Validation of CTP, MELD & MELD Na Scoring Systems for Predicting Treatment Outcome of Cirrhotic patients in Bangladesh- An observational study
Article Information
Syeda Nur-E-Jannat*, 1, Dewan Saifuddin Ahmed2
1Assistant Professor, Department of Gastroenterology, Dhaka Medical College, Dhaka, Bangladesh
2Professor, Department of Gastroenterology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
*Corresponding author: Syeda Nur-E-Jannat. Assistant Professor, Department of Gastroenterology, Dhaka Medical College, Dhaka, Bangladesh
Received: 14 April 2023; Accepted: 19 April 2023; Published: 26 April 2023
Citation: Syeda Nur-E-Jannat, Dewan Saifuddin Ahmed. Validation of CTP, MELD & MELD Na Scoring Systems for Predicting Treatment Outcome of Cirrhotic patients in Bangladesh- An observational study. Fortune Journal of Health Sciences. 6 (2023): 182-190.
View / Download Pdf Share at FacebookAbstract
Background: Cirrhosis of liver is a very common medical problem. There is no satisfactory curative treatment option for end stage liver disease (ESLD) other than liver transplantation (LT). Due to scarcity of liver donors worldwide, a good prognostic model predicting highest risk of dying and to prepare a ‘priority list’ in waiting list candidates is essential for proper timing of LT to reduce mortality and improve success rate.
Objectives: The aim of this study was to evaluate the validity of Child-Turcotte-Pugh (CTP), MELD and MELD Na score for predicting treatment outcome (1 month, 3-month, 6-month mortality) of cirrhotic patients in Bangladesh.
Methods: This was an observational study conducted at Bangabandhu Sheikh Mujib Medical University, Dhaka, from April 2012 to March 2014. Total 92 patients with cirrhosis (mean age 48.7±12.3 yrs) were prospectively evaluated and followed up for 6 months and outcome were assessed as 1 month, 3 month and 6 month mortality. CTP, MELD, MELD Na score were calculated at baseline. Receiver operating characteristic (ROC) curves were used to determine the cutoff values for each score with the best sensitivity and specificity in discriminating between patients who survived and those who died.
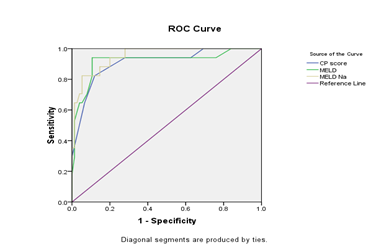
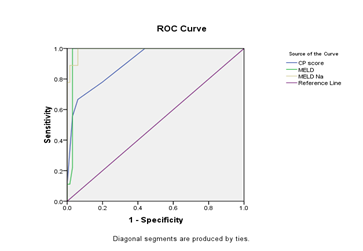
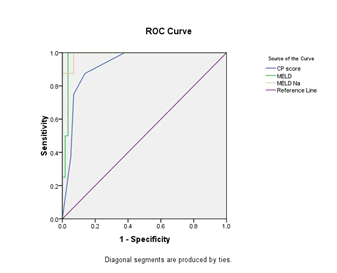
Results: Total 92 patients with liver cirrhosis were enrolled. The mean age of the patients was 48.7±12.3 yrs with a range of 18-68 yrs. ROC curve showed area under curve (c- statistics) for CTP, MELD and MELD Na score. For 1 month mortality cut off value of CTP, MELD, MELD Na score was 10.5, 20, 18 respectively with a sensitivity of 64.7%, 76.5%, 88.2% and specificity 93.3%, 90.7 %, 89.3 % respectively. For 3 month mortality cut off value of CTP, MELD, MELD Na score was 10.5, 19 and 18 with a sensitivity of 66.7% 77.8%, 88.9% and specificity of 93.9%, 93%, 93.7% respectively. For 6 month mortality cut off value of CTP, MELD, MELD Na score was 11.5, 18.5 and 18 with a sensitivity of 62.5%, 87.5%, 87.5% and specificity of 94.8%, 89.7%, and 92.6% respectively. MELD Na had the highest AUC in predicting 1 month, 3 month and 6 month mortality among all prognostic models.
