Young South Asian Women with ST Elevation Myocardial Infarction (STEMI)-Should we be Worried?
Article Information
Salik ur Rehman1*, Aisha Siddiqui2, Aysha Almas3, Aamir Hameed Khan4
1MBBS, FCPS (Cardiology) Instructor, Adult Cardiology, Aga Khan University Hospital, Karachi, Pakistan
2MBBS, Medical officer, Section of Internal Medicine, Department of Medicine, Aga Khan University Hospital, Karachi, Pakistan
3MBBS, MSc Clinical Research, FCPS (Medicine), FACP, PhD (Medical science), Karolinska Institutet, Associate professor of Medicine, Department of Medicine, Aga Khan University Hospital, Karachi, Pakistan
4MBBS, FCPS (Medicine and Cardiology), Professor of Cardiology, Service line Chief, Section of Adult Cardiology, Aga Khan University Hospital, Karachi, Pakistan
*Corresponding author: Salik ur Rehman, MBBS, FCPS (Cardiology) Instructor, Adult Cardiology, Aga Khan University Hospital, Karachi, Pakistan.
Received: 14 February 2022; Accepted: 21 February 2022; Published: 08 March 2022
Citation: Salik ur Rehman, Aisha Siddiqui, Aysha Almas, Aamir Hameed Khan. Young South Asian Women with ST Elevation Myocardial Infarction (STEMI)-Should We Be Worried?. Cardiology and Cardiovascular Medicine 5 (2022): 83-91.
View / Download Pdf Share at FacebookAbstract
Background and Objective: Young women with STEMI fare worse than men. Data for such patients in particular South Asians (SA) is sparse. Therefore, this study explored the common risk factors, angiographic features and outcomes in these patients.
Methods: It was a cross-sectional study done from 2013-2019 on female STEMI patients <45 years who underwent Coronary Catheterization and revascularization at Aga Khan University Hospital, Pakistan. Subjects with revascularizations or MI were excluded.
Results: From a total of 1575 STEMI patients, only 26 (1.6%) were young women. Mean age was 41.2 (+3.5) years and mean BMI was 27.4 (+5.1) kg/m2. Half of the patients were diabetic (n=14) or obese (n=13). Positive family history or history of HTN was seen in a third and smoking in none. Median LDL was 135.5 mg/dl and mean total cholesterol was 203 mg/dl. More than half (56%) patients presented with Anterior STEMI and PCI was the commonest mode of revascularization. Majority, (82%, n=19) had Single vessel disease with lesions in Left Anterior Descending (LAD). Proximal LAD lesions required stents 27.6 (+10) mm long and 3.0 (+0.4) mm wide on average. Mortality was seen in one patient. A third of patients (n=9) presented with heart failure whereas a quarter (n=7) with hypotension. A minority required mechanical ventilation, Cardiopulmonary resuscitation or temporary pacemaker.
Conclusions: STEMI is relatively uncommon in young SA women. Associated risk factors are Diabetes, obesity and positive family history. SVCAD with LAD involvement is the most common pattern. Rates of mortality, heart failure admissions or repeat revascularizations are minimal.
Keywords
Adult; Asians; Coronary Angiography; Outcome Measures; ST Elevation Myocardial Infarction; Women
Adult articles; Asians articles; Coronary Angiography articles; Outcome Measures articles; ST Elevation Myocardial Infarction articles; Women articles
Article Details
1. Introduction
Ischemic Heart Disease (IHD) is the single most important cause of death globally, surpassing nearly 9 million deaths in 2016 according to the World Health Organization (WHO) [1] Still, nearly three-quarter of cardiovascular deaths occur in Low- And Middle-Income Countries (LMIC) mainly because of insufficient health facilities and poverty delaying identification and treatment [2] Although elder age and male gender are usually associated to Coronary Artery Disease (CAD) and the data for this population is vast, recent studies have indicated increasing proportion of Myocardial Infarction (MI) related hospitalizations in young patients over previous years, especially among women along an increasing prevalence of Hypertension (HTN) and Diabetes Mellitus (T2DM) [3]. Heart disease is the leading cause of death for women in the United States accounting for every 1 in 4 deaths [4] Young women are sometimes the sole bread winners of their families or are in their childbearing years and the effect of MI at such a young age can be devastating. Moreover, compared to men, young women have longer length of stays and greater in-hospital mortality in addition to more comorbidities [5, 6]. The Nationwide Inpatient Sample Database study of young adults with STEMI from 2004 to 2011 in the United States states that young women are less likely to undergo coronary angiography or revascularization, and experience significant delays in getting treatment if compared to young men. Despite adjustment for socio-demographics, comorbidities, and clinical factors, these differences persist [7]. Few studies have explored the clinical characteristics and outcomes of young women in SA population and therefore more information is required. Studies have suggested in-hospital mortality rates as high as 6.5% in young SA women with ST elevated MI [8] In Pakistan, a significant proportion of women are under educated and tend to get married at an early age. Previous data shows that CV risk factors become prominent at an early age and lack of awareness awareness about how to control these risk factors aids disease development and propgression. Other contributory factors are under recognition of CVD due to atypical symptoms and dependence on males for access to health care. Therefore, this study aimed to look at the burden of risk factors, disease patterns and outcomes in this patient subgroup.
