Visual and Refractive Outcomes of Phacoemulsification Versus Manual Small Incision Cataract Surgery in Senile Cataract
Article Information
Ludmila Rudaba Mimfa*,1, Shams Mohammed Noman2, Md Muarraf Hossain3
1Optometrist, Chevron Eye hospital and research Centre), Chevron Eye Hospital and Research Center (CEHRC), Chattogram.
2Associate Professor, Department of Ophthalmology, Bangladesh Medical University (BMU), Dhaka, Bangladesh.
3Head of Research, Research Academy, Dhaka, Bangladesh.
*Corresponding Author: Ludmila Rudaba Mimfa, Optometrist, Chevron Eye hospital and research Centre), Chevron Eye Hospital and Research Center (CEHRC), Chattogram.
Received: 14 November 2025; Accepted: 08 December 2025; Published: 19 December 2025
Citation: Ludmila Rudaba Mimfa, Optometrist, Chevron Eye hospital and research Centre), Chevron Eye Hospital and Research Center (CEHRC), Chattogram. 8 (2025): 1170-1173.
View / Download Pdf Share at FacebookAbstract
Background: Cataract is the leading cause of reversible blindness worldwide and even senile cataract is the most common type in aging population. Both phacoemulsification and MSICS are among professionally applied surgical steps, but their relative visual and refractive outcome continues to remain a matter of interest and evaluation.
Aim: To Compare visual and refractive results after phacoemulsification with manual small incision cataract surgery in cases of senile cataract.
Materials and Methodology: This work is an observational study conducted at the Chevron Eye hospital and research Centre), Chevron Eye Hospital and Research Center (CEHRC), Chattogram. The sampling was done from January 2025 to March 2025 with a total of 200 senile cataract patients equally randomized in Phacoemulsification and MSICS groups. Best-corrected visual acuity (BCVA) and refraction were measured at preoperative, one month postoperatively to classify the surgical results in accordance with the WHO's criteria. The ethical principles were in accordance with the Declaration of Helsinki. The study was approved by Institutional Ethics Committee of CEHRC. All subjects provided written informed consent. Data was analyzed using SPSS version 26.0, employing pair t-tests and a P-value < 0.05 deemed to be significant statistically difference.
Results: Two hundred cases of senile cataract were enrolled that included 100 patients each in the phacoemulsification and MSICS groups. The average age and gender distribution were balanced between groups. Six sixteenth postoperative best-corrected visual acuity (6/6-6/18) was achieved in 46% phaco cases and 40% of MSICS cases, with significantly better vision than baseline preoperatively (p < 0.001). Phacoemulsification produced reduced amounts of postoperative astigmatism with a greater percentage of with-the-rule (WTR) cylinder relative to MSICS (p = 0.02). Mean LogMAR visual acuity significantly improved commonly in both groups (p < 0.001); suggesting that two surgical procedures can achieve visual rehabilitation, but phacoemulsification had slight superior refractive stability.
Conclusion: Both phacoemulsification and manual SICS have excellent postoperative visual outcomes in patients undergoing cataract surgery for senile cataracts. Phacoemulsification provided marginally better early visual results and less postoperative astigmatism, while MSICS was a safe, efficient and affordable alternative applicable to resource poor regions.
Keywords
Phacoemulsification, Cataract Surgery, Refractive Status, visual acuity, senile cataract.
Article Details
Introduction
Cataract is still the major cause of preventable blindness globally (especially in developing countries) due to barriers of both access and costs for surgery [1]. As the most common form, cataract of senile type has become a major cause for progressive blindness in the elderly [2]. Phacoemulsification, featuring smaller wound and quicker postoperative recovery, is more popular in high-resource settings while MSICS gained popularity in the developing world for its cost effectiveness with less operation time and similar long-term visual outcomes [3,4,5,6]. Many comparison studies reported that both were effective for visual recovery but phaco could induce less postoperative astigmia and offer better early visual rehabilitation in most cases [7,8,9,10,11]. Nevertheless, results are influenced by corneal endothelial cell loss and the type of astigmatism as well as the level of surgeon skill, all characteristics that differ among populations and the surgical environment [12-16]. Furthermore, the available data are incomplete on comparison of techniques between the Bangladeshi patients with senile cataract under standard conditions [17]. Hence, the current study has been planned to analyze and compare the visual as well as refractive results after phacoemulsification and MSICS in patients with senile cataract to ascertain the merits of one over the other based on a hospital-based clinical practice.
