Visual Outcome of Patients with Idiopathic Intracranial Hypertension Treated with Oral Acetazolamide: A Single Centre Study
Article Information
Md. Aminur Rahman1*, A. K. M. Shahidur Rahman2, Md. Hamidul Mulk3, Naoroze Ferdous Romance4, Arzumand Binte Yousuf Muna5, Rehnuma Sadia Siddiqua6, Md. Mahmudur Rahman7, Zakia Yasmin6
1Assistant Surgeon, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
2Medical Officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
3Assistant Surgeon, 250 Beded District Hospital, Chapainwabgang, Bangladesh
4Medical Officer, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
5Consultant Ophthalmologist, Lions Eye Institute and Hospital, Dhaka, Bangladesh
6Consultant Ophthalmologist, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh
7Resident Surgeon (Ophthalmology), Rangpur Medical College Hospital, Rangpur, Bangladesh
*Corresponding author: Dr. Md. Aminur Rahman, Assistant Surgeon, Department of Ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh. E-mail: aminur36th@gmail.com
Received: 21 June 2023; Accepted: 28 June 2023; Published: 10 July 2023
Citation: Rahman MA, Rahman AKMS, Mulk MH, Romance NF, Muna ABY, Siddiqua RS, Rahman MM, Yasmin Z. Visual Outcome of Patient with Idiopathic Intracranial Hypertension Treated with Oral Acetazolamide: A Single Centre Study. Journal of Ophthalmology and Research. 6 (2023): 28-35.
View / Download Pdf Share at FacebookAbstract
Idiopathic intracranial hypertension (IIH) is a disorder primarily among overweight women of childbearing age, characterized by increased intracranial pressure (ICP) with its associated features. Acetazolamide (AZM) is commonly used to treat IIH, but there is insufficient information to establish an evidence base for its use. This study was designed to evaluate the visual outcome of patient with IIH treated with oral acetazolamide. A total of forty-nine (49) patients with IIH treated with oral acetazolamide (500 mg twice daily) were followed up after 3 months and 6 months. Bestcorrected visual acuity (BCVA) was recorded, visual field analysis was done and papilledema was graded accordingly. Mean value of the BCVA, scores of papilledema and mean deviations of the follow-up periods were compared with that of baseline values. The mean age of the study patients was 25.3±8.7 years with a female predominance (83.7%) and majority (65.3%) of them was over-weight/obese. Headache, nausea, double vision, transient vision loss, tinnitus, dimness of vision and low back pain were the presenting features. The mean cerebrospinal fluid (CSF) opening pressure of the study patients was 323.7±46.1 mm H2O. The mean BCVA in log MAR unit, perimetric mean deviation (PMD) and papilledema of both eyes were reduced significantly over time. In this study common side effects of AZM were paresthesia, dysgeusia, lethargy, anorexia, nausea and polyuria. This study concluded that oral acetazolamide 500 mg twice daily is effective in reduction of symptoms/signs and improve visual outcome among patients with idiopathic intracranial hypertension with minimum side effects.
Keywords
Acetazolamide (AZM), Cerebrospinal Fluid (CSF), Idiopathic Intracranial Hypertension (IIH), Visual Outcome
Acetazolamide (AZM) articles; Cerebrospinal Fluid (CSF) articles; Idiopathic Intracranial Hypertension (IIH) articles; Visual Outcome articles
Article Details
1. Introuduction
Idiopathic intracranial hypertension (IIH) is the syndrome of elevated intracranial pressure (ICP) in the absence of space occupying or vascular lesions and without enlargement of the cerebral ventricles, for which no definite cause can be identified [1]. Patients with IIH usually obese, female of childbearing age [2]. The reported incidence was approximately 0.9-1.7 per 100,000 in Western societies, which may be as high as 14.88 per 100,000 in the obese population [3, 4]. The pathophysiology underlying the raised intracranial pressure is still unclear. Excess cerebrospinal fluid (CSF) production, increased brain water content, reduced CSF absorption, increased cerebral venous pressure and endocrine dysfunction are the main determinants of increased intracranial pressure [4]. Apart from female sex and obesity there are no proven associations in idiopathic intracranial hypertension [4]. Some studies showed that vitamin A deficiency, medications (corticosteroid, oral retinoids, levonorgestrel, tetracycline antibiotics, particularly minocycline and doxycycline etc.), diseases (systemic arterial hypertension, diabetes mellitus, thyroid disease, hypoparathyroidism, iron deficiency anaemia etc.), pregnancy and menstrual dysfunction are associated with idiopathic intracranial hypertension [4, 5]. Patients often present with one or more symptoms of headache, transient visual obscurations, and pulsatile tinnitus [6, 7]. Alterations in visual function may include subjective blurred vision, visual field defects, and binocular diplopia [6]. Modified Dandy diagnostic criteria are used to level the IIH which include; symptoms/signs of increased intra cranial pressure (ICP), no localizing neurologic signs except for unilateral/bilateral 6th nerve palsies, increased CSF opening pressure with normal CSF composition, no evidence of