Conclusions: CTP, MELD, MELD Na scores were good prognostic model to predict 1 month, 3 month and 6 month mortality. MELD Na was found to be the best predictor with highest AUC.
Keywords
Child-Turcotte-Pugh (CTP), MELD, MELD Na, Cirrhosis, Chronic liver disease, Liver Transplantation (LT)
Article Details
1. Introduction
End-stage liver disease (ESLD) results from a variety of hepatic insults like viral hepatitis, alcohol and metabolic liver discuses. There is no specific treatment apart from management of its complications. Only Liver transplantation (LT) prolongs survival and improves the quality of life [1]. Due to paucity of liver donors worldwide, a good prognostic model identifying patients at highest risk of dying from ESLD is essential. The Child-Turcotte-Pugh (CTP) score has been widely used over 40 years for prognostication of patients with cirrhosis [2]. However, subjectivity of some parameters and the discontinuous scale on which other parameters are scored has limited its ability to discriminate [2, 3]. The model for end-stage liver disease (MELD) score was introduced in 1999. It was first developed to predict 3-months mortality in patients undergoing transjugular intrahepatic portosystemic shunt [4]. MELD score is now widely used in Western countries to determine the prognosis of patients with cirrhosis [5, 6]. In February 2002, United Network of Organ Sharing (UNOS) replaced CTP score with MELD score for waiting list prioritization [7].Subsequently it was found thatcirrhosis with persistent ascites and hyponatremia, had a higher mortality than that predicted by the MELD score alone [8-12]. Ascites and low serum Na were independent predictors of mortality in patients with low MELD score (<21) [9]. "MELD-Na" score was first established in 2006 [11]. Studies in Koren and Hongkong both confirmed that MELD-Na performed better than MELD in predicting 3-months and 1- year mortality [13, 14].
The spectrum of liver disease seen in Asia is different from that in Western countries. In Bangladesh, nearly 20 million people were suffering from chronic liver diseases, about 15 million hepatitis-B virus related, 800,000 people from hepatitis-C virus [15]. Viral hepatitis is the commonest aetiology in Asia-Pacific region including Bangladesh whereas in Western country alcohol is the commonest cause. For an underdeveloped country like Bangladesh, considering the difference in aetiology of cirrhosis, difference in socioeconomic status, nutritional status, BMI of people, treatment facilities between the people of Bangladesh and that of Western country, the natural course of the disease and life expectancy of cirrhotic patients of our country can also be different.
The applicability of CTP, MELD, MELD Na score as a prognostic marker has not yet been evaluated in Bangladeshi patients with cirrhosis. This study is intended to evaluate the CTP, MELD and MELD Na score in predicting short term and long-term outcome (1 month, 3-month and 6 month mortality) in cirrhotic patients of Bangladesh. This current analysis may provide a road map for issues to be considered in future.
2. Objective of the Study
The aim of this study was to evaluate the validity of CTP, MELD and MELD Na score (cut off value with specificity, sensitivity, accuracy, PPV, NPV) for predicting treatment outcome (1 month, 3 month, 6 month mortality) of cirrhotic patients in Bangladesh.
3. Materials and Methods
This was an observational study conducted at Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh, from April 2012 to March 2014. Total 92 patients with cirrhosis (mean age 48.7±12.3 yrs) were prospectively evaluated and followed up for 6 months and outcome were assessed as 1 month, 3 month and 6 month mortality. Adults aged 18 years and above, diagnosed as cirrhosis of liver by clinical, biochemical, ultrasonography, fibroscan of liver and endoscopic findings were included in this study. Patients with hepatocellular carcinoma (HCC), other comorbidities like Diabetes Mellitus (DM), Chronic kidney disease (CKD), Chronic obstructive pulmonary disease (COPD), Ischemic heart disease (IHD), malignancy (non hepatic), pregnancy and who quit regular follow up upto 6 months or till death were excluded from this study. In all patients a detailed clinical examination, grade of encephalopathy, severity of ascites was documented. Serum bilirubin, serum albumin, serum creatinine, serum electrolyte, prothrombin time with INR were done during admission prior to inclusion in the study and also during follow up. A detailed evaluation for aetiology of cirrhosis were also done. The whole procedure was explained to patients and informed written consent was taken.