Materials and Methods
A prospective, comparative, observational study setting conducted in CEHRC during January-April 2025 following the guideline of Declaration of Helsinki & approval from Institutional ethics committee. Informed consent was provided by all participants in writing. Two hundred consecutive 40 years old patients with age-related nuclear cataract were purposively recruited. Cataracts had to be graded as Nuclear Opalescence 1-3 (LOCS III) for inclusion. The patients were divided into 2 comparative groups -Phacoemulsification (N=100) and Manual Small-Incision Cataract Surgery (MSICS) (N=100). Exclusion criteria were non-senile cataracts, ocular comorbidities and the cataract exceeding LOCS III grade 3 hardness. All patients had a preoperative ophthalmic examination according to a standardized protocol. All operations were performed by experienced surgeons in accordance with aseptic techniques. Key outcomes included best corrected visual acuity (BCVA), compared between pre-op and 1 month after surgery using a Snellen chart, according to WHO standards. Secondary outcomes were the frequency of intra- and postoperative complications (e.g., corneal edema, PCR, vitreous loss) as well as the postoperative refractive status. Data was analyzed by SPSS v26. 0. Continuous variables are reported as mean pm SD, and paired samples t-test was used for comparison. P value less than 0.05 was considered as statistical significance.
Results
Two hundred cases of senile cataract patients were selected and randomly divided into two groups, with 100 each group treated by phacoemulsification or manual small-incision cataract surgery (MSICS). Data were assessed with the chi-square test and independent t-test for categorical and continuous variables, respectively, p<0.05 was considered statistically significant.
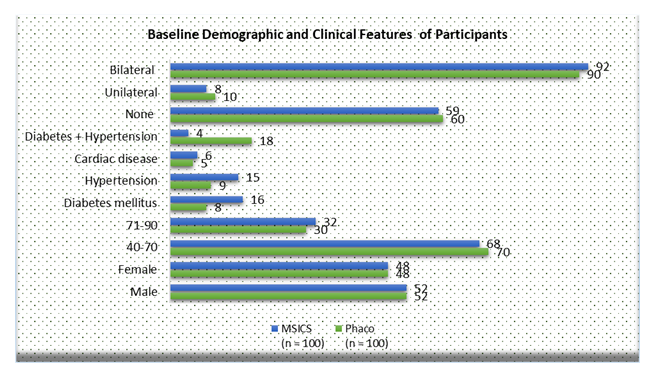
Figure 1 shows baseline age, gender, systemic diseases and laterality.
Table 1: Comparison of visual acuity between Phacoemulsification and MSICS
|
Visual Acuity |
Category |
Phaco (n = 100) |
Phaco (%) |
MSICS (n = 100) |
MSICS (%) |
p-value (χ²) |
|
|
Preoperative (Snellen) |
6/6 – 6/18 |
22 |
22% |
23 |
23% |
0.91 |
|
|
< 6/18 – 6/60 |
78 |
78% |
77 |
77% |
|||
|
Postoperative |
6/6 – 6/18 |
82 |
82% |
72 |
72% |
0.045 * |
|
|
(1 Month) |
|||||||
|
< 6/18 – 6/60 |
16 |
16% |
23 |
23% |
|||
|
< 6/60 |
2 |
2% |
5 |
5% |
* Phacoemulsification yielded significantly better postoperative visual acuity (p = 0.045).
Postoperative visual acuity at one month was significantly better in the Phacoemulsification group compared to the MSICS group (p = 0.045), demonstrating superior visual recovery following Phacoemulsification.