hydrocephalus/mass/structural/vascular lesion on imaging and no other cause of increased ICP identified [8]. Definite diagnosis requires the presence of papilledema and elevated opening pressure on lumbar puncture (LP) [4]. Perimetry is the best diagnostic method to evaluate the patients in follow up periods [9]. Most common type of visual field defects in idiopathic intracranial hypertension (IIH) include; an enlarging blind spot, loss of nasal or temporal visual field, or generalized visual field constriction [10]. Perimetric mean deviation (PMD) is one of the important variables of visual outcome [6]. It also help escalation of dose of acetazolamide (AZM) as the PMD improved to equal to or better than -1 dB in each eye signifies adequate improvement for dose adjustment [11]. Reduction of body weight, medical treatment and surgery are the main options for the management of IIH [4, 8]. The specific treatment approach depends on the severity and the time course of disease with definitive goals to alleviate the symptoms including headache and to preserve the vision [8]. Indications for starting medical treatment for patients with IIH are visual field changes and symptoms of elevated ICP [4, 8]. The carbonic anhydrase inhibitor acetazolamide (AZM) is the drug most commonly used to treat idiopathic intracranial hypertension [6]. Other diuretics, such as furosemide, are sometimes used if acetazolamide is poorly tolerated [8, 12]. The mechanism of action of acetazolamide is likely multi-factorial. Acetazolamide has been found to reduce CSF production in humans by 6-50% [8, 11]. It has been thought to work by inhibition of carbonic anhydrase that causes a reduction in transport of sodium ions across choroid plexus epithelium [11]. Also, it changes the taste of foods and causes carbonated beverages to taste metallic, this may aid the patient in weight loss [8, 11]. Additionally, some patients experience nausea, further helping them to lose weight [8, 11]. Acetazolamide is usually started at a dose of 0.5–1 g/day and can be gradually increased until clinical improvement is seen or a dose of 3–4 g/day is reached, unless the patient develops intolerable side effects [8, 12]. Although the safety and tolerability of acetazolamide dosing at 1 g/day has been documented, there is uncertainty regarding the safety and tolerability of acetazolamide beyond 1 g/day due to the lack of high-level clinical evidence [13]. Visual outcome is the measurement of visual function and papilledema grading, in which visual function consist of best corrected visual acuity (BCVA) and visual field (grading of field defects and perimetric mean deviations) [9]. This present study was designed to evaluate the visual outcome of patients with idiopathic intracranial hypertension treated with oral acetazolamide at a tertiary eye care centre in Bangladesh.
2. Methodology
This prospective observational study was conducted at Department of Neuro-ophthalmology, National Institute of Ophthalmology and Hospital (NIO&H), Dhaka, Bangladesh from December 2019 to October 2021. The research protocol was approved by the ethical review committee of NIO&H. A total of forty-nine (49) patients with idiopathic intracranial hypertension (IIH) diagnosed by modified dandy diagnostic criteria were enrolled for this study using purposive sampling technique [8]. All patients of idiopathic intra-cranial hypertension (IIH) selected for treatment with oral acetazolamide were included. Patients with co-existing intra-ocular and ocular surface disease, patients having history of ocular surgery and trauma in the previous six months, patients suffering from systemic immunological disease, pregnant patients and patients with age less than twelve years were excluded from this study. After selection informed written consent was obtained from each study participant. Detail history was taken from all the selected patients; then detail ophthalmic as well as systemic examination was performed and all relevant investigations were done. Acetazolamide 500 mg twice daily tablet was prescribed in all the study subjects. Then they were advised to follow-up after 3 months and at 6 month. Best-corrected visual acuity (BCVA) was recorded on Snellen acuity chart and converted into Log MAR unit. Visual field analysis was done by Humphrey visual field analysis 24-2 testing pattern. Visual field changes were graded into grade-1 (normal), grade-2 (enlarged blind spot), grade-3 (nasal or temporal defect) and grade-4 (concentric constriction) [14]. Perimetric mean deviation (PMD) was recorded at baseline and at follow up periods. Papilledema was graded according to modified Frisein scale and were scored into 1= no papilledema, 2= grade 1, 3= grade 2, 4= grade 3, 5= grade 4 and 6= grade 5 [15]. All the relevant data were recorded in a pre-designed data collection sheet, during baseline after 3 months and at 6 months of starting treatment. Mean values of the best-corrected visual acuity (BCVA), scores of papilledema and mean deviations of the follow-up periods were compared with that of baseline values. Demographic variables, clinical features, visual outcome variables and drug reactions of all study patients were recorded accordingly.