Severity of liver disease was calculated according to CTP, MELD and MELD-Na score. CTP score were calculated on the basis of the presence and severity of ascites and hepatic encephalopathy, the prolongation of prothrombin time, the level of serum bilirubin and albumin. MELD score were calculated with serum creatinine, bilirubin and INR using the online calculator available at the Mayo clinic website (http://www.mayoclinic.org/gi-rst/mayomodel7.html). MELD Na score was then calculated using the formula MELD-Na = MELD + 1.59 x (135 - Na).11 For analysis (to asses mortality), patients were categorized into two groups CTP ≤ 9, CTP > 9, MELD & MELD-Na score < 20 & ≥ 20. All patients were followed up at 1 month, 3 month and 6 month or till death and during each follow up were divided into two groups - those who died due to hepatic failure due to liver cirrhosis and those who survived.
All data were entered into Statistical Packages for the Social Sciences (SPSS 17) software for analysis. Continuous variables were expressed as mean with standard deviation and categorical variables as count with percentage. Groups were compared using Student’s t-test for continuous variables, and chi-squared test for categorical variables. Receiver-operating characteristic (ROC) curves were used to determine the cut off values of CTP score, MELD score, MELD Na score with the best sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV) and accuracy in discriminating between patients who survived and those who died.
4. Observations and Results
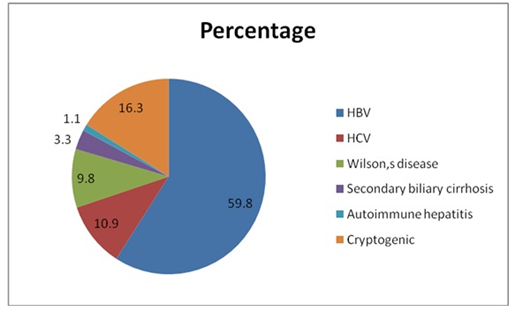
Total 92 patients were enrolled in this study. The mean age of patients was 48.7±12.3 yrs. Among them, 29 (31.5%) patients were between 41-50 yrs and 22 (23.9%) were between 31-40 yrs. Only six (6.5%) patients were younger than 20 yrs. 73 (79.3%) patients were male. The most common aetiology was HBV related cirrhosis (59.8%) followed by HCV (10.9%), Wilson’s disease (9.8%), secondary biliary cirrhosis (3.3%), autoimmune hepatitis (1.1 %). Cryptogenic cirrhosis constituted 16.3% cases. (Figure 1)
During 6 months of follow up, out of 92 patients total 34 patients died of which 17 patients died within 1st month, 9 patients died within 2nd to 3rd month, 8 patients died within 3 months to 6 months.(Table -1). The number of patients and the mortality in each CTP, MELD and MELD-Na classes are shown in Table 2. The higher the score, the greater the risk of death. After enrollment of each patient, 1 month, 3 month and 6 month mortality was predicted considering a reference cutoff value of CTP, MELD and MELD Na score of 1 month, 3 month and 6 month mortality respectively (Table 3-5). Predicted death were compared to actual death which was statistically significant between the specific cut off values. The higher score, greater the risk of death.