2. Methods
This observational study was conducted at the Aga Khan University Hospital (AKUH), Karachi, Pakistan from January 2013 to June 2020. All patients between 18 to 45 years of age with their first presentation as STEMI underwent Coronary Angiography (CAG) with/without attempt to Percutaneous Coronary Intervention (PCI) and were recruited. ICD diagnosis codes 140.0-140.6 were used to collect data on these patients using Data were collected using Health Information Management System (HIMS). Patients with prior MI or revascularization were excluded. Ethical exemption from Ethical Review Committee (ERC) at AKUH was obtained (ERC number 5438-Med-ERC-18). Data was gathered for comorbids, outcomes, and coronary disease patterns on a pre-designed proforma. Data for comorbids included obesity, diabetes, HTN, smoking, family history of Premature Coronary Artery Disease (FHx-PMCAD) and lipid profiles. On the basis of HbA1c, patients were grouped as pre-diabetics (5.7-6.4%) or as diabetics (>6.5%) [9] FHx-PMCAD was deemed positive if a parent, sibling, or a first-degree relative had CAD (males <55 years and females <65 years ) or a history of sudden cardiac death (SCD)[10] Patients with known HTN on antihypertensive drugs or those with peristent readings >140/90 mmHg were grouped as hypertensives [11]. Former/current smoker or who used chewable tobacco were counted as positive .12 Patients with a BMI of >27.5 kg/m2 or between 23-27.5 kg/m2 were considered as obese or overweight respectively as per the Asian cut-off values [13] With ACS, LDL-C levels >150 mg/dl and LDL-C/HDL-C ratio >2.7 correlate well with increased risk of stent thrombosis, target lesion revascularization, and MACE, hence these values were considered elevated on presentation [14, 15].
At out center, Coronary Angiograms (CAG) are interpreted by at least one expert interventional cardiologist. Eyeballing method (visual estimation) is done to quantify the nature and length of the lesion. Vessels stenoses >50% were counted as diseased while those <50% was classified as non-obstructive [16]. Disease was classified as one vessel disease (SVCAD), two-vessel disease (2VCAD), or three vessel disease (3VCAD). Each vessel was sub-classified as either a proximal or mid to distal disease with respect to origin of (major branches) first septal for Left Anterior Descending (LAD), Right ventricular marginal (RV marginal) in case of Right Coronary Artery (RCA), and first Obtuse Marginal (OM1) in case of the Left Circumflex (LCx). Patients were followed for a mean duration of 3.8 (+2.5) years and were evaluated for short and long term mortality, heart failure, stroke, Cardiogenic shock, need for Cardiopulmonary Resuscitation (CPR) or mechanical ventilation during the clinical course and need for repeat revascularization after the indexed hospital admission. Patients who were lost to follow up were called and enquired about their well-being. Contact with 3 patients was not possible.
3. Results
In our study, of 1575 patients presenting with STEMI from January 2013 to June 2020, there were only 26 (1.6%) young female patients presenting with STEMI over the course of 6.5 years. Mean age was 41.2 (+3.5) years. More than half of patients were diabetic (n=14, 54%) whereas a significant number of the remiander had pre-diabetess. Mean BMI was 27.4 (+5.1) kg/m2 and half of the patients (n=13, 50%) were obese with BMI >27.5 kg/m2 as per the SA cutoff for increased risk.. FHx-PMCAD was seen in more than a third (n=10, 38.4%) patients, HTN in 9 patients and smoking in none. (Table 1).