Statistical analysis
All collected data were cross-checked and compiled. Statistical analysis was done by using window-based software statistical package for social science (SPSS) version- 26. Categorical data were presented as frequency with percentage and continuous data were expressed as mean with standard deviation (SD). The statistics used in this study was descriptive statistics. Paired ‘t’ test was done for analysis of quantitative data and Chi-square test was performed for qualitative data. A p value <0.05 was considered as statistically significant.
3. Results and Observations
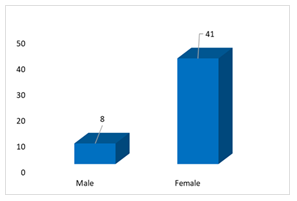
The present study was intended to evaluate the visual outcome of patient with idiopathic intracranial hypertension (IIH) treated with oral acetazolamide. Total 49 patients fulfilled the selection criteria were treated with acetazolamide (500 mg twice daily) and followed up at 3 and 6 months. The mean age of the study patients was 25.3±8.7 years which ranged from 15.0-44.0 years. Out of 49 patients; 13 (26.5%) patients were in 15-20 years age group, 10 (20.4%) patients were in 20-25 years age group, 10 (20.4%) patients were in 25-30 years age group, 6 (12.2%) patients within 30-35 years and another 10 (20.4%) patients were more than 35 year (Table- 1). Of them, 41 (83.7%) patients were female and 8 (16.3%) patients were male (Figure-1).
Table 1: Age distribution of the study patients (N-49)
|
Age (years) |
Frequency (n) |
Percentage (%) |
|
Mean ± SD |
25.3±8.7 years |
|
|
Range |
15.0 - 44.0 years |
|
|
Age groups |
||
|
15-20 years |
13 |
26.5 |
|
20-25 years |
10 |
20.4 |
|
25-30 years |
10 |
20.4 |
|
30- 35 years |
6 |
12.2 |
|
>35 year |
10 |
20.4 |
In this study; the mean body mass index (BMI) of the study patients was 29.3±5.4 kg/m2, which was ranged from 18.2 - 38.3 kg/m2. Among total study patients; 17 (34.7%) patients had normal body weight (BMI: 18.5 – 24.9 kg/m2), 12 (24.5%) patients had over weight (BMI: 25.0 – 29.9 kg/m2) while 20 (40.8%) patients were obese (BMI: >30.0 kg/m2) (Table- 2).
Table 2: Distribution of study patients according to the body mass index (BMI) (N=49)
|
BMI (kg/m2) |
Frequency (n) |
Percentage (%) |
|
Mean ± SD |
29.3±5.4 kg/m2 |
|
|
Range |
18.2 – 38.3 kg/m2 |
|
|
18.5 – 24.9 (normal) |
17 |
34. 7% |
|
25.0 – 29.9 (over weight) |
12 |
24.50% |
|
≥30.0 (obese) |
20 |
40.80% |
Regarding clinical presentations; 47 (95.9%) study patients had headache, 26 (53.1%) patients had nausea, 23 (46.9%) patients had double vision and 16 (32.7%) patients had transient vision loss. A few patients had tinnitus (n=6, 12.2%), dimness of vision (n=4, 8.2%) and low back pain (n=2, 4.1%) (Table-3).
