritated for no reason. I felt released after the hospital visit.” |
He became gentle and peaceful with less changes in his emotions, and began to feel warmth for his wife. |
|
Motivation |
Not interested in hobbies, such as reading and walking |
Mr. T said, “I did not want to read a book because I could not understand the story at all. However, I wanted to enjoy light reading, such as a magazine.” |
He began to enjoy light reading, such as magazines. He began to walk for 40 minutes to 1 hour every day. |
|
Risk judgement |
Frequently driving dangerously. Hoping to drive a car and buy a new car. Trying to buy a new car and disagreeing with his families’ recommendation to stop driving. |
Mr. T said, “It was good for me to stop driving because many accidents had occurred recently.” |
He agreed to sell his car, and now goes out by bicycle or bus. |
Table 2: Reflection on past conduct/changes in actions after hospital visit.
Regarding the short temper of Mr. T in the past, he reviewed that he became irritated with no reason, and said, “I felt relieved after visiting the clinic.” Actually, his wife also felt that he became more gentle and peaceful with fewer changes in his feelings. Six months after the first visit, he bought a piece of cake for his wife to thank her for her assist in New Year days. She was deeply moved by his gentle concern, which had been seen before the disease onset. Regarding the changes in her husband, she expressed that he seemed to show growth.
In addition, although reading was his hobby, Mr. T had not read any book for about 1 year. To this end, he reviewed that he did not want to read a book because he could not understand the story at all. After his actions changed, he hoped to enjoy light reading, such as a magazine, and began to buy his favorite books. Four months after the interview, he brought an introductory book about Russia, written from the perspective of national interest, when he visited the outpatient department of our clinic. Regarding exercise habits, he began to walk for 40 minutes to 1 hour every day.
In addition, since he frequently tried to ignore the red-light and drove carelessly, his family who rode together in the car with him recommended him to stop driving. Since he liked cars, he did not accept the recommendation. Furthermore, he attempted to buy a new car upon a safety inspection, because he still wanted to drive a car. However, after commencement of the treatment, he said that it was good for me to stop driving because many accidents had occurred recently.” He agreed to sell his car, and more recently goes out by bicycle or bus.
2.14 SPECT images after self-reflection/treatment
In the SPECT images after self-reflection/treatment, it was confirmed that the blood flow in the right medial prefrontal area, which had been decreased due to the remote effect,10 was improved (see Figure 3).
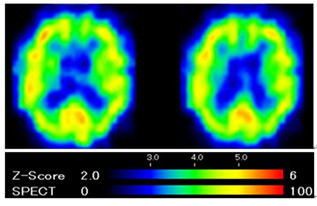
Figure 3: SPECT images after self-reflection/treatment.
2.15 Successive clinical course
About 6 months after the interview, Mr. T said again, “It was good for me to visit the specialty outpatient clinic, because I felt relieved. Before the visit, I had become delusional about the anxiety of developing dementia. I was able to make a decision based on clinical data. Worrying about the possibility of dementia alone was like grabbing on to a cloud.”
3. Discussion
Although Mr. T cancelled the scheduled examination 2 year ago, he decided to visit a specialty outpatient clinic when moved by the recommendation of his grandchild, and this was the starting line of the treatment. Thereafter, 2 propositions, “It is not my fault because the disease caused the symptoms,” and “I do not develop dementia,” led to changes in his actions after he reviewed his own past circumstances and conduct. Even for caregivers, explanation about the disease state led to review and changes in their communication with him, decreasing the circumstances in which he easily became angry.
There were several qualitative studies on subjective experience for stroke and self-esteem of health. Hyakuta [11] interviewed stroke patients, and found 5 patterns of recovery based on changes in the aspects of lack of comprehension, actually feeling, happiness, ambivalence, and new values. Conventionally, bouts of despondency have been considered a negative factor that hinders rehabilitation, but after overcoming, the patients not only recovered to the original level, but was able to proceed to a new level. He concluded that bouts of despondency can be perceived as an opportunity to promote recovery and suggest the need to support that opportunity with care. He [12] also tried to clarify how stroke patients experienced in chronic phase. During the course of rehabilitation, the patients wavered between the relatively positive experience of getting accustomed and the negative experience of “impatience. Patients with the more positive experiences noted that they realized that this is a product of stroke, while patients with more negative experiences noted disappointment. These experiences did not change in a stepwise fashion, but rather wavered during the course of recovery and were associated with rehabilitation continuation factors.
Yokoyama et al. [13] analyzed the changes in self-esteem after stroke, and found it be correlated with activity of daily living, back-to-work situation, subjective health, and emotional support provider. They suggest that it is necessary to improve the level of self-esteem, every time after stroke should spent focusing on particular attention to the patient’s health condition.
For the case Mr. T, as a neurological explanation, it was suggested that the functions of the left hemisphere were preserved, and his linguistical or logical understanding was favorable in the explanation by the physician about the brain imaging findings, prognosis, drug administration, diet, exercise, and other cautions about daily life. We discuss the following, which enabled reflection on past conduct and changes in actions in the future: the first proposition: “It is not my fault because the disease caused the symptoms,” and the second proposition: “I do not develop dementia.”
