Laser Ablation of Metastatic Lymph Nodes in the Neck for Oral Carcinoma-Technique and Viability of the Procedure
Article Information
Rusy Bhalla1*, Seemantini Bhalla1, Duleep Bhonsale2, Ashish Kapadia2
1Department of Oncology, Orchid Center for Laser surgery, Mumbai, India
2Department of Radiology, Orchid Center for Laser surgery, Mumbai, India
*Corresponding Author: Dr. Rusy Bhalla, S1 Link Square mall, Opp KFC Linking Road, Bandra west, Mumbai 400050, India
Received: 12 March 2021; Accepted: 22 March 2021; Published: 26 March 2021
Citation: Rusy Bhalla, Seemantini Bhalla, Duleep Bhonsale, Ashish Kapadia. Laser Ablation of Metastatic Lymph Nodes in the Neck for Oral Carcinoma-Technique and Viability of the Procedure. Journal of Radiology and Clinical Imaging 4 (2021): 027-035.
View / Download Pdf Share at FacebookAbstract
Background: Presence of macro and microdisease in the neck in cases of Oral carcinoma is a major barrier in full recovery of the patient. Conventionally the problem has been handled by Neck dissection popularly referred to as Radical Neck dissection and its many variants like Modified neck dissection and supraomohyoid dissection. The surgery assumes that removal of the fat containing lymph nodes is effective in spread of the disease. The major stumbling block is presence of extra nodal spread in enlarged lymph nodes. Percutaneous lymph node laser ablation (PLALN) is becoming more popular in many centers for necrosing the lymph nodes effectively without the neck dissection. There are obvious advantages and disadvantages to this procedure. This study was aimed at verifying the effectiveness of the procedure and aimed to understand the reason for success and failure if any. Attempt has also been made to understand the Anatomy of Neck Lymphatic system and understand the cellular structure of lymph nodes which would make the procedure effective.
Patients and Methods: 46 patients were of oral carcinoma were included in this observational study. These patients were having Metastatic lymph nodes on Ultrasonography and MRI scans prior to the procedure. The primary tumours were handled by Laser ablation and PLALN was carried out as a part of the procedure.
Results: The procedure was safe and effective in 100 % of cases in necrosing the lymph nodes less than 2.0 cms in longest diameter. It was 70% effective in handling lymph nodes more than 2.0 cms in diameter. It was less than 20% effective in handling lymph nodes more than 3.5 cms in diameter. There was no major side effect of the procedure in any patient.
Conclusion: PLALN is an effective procedure for handling of Meta
Keywords
Lymph node management; Laser ablation; Oral cancer
Lymph node management articles; Laser ablation articles, Oral cancer articles
Lymph node management articles Lymph node management Research articles Lymph node management review articles Lymph node management PubMed articles Lymph node management PubMed Central articles Lymph node management 2023 articles Lymph node management 2024 articles Lymph node management Scopus articles Lymph node management impact factor journals Lymph node management Scopus journals Lymph node management PubMed journals Lymph node management medical journals Lymph node management free journals Lymph node management best journals Lymph node management top journals Lymph node management free medical journals Lymph node management famous journals Lymph node management Google Scholar indexed journals Laser ablation articles Laser ablation Research articles Laser ablation review articles Laser ablation PubMed articles Laser ablation PubMed Central articles Laser ablation 2023 articles Laser ablation 2024 articles Laser ablation Scopus articles Laser ablation impact factor journals Laser ablation Scopus journals Laser ablation PubMed journals Laser ablation medical journals Laser ablation free journals Laser ablation best journals Laser ablation top journals Laser ablation free medical journals Laser ablation famous journals Laser ablation Google Scholar indexed journals Oral cancer articles Oral cancer Research articles Oral cancer review articles Oral cancer PubMed articles Oral cancer PubMed Central articles Oral cancer 2023 articles Oral cancer 2024 articles Oral cancer Scopus articles Oral cancer impact factor journals Oral cancer Scopus journals Oral cancer PubMed journals Oral cancer medical journals Oral cancer free journals Oral cancer best journals Oral cancer top journals Oral cancer free medical journals Oral cancer famous journals Oral cancer Google Scholar indexed journals Percutaneous lymph node laser ablation articles Percutaneous lymph node laser ablation Research articles Percutaneous lymph node