Table 3: Distribution of study patients by clinical presentations (N=49)
|
Clinical presentations* |
Frequency (n) |
Percentage (%) |
|
Headache |
47 |
95.9 |
|
Nausea |
26 |
53.1 |
|
Double vision |
23 |
46.9 |
|
Transient vision loss |
16 |
32.7 |
|
Tinnitus |
6 |
12.2 |
|
Dimness of vision |
4 |
8.2 |
|
Low back pain |
2 |
4.1 |
*Multiple responses
The mean cerebrospinal fluid (CSF) opening pressure of the study patients was 323.7±46.1 mm H2O, which ranged from 260.0 – 420.0 mm H2O. We found; 15 (30.6%) study patients had <300 mm H2O CSF opening pressure, 20 (40.8%) patients ha
d 300-350 mm H2O CSF opening pressure, while 14 (28.6%) patients had >350 mm H2O CSF opening pressure (Table- 4).
Table 4: Distribution of the study patients on cerebrospinal fluid (CSF) opening pressure (N=49)
|
CSF opening pressure |
Frequency (n) |
Percentage (%) |
|
Mean ± SD (mm H2O) |
323.7±46.1 |
|
|
Range (mm H2O) |
260.0 – 420.0 |
|
|
250-300 mm H2O |
15 |
30.60% |
|
300-350 mm H2O |
20 |
40.80% |
|
>350 mm H2O |
14 |
28.60% |
Grading of visual field defects revealed that 2 (4.1%) patients had grade 1 (normal) visual fields (both eyes); nasal or temporal defect (Grade 3) was present among 22 (44.9%) patients in right eye and 24 (49.0%) patients in left eye. Enlarged blind defect (Grade 2) was present among 17 (34.7%) patients in their both eyes. Concentric constricted visual field (Grade 4) was present among 8 (16.3%) patients in right eye and 6 (12.2%) patients in left eye (Table- 5).
Table 5: Distribution of study patients on grading of visual field defects (N=49)
|
Grading of visual field defects |
Right eye |
Left eye |
|
Grade 1 (Normal) |
2 (4.1%) |
2 (4.1%) |
|
Grade 2 (Enlarged blind defect) |
17 (34.7%) |
17 (34.7%) |
|
Grade 3 (nasal or temporal defect) |
22 (44.9%) |
24 (49.0%) |
|
Grade 4 (Concentric constricted) |
8 (16.3%) |
6 (12.2%) |
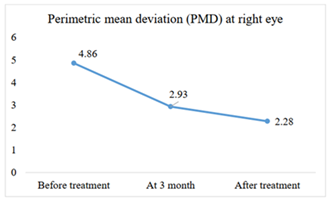
We observed the mean value of mean deviation in dB of both (right and left) eye by Humphrey visual field analyser (HVFA) (24-2) of the study subjects at different follow-up periods (taking absolute values). The baseline value of mean of perimetric mean deviation (PMD) at right eye was -4.86dB. After treatment with acetazolamide, the PMD reduced to -2.93dB and -2.28dB at 3 months and at 6 months respectively (Figure- 2).
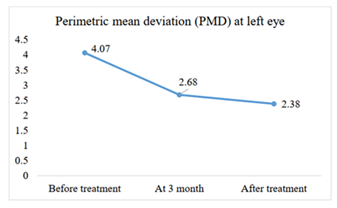
Similarly, the baseline value of the mean of perimetric mean deviation (PMD) at left eye was -4.07dB. After treatment with acetazolamide, the PMD reduced to -2.68dB and -2.38dB at 3 months and at 6 months respectively (Figure- 3).
Table 6 shows the comparison of mean values of mean deviation from baseline with that of final follow-up (at 6 month). The baseline value of the mean of perimetric mean deviation (PMD) at right eye was -4.86±1.67dB and that was decreased (-2.28±1.51dB) significantly after treatment (p<0.001). In accordance, before treatment the mean of PMD at left eye was --4.07±2.06dB and after treatment that was -2.38±1.94dB, which was also decreased significantly after treatment (p<0.001) (Table- 6).