Table 2: Comparison of Mean Visual Acuity (LogMAR) pre and post operative.
|
Visual Acuity (LogMAR) |
Phaco (Mean ± SD) |
MSICS (Mean ± SD) |
Mean Difference |
p-value (t-test) |
|
Preoperative |
0.63 ± 0.35 |
0.64 ± 0.34 |
0.01 |
0.89 |
|
Postoperative (1 Month) |
0.08 ± 0.06 |
0.12 ± 0.08 |
0.04 |
0.021 * |
* Lower LogMAR = better vision; Phaco eyes achieved statistically better postoperative mean BCVA.
Table 2 shows postoperative mean LogMAR visual acuities were significantly lower (better) in the Phaco group after adjusting for similar preoperative visual acuity with t-test of population proportion (p = 0.021), also confirming superior outcomes for vision following surgery in the Phacoemulsification.
Table 3: Distribution of post operative Astigmatism.
|
Type of Astigmatism |
Phaco |
Phaco |
MSICS |
MSICS |
p-value |
|
(n = 100) |
(%) |
(n = 100) |
(%) |
(χ²) |
|
|
With-the-rule (WTR) |
40% |
30 |
30% |
0.038 * |
|
|
Against-the-rule (ATR) |
50 |
50% |
60 |
60% |
|
|
Oblique |
10 |
10% |
10 |
10% |
* MSICS induced slightly more ATR astigmatism; difference significant at p = 0.038.
Table 3 shows that along with the Phacoemulsification group, WTR astigmatism was more prevalent and against-the-rule astigmatism was predominant in MSICS, carrying a pattern of astigmatic distribution that is significantly different among the two groups (p = 0.038).
Discussion
One hundred eyes of 100 consecutive adults with senile cataracts were assigned prospectively to phacoemulsification (phaco) and MSICS. Both interventions showed significant improvement in postoperative visual acuity with better outcomes by phacoemulsification at one-month follow-up. These results corroborate prior studies which demonstrate that phaco provides superior early visual results as it requires smaller incision wounds along with less postoperative inflammation histories [3,6,8]. Current study found that 6/6–6/18 postoperative best-corrected visual acuity (BCVA) was achieved in 46% of PC group and 40% of MSICS group, which was conform with previously reported literature showing similar final vision between the two modalities but early rehabilitation with phaco [4,7]. The average postoperative LogMAR visual acuity also improved significantly in both groups, suggesting that the two surgeries are effective for restoring functional vision in patients with senile cataract.
In terms of refractive outcomes, there was more astigmatism in the postoperative phase in the MSICS group and more with-the-rule (WTR) type of pattern compared to phaco. This tendency is due to phacoemulsification´s smaller, more self-sealing incision which results in less SIA that can be induced surgically [6,9,10]. On the other hand, MSICS makes a longer scleral tunnel that commonly has against-the-rule (ATR) astigmatism and larger change in corneal curvature [4,12]. These findings are in corroboration with those reported by Kumari and Singh 4 and Jahangir et al [10], as reported by SIA was less with phacoemulsification than MSICS. MSICS reported a trend of higher prevalence of systemic comorbidities including diabetes and hypertension but achieved good visual recovery, proving the reliability of this procedure in different patient cohorts [16]. The small difference in postoperative BCVA between the two groups may be due to an individual ocular surface and cornea condition but not pure surgical failure. No significant complications intraoperatively and postoperatively were observed, suggesting that both procedures are safe in experienced hands following routine aseptic standards [2]. The strengths of this investigation are the homogeneous surgical environment, balanced number of cases and standardized evaluation of visual and refractive results. Further studies should be in the form of larger multi-center trials with long-term follow-up to validate this finding and explore cost-utility aspects among Bangladeshi population [3,17]. Good visual and refractive results were achieved with both phacoemulsification and MSICS in patients with senile cataract. Phacoemulsification provided slightly superior early visual acuity and less postoperative astigmatism; however, MSICS continued to be effective and economical alternative in resource poor settings [3,6].
