Vital Signs Monitoring based on a Developed Accelerometer Sensor for Sporty Purposes
Article Information
Atefeh Valipour*, Keivan Maghooli
Department of Biomedical Engineering, Science and Research Branch, Islamic Azad University, Tehran, Iran
*Corresponding Author: Atefeh Valipour, Department of Biomedical Engineering, Science and Research Branch, Islamic Azad University, Tehran, Iran
Received: 14 June 2019; Accepted: 01 July 2019; Published: 08 July 2019
Citation: Atefeh Valipour, Keivan Maghooli. Vital Signs Monitoring based on a Developed Accelerometer Sensor for Sporty Purposes. Journal of Orthopaedics and Sports Medicine 1 (2019): 051-059.
View / Download Pdf Share at FacebookAbstract
This paper proposes developing a wireless sensor for heartbeat and respiration rate monitoring for the sportsman. The developed wireless sensor, includes an accelerometer sensor, a processor and a transceiver which operates in Industrial, Scientific and Medical (ISM) band and the frequency of 2.54 to connect with a central node for transmitting the measured data. In order to evaluate the accuracy of the presented sensor, the different experiments are carried out on several volunteers and the resultant data are compared to a gold standard for respiration rate and also heartbeat as a reference. As the outcomes illustrate, the root means square error (RMSE) and the standard deviation of the error (SD) are calculated less than 2.8 and 1.43 beats per minutes as well as 1.01 and 0.85 breaths per minutes for the heartbeat and respiration rate, respectively. Therefore, the sensor can account a good alternative for cardiorespiratory system monitoring for sporty application, due to low-cost, portable and also availability.
Keywords
Monitoring, Cardiorespiratory system, Motion sensor, Sportsman
Seismocardiogram articles Seismocardiogram Research articles Seismocardiogram review articles Seismocardiogram PubMed articles Seismocardiogram PubMed Central articles Seismocardiogram 2023 articles Seismocardiogram 2024 articles Seismocardiogram Scopus articles Seismocardiogram impact factor journals Seismocardiogram Scopus journals Seismocardiogram PubMed journals Seismocardiogram medical journals Seismocardiogram free journals Seismocardiogram best journals Seismocardiogram top journals Seismocardiogram free medical journals Seismocardiogram famous journals Seismocardiogram Google Scholar indexed journals Bloodstream articles Bloodstream Research articles Bloodstream review articles Bloodstream PubMed articles Bloodstream PubMed Central articles Bloodstream 2023 articles Bloodstream 2024 articles Bloodstream Scopus articles Bloodstream impact factor journals Bloodstream Scopus journals Bloodstream PubMed journals Bloodstream medical journals Bloodstream free journals Bloodstream best journals Bloodstream top journals Bloodstream free medical journals Bloodstream famous journals Bloodstream Google Scholar indexed journals Physical activity articles Physical activity Research articles Physical activity review articles Physical activity PubMed articles Physical activity PubMed Central articles Physical activity 2023 articles Physical activity 2024 articles Physical activity Scopus articles Physical activity impact factor journals Physical activity Scopus journals Physical activity PubMed journals Physical activity medical journals Physical activity free journals Physical activity best journals Physical activity top journals Physical activity free medical journals Physical activity famous journals Physical activity Google Scholar indexed journals Cardiovascular articles Cardiovascular Research articles Cardiovascular review articles Cardiovascular PubMed articles Cardiovascular PubMed Central articles Cardiovascular 2023 articles Cardiovascular 2024 articles Cardiovascular Scopus articles Cardiovascular impact factor journals Cardiovascular Scopus journals Cardiovascular PubMed journals Cardiovascular medical journals Cardiovascular free journals Cardiovascular best journals Cardiovascular top journals Cardiovascular free medical journals Cardiovascular famous journals Cardiovascular Google Scholar indexed journals Electrocardiogram articles Electrocardiogram Research articles Electrocardiogram review articles Electrocardiogram PubMed articles Electrocardiogram PubMed Central articles Electrocardiogram 2023 articles Electrocardiogram 2024 articles Electrocardiogram Scopus articles Electrocardiogram impact factor journals Electrocardiogram Scopus journals Electrocardiogram PubMed journals Electrocardiogram medical journals Electrocardiogram free journals Electrocardiogram best journals