Table 6: Comparison of mean values of mean deviation of baseline with that of final follow-up
|
Eye examined |
Baseline |
At final follow-up |
p value |
|
Right eye |
-4.86±1.67 |
-2.28±1.51 |
<0.001s |
|
Left eye |
-4.07±2.06 |
-2.38±1.94 |
<0.001s |
p value obtained by paired t test, s= significant
Analysis of papilledema grades at baseline, 3 months, and 6 months after treatment revealed significant improvements in both right and left eyes (p<0.05). The percentage of patients with no grade papilledema increased from 0% at baseline to 46.9% at 3 months and further to 75.5% at 6 months in the right eye; while in the left eye, the corresponding values were 0%, 49.0%, and 71.4% respectively. The reduction in higher grades of papilledema was also evident; with significant reduction observed in different grades over time (p<0.05). These results indicated that oral acetazolamide treatment effectively reduces papilledema and improves visual outcome in patients with idiopathic intracranial hypertension (Table- 7).
Table 7: Distribution of papilledema (grades) at different assessment periods among the study patients (according to Frisén scale) (N= 49)
|
Grade of papilledema |
Right eye |
Left eye |
||||||||
|
|
Base line |
3 months after Treatment |
6 months after treatment |
Base line |
3 months after treatment |
6months after treatment |
||||
|
No grade of papilledema |
0(0.0) |
23 (46.9) |
37 (75.5) |
0(0.0) |
24 (49.0) |
35 (71.4) |
||||
|
Grade 1 |
02(4.1) |
11 (22.4) |
08 (16.3) |
02 (4.1) |
12 (24.5) |
08 (16.3) |
||||
|
Grade 2 |
14 (28.6) |
05 (10.2) |
04 (8.2) |
17 (34.7) |
07 (14.3) |
06 (12.2) |
||||
|
Grade 3 |
12 (24.5) |
07 (14.3) |
0(0.0) |
10 (20.4) |
06(12.2) |
0(0.0) |
||||
|
Grade 4 |
05 (10.2) |
03 (6.1) |
0(0.0) |
05 (10.2) |
0(0.0) |
0(0.0) |
||||
|
Grade 5 |
16 (32.7) |
0 (0.0) |
0(0.0) |
15 (30.6) |
0(0.0) |
0(0.0) |
||||
|
Comparison (Right eye) |
p-value |
Comparison (Left eye) |
p-value |
|||||||
|
Baseline vs 3 months |
<0.001S |
Baseline vs 3 months |
<0.001S |
|||||||
|
Baseline vs 6 months |
<0.001S alleviate |
Baseline vs 6 months |
<0.001S |
|||||||
|
3 months vs 6 months |
0.004S alleviate |
3 months vs 6 months |
0.023S |
|||||||
Values within parenthesis indicates corresponding percentage, p-value obtained by Chi-square test, s= significant
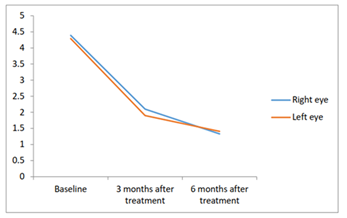
In right eye mean score of grading of papilledema was 4.39 at baseline; it was 2.1 and 1.33 after 3 and 6 months of treatment respectively. In left eye mean score of grading of papilledema was 4.29 at baseline; that was 1.90 and 1.41 after 3 and 6 months of treatment respectively. Changes of mean scores of papilledema grading from baseline in all instances were statistically significant (p<0.001, p values obtained by paired t test) (Figure- 4).
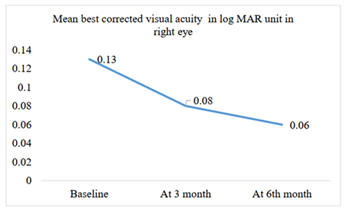
The mean best corrected visual acuity (BCVA) in log MAR unit before treatment (baseline) in right eye was 0.13. After treatment with acetazolamide, the mean BCVA was reduced to 0.08 at 3 months. At the end of 6 months, the mean BCVA was reduced to 0.06 (Figure- 5).
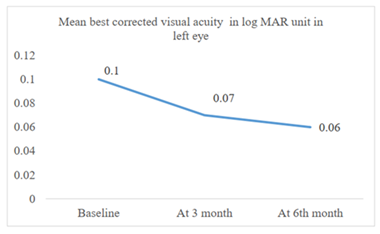
The mean best corrected visual acuity (BCVA) in log MAR unit before treatment (baseline) in left eye was 0.10. After treatment with acetazolamide, the BCVA was reduced to 0.07 at 3 months. At the end of 6 months, the BCVA was reduced to 0.06 (Figure- 6).