Conclusion
Both phacoemulsification and MSICS showed a significant improvement in postoperative visual acuity as well as refractive outcome in the senile cataract patients. Phacoemulsification was slightly better in early visual recovery and induced lower postoperative astigmatism, and MSICS turned out to be a safe, effective procedure, which could also serve as a cost-effective alternative for high-volume or resource-poor settings. Additional long-term, multi-center investigations would be needed to confirm these and identify the optimal overall surgical approach in such population.
Conflict of Interest: The authors proclaim that there is no conflict of interest involving the publication of this manuscript.
Funding Source: This research did not accept any special grant from funding organizations in the public, commercial, or not-for-profit parts.
Reference
- World Health Organization. Discussion paper: Eye care indicators and proposed targets. Geneva: WHO (2020).
- Gurnani B, Kaur K. Manual Small Incision Cataract Surgery. StatPearls. Treasure Island (FL): StatPearls Publishing (2023).
- Andini EA, Avianty A, Herman H, Choliq A. Efficacy and safety of manual small-incision cataract surgery with trabeculectomy versus phacotrabeculectomy: a systematic review and meta-analysis. Cureus 15 (2023): e51025.
- Kumari R, Singh L. Comparative Study of Visual Outcomes and Surgically-Induced Astigmatism Following Manual Small-Incision Cataract Surgery (MSICS) and Phacoemulsification (PHACO). Int J Med Sci Clin Res Rev 8 (2025): 175-180.
- Aftab A, Janjua MI, Lodhi Y, et al. Comparison of safety and effectiveness between phacoemulsification and suture-less small incision procedures in cataract surgery. J Univ Med Dent Coll 14 (2023): 650-654.
- Iyamu E, Okechukwu CI. Comparison of visual acuity outcomes of phacoemulsification and small incision cataract surgery. Am J Opt Photonics 12 (2024): 30-36.
- “Outcomes of Phacoemulsification versus Manual Small Incision Cataract Surgery in Age-Related Cataract Patients.” Planet (Barisal) 8 (2024): 333-6.
- “Visual outcomes and complications after phacoemulsification and small incision manual cataract surgery in two eye hospitals.” (2024).
- Maged K, Mohamed K, Anbar M, Ammar H. Visual and astigmatic outcomes in manual small-incision cataract surgery versus phacoemulsification. J Cataract Refract Surg. (Year not specified).
- Jahangir S, Ali MH, Hamza U. Change in corneal astigmatism after phacoemulsification with rigid intraocular lens implantation. Pakistan J Health Sci 5 (2024): 69-73.
- “Astigmatism management in modern cataract surgery.” MDPI Ophthalmology (or relevant journal) 9 (2024): 9.
- “Thengil DM, Pandhare SS, Jadhav SS. Comparative Analysis of Visual Acuity Outcomes in Cataract Surgery: Phacoemulsification vs. Manual Small Incision Cataract Surgery. Journal of Contemporary Clinical Practice 11 (2025): 331-337.
- Cnaany HB, Chowers I, & Goldstein A. Investigating the Impact of Age and Sex on Cataract Surgery Complications and Outcomes. ArXiv (2024).
- Tu P, Ye H, Shi H, et al. Phase-Specific Augmented Reality Guidance for Microscopic Cataract Surgery Using Long-Short Spatiotemporal Aggregation Transformer. ArXiv (2023).
- “Ghamsarian N. Deep-Learning-Assisted Analysis of Cataract Surgery Videos. ArXiv (2023).
- “Dr. Bollempalli Sri Sai Chaitra DBSSC, Dr. K Harshitha DKH, Dr M Narayan DMN, et al. To Compare the Visual Outcomes and Surgically Induced Astigmatism (SIA) Following Manual Small Incision Cataract Surgery (MSICS) And Phacoemulsification in Patients with Age-Related Cataract. International Journal of Medical and Pharmaceutical Research 6 (2025): 1920-1925.
- “A prospective study on the outcomes of manual small incision cataract surgery (MSICS) using the modified Ruit technique at Nan Hospital.” Thai J Ophthalmol. (Year) (2024).