Wound Management in Gynaecological Surgery: A Tertiary Care Hospital Study in Bangladesh
Article Information
Sabrin Farhad1*, Bipul Kumar Biswas2, Shamima Haque Chowdhury3, Roknuzzman4
1Assistant Professor, Department of Obstetrics and Gynaecology, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
2Assistant Professor, Department of Gynecology and Obstetrics, Kustia Medical College Hospital, Kustia, Bangladesh
3Professor, Head of Department, Department of Obstetrics and Gynaecology, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
4Registrar, Department of Surgery, Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
*Corresponding Author: Dr. Sabrin Farhad, Assistant Professor, Department of Obstetrics and Gynaecology,
Uttara Adhunik Medical College and Hospital, Dhaka, Bangladesh
Received: 22 March 2022; Accepted: 18 April 2022; Published: 02 May 2022
Citation: Sabrin Farhad, Bipul Kumar Biswas, Shamima Haque Chowdhury, Roknuzzman. Wound Management in Gynaecological Surgery: A Tertiary Care Hospital Study in Bangladesh. Obstetrics and Gynecology Research 5 (2022): 122-130.
View / Download Pdf Share at FacebookAbstract
Background: Wound infection is one of the most prevalent problems associated with surgical therapy, accounting for a large amount of morbidity in gynae-cologic surgical hospitalizations. To avoid potential problems like surgical-site infections and wound dehi-scence, it's critical to care for post-operative wounds properly in the community.
Objective: The objective of the study was to assess the prevalence of wound infection and its management system in gynecological surgery in a tertiary care hospital in Bangladesh.
Method: This cross-sectional study was conducted from January 2019 to December 2020 at Uttara Adhu-nik Medical College & Medical College Hospital, Dhaka, Bangladesh. This study was purposively con-ducted among 220 female patients who were admitted to the obstetrics & gynaecology department with gyn- aecological wounds & their infections.
Results: Among 220 patients, 12.7% of patients were below 20 years old and the maximum number of patients (46.3%) were between 20 to 29 years old. 60% of patients’ socioeconomic status was a middle-class state. The rate of antibiotic prophylaxis was higher (31%) in combined surgery patients, length of hospital stay was higher among vaginal surgery patients, rehos-pitalization was observed higher (29%) among abdo-minal surgery patients, and most repeated surgeries were found to be higher (24%) in abdominal surgery patients. Maximum patients (31.8%) had hypertension and minimum patients (3.86%) had fever on admis-sion. Maximum patients (33%) had operative site infection and minimum patients (6%) had post-operative ileus.
Conclusion: Optimal surgical wound management is a crucial component of post-operative recovery, and health care practitioners should keep an eye on the progress of acute wound healing, prevent wound problems, and treat them correctly if they occur.
Keywords
Wound Management, Gynecological, Tertiary Care Hospital
Wound Management articles Wound Management Research articles Wound Management review articles Wound Management PubMed articles Wound Management PubMed Central articles Wound Management 2023 articles Wound Management 2024 articles Wound Management Scopus articles Wound Management impact factor journals Wound Management Scopus journals Wound Management PubMed journals Wound Management medical journals Wound Management free journals Wound Management best journals Wound Management top journals Wound Management free medical journals Wound Management famous journals Wound Management Google Scholar indexed journals Gynecological articles Gynecological Research articles Gynecological review articles Gynecological PubMed articles Gynecological PubMed Central articles Gynecological 2023 articles Gynecological 2024 articles Gynecological Scopus articles Gynecological impact factor journals Gynecological Scopus journals Gynecological PubMed journals Gynecological medical journals Gynecological free journals Gynecological best journals Gynecological top journals Gynecological free medical journals Gynecological famous journals Gynecological Google Scholar indexed journals Tertiary Care Hospital articles Tertiary Care Hospital Research articles Tertiary Care Hospital review articles Tertiary Care Hospital PubMed articles Tertiary Care Hospital PubMed Central articles Tertiary Care Hospital 2023 articles Tertiary Care Hospital 2024 articles Tertiary Care Hospital Scopus articles Tertiary Care Hospital impact factor journals Tertiary Care Hospital Scopus journals Tertiary Care Hospital PubMed journals Tertiary Care Hospital medical journals Tertiary Care Hospital free journals Tertiary Care Hospital best journals Tertiary Care Hospital top journals Tertiary Care Hospital free medical journals Tertiary Care Hospital famous journals Tertiary Care Hospital Google Scholar indexed journals urinary retention articles urinary retention Research articles urinary retention review articles urinary retention PubMed articles urinary retention PubMed Central articles urinary retention 2023 articles urinary retention 2024 articles urinary retention Scopus articles urinary retention impact factor journals urinary retention Scopus journals urinary retention PubMed journals urinary retention medical journals urinary retention free journals urinary retention best journals urinary retention top journals urinary retention free medical