The baseline value of mean of visual acuity in log MAR at right eye was 0.13±0.25 and after treatment that was 0.06±0.07. The baseline value of mean visual acuity of left eye was 0.11±0.24 and after treatment it was 0.06±0.13. It was observed that, the mean best corrected visual acuity (BCVA) in log MAR unit of both eyes among the study patients was significantly improved after treatment (p<0.05) (Table- 8).
Table 8: Comparison of mean best corrected visual acuity in log MAR unit of both eyes among the study patients before and after treatment (N=49)
|
Eye examined |
Mean best corrected visual acuity in log MAR unit |
p value |
|
|
Before treatment |
After treatment |
||
|
(Mean±SD) |
(Mean±SD) |
||
|
Right eye |
0.13±0.25 |
0.06±0.07 |
0.003s |
|
Left eye |
0.11±0.24 |
0.06±0.13 |
0.001s |
p value obtained by paired t test, s= significant,
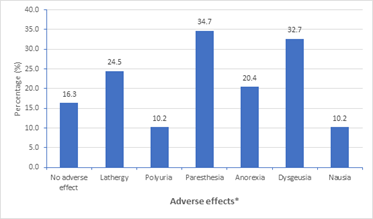
Regarding adverse effects of treatment among the study patients; out of 49 patients, 8 (16.3%) patients did not have any adverse effects. However, 17 (34.7%) patients had paresthesia, 16 (32.7%) patients had dysgeusia, 12 (24.5%) patients had lethargy, 10 (20.4%) patients had anorexia, followed by nausea (10.2%) and polyuria (10.2%) (Figure-8).
*Multiple responses
4. Discussion
Idiopathic intracranial hypertension (IIH) is a syndrome characterized by increased intracranial pressure of unknown cause, occurring most commonly in obese women of childbearing age [11]. Acetazolamide (AZM) is commonly used to treat idiopathic intracranial hypertension (IIH), but there is insufficient information to establish a basis of evidence for its use among Bangladeshi population. This present study was designed to evaluate the visual outcome of patient with idiopathic intracranial hypertension (IIH) treated with oral acetazolamide. A total of 49 patients of idiopathic intracranial hypertension, who were treated with acetazolamide (500 mg twice daily) were followed to assess the reduction of intracranial pressure (ICP)/symptoms/signs and to evaluate the visual outcome. Data were collected at baseline, 3 months and 6 months after starting acetazolamide therapy. The parameters assessed were papilledema grading, perimetric mean deviation (PMD) and best corrected visual acuity (BCVA). In this study, the mean age of the study patients was 25.3±8.7 years which ranged from 15 years to 44 years. It was reported that, idiopathic intracranial hypertension (IIH) is predominantly a disease of younger adults [5]. A retrospective study of Hatem CF et al. among Danish population found the mean age at diagnosis was 29.5 years [9]. Another multicenter trial of Smith SV and Friedman DI also observed the average age was 29 years [6]. These findings were consistent with the present study. In this current study, 83.7% of the participants were female and two third of the study patients had over weight, mean body mass index (BMI) was 29.3±5.4 kg/m2 (ranged from18.2 kg/m2 to 38.3 kg/m2). It was documented that, the incidence of IIH is highest among young overweight women [6, 9]. In this study, patients often presented with one or more symptoms of headache, transient visual obscurations, and pulsatile tinnitus. Alterations in visual function may include subjective blurred vision, visual field defects, and binocular diplopia [6]. Most of the patients (95.9%) of this present study had headache. Almost half of the study patients had nausea (53.1%) and double vision (46.9%). 32.7 % patients presented with transient vision loss; while tinnitus (12.2%), dimness of vision (8.2%) and low back pain (4.1%) were also complained by some patients. These findings were consistent with related previous studies [6, 7, 11, 16]. In this current study all patients presented with CSF opening pressure more than 250 mm of H2O and mean CSF pressure of the study patients was found 323.7±46.1 mm of H2O which ranged from 260.0 mm of H2O to 420.0 mm of H2O. These results were supported by a couple of previous study [17, 18]. In this study out of 49 patients; nasal or temporal defect was present in 44.9% patients in their right eye and 49.0% patients in their left eye, enlarged blind defect was present in 34.7% patients in both eyes and concentric constricted visual field was also present among 16.3% patients in their right eye and 12.2% patients in their left eye. The reported most common field defects were enlarged blind spots, arcuate defects, nasal steps, and global constriction of the visual fields [2]. It was also documented that enlarged blind spot was the most common perimetric findings [11]. In this study, the baseline value of