|
Comorbids |
Values |
|
Glycemic dysregulation: (n=19, 73%) |
Prediabetes: 5 (19.2%) patients |
|
Diabetes: 14 (54%) patients | |
|
Mean HbA1C: 7.9 (+2.4) | |
|
Elevated BMI:* |
BMI >27.5 kg/m2: 13 (50%) patients |
|
BMI between 23-27.5 kg/m2: 8 (31%) patients | |
|
Mean BMI (kg/m2): 27.4 (+5.1) | |
|
Positive family history: |
10 (38.4% ) patients |
|
Lipids (mg/dl)** |
Mean total cholesterol: 203 (+44) |
|
Median LDL: 144 (+47) | |
|
Mean HDL was 44.5 (+11.5) | |
|
Hypertension: |
9 (34%) patients |
|
Tobacco use: |
None |
|
*South Asian cutoff values **Values were missing for 8 patients | |
Table 1: Co-morbid conditions prevalent in young females with STEMI.
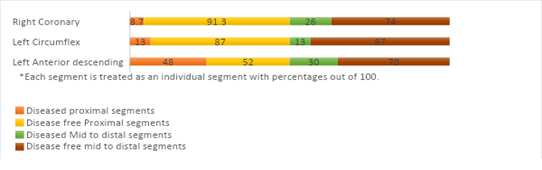
More than half of the patients (n=14, 54%) presented with STEMI involving the anterior territory. Left anterior descending was the most diseased vessel (n=20, 77%) including culprit and non-culprit lesions and was the most common non-culprit vessel. Nearly half (n=12, 46%) of the patients presented with inferior, inferio-lateral or inferio-posterior STEMI with 4 patients presenting with RV infarct. RCA was diseased in 9 (34.6%) patients followed by LCx involvement in only 2 patients. The most common diseased segment was Proximal LAD. Further details of segment wise disease distribution can be seen in (figure 1). Majority of young females (n=20, 76.9%) had SVCAD while Multivessel Disease (MVD) was seen in nearly a quarter (n=6, 23%) patients. Of those with MVD, only one patient each underwent multivessel PCI or CABG. The remainder either had borderline non-culprit disease or refused multivessel PCI after culprit PCI due to financial constraints. Proximal LAD lesions required stents 27.6 (+10) mm long and 3.0 (+0.4) mm wide on average. Mid or distal LAD lesions required stents as long as 21.7 (+4.7) mm or as wide as 2.4 (+0.3) mm. Mortality was seen in one only patient. A third of patients (n=9, 34%) presented with heart failure symptoms requiring diuretics on arrival whereas more than a quarter (n=7, 27%) were hypotensive requiring vasopressors. Four patients required mechanical ventilation whereas 2 patients each required Cardiopulmonary resuscitation or temporary pacemaker. Only one patient developed VT/VF during the clinical course. During the mean follow-up of 3.8 (+2.5) years, there were no additional mortalities, heart failure hospitalizations, repeat revascularizations or need for Cardiovascular Implantable Electronic Device. Only one patient developed anginal symptoms who was optimized on medical therapy.
4. Discussion
This study describes the clinical characteristics, angiographic features and outcomes of young women with AMI in Pakistani population. In our study, young women made up only 1.6% (n=26) patients presenting with STEMI. Interestingly, T2DM was the most common risk factor followed by obesity and FHx-PMCAD. The primary reperfusion strategy was PCI. SVCAD involving the LAD was the most common pattern. Overall prognosis was favorable. Studies have labelled patients aged <45 years as young as they have less co-morbids and better prognosis [17] However, contrary to older patients, young patients have not had equivalent reductions in Acute MI (AMI) hospitalizations with prognosis unfavorable with regards to young women. Women have higher mortality and rates of heart failure emphasizing the need to address certain risk factors and coronary lesions effecting outcomes [18] In developed countries, young women usually present at mean ages of 40.7+3.7 years with Acute Coronary Syndrome (ACS) which is not much different from other studies done in SA population are more likely to be smokers, have HTN and FHx-PMCAD with high percentages of dyslipidemia [5, 6, 8] However, these patterns differ in an LMIC where tobacco use is strikingly low (6% for young Pakistani women) and an emphasis on smoking cessation stands less relevant [8, 19] Conversely, T2DM was found to be the most prevalent risk factor in our study which is also endorsed by other SA studies [8] Also SA women have clustering of multiple CAD risk factors including obesity [19] However, data specific for young SA women is sparse. Both T2DM and obesity are potential modifiable risk factors and can play an important role in reducing cardiovascular risk. In addition, a family history of PMCAD is an independent risk factor and also correlates to disease complexity [20] In developed countries, as high as 40% of young women with CAD may have a FHx-PMCAD [5]. These results are also comparable to our study. Dysfunctional and lower levels of HDL-C or higher Lipoprotein (a) concentrations can be responsible for this [20] Also, a significant proportion of these women are hypertensive creating room for further risk factor modification. In Pakistan, prevalence of HTN in women is slightly greater than males which can be attributed to lack of physical activity, dietary patterns, and higher BMI and limited resources for health related issues.5, 8 In addition, abnormal lipid parameters in the setting of ACS such as LDL-C levels >150 mg/dl predict microvascular injury (due to increased inflammation as well as endothelial dysfunction) [14]. Similarly, higher LDL-C/HDL-C ratio i.e. >2.7 during ACS correlates with adverse outcomes [15] However specific data pertaining to young women are still under-explored.