journals urinary retention famous journals urinary retention Google Scholar indexed journals urinary tract articles urinary tract Research articles urinary tract review articles urinary tract PubMed articles urinary tract PubMed Central articles urinary tract 2023 articles urinary tract 2024 articles urinary tract Scopus articles urinary tract impact factor journals urinary tract Scopus journals urinary tract PubMed journals urinary tract medical journals urinary tract free journals urinary tract best journals urinary tract top journals urinary tract free medical journals urinary tract famous journals urinary tract Google Scholar indexed journals postoperative articles postoperative Research articles postoperative review articles postoperative PubMed articles postoperative PubMed Central articles postoperative 2023 articles postoperative 2024 articles postoperative Scopus articles postoperative impact factor journals postoperative Scopus journals postoperative PubMed journals postoperative medical journals postoperative free journals postoperative best journals postoperative top journals postoperative free medical journals postoperative famous journals postoperative Google Scholar indexed journals hemostasis articles hemostasis Research articles hemostasis review articles hemostasis PubMed articles hemostasis PubMed Central articles hemostasis 2023 articles hemostasis 2024 articles hemostasis Scopus articles hemostasis impact factor journals hemostasis Scopus journals hemostasis PubMed journals hemostasis medical journals hemostasis free journals hemostasis best journals hemostasis top journals hemostasis free medical journals hemostasis famous journals hemostasis Google Scholar indexed journals public health articles public health Research articles public health review articles public health PubMed articles public health PubMed Central articles public health 2023 articles public health 2024 articles public health Scopus articles public health impact factor journals public health Scopus journals public health PubMed journals public health medical journals public health free journals public health best journals public health top journals public health free medical journals public health famous journals public health Google Scholar indexed journals healthcare system articles healthcare system Research articles healthcare system review articles healthcare system PubMed articles healthcare system PubMed Central articles healthcare system 2023 articles healthcare system 2024 articles healthcare system Scopus articles healthcare system impact factor journals healthcare system Scopus journals healthcare system PubMed journals healthcare system medical journals healthcare system free journals healthcare system best journals healthcare system top journals healthcare system free medical journals healthcare system famous journals healthcare system Google Scholar indexed journals gynecological surgery articles gynecological surgery Research articles gynecological surgery review articles gynecological surgery PubMed articles gynecological surgery PubMed Central articles gynecological surgery 2023 articles gynecological surgery 2024 articles gynecological surgery Scopus articles gynecological surgery impact factor journals gynecological surgery Scopus journals gynecological surgery PubMed journals gynecological surgery medical journals gynecological surgery free journals gynecological surgery best journals gynecological surgery top journals gynecological surgery free medical journals gynecological surgery famous journals gynecological surgery Google Scholar indexed journals
Article Details
1. Introduction
Surgical operations involving the female genital tract are handled by gynaecological surgery services. It also addresses the breasts and pelvic, as well as operations involving the uterus, its appendages, and urinary incontinence repair [1]. Hysterectomy is the most common gynecological procedure; others include tubal ligation, curettage, cystectomy, and salpingec-tomy [1, 2]. Every surgery has a risk of complications; prognosis depends on prompt diagnosis and timely management [3]. Gynaecological surgeries can be diverse and include surgical site infections (SSIs), fever, upper respiratory infections (URI), urinary rete-ntion, urinary tract infections (UTI), and abdominal distension [4]. In such cases surgical site infections account for 0.5% to 15% of the total postoperative complications as most commonly encountered ones [5]. According to the WHO (World Health Organi-zation report, it complicates 11.8 out of 100 surgical procedures in low as well as middle-income countries [6]. Acute wounds usually progress through an orderly sequential trajectory of hemostasis, maturation, proli-feration, and remodeling [7]. After initial dermal tissue injury, hemostasis by platelet aggregation, fibrin clot formation, and subsequent coagulation pathways [8]. Early detection of wound complications is crucial to improving patients’ quality of life and reducing hospital readmission [9]. In such cases, if antibiotic therapy is commenced, it should be administered based on the most likely causative organisms as well as the patient’s allergy status, with consideration of local antibiotic resistance [10]. Cleaning of wounds can be performed with potable tap water [11]. Applic-ation of local dressings depends upon the wound characteristics and dressing features, like absorption capacity, adherence, and even cost-effectiveness [12].