perimetric mean deviation (PMD) at right eye was -4.86dB. After treatment with acetazolamide, the PMD reduced to -2.93dB and -2.28dB at 3 months and at 6 months respectively. Similarly, the baseline value of perimetric mean deviation (PMD) at left eye was -4.07dB. After treatment with acetazolamide, the PMD reduced to -2.68dB and -2.38dB at 3 months and at 6 months respectively. The main reduction of PMD was observed at 3rd month. The PMD of both eyes reduced significantly at 6 months follow up periods. Mean changes of PMD in right eye was 2.59dB and fellow eye was 1.69dB over six months follow up. In a previous study it was found that mean improvement of mean deviation in study eye was 1.43dB and 0.87dB in fellow eye [6]. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee (2014) reported that mean improvement was significantly greater in the acetazolamide group than the placebo group at 6 months [19]. It was reported that permetric mean deviation (PMD) significantly improved after treatment of IIH with acetazolamide from -7dB to -2dB [20]. Majority of the patients of the present study had initial PMD >-2.27dB. Therefore, the improvement of PMD of this present study was consistent with related previous studies [19, 20]. In this current study, before starting acetazolamide treatment 28.6% study patients had grade 2 papilledema and 32.7% patients had grade 5 papilledema in their right eyes while 34.7% patients had grade 2 papilledema and 30.6% patients had grade 5 papilledema in their left eyes. After acetazolamide treatment significant visual improvement was observed; as 75.5% and 71.4% study patients had grade 0 papilledema in their right and left eyes respectively. However, grade 2 papilledema was found in right eye of 4 (8.2%) patients and in left eye of 6 (12.2%) study patients at final follow up periods, but 8 (16.3%) study patients had stage 1 papilledema in both eyes at final follow up periods. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee (2014) stated that acetazolamide treatment was associated with a significant reduction in papilledema grades [19]. Papilledema can improve by a reduction in CSF pressure or by decreasing loss of optic nerve axons [19]. A case series reported that three patients suffering from IIH were completely free of signs and symptoms after 3 months of treatment with 1000 mg of Diamox (Acetazolamide) each day [13]. Regarding measurement of central visual function, visual acuity is relatively unaffected in IIH unless the optic disc edema is so extensive that it also involves the macula, or if optic nerve ischemia occurs [6]. In this study, mean BCVA in log MAR unit significantly reduced after treatment with acetazolamide. However, the NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee (2014) found no significant difference in visual acuity at 6 months compared to baseline [19]. This achievement might be due to the fact that 5 study patients had >0.48 BCVA at baseline. In this study, the most common side effects of acetazolamide (AZM) were paresthesia (34.7%) and dysgeusia (32.7%) followed by lethargy, anorexia, nausea and polyuria. In this context related previous studies stated that the most common side effects of acetazolamide (AZM) are paresthesia followed by fatigue and gastrointestinal symptoms [21, 22]. Paresthesia, dysgeusia and possibly fatigue are likely dose-dependent phenomena and may thus be avoidable by using low-dose AZM and respond to dose reduction; on the other hand, some gastrointestinal symptoms may reflect local irritation and thus be improved by administering AZM with food. As headache and transient obscuration of vision is the first presenting symptoms of IIH and oral acetazolamide effectively reduce these features with improve visual outcome. Oral acetazolamide may be the first line of treatment in alleviating symptoms and signs with improvement of visual outcome in patients with IIH.
Conclusion
This study demonstrated that, idiopathic intracranial hypertension (IIH) is prevalent in over-weight/obese women of reproductive age. Headache, nausea, double vision, transient vision loss, tinnitus, dimness of vision and low back pain are the presenting features of IIH. Analysis of the findings of this study revealed that, oral acetazolamide 500 mg twice daily is effective in reduction of symptoms/signs and improvement of visual outcome with minimum side effects among patients having idiopathic intracranial hypertension.
Limitations of the study
It was a single centre study with a relatively small sample size. In this study only mean values were compared, individual analysis was not done.