The first proposition suggests the importance of insight about oneself from the third person perspective. Schwartz and Begley [14] who performs cognitive behavioral therapy as treatment for patients with obsessive-compulsive disorder who are troubled over obsessive thoughts, attaches a high value to “awareness” (mindfulness), i.e., “It is not my fault because the disease caused the symptoms.” In addition, it has also been reported that the blood flow in the medial prefrontal lobe improved in patients who successfully overcame obsessive thoughts and changed their actions by viewing themselves from the third person. Mr. T also exhibited improved blood flow in the right medial prefrontal lobe, which is related to self-consciousness of actions, in the SPECT findings after his reflection and changes in actions, and the improvement corresponded to his reflection.
Regarding the second proposition, we had mixed feelings. The attending physician had a therapeutic policy not to use the word, “dementia,” which might be misunderstood as AD; although the patient met the diagnostic criteria for VaD. From this, the patient had a sense of security and felt comfortable, understanding that he would not develop dementia. This was a mainspring of his actions. It was real that he had a negative image of dementia, and might have changed his actions by differentiating himself to deny the hopelessness.
The diagnosis of dementia ensures the treatment, prognosis, quality of life (QOL), and dignity of individuals, while, unfortunately, causing prejudice and infringement of right due to its negative image. Among the names of diseases and symptoms, dementia may be considered as a social label in many cases. Explanation of the disease state provides more merits to patients and their family, than announcement of the word, “dementia.” It may be necessary to review the word, “dementia,” because it is a name that describes symptoms, as seen in “fever,” “diarrhea,” etc. For example, there are no words, such as “fever cafe” and “diarrhea driver.”
Traphagan [15] suggests that BOKE, dementia, and AD have a higher social sense of alienation, in this order, in Japan. It has also been reported that, although psychological fragmentation might be a social label, the rate of announcement of this disease has increased since its name was changed to integration dysfunction syndrome. The current case made us consider “dementia” as a “social model.”
Funding
The authors have not declared a specific grand for this research from any funding agency in the public.
Competing Interests
None declared.
Patient Consent for Publication
Obtained
Ethics Approval
Yes
References
- Takada J, Meguro K, Sato Y, et al. Life concerns of elderly people living at home determined by Community General Support Center staff: Implications for organizing more effective integrated community care system. The Kurihara Project. Psychogeriatrics 14 (2014): 188-195.
- Mizutani K. When you meet an illness. Jap J Geriatr Psychiatr 26 (2015): 961-966.
- Ishii H, Meguro K, Yamaguchi S, et al. Prevalence and cognitive performances of vascular cognitive impairment no dementia in Japan: the Osaki-Tajiri Project. Eur J Neurol 14 (2007): 609-616.
- Meguro K. Cholinesterase inhibitors are compatible with psychosocial intervention for Alzheimer disease patients suggested by neuroimaging findings. Psychiatr Res 259 (2017): 29-33.
- Folstein MF, Folstein SE, McHugh PR. ‘Mini-Mental State’: A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12 (1975): 189-198.
- Shimada Y, Meguro K, Kasai M, et al. Necker cube copying ability in normal elderly and Alzheimer’s disease. A community-based study: The Tajiri Project. Psychogeriatrics 6 (2006): 4-9.
- Oonuma J, Kasai M, Meguro K, et al. Non-3D pattern of copying Necker cube as a risk of dementia among non-demented population: Reanalysis from the Tajiri project. Psychogeriatrics 16 (2016): 298-304.
- Monteiro IM, Boksay I, Auer SR, et al. Addition of a frequency-weighted score to the Behavioral Pathology in Alzheimer's Disease Rating Scale: The BEHAVE-AD-FW: Methodology and reliability. Eur Psychiatr 16 (2001): 5s-24s.
- Sutcliffe C. A new version of the Geriatric Depression Scale (Residential) (GDS-12R). Int Psychogeriatr 12 (2000): 173-181.
- Baron JC, D’Antona R, Pantano P, et al. Effects of thalamic stroke on energy metabolism of the cerebral cortex. A positron emission tomography in man. Brain 109 (1986): 1243-1259.
- Hyakuta T. The subjective experience of the recovery process for stroke patients: From acute to recovery period. Hiroshima Univ J Health Sci 2 (2002): 41-50.
- Hyakuta T. Experiences of stroke patients in chronic phase. Jap Red Cross Hiroshima Coll Nurs 9 (2009): 1-10.
- Yokoyama J, Miyakoshi Y. Factors associated with changes in self-esteem after stroke. Jap J Nurs Res 31 (2008): 55-65.
- Schwartz JM, Begley S. The mind and the brain. Harper Collins Publications Inc, NY (2003).
- Traphagan JW. Localizing senility: Illness and agency among older Japanese. J Cross-Cult Gerontol 13 (1998): 81-98.