A complication is an unintended consequence of surg-ery that has an adverse effect on the patient and would not have occurred if the surgery had been completed according to the procedures [13-15]. Many microbes (germs) reside in and on our bodies, as well as in our surroundings. Our bodies have built-in defenses again-st potentially harmful pathogens. Germs can penetrate the incision that a surgeon creates through the skin during an operation, causing a surgical wound infect-ion. Unintentional or involuntary activities might result in an incident, which is defined as an event or scenario that could have caused or caused unnecessary harm [14, 15]. Surgical complications are a significant issue from a clinical, legal, and public health stand-point because of the financial burden they place on the healthcare system. Surgical problems in gynecological surgery are more common in some populations than others. The result of surgery is influenced by socio-demographic factors, comorbidities, medical history, indications for the procedure, and the surgeon's experience [16]. Because the danger of complications rises with the complexity of the surgical process and the surgeon's experience, accumulating surgical experience combined with preventative procedures can greatly minimize the rate of complications [17].
When compared to laparoscopic, abdominal, and vaginal hysterectomy, patients undergoing robotic-assisted laparoscopic hysterectomy have a signifi-cantly lower risk of re-admission; additionally, the robotic technology has a lower rate of hospital stay and generates less bleeding, according to Martino et al. [18]. Surgical site infections are the most prevalent complication, occurring between 2.2 % and 10% of the time [19, 20], followed by transfusion (4%), pelvic abscesses (1.5%), reoperation (2%), and wound dehiscence (2%) [20]. Wound infection is one of the most prevalent problems associated with surgical treatment of patients, accounting for 8-10% of gynaecologic surgical hospitalizations and causing significant morbidity. From time to time, strategies for preventing wound infections have been proposed [21]. Despite numerous revisions to the protocols for the preoperative, intraoperative, and postoperative mana-gement of the patient, the increased prevalence of wound gape in the postoperative period poses a significant challenge to gynecologists. Given that all tertiary care hospitals adhere to the same basic norms, a cross-sectional study was conducted to determine the prevalence of wound infection and its management system in the postoperative period.
1.1 Objective
The objective of the study was to assess the prevalence of wound infection and its management system in gynecological surgery in a tertiary care hospital in Bangladesh.
2. Materials and Methods
2.1 Type of study
A cross-sectional study.
2.2 Place of study
Uttara Adhunik Medical College & Medical College Hospital.
2.3 Period of study
January 2019 to December 2020.
2.4 Sample size
220 female Patients.
2.5 The procedure for collecting and analyzing data
Data were entered in the computer using SPSS (Statistical Package for Social Science) version 21.0. The level of significance was considered as a “P” value less than 0.05 and double-checked before analysis.