laser ablation review articles Percutaneous lymph node laser ablation PubMed articles Percutaneous lymph node laser ablation PubMed Central articles Percutaneous lymph node laser ablation 2023 articles Percutaneous lymph node laser ablation 2024 articles Percutaneous lymph node laser ablation Scopus articles Percutaneous lymph node laser ablation impact factor journals Percutaneous lymph node laser ablation Scopus journals Percutaneous lymph node laser ablation PubMed journals Percutaneous lymph node laser ablation medical journals Percutaneous lymph node laser ablation free journals Percutaneous lymph node laser ablation best journals Percutaneous lymph node laser ablation top journals Percutaneous lymph node laser ablation free medical journals Percutaneous lymph node laser ablation famous journals Percutaneous lymph node laser ablation Google Scholar indexed journals Oral carcinoma articles Oral carcinoma Research articles Oral carcinoma review articles Oral carcinoma PubMed articles Oral carcinoma PubMed Central articles Oral carcinoma 2023 articles Oral carcinoma 2024 articles Oral carcinoma Scopus articles Oral carcinoma impact factor journals Oral carcinoma Scopus journals Oral carcinoma PubMed journals Oral carcinoma medical journals Oral carcinoma free journals Oral carcinoma best journals Oral carcinoma top journals Oral carcinoma free medical journals Oral carcinoma famous journals Oral carcinoma Google Scholar indexed journals MRI scan articles MRI scan Research articles MRI scan review articles MRI scan PubMed articles MRI scan PubMed Central articles MRI scan 2023 articles MRI scan 2024 articles MRI scan Scopus articles MRI scan impact factor journals MRI scan Scopus journals MRI scan PubMed journals MRI scan medical journals MRI scan free journals MRI scan best journals MRI scan top journals MRI scan free medical journals MRI scan famous journals MRI scan Google Scholar indexed journals sonography articles sonography Research articles sonography review articles sonography PubMed articles sonography PubMed Central articles sonography 2023 articles sonography 2024 articles sonography Scopus articles sonography impact factor journals sonography Scopus journals sonography PubMed journals sonography medical journals sonography free journals sonography best journals sonography top journals sonography free medical journals sonography famous journals sonography Google Scholar indexed journals Radical neck dissection articles Radical neck dissection Research articles Radical neck dissection review articles Radical neck dissection PubMed articles Radical neck dissection PubMed Central articles Radical neck dissection 2023 articles Radical neck dissection 2024 articles Radical neck dissection Scopus articles Radical neck dissection impact factor journals Radical neck dissection Scopus journals Radical neck dissection PubMed journals Radical neck dissection medical journals Radical neck dissection free journals Radical neck dissection best journals Radical neck dissection top journals Radical neck dissection free medical journals Radical neck dissection famous journals Radical neck dissection Google Scholar indexed journals metastatic cells articles metastatic cells Research articles metastatic cells review articles metastatic cells PubMed articles metastatic cells PubMed Central articles metastatic cells 2023 articles metastatic cells 2024 articles metastatic cells Scopus articles metastatic cells impact factor journals metastatic cells Scopus journals metastatic cells PubMed journals metastatic cells medical journals metastatic cells free journals metastatic cells best journals metastatic cells top journals metastatic cells free medical journals metastatic cells famous journals metastatic cells Google Scholar indexed journals General anaesthesia articles General anaesthesia Research articles General anaesthesia review articles General anaesthesia PubMed articles General anaesthesia PubMed Central articles General anaesthesia 2023 articles General anaesthesia 2024 articles General anaesthesia Scopus articles General anaesthesia impact factor journals General anaesthesia Scopus journals General anaesthesia PubMed journals General anaesthesia medical journals General anaesthesia free journals General anaesthesia best journals General anaesthesia top journals General anaesthesia free medical journals General anaesthesia famous journals General anaesthesia Google Scholar indexed journals
Article Details
1. Introduction
Thermal ablation is gaining popularity in destruction of tumours in various centers of the world. (Emiliano). Laser ablation is now a recognized procedure approved by USFDA for soft tissue tumours [1].