Young women with ACS seldom have multivessel disease, coronary calcification or ostial lesions but they still have predilection of significant CAD in the LAD.5 However, when compared to age matched men, there are not many gender related differences except that young women are less likely to have multivessel or left main bifurcation disease. The commonest pattern is SVD with LAD involvement with a significant number with normal or non-obstructive patterns [21] Despite the similarities, mortality rates are higher in women. This highlights the idea that factors such as lower coronary flow reserve, functional differences in smooth muscle function in the vessel wall and vascular stiffness might contribte to adverse outcomes [22]. In our study, none of the patients had non-obstructive coronaries and only a minority had MVD. Unlike men, rates of AMI and hospital admissions have increased in young women and young age does not provide protection. Even after adjustment for guideline-directed medications or revascularization, young women have adverse short term outcomes. However, the trend for mortality has declined but women still tend to have longer in-hospital stays. In-hospital mortality rates of as high as 2.3% can be observed in developed countries [6]. Other than reasons such as lack of or atypical symptoms and increased total ischemic time, attributable reasons that seem responsible for this paradox appear to be differences in comorbids (e.g. T2DM and depression, both known to be associated to adverse prognosis in young women but not elder women) and coronary anatomy (small vessel caliber, vascular stiffness and less atherosclerosis leading to less preconditioning and collaterals) [23] Poor outcomes such as Cardiogenic Shock (CS) can be associated to atypical symptoms and delayed diagnosis. Although women with CS derive the same benefit from revascularization as men, they are more likely to have adverse clinical characteristics and mechanical complications [24] Studies show that women are less likely to present with Ventricular fibrillation (VF) or Sudden Cardiac Death (SCD) and are less likely to receive out-of-hospital cardiopulmonary resuscitation [25]. However, when compared with an equal proportion of men with SCA, women have a tendency for poorer prognosis in the setting of STEMI. In developed countries, young women also have longer lengths of stay averaging about 4 days from admission and have increased overall repeat hospitalizations for all causes [18] Data from developing countries is sparse.
5. Strengths and Limitations
To the best of our knowledge, this is one of the few studies focusing on outcomes of young SA women presenting with STEMI. However, there are several limitations. The study was able to recruit only a small number of patients due to rarity of this disease in this age group. The study was single-centered and the results may not be generalizable. We did not address other confounders like dietary patterns, medications and exercise status. A significant amount of data on lipid profiles was not available. We did not address the non-traditional risk factors which might also play an important role in PMCAD. Further studies pertaining to young women with ACS are required recruiting a larger sample size and addressing these limitations.
6. Conclusion
In conclusion, young SA women rarely present with STEMI. T2DM, obesity and positive FHx-PMCAD are common risk factors. LAD is the most common and most frequent vessel involved. The prognosis is overall favorable with minimum rates of short and long term mortality, CPR, mechanical ventilation and long-term need of heart failure hospitalizations or repeat revascularizations.
Funding statement
There was no funding involved in this study in regards to data collection and analysis, decision to publish, or preparation of the manuscript.
Conflict of Interest
None.
Disclosure
Nothing to disclose
References
- Nowbar AN, Gitto M, Howard JP, et al. Mortality From Ischemic Heart Disease. Circulation Cardiovascular quality and outcomes 12 (2019): 005375.
- World Health Organization. Cardiovascular diseases (CVDs) 17 May 2017.