Electrocardiogram top journals Electrocardiogram free medical journals Electrocardiogram famous journals Electrocardiogram Google Scholar indexed journals Microelectromechanical articles Microelectromechanical Research articles Microelectromechanical review articles Microelectromechanical PubMed articles Microelectromechanical PubMed Central articles Microelectromechanical 2023 articles Microelectromechanical 2024 articles Microelectromechanical Scopus articles Microelectromechanical impact factor journals Microelectromechanical Scopus journals Microelectromechanical PubMed journals Microelectromechanical medical journals Microelectromechanical free journals Microelectromechanical best journals Microelectromechanical top journals Microelectromechanical free medical journals Microelectromechanical famous journals Microelectromechanical Google Scholar indexed journals Chest and abdomen articles Chest and abdomen Research articles Chest and abdomen review articles Chest and abdomen PubMed articles Chest and abdomen PubMed Central articles Chest and abdomen 2023 articles Chest and abdomen 2024 articles Chest and abdomen Scopus articles Chest and abdomen impact factor journals Chest and abdomen Scopus journals Chest and abdomen PubMed journals Chest and abdomen medical journals Chest and abdomen free journals Chest and abdomen best journals Chest and abdomen top journals Chest and abdomen free medical journals Chest and abdomen famous journals Chest and abdomen Google Scholar indexed journals Respiration rate articles Respiration rate Research articles Respiration rate review articles Respiration rate PubMed articles Respiration rate PubMed Central articles Respiration rate 2023 articles Respiration rate 2024 articles Respiration rate Scopus articles Respiration rate impact factor journals Respiration rate Scopus journals Respiration rate PubMed journals Respiration rate medical journals Respiration rate free journals Respiration rate best journals Respiration rate top journals Respiration rate free medical journals Respiration rate famous journals Respiration rate Google Scholar indexed journals Transreceiver articles Transreceiver Research articles Transreceiver review articles Transreceiver PubMed articles Transreceiver PubMed Central articles Transreceiver 2023 articles Transreceiver 2024 articles Transreceiver Scopus articles Transreceiver impact factor journals Transreceiver Scopus journals Transreceiver PubMed journals Transreceiver medical journals Transreceiver free journals Transreceiver best journals Transreceiver top journals Transreceiver free medical journals Transreceiver famous journals Transreceiver Google Scholar indexed journals Sporty articles Sporty Research articles Sporty review articles Sporty PubMed articles Sporty PubMed Central articles Sporty 2023 articles Sporty 2024 articles Sporty Scopus articles Sporty impact factor journals Sporty Scopus journals Sporty PubMed journals Sporty medical journals Sporty free journals Sporty best journals Sporty top journals Sporty free medical journals Sporty famous journals Sporty Google Scholar indexed journals
Article Details
1. Introduction
Currently, there are many elderly people, who suffer from poor health. According to this, the long-term attention to them is considered a very important issue for their health. In other words, identifying and tracking daily physical activity is a key factor in assessing the health and quality of life. Thus, continuous monitoring of the health status of patients can prevent injuries and also ensure their social life. For example, cardiovascular signals are important indicators for evaluating the health of patients due to the rapid growth of cardiovascular deaths [1]. Recently, a large number of cardiovascular monitoring systems have emerged in medical centers in recent decades to reduce these deaths [2]. Continuous cardiovascular monitoring techniques can be divided into three measurement methods: devices that measure movement and tissue changes, devices that measure the flow of air, and devices that measure
changes in the blood. One of the biggest problems patients suffer is the wasting time and cost to visit the clinics, especially in remote areas [3]. Additionally, the patients experience the drawbacks when visiting these places. Recently, telemedicine has emerged benefiting advances in communications technology and telecommunication in order to offer the patients a variety of home-based systems at home using wearable sensors [4-7].
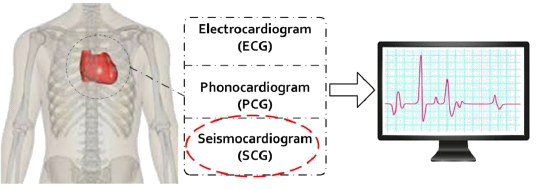
Figure 1: A variety of cardiorespiratory system monitoring and our method.