Main methods of laser Ablation include [2].
- Radiofrequency
- Microwave
- Cryoablaton
Laser offers a controlled thermal ablation with real time visualization under sonography control. In all recent studies therefore laser is becoming increasingly popular in multiple clinical conditions for soft tissue tumours namely Liver, Lung, Thyroid, Oral malignancies [3-7]. Laser ablation for Unresectable Mesentric lymph nodes has been performed with promising results [8]. Lymph nodes are present in a majority of oral cancer patients. Enlarged lymph nodes present as swelling in the submandibular region (Figure 4). In late stages of Carcinoma of oral cavity lymph nodes more than 2.5 cms were present. Most of these lymph nodes had a breach of capsule (Figure 10). Conventionally Lymph nodes in operable cases are handled by neck dissection. The extent of dissection may vary depending on the severity of the case [9]. PLALN was a part of procedure of ablation of Primary Carcinoma through laser ablation [6]. To understand the efficacy of PLALN one must take a look at the anatomy of a lymph node and the lymphatic system. The neck lymphatic system is divided into lymphatics and lymph nodes draining into subclavian vein. Metastatic cells traverse the lymphatics to reach the lymph nodes. Important observation is that they do not multiply in the lymphatics since there is no blood supply inside, but serve only for transit passage for the lymph nodes. The lymph node has an afferent artery and lymphatic vessels and efferent veinule and lymphatic vessel. It is covered by the capsule (Figure 1).
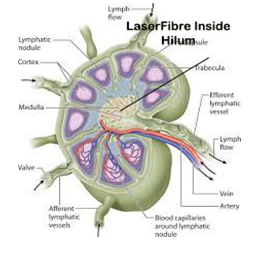
Figure 1: Anatomy of Lymph Node with laser fiber in Hilum.
Any increase in volume due to metastasis is reflected in the following way (Figure 8).
- Loss of fatty hilum.
- Increase in size
- Loss of oval structure to a round shape.
- Further increase can outstrip the blood supply and cause necrosis of the central area.
Destruction of fatty hilum by laserising it effectively devasucalrises the lymph node and leads to necrosis of the lymph node. (Figure 9). This causes a direct and indirect necrosis of the metastatic cells. Over a period the necrosed lymph node is reabsorbed (Figures 5, 6 and 7). The Radical neck dissection (RND) in late stages of Oral carcinoma has a high recurrence rate especially in enlarged lymph nodes [10]. The recurrence rates in stage 4 lesions are ranging from 30 to 70% [11, 12]. There is however no significant survival noted in the extent of RND [11]. On examining through the literature we could not find any reference as to the reason for recurrence after RND and nature of recurrence.
Our group postulated the reason for metastatic deposits as thus below
Removal of the lymphatic system by neck dissection leads to opening of afferent lymphatics and in presence of metastatic cells in the lymphatic vessels leads to a spillage in the neck spaces and leads to an implantation of metastatic cells. A good blood supply due to dissection in the operated areas leads to a growth of metastatic cells in the opened neck spaces. Recurrence rates are seen to be higher in clinically palpable lymph nodes. Various studies give figures from 20 to 30% [13]. Neck dissection in clinically enlarged lymph nodes may become the direct cause of metastatic deposits in the neck. These are mistakenly referred as lymph nodes. The difference can be made out by lack of capsule in these deposits on sonography.
2. Patients and Methods
46 patients were included in the study (Figure 2) The procedure was explained in detail to the patients. The procedure was carried out under General anaesthesia. All patients had a primary oral carcinoma which was handled by Laser Ablation. The PLALN was a part of the procedure. The lymph nodes were visualized under sonography control and an 18 No needle was manipulated percutaneously to the center of the lymph node (Figures 3, 8). The fiber was activated and the center of lymph node was laserised including the surrounding upto the capsule. Larger lymph nodes had laserisation upto and including the capsular area. The result was a hyperechogenic lymph node (Figure 11).