Table 1: Treatment outcome (mortality) at different follow up (n=92)
|
Mortality |
Number of Patients |
Outcome |
|||
|
Death |
Alive |
||||
|
|
n |
% |
n |
% |
|
|
1st month |
92 |
17 |
18.5 |
75 |
81.5 |
|
3rd months |
75 |
9 |
9.8 |
66 |
71.7 |
|
6th months |
66 |
8 |
8.7 |
58 |
63 |
Table 2: distribution of mortality in different classes of CTP, MELD and MELD Na score (n=92).
|
Total patients (n=92) |
No of died (n=34) |
P value |
|
|
CTP |
n % |
n % |
|
|
A-B (≤ 9) |
55 59.8 |
4 7.3 |
0.001s |
|
C (> 9) |
37 40.2 |
30 81.1 |
|
|
MELD |
|||
|
< 20 |
57 61.9 |
9 15.8 |
0.001s |
|
≥ 20 |
35 38.1 |
25 71.4 |
|
|
MELD Na |
|||
|
< 20 |
46 50 |
3 6.5 |
0.001s |
|
≥ 20 |
46 50 |
31 67.4 |
s= significant
P value reached from Z test
Table 3: distribution of predicted mortality and actual death according to reference cut-off value of CTP, MELD, and MELD Na score at 1 month follow up (92).
|
At 1 month |
Outcome |
p-Value |
|
|
CTP |
Death (n=17) |
Alive (n=75) |
|
|
>9.5 |
16 |
21 |
0.001s |
|
≤9.5 |
1 |
54 |
|
|
MELD |
|||
|
>17 |
16 |
8 |
0.001s |
|
≤17 |
1 |
67 |
|
|
MELD Na |
|||
|
>18 |
16 |
21 |
0.001s |
|
≤18 |
1 |
54 |
|
s=significant, p-value reached from chi-squared test
Table 3 shows that for 1 month mortality considering the cut-off value of CTP score of 9.5. [16], 37 patients had CTP score > 9.5 (predicted death), of which 16 patients died (actual death) within 1 month, 21 patients survived. With CTP score ≤9.5, 54 patients remained alive, and only 1 died. Considering the cut-off value of MELD score 17, [16] 24 patients had MELD score > 17 (predicted death); among them, 16 patients died (actual death), and 8 patients survived. With MELD score ≤17,67, patients remain alive and only 1 died. Considering the cut-off value of MELD Na score 18.16, 37 patients had MELD Na score > 18 (predicted death); among them, 16 patients died (actual death). 21 patients survived. With MELD Na score ≤18, 54 patients remain alive and only 1 died. The higher the score, the greater the risk of death.
Table 4: Distribution of predicted mortality and actual death according to reference cut off value of CTP, MELD, MELD Na score at 3 month follow up (n=75)
|
At 3 month |
Outcome |
p-Value |
|
|
CTP |
Death (n=9) |
Alive (n=66) |
|
|
>9.5 |
7 |
13 |
0.001s |
|
≤9.5 |
2 |
53 |
|
|
MELD |
|||
|
>18.6 |
7 |
2 |
0.001s |
|
≤18.6 |
2 |
64 |
|
|
MELD Na |
|||
|
>18.6 |
8 |
3 |
0.001s |
|
≤18.6 |
1 |
63 |
|
s=significant, p-value reached from chi-squared test
Table 4 shows that for three months of mortality, considering the cut-off value of CTP score 9.5. [17], 20 patients had CTP>9.5 (predicted death), but actual death was 7. Patients with CTP score ≤9.5, 53 remained alive, and only two died. Considering the cut-off value of the MELD score 18.6. [17], nine patients had MELD > 18.6 (predicted death), but actual death was 7. With MELD scores ≤18.6, 64 patients remained alive, and only two died. Considering the cut-off value MELD Na score of 18.6. [17], 11 patients had MELDNA score > 18.6 (predicted death), but actual death was 8. Patients with MELD Na score ≤ 18.6, 63 remained alive, and only one died. The higher the score, the greater the risk of death.