3. Results
Table 1 showed the demographic characteristics of the participants of the study. Among 220 patients, 28(12.7%) patients were below 20 years old and the maximum number of patients 102(46.3%) were between 20 to 29 years old. Their marital status, residence, live births, number of abortions are stated below. And 116(60%) patients’ socioeconomic status was a middle-class state. Table 2 showed the status of the morbidity associated with wound infection. In our study, there were 3 types of surgeries classified among patients (Abnormal surgery, vaginal surgery, and combined surgery). The rate of antibiotic prophylaxis was higher (31%) in combined surgery patients, length of hospital stay was higher among vaginal surgery patients, rehospitalization was observed higher (29%) among abdominal surgery patients, and most repeated surgeries were found to be higher (24%) in abdominal surgery patients. Table 3 showed the status of the various coexisting risk factors in wound infection cases. Maximum patients (31.8%) had hypertension and minimum patients (3.86%) had fever on admission. Table 4 showed the hospital stay of the patients is shown. Here, maximum patients (39.4%) stayed 15-21 days. Minimum patients (1.7%) stayed below 7 days in the hospital. Figure IV shows the type of gynecological surgery complications. Here, maximum patients (33%) had operative site infection and minimum patients (6%) had postoperative ileus.
|
Variables |
n |
% |
|
Age group |
||
|
<20 yrs. |
28 |
12.7 |
|
20-29 yrs. |
102 |
46.3 |
|
30-39 yrs. |
48 |
21.8 |
|
40-49 yrs. |
24 |
11.0 |
|
≥ 50 yrs. |
18 |
8.2 |
|
Marital status |
||
|
Stable |
103 |
46.8 |
|
Unstable |
117 |
53.1 |
|
Residence |
||
|
Urban |
172 |
78.1 |
|
Rural |
48 |
21.8 |
|
Live Birth |
||
|
No deliveries |
87 |
39.5 |
|
At least one birth |
133 |
60.5 |
|
Abortions |
||
|
Yes |
39 |
17.7 |
|
No |
181 |
82.3 |
|
Socioeconomic state |
||
|
Lower Class |
48 |
34.3 |
|
Middle Class |
116 |
60.0 |
|
Upper Class |
56 |
5.7 |
Table 1: Demographic characteristics of the study population (N=220).
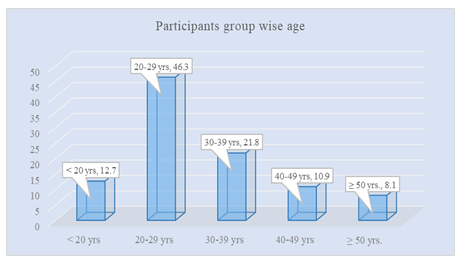
Figure 1: Participants Age-wise Group.
|
Variables |
Abdominal surgery |
Vaginal surgery |
Combined Surgery |
P-Value |
|
Antibiotic prophylaxis (%) |
21.0 |
17.0 |
31.0 |
0.071 |
|
Length of stay (Avg.) in days |
7 |
8 |
6 |
0.415 |
|
Rehospitalization |
29.0 |
17.0 |
9.0 |
0.082 |
|
Repeat surgery |
24.0 |
13.0 |
1.0 |
0.013 |
Table 2: Morbidity associated with wound infection (N=220).
|
Risks Factors |
% |
P-Value |
|
Nil |
53.2 |
0.544 |
|
Hypertension |
31.8 |
0.011 |
|
GDM/overt DM/IGT |
8.97 |
0.116 |
|
PROM |
6.63 |
0.968 |
|
Fever on admission |
3.86 |
0.231 |
Table 3: Various coexisting risk factors in wound infection cases.
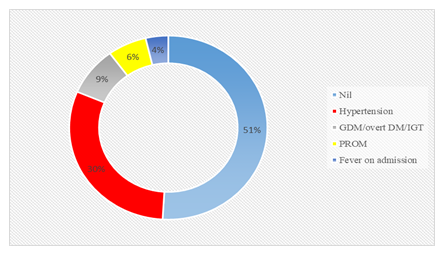
Figure 2: Various coexisting risk factors in wound infection cases.
|
Hospital stay (days) |
% |
P-value |
|
0-7 days |
1.7 |
0.432 |
|
8-14 days |
24.5 |
0.235 |
|
15-21days |
39.4 |
0.014 |
|
22-28 days |
31.5 |
0.117 |
|
29-35 days |
2.9 |
0.803 |
Table 4: Hospital stay for wound healing (N=220).