- Arora S, Stouffer GA, Kucharska-Newton AM, et al. Twenty Year Trends and Sex Differences in Young Adults Hospitalized With Acute Myocardial Infarction. Circulation 139 (2019): 1047-1056.
- Kochanek KD, Xu J, Murphy SL, et al. Deaths: preliminary data for 2009. National vital statistics reports : from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System 59 (2011): 1-51.
- Ricci B, Cenko E, Vasiljevic Z, et al. Acute Coronary Syndrome: The Risk to Young Women. Journal of the American Heart Association 6 (2017).
- Gupta A, Wang Y, Spertus JA, et al. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. Journal of the American College of Cardiology 64 (2014): 337-345.
- Khera S, Kolte D, Gupta T, et al. Temporal Trends and Sex Differences in Revascularization and Outcomes of ST-Segment Elevation Myocardial Infarction in Younger Adults in the United States. Journal of the American College of Cardiology 66 (2015): 1961-1972.
- Venkatason P, Zubairi YZ, Zaharan NL, et al. Characteristics and short-term outcomes of young women with acute myocardial infarction in Malaysia: a retrospective analysis from the Malaysian National Cardiovascular Database registry. BMJ Open 9 (2019): 030159.
- American Diabetes A. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2020. Diabetes Care 43 (2020): 14-31.
- Cohen R, Budoff M, McClelland RL, et al. Significance of a positive family history for coronary heart disease in patients with a zero coronary artery calcium score (from the Multi-Ethnic Study of Atherosclerosis). Am J Cardiol 114 (2014): 1210-1214.
- Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report JAMA 289 (2003): 2560-2572.
- Barua RS, Rigotti NA, Benowitz NL, et al. 2018 ACC Expert Consensus Decision Pathway on Tobacco Cessation Treatment: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. Journal of the American College of Cardiology 72 (2018): 3332-3365.
- Consultation WHOE. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 363 (2004): 157-163.
- Reindl M, Reinstadler SJ, Feistritzer HJ, et al. Relation of Low-Density Lipoprotein Cholesterol With Microvascular Injury and Clinical Outcome in Revascularized ST-Elevation Myocardial Infarction. Journal of the American Heart Association 6 (2017).
- Zhong Z, Hou J, Zhang Q, et al. Assessment of the LDL-C/HDL-C ratio as a predictor of one year clinical outcomes in patients with acute coronary syndromes after percutaneous coronary intervention and drug-eluting stent implantation. Lipids Health Dis 18 (2019): 40.
- Rosenthal RL. The 50% coronary stenosis. Am J Cardiol 115 (2015): 1162-1165.
- Gulati R, Behfar A, Narula J, et al. Acute Myocardial Infarction in Young Individuals. Mayo Clin Proc 95 (2020): 136-156.
- Wilmot KA, O'Flaherty M, Capewell S, et al. Response to Letter Regarding Article, "Coronary Heart Disease Mortality Declines in the United States From 1979 Through 2011: Evidence for Stagnation in Young Adults, Especially Women". Circulation 133 (2016): 433.
- Pakistan Health Research Council. Non-Communicable Diseases Risk Factors Survey - Pakistan 2016.
- Yusuf S, Hawken S, Ounpuu S, et al. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet 364 (2004): 937-952.
- Ezhumalai B, Jayaraman B. Angiographic prevalence and pattern of coronary artery disease in women. Indian heart journal 66 (2014): 422-426.
- Handberg E, Johnson BD, Arant CB, et al. Impaired coronary vascular reactivity and functional capacity in women: results from the NHLBI Women's Ischemia Syndrome Evaluation (WISE) Study. Journal of the American College of Cardiology 47 (2006): 44-49.
- Cenko E, Yoon J, Kedev S, et al. Sex Differences in Outcomes After STEMI: Effect Modification by Treatment Strategy and Age. JAMA internal medicine 178 (2018): 632-639.
- Wong SC, Sleeper LA, Monrad ES, et al. Absence of gender differences in clinical outcomes in patients with cardiogenic shock complicating acute myocardial infarction. A report from the SHOCK Trial Registry. Journal of the American College of Cardiology 38 (2001): 1395-1401.
- Blewer AL, McGovern SK, Schmicker RH, et al. Gender Disparities Among Adult Recipients of Bystander Cardiopulmonary Resuscitation in the Public. Circulation Cardiovascular quality and outcomes 11 (2018): 004710.