3. Results
All patients tolerated the procedure well. There was no intraoperative complications. 8 patients had a hematoma which was managed by compression. Most lymph nodes showed a full regression in 2 months (Figures 4-7). Results have shown that efficacy of the procedure is inversely proportional to the size of the lesion due to extracapsular spread in larger lymph nodes (Figure 3).
Demography of patients
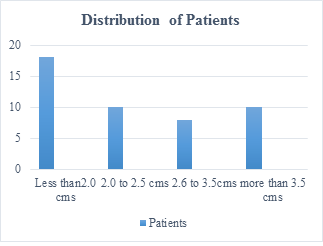
Figure 2: The distribution of patients with size of lymph nodes.
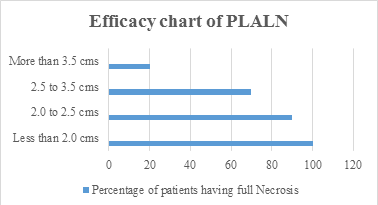
Figure 3: Percentage of patients having 100% necrosis grouped by size of Lymph Nodes Visualized on sonography after 4 weeks.

Figure 4: Lymph Node swelling with Arrow pointing to the swelling.

Figure 5: Arrow pinting to resoluton of Lymph Node. Oral deformity due to Laser ablation at angle of mouth involvement.
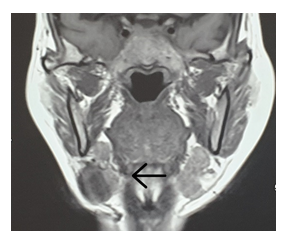
Figure 6: Arrow poining to Submandibular Lymph Node.
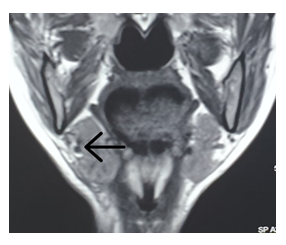
Figure 7: Arrow pointing to Total resolution of Swelling.

Figure 8: Needle with Laser fibre inside Lymph Node. Note round shape and lack of fatty hilum.
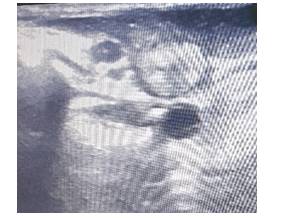
Figure 9: Post PLALN picture of Necrosed Lymph Node showing Hyperechogenecity ,seen after 2 weeks. The lymph Node is lying above Jugular vein.
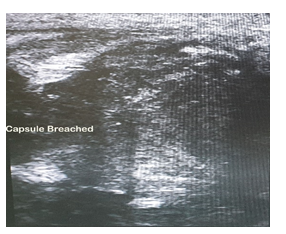
Figure 10: Large lymph node in neck showing breach of capsule.
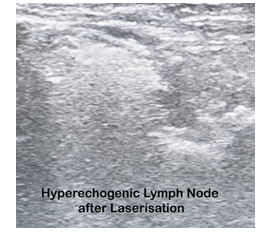
Figure 11: Hyperechogenic Lymph Node immediately after laserisation.
4. Discussion
With rapid development of imaging technology, Surgery is becoming more focused and minimal. Laser ablation is playing a very important part in this regard [1, 6, 14]. The most common methods used are Radiofrequency and laser for ablation techniques [7]. Laser ablation of lymph nodes is being practiced in select centers due to different skill sets requirements from conventional surgery. The laser destruction of tissue including tissue protein denaturation, coagulative necrosis, tissue liquefaction, vaporization, and carbonization occurs instantaneously [15]. Lymph node management especially in inaccessible or areas close to major vessels has always been difficult to treat with conventional surgery. Many studies have used Laser for Lymph nodes in neck for thyroid carcinoma and Mesentric lymph Nodes. The easy application of sonography and appropriate laser makes it a worthwhile alternative for inoperable patients. The results have been encouraging from all quarters. Presence of Lymph Node places the patient in stage 3. Enlarged lymphnode or multiple lymph nodes places the patient in stage 4 [16]. The ability to laserise the enlarged lymph nodes adds to the survival period of patients [4, 6, 7, 14, 17].