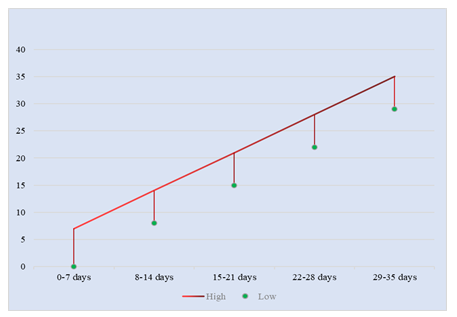
Figure 3: Hospital stay for wound healing.
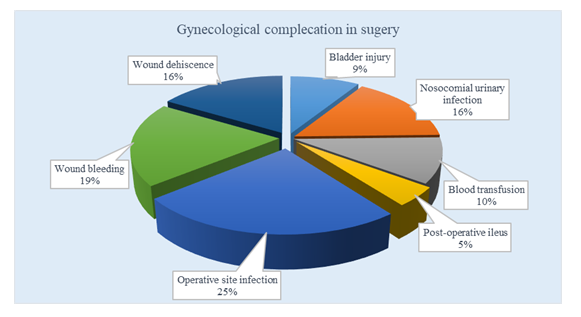
Figure 4: Type of gynecological surgery complications.
4. Discussion
One of the most common consequences of gynae-cologic surgery is wound infection. Its prevalence is linked to the highest rate of reoperation, the longest stay in the hospital, and the biggest cost rise of any postoperative gynaecologic complication [16]. Adeq-uate postoperative surgical wound care is critical for avoiding complications such as surgical-site infections (SSIs), wound dehiscence, and hematomas. General practitioners have a crucial role in managing patients' postoperative wounds in the community, and it's critical to understand the principles of postoperative wound treatment in order to reduce the risk of wound complications. The operating surgeon has a problem in the form of postoperative wound infection. The increasing occurrence of wound dehiscence has harmed the field of surgery's success in terms of developments in surgical methods and the easy availability of surgery as a therapy option. Wound healing is a complicated process that is influenced by both internal and environmental influences. Comor-bidities such as diabetes and hypertension are caused by internal factors. Wound infection, typical suturing procedures, suture materials, and wound care are examples of external variables. Preoperative prepara-tion, postoperative wound care, suture materials, and suturing methods or practice vary from one institute to the next. Varied institutes have different practices when it comes to changing dressings after surgery. The standard procedure is to replace the dressing on the second and third postoperative days. Wound cellulitis and seroma formation are the most common infections. These issues usually appear within the 3-5 postoperative days. Adequate assessment of postsu-rgical infectious morbidity necessitates meticulous follow-up of outpatient records and readmission tracking, which may not occur at the same facility as the main treatment. Antibiotic and antimicrobial prophylaxis for vaginal procedures has been shown to reduce infectious morbidity. Hemself et al. [22] found that only 8% of women undergoing vaginal hyster-ectomy who were administered cefoxitin developed the significant postoperative infection, compared to 57 percent of women who were given placebo in a prospective, randomized, double-blind research. Age, obesity, nutritional status, preoperative medical dis-orders like anemia, diabetes, jaundice, use of steroids, poor intraoperative preparation, emergency or elective surgeries, duration and type of surgeries, postoperative wound site contamination wound infection [18]. A careful examination and meticulous evaluation of the physiological requirements for wound healing will help you understand why certain wounds heal rapidly and others take longer [19]. Appropriate surgical attire and regular hand washing, as well as acceptable theater cleanliness, are thought to be important factors in avoiding infections, according to scientists. Regar-dless of the wound healing mechanism, the goals of post-operative wound care are to ensure that the wound heals quickly, without problems, and with the greatest functional and aesthetic results possible [19]. Wound borders should be well approximated in wounds that are intended to heal through primary healing.
5. Conclusion
Optimal surgical wound management is a crucial component of post-operative recovery, and health care practitioners should keep an eye on the progress of acute wound healing, prevent wound problems, and treat them correctly if they occur. The prompt asses-sment of the wound, adequate washing and dressing, and early diagnosis and intervention of wound comp-lications are all important aspects of postoperative wound management.