Recommendation
Further large scale study should be done by using different doses of acetazolamide to assess its efficacy in idiopathic intracranial hypertension (IIH). A multicentre study with long term follow-up is recommended to assess the recurrence of the disease after withdrawal of the drug.
Conflicts of interest
All authors declared that they have no conflict of interest regarding this publication.
References
- Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 59 (2002): 1492-5.
- Ambika S, Arjundas D, Noronha V. Clinical profile, evaluation, management and visual outcome of idiopathic intracranial hypertension in a neuro-ophthalmology clinic of a tertiary referral ophthalmic center in India. Annals of Indian Academy of Neurology 13 (2010): 37.
- Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri: population studies in Iowa and Louisiana. Archives of Neurology 45 (1988): 875-7.
- Acheson JF. Idiopathic intracranial hypertension and visual function. British medical bulletin 79 (2006): 233-44.
- Ball AK, Clarke CE. Idiopathic intracranial hypertension. The Lancet Neurology 5 (2006): 433-42.
- Smith SV, Friedman DI. The idiopathic intracranial hypertension treatment trial: a review of the outcomes. Headache: The Journal of Head and Face Pain 57 (2017): 1303-10.
- Mezaal M, Saadah M. Idiopathic intracranial hypertension in Dubai: nature and prognosis. Acta neurologica scandinavica 112 (2005): 298-302.
- Thurtell MJ, Wall M. Idiopathic intracranial hypertension (pseudotumor cerebri): recognition, treatment, and ongoing management. Current treatment options in neurology 15 (2003): 1-2.
- Hatem CF, Yri HM, Sørensen AL, et al. Long-term visual outcome in a Danish population of patients with idiopathic intracranial hypertension. Acta Ophthalmologica 96 (2018): 719-23.
- Pollak L, Zohar E, Glovinsky Y, et al. Reevaluation of presentation and course of idiopathic intracranial hypertension–a large cohort comprehensive study. Acta Neurologica Scandinavica 127 (2013): 406-12.
- Wall M, Kupersmith MJ, Kieburtz KD, et al. The idiopathic intracranial hypertension treatment trial: clinical profile at baseline. JAMA neurology 71 (2014): 693-701.
- Randhawa S, Van Stavern GP. Idiopathic intracranial hypertension (pseudotumor cerebri). Current opinion in ophthalmology 19 (2008): 445-53.
- Tomsak RL, Niffenegger AS, Remler BF. Treatment of pseudotumor cerebri with Diamox (acetazolamide). Journal of Neuro-Ophthalmology 8 (1988): 93-8.
- Bruce BB, Preechawat P, Newman NJ, et al. Racial differences in idiopathic intracranial hypertension. Neurology 70 (2008): 861-7.
- Scott CJ, Kardon RH, Lee AG, et al. Diagnosis and grading of papilledema in patients with raised intracranial pressure using optical coherence tomography vs clinical expert assessment using a clinical staging scale. Archives of Ophthalmology 128 (2010): 705-11.
- Radhakrishnan K, Thacker AK, Bohlaga NH, et al. Epidemiology of idiopathic intracranial hypertension: a prospective and case-control study. Journal of the neurological sciences 116 (1993): 18-28.
- Wall M, White W. Asymmetric papilledema in idiopathic intracranial hypertension: prospective interocular comparison of sensory visual function. Investigative ophthalmology & visual science 39 (1998): 134-42.
- Kesler A, Hadayer A, Goldhammer Y, et al. Idiopathic intracranial hypertension: risk of recurrences. Neurology 63 (2004): 1737-9.
- Wall M, McDermott MP, Kieburtz KD, et al. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. Jama 311 (2014): 1641-51.
- Mikkilineni S, Trobe JD, Cornblath WT, et al. Visual field mean deviation at diagnosis of idiopathic intracranial hypertension predicts visual outcome. Journal of neuro-ophthalmology: the official journal of the North American Neuro-Ophthalmology Society 39 (2019):186.
- Schmickl CN, Owens RL, Orr JE, et al. Side effects of acetazolamide: a systematic review and meta-analysis assessing overall risk and dose dependence. BMJ open respiratory research 7(2020): 000557.
- Cello KE, Keltner JL, Johnson CA, et al. NORDIC Idiopathic Intracranial Hypertension Study Group. Factors affecting visual field outcomes in the idiopathic intracranial hypertension treatment trial. Journal of Neuro-Ophthalmology 36 (2016): 6-12.