The wearable sensors can record the patients vital signs in smart homes and then transmit the information to medical centers and clinics through the Internet [8]. There are ample wearable commercial systems that are commonly used for cardiovascular systems monitoring, including electrocardiogram (ECG) [8], phonocardiogram (PCG) [9] and seismocardiogram (SCG) [11] (Figure 1). An ECG device measure and record the electrical activity in the heart. When a heartbeat is made, the heart emits a series of electrical discharge spikes that can be recorded using electrodes on the surface of the body. An ECG tracing is affected by patient motion. Another problem for the device is a stress on the patient [10]. In another system, namely PCG, are based on recording and detecting heart sounds, which are made by the various cardiac structures pulsing and moving blood and also are caused by the acceleration and deceleration of blood and turbulence developed during rapid blood flow. However, the PCG is produced from the bloodstream and cannot cover frequencies below 25 Hz [12-13]. Today, the seismocardiogram (SCG) emerge to alleviate the disadvantages associated with ECG and PCG systems [14]. The chest makes variations during the heart and respiration activities that the vibration can be recorded by placing a microelectromechanical (MEMS) accelerometer on the sternum while the patient lies supine [15-16]. The MEMS accelerometer sensor can accurately measure the acceleration of three-axis length, width, and height [17]. Indeed, the SCG systems can be employed to measure the produced accelerations of the chest wall by a myocardial movement [14]. Recently, the SCG system is recommended for health-care instead ECG and PCG due to be comfortable, non-bulky and non-intrusive.
In this paper, a system for vital signs of cardiorespiratory system monitoring based on accelerometer sensors is presented. The system includes a microcontroller, a motion sensor, and a transreceiver. The developed sensor records heart and lung movements that will obtain heartbeat and respiration rate after using high and low pass filter, respectively. Compared to other SCG systems [18-19], this system can estimate the heart rate with more accuracy. So that the mean square error for heart rate is 2.8 beats per minute and for breathing 1.01 breaths per minute. In addition, it has a smaller hardware system and lower weight than [18-19].
2. Material and Method
2.1 The proposed method
As Figure 2 shows, cardiovascular systems result in the small movements in the chest. The movements can be converted into two movements: short and long-term, which are supposed as a heart rate and respiration, respectively. Accordingly, the movements can be extracted from the chest using equation 1.
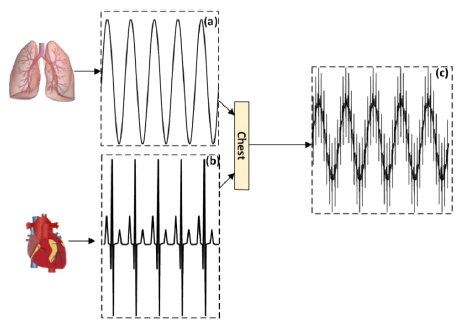
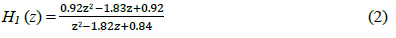
Figure 2: The proposed mechanism, (a) respiration rate; (b) heartbeat and (c) total lung and heart activities.

Where DL is associated with lung activities or with low frequency movements (Figure 2a). While DH is movements with higher frequencies for cardiac activity (Figure 2b). Also, DT is the sum of the two previous movements that are obtained from the chest (Figure 2c). In order to obtain this DT, a motion sensor can measure both short and long-term movements of the chest and abdomen. For this purpose, an accelerometer is used.
2.2 Hardware
The developed system for heart rate and respiration rate estimation includes a wireless motion sensor, a central node and a personal computer for displaying data (Figure 3). The wireless motion sensor, including an accelerometer sensor, a microcontroller (AVR-Atmega 32), and a transreceiver operating ISM band and at a frequency of 2.54 GHz (Figure 4a). The microcontroller is communicated with the accelerometer sensor through the I2C protocol for taking the updated data. Then, the data are sent to transreceiver through SPI protocol. The transreceiver wirelessly transmits the data to the central node. It should be noted that the sensor node is designed and is mounted on a small PCB and its voltage supply with a 3.7-volt lithium polymer battery.
The developed central node also includes a transreceiver, a processor (atmega32) and a USB converter to the TTL (Figure 4b). First, the transreceiver receives the data from the sensor node and send the data through SPI protocol to the microcontroller. The microcontroller takes them and transmits the data to USB to TTL converter through serial
port (UART protocol). The obtained data are recorded and saved in the Personal Computer (PC) for further processing. The central node's components are mounted on another PCB and its voltage are supplied through USB voltage. In fact, the central node is the main controller for connecting to the computer which is used to store data at a sample rate of 50 Hz. One of the important features of the developed system is more reliable for transmitting data wirelessly. Other feature of the transreceiver consists of low cost, and high send and receive rates. The transreceiver has a power consumption of 0 dB and the rate of information transmitter 1.8 Mbps.