5. Conclusion
PLALN is a safe and viable procedure for accessible and inaccessible lymph nodes in Oral carcinoma. The procedure is predictable for smaller lymph nodes. The procedure has its advantages since the destruction can be done in real time. Earlier presentation is necessary for taking full advantage of the procedure in oral carcinoma. PLALN is a skilled procedure and requires a training in Interventional sonography.
Funding and Conflict of Interests
The authors declare that they have no funding and there is no conflicting interests.
References
- Radiation-Emitting Products, Surgical and Therapeutic Products, Medical Lasers. FDA (2020).
- Emiliano Schena, Paola Saccomandi and Yuman Fong. Laser Ablation for Cancer: Past, Present and Future. J Funct Biomater 8 (2017): 19.
- Pacella CM, Mauri G, Achille G, et al. Outcomes and Risk Factors for Complications of Laser Ablation for Thyroid Nodules: A Multicenter Study on 1531 Patients. The Journal of clinical endocrinology and metabolism 100 (2015): 3903-3910.
- Wu X, Zhou P, Ma S, et al. Ultrasound-guided laser thermal ablation for treatment of small liver cancer at high-risk sites. Nan fang yi ke da xue xue bao = Journal of Southern Medical University 36 (2016): 120-125.
- Mauri G, Cova L, Monaco CG, et al. Benign thyroid nodules treatment using Percutaneous Laser Ablation (PLA) and Radiofrequency Ablation (RFA). International journal of hyperthermia 33 (2017): 295-299.
- Rusy Bhalla, Seemantini Bhalla, Duleep Bhonsale, et al. Laser Ablation Surgery in Late Stage Buccal Cancer. Cancer and Oncology Research 6 (2020): 47-52.
- Machi J, Oishi AJ, Furumoto NL, et al. Sonographically guided radio frequency thermal ablation for unresectable recurrent tumors in the retroperitoneum and the pelvis. J Ultrasound Med 22 (2003): 507-513.
- Jiang T, Deng Z, Tian G, et al. Percutaneous laser ablation: a new contribution to unresectable high-risk metastatic retroperitoneal lesions?. Oncotarget 8 (2017): 2413-2422.
- Jatin P Shah, Ziv Gil. Current Concepts In Management Of Oral Cancer-Surgery. Oral Oncol 45 (2009): 394-401.
- Lim JY, Lim YC, Kim SH, et al. Factors predictive of successful outcome following salvage treatment of isolated neck recurrences. Otolaryngol Head Neck Surg 142 (2010): 832-837.
- Andersen PS, Chakera AH, Thamsborg AK, et al. Recurrence and survival after neck dissections in cutaneous head and neck melanoma. Dan Med J 61 (2014): A4953.
- Jones AS, Tandon S, Helliwell TR, et al. Survival of patients with neck recurrence following radical neck dissection: utility of a second neck dissection? Head Neck 30 (2008): 1514-1522.
- Wang B, Zhang S, Yue K, et al. The recurrence and survival of oral squamous cell carcinoma: a report of 275 cases. Chin J Cancer 32 (2013): 614-618.
- Mauri G, Cova L, Tondolo T, et al. Percutaneous laser ablation of metastatic lymph nodes in the neck from papillary thyroid carcinoma: preliminary results. J Clin Endocrinol Metab 98 (2013): 1203-1207.
- Ehsan Azma and Nassimeh Safavi. Diode Laser Application in Soft Tissue Oral Surgery Ehsan Azma and Nassimeh Safavi. J Lasers Med Sci 4 (2013): 206-211.
- Neukam FW, Stelzle F. Laser tumor treatment in oral and maxillofacial surgery. Physics Procedia 5 (2010): 91-100.
- Oral Cavity and Oropharyngeal Cancer Stages. Early Detection, Diagnosis, And Staging. Cancer (2021).
- Pacella CM, Francica G, Di Lascio FM, et al. Long-term outcome of cirrhotic patients with early hepatocellular carcinoma treated with ultrasound-guided percutaneous laser ablation: a retrospective analysis. Journal of clinical oncology 27 (2009): 2615-2621.