References
- Coelho SM, Perez Ede L, Lins CD, et al. Epidemiological profile and postoperative complications of women undergoing gynec-ological surgery in a reference center in the northern Brazilian legal amazon. Rev Col Bras Cir 42 (2015): 372-375.
- Barbosa G, Garnica L. Prevalencia de complicacionesy factores predisponentes en cirugía ginecológica por patología benigna en el hospital universitario San Ignacio: Bogotá, Colombia. Rev Chil Obstet Ginecol 80 (2015): 456-461.
- Ortiz-Martínez RA, Betancourt-Cañas AJ, Bolaños-Ñañez DM, et al. Prevalence of surgical complications in gynecological surgery at the Hospital Universitario San José in Popayán, Colombia. 2015. Rev. Fac. Med 66 (2018): 529-535.
- Bahadur A, Mundhra R, Kashibhatla J, et al. Intraoperative and Postoperative Compli-cations in Gynaecological Surgery: A Retrospective Analysis. Cureus 13 (2021): e14885.
- Bangal VB, Borawake SK, Shinde KK, et al. Study of surgical site infections following gynaecological surgery at tertiary care teaching hospital in rural India. Int J Biomed Res 5 (2014): 113-116.
- World Health Organization 2016: Global guidelines on the prevention of surgical site infection (2016).
- Barbul A. Wound healing. In: Brunicardi FC, Andersen DK, Billiar TR et al (eds) Schwartz’s principles of surgery, Eighthth edn. The McGraw-Hill Companies, Inc, Columbus (2005): 165-182
- Nicks BA, Ayello EA, Woo K, et al. Acute wound management: revisiting the approach to assessment, irrigation, and closure considerations. Int J Emerg Med 3 (2010): 399-407.
- Sinha Sankar. Management of post-surgical wounds in general practice. Australian journal of general practice 48 (2019): 596-599.
- Yao K, Bae L, Yew WP. Post-operative wound management. Aust Fam Physician 42 (2013): 867-870.
- Weiss EA, Oldham G, Lin M, et al. Water is a safe and effective alternative to sterile normal saline for wound irrigation prior to suturing: A prospective, double-blind, rand-omised, controlled clinical trial. BMJ Open 3 (2013): e001504.
- Ubbink DT, Brölmann FE, Go PM, et al. Evidence-based care of acute wounds: A perspective. Adv Wound Care (New Rochelle) 4 (2015): 286-294.
- Sokol DK, Wilson J. What is a surgical complication?. World J Surg 32 (2008): 942-944.
- Taylor-Adams S, Vincent C. System Anal-ysis of Clinical Incidents: The London Protocol. London: Clinical Safety Research Unit, Imperial College (2004).
- World Health Organization. Marco Concep-tual de la Clasificación Internacional para la Seguridad del Paciente. Informe Técnico Definitivo. WHO (2009).
- Erekson EA, Yip SO, Ciarleglio MM, et al. Postoperative complications after gyneco-logic surgery. Obstet Gynecol 118 (2011): 785-793.
- Tian YF, Lin YS, Lu CL, et al. Major complications of operative gynecologic laparoscopy in southern Taiwan: a follow-up study. J Minim Invasive Gynecol 14 (2007): 284-292.
- Martino MA, Berger EA, McFetridge JT, et al. A comparison of quality outcome meas-ures in patients having a hysterectomy for benign disease: robotic vs. non-robotic approaches. J Minim Invasive Gynecol 21 (2014): 389-393.
- Jaiyeoba O. Postoperative infections in obstetrics and gynecology. Clin Obstet Gyne-col 55 (2012): 904-913.
- Stany MP, Farley JH. Complications of gynecologic surgery. Surg Clin North Am 88 (2008): 343-359.
- Al Jama FE. Risk factors for wound infection after lower segment cesarean section. Qatar Med J 12 (2012): 26-31.
- Gruenigen Vivian, Coleman Robert, Li Andy, et al. Bacteriology and Treatment of Malodorous Lower Reproductive Tract in Gynecologic Cancer Patients. Obstetrics and gynecology 96 (2000): 23-27.