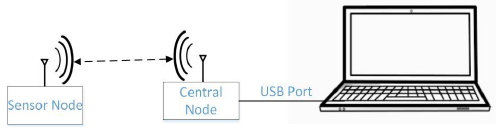
Figure 3: The measurement setup for estimation of heartbeat and respiration rate.
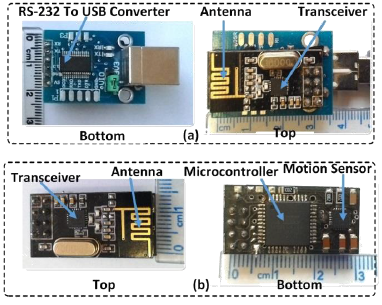
Figure 4: The Prototype of the developed system (a) the sensor node; (b) the developed central node.
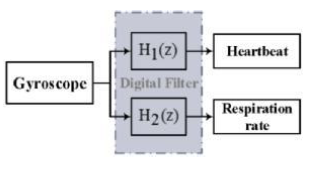
Figure 5: Digital signal processing for separation of the heartbeat and respiration rate.
3. Signal Processing
In order to separate the heartbeat from the respiration rate in the raw data, a digital filter is used (Figure 5). The digital filter includes of a high-pass and low-pass Butterworth filter, which are a second-order digital filter with a sampling rate of 50 Hz and a cut of the frequency of 0.5 Hz, to separate the heart rate and the breath rate from the chest signal, respectively. The high-pass filter is as follows:
And the low-pass filter is as follows:
4. Results and Discussion
As previously mentioned, using a patient-monitoring system at home can be very effective due to the death rate associated with cardiovascular systems is severely rising. Although there are many systems in the market for this purpose, a system can be used at home that has been features such as high accuracy and low cost as well as portability.
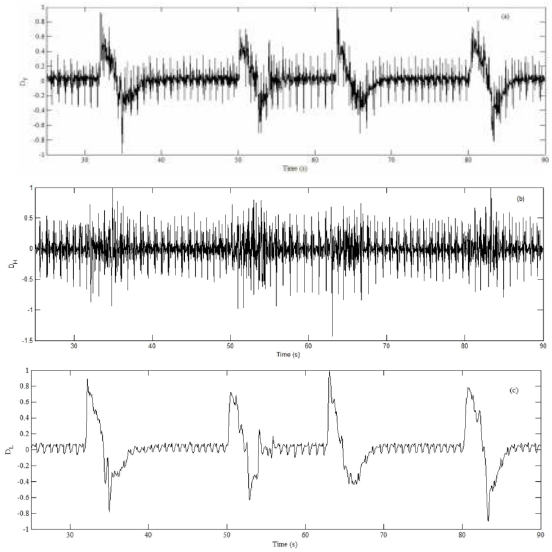
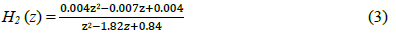
Figure 6: The obtained result of the holding breath test for (a) raw signal; (b) the heartbeat and (c) the respiration rate.
In order to investigate the accuracy of the presented system, an ECG device, similar to [20], is mounted on the patient's chest along the developed sensor for comparison of the heart rate of the presented sensor with a reference (gold standard). This ECG device is a single-mode ECG that measures the typical ECG data and can transfer those data through a USB port to the computer to evaluate the data. Also, a belt around the abdomen, like in [21], is used for evaluating the precision of the respiration rate in the proposed system.
In the first test, the volunteer is asked to hold his breath in a lying condition and take a deep breath after a few seconds. The volunteer repeatedly performed this test within 3 minutes. These results averagely indicate the respiratory rate is 5 per minute and the heart rate is 68 per minute for this period while the gold standards show respiration and heartbeat 5 breaths per minute and 69 beats per minute, respectively. The snapshot of the results have been selected and shown in Figure 6a, 6b, and 6c for raw data, after using the high pass filter and low pass filter, respectively. In another test, while the volunteer lies his face upward (supine), the developed sensor averagely measured his heart rate 76 breaths per minute and respiration rate 29 breaths per minute for 3 minutes. The gold standard also indicates that the mean values 30 and 74, respectively, for respiration rate and heartbeat. The results of this test, which are related to the raw data of the developed sensor and passing through the high pass and low pass filter, are shown in Figure 7a, 7b, and 7c in turn.
In order to further evaluate the results of the proposed system, the Bland-Altman analysis is considered for respiration and heart rate, separately as Figure 8. Figure 8 (I) shows the Bland-Altman plot is extracted from two supine and holding breath tests for 90 pairs of measurements of the developed system and the reference system in for breath rate. This plot is determined by the difference and the mean of the breath from the obtained results [22-23]. So the horizontal axis in the plot is average of breath from the developed system and the reference system in [21], as well as the vertical axis, is the difference between the breath of the developed system and the reference system. As these results reveal, the average error is 0.1 breaths per minute, with a 95% compatibility range between -1.14 and 1.35 breaths per minute.
Also, the Bland-Altman plot for heart rate are derived from two mentioned tests with 90 pairs measurements of the developed system and the reference system in [20] and are shown in Figure 8 (II). In this case, the average error is 0.24 beats per minute with a 95\% compatibility range between -2.23 and 2.71 beats per minute. With the help of this Bland-Altman plot, other valuable information can be obtained. For example, the mean squared error and standard deviation for respiration rate are 1.43 and 0.85 breaths per minute, respectively, as well as for heart rate 2.8 and 1.01, separately. Accordingly, very good compatibility between the proposed system and the ECG reference system [19] as well as the abdominal belt for the reference system in [21] of respiration is obtained. Finally, the results of this sensor reveal that the developed sensor is an ideal candidate for monitoring heart rate and respiration. Also, it can be a good alternative to the other works because of good accuracy, portability, and affordability.
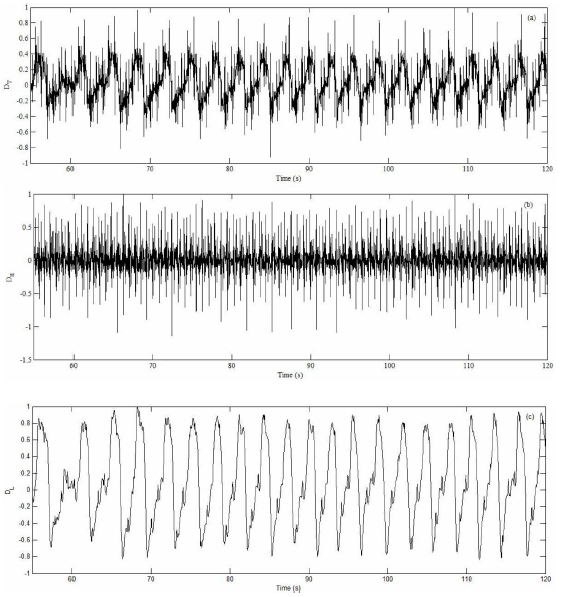
Figure 7: The obtained result of the supine test for (a) raw signal; (b) the heartbeat and (c) the respiration rate.
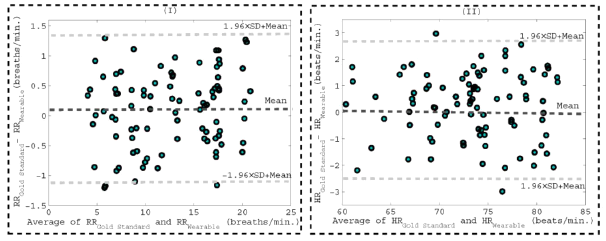
Figure 8: The Bland-Altman plot for (I) respiration and (II) heartbeat. The plot is based on the obtained data of the developed sensor and a gold standard.
5. Conclusion
In this paper, developing a motion sensor based on SCG for measuring heart rate and respiration was described. This sensor was made with the help of a very small and low weight PCB. To investigate the accuracy of the sensor, two tests were performed and the heartbeat and respiration rate values obtained from these tests and then, were compared with a commercial ECG device as well as a commercial respiratory diagnostic device for reference. The results showed that the proposed sensor measures heartbeat and respiration rate with mean square errors of 2.8 and 1.01 beat per minute, respectively, while the standard deviations are 1.43 and 0.85, separately. As a consequent, this sensor can be an appropriate alternative to monitor the vital signs of the cardiorespiratory system for a long time.
References
- Patel M and Wang J. Applications, challenges, and prospective in emerging body area networking technologies. IEEE Wireless Communications Magazine 17 (2010): 80-88.
- Li KF. Smart home technology for telemedicine and emergency management. Journal of Ambient Intelligence and Humanized Computing 4 (2013): 535-546.
- Amadi-Obi A, Gilligan P, Owens N, et al. Telemedicine in prehospital care: a review of telemedicine applications in the pre-hospital environment. International journal of emergency medicine 7 (2014): 1.
- Abbasi-Kesbi R, Nikfarjam A, Memarzadeh-Tehran H. A Patient-Centric Sensory System for In-Home Rehabilitation. IEEE Sensors Journal 17 (2017): 524-533.
- Nikfarjam A and Abbasi-kesbi R. A mini wearable wireless sensor for rehabilitation applications. Robotics and Mechatronics (ICROM), 3rd RSI International Conference on IEEE (2015): 618-622.
- Abbasi-Kesbi R and Nikfarjam A. A miniature sensor system for precise hand position monitoring. IEEE Sensors Journal 18 (2018): 2577-2584.
- Valipour A and Abbasi-Kesbi R. A heartbeat and respiration rate sensor based on phonocardiogram for healthcare applications. In 2017 Iranian Conference on Electrical Engineering (ICEE) (2017): 45-48.
- Gonzales L, Walker K, Keller K, et al. Textile sensor system for electrocardiogram monitoring. Virtual Conference on Applications of Commercial Sensors (VCACS), IEEE (2015): 1-4.
- Xiao Y, Xiao S, Cao Z, et al. The phonocardiogram exercise test’ Engineering in Medicine and Biology Magazine, IEEE 18 (1999): 111-115.
- Cifkova R. Advantages and disadvantages of ECG diagnosis in left ventricular hypertrophy. Vnitrni lekarstvi 48 (2002): 103-108.
- Bifulco P, Gargiulo G, dAngelo G, et al. Monitoring of respiration, seismocardiogram and heart sounds by a pvdf piezo film sensor. 20th IMEKO TC4 Symposium on Measurements of Electrical Quantities: Research on Electrical and Electronic Measurement for the Economic Upturn 11 (2014): 12.
- Durand LG and Pibarot P. Most Recent Advancements in Digital Signal Processing of the Phonocardiogram. Critical Review in Biomedical Engineering 45 (2017).
- Abbasi-Kesbi R, Valipour A and Imani K. Cardiorespiratory system monitoring using a developed acoustic sensor. Healthcare technology letters 5 (2018): 7-12.
- Inan OT, Migeotte PF, Park KS, et al. Ballistocardiography and seismocardiography: A review of recent advances. IEEE journal of biomedical and health informatics 19 (2015): 1414-1427.
- Aescher M, Matthies DJ, Trimpop J, et al. A study on measuring heart-and respiration-rate via wrist-worn accelerometer-based seismocardiography (SCG) in comparison to commonly applied technologies. In Proceedings of the 2nd international Workshop on Sensorbased Activity Recognition and Interaction ACM (2018): 2.
- Salerno DM and Zanetti J. Seismocardiography for monitoring changes in left ventricular function during ischemia. Chest, Elsevier 100 (1991): 991-993.
- Abbasi-kesbi R and Nikfarjam A. Denoising MEMS Accelerometer Sensors Based on L2-Norm Total Variation Algorithm. Electronics Letters 53 (2017).
- Tadi MJ, Koivisto T, Pankaala M, et al. Accelerometerbased method for extracting respiratory and cardiac gating information for dual gating during nuclear medicine imaging. Journal of Biomedical Imaging (2014): 6.
- Dinh A, Choi Y, Ko SB. A heart rate sensor based on seismocardiography for vital sign monitoring systems. Electrical and Computer Engineering (CCECE), 2011 24th Canadian Conference (2011): 665-668.
- Products: M-80, Beurer Germany, Hallandale Beach, Florida.
- Respiration Monitor Belt, Vernier.
- Abbasi-Kesbi R, Memarzadeh-Tehran H, Jamal Deen M. A Technique to Estimate the Human Reaction Time Based on Visual Perception. Healthcare Technology Letters 4 (2017): 73.
- Atkinson G, Nevill AM. Statistical methods for assessing measurement error (reliability) in variables relevant to sports medicine. Sports medicine 26 (1998): 217-238.