Table 5: Distribution of predicted mortality and actual death according to reference cut off value of CTP, MELD, MELD Na score at 6 month follow up (66)
|
At 6 month |
Outcome |
p-Value |
|
|
CTP |
Death (n=9) |
Alive(n=66) |
|
|
>10 |
6 |
4 |
0.001s |
|
≤10 |
2 |
54 |
|
|
MELD |
|||
|
>17.9 |
8 |
2 |
0.001s |
|
≤17.9 |
0 |
56 |
|
|
MELD Na |
|||
|
>19 |
7 |
2 |
0.001s |
|
≤19 |
1 |
56 |
|
s=significant, p-value reached from chi-squared test
Table 5 shows that for 6-month mortality, considering the cut-off value of CTP score 10. [18], 10 patients had CTP> 10 (predicted death), but actual death was 6. Patients with CTP score ≤ 10, 54 remained alive and only 2 patients died. Considering the cut-off value of MELD score 17.9. [18], 10 patients had MELD> 17.9 (predicted death), but actual death was 8. All (56) patients with MELD score ≤17.9 remained alive. For 6 month mortality with the cut-off value MELD Na score 19. [18] 9 patients had MELD Na> 19, and were expected to have death after 6 months (predicted death), but actual death was 7. Patients with MELD Na scores ≤19, 56 remained alive, and only 1 patient died. The higher the score, the greater the risk of death.
Table 6: Comparison of CTP, MELD and MELD Na score between death and alive patients at different follow up (n=92).
|
Follow up |
Outcome |
p-Value |
|
|
Death |
Alive |
||
|
CTP |
Mean±SD |
Mean±SD |
|
|
1 month |
11.76±1.52 |
8.55±1.85 |
0.001s |
|
3 month |
11.11±1.45 |
8.08±1.69 |
0.001s |
|
6 month |
11±1.07 |
7.97±1.68 |
0.001s |
|
MELD |
|||
|
1 month |
23.71±6.03 |
13.84±3.55 |
0.001s |
|
3 month |
22±4.24 |
13.29±2.92 |
0.001s |
|
6 month |
21.88±2.59 |
13.43±2.56 |
0.001s |
|
MELD Na |
|||
|
1 month |
34.37±12.09 |
15.76±5.21 |
0.001s |
|
3 month |
35.07±10.15 |
13.98±3.25 |
0.001s |
|
6 month |
36.78±9.06 |
14.25±3.34 |
0.001s |
s=significant, p-value reached from chi-squared test
Table 6 shows the mean CTP, MELD and MELD Na scores in those who survived and those who died. The mean CTP score was significantly lower in patients who survived (8.55±1.85, 8.08 ±1.69, 7.97±1.68 at 1 month, 3 month and 6 month) compared to those who died (11.76±1.52, 11.11±1.45, 11±1.07 at 1 month, 3 month and 6 month) respectively (P<0.001). The mean MELD score was also significantly lower in those who survived (13.84 ± 3.55, 13.29±2.92, 13.43±2.56 at 1 month, 3 month and 6 month respectively) than in those who died (23.71±6.03, 22±4.24, 21.88 ± 2.59 at 1 month, 3 month and 6 month respectively) (P<0.001). The mean MELD Na score was also significantly lower in those who survived (15.76 ± 5.21, 13.98±3.25, 14.25±3.34 at 1 month, 3 month and 6 month respectively) than in those who died (34.37±12.09, 35.07±10.15, 36.78±9.06 at 1 month, 3 month and 6 month respectively) (P<0.001).
Table 7: Sensitivity, specificity, accuracy, PPV, NPV of CTP, MELD, MELD Na score to predict mortality with the best predictive cut offs at 1, 3 & 6 month
|
Score |
Cut off |
AUC |
Sensitivity (%) |
Specificity (%) |
Accuracy (%) |
PPV (%) |
NPV (%) |
|
|
1 month |
CPT |
10.5 |
0.922 |
64.7 |
93.3 |
88 |
68.8 |
92.1 |
|
MELD |
20 |
0.978 |
76.5 |
90.7 |
88 |
65.0 |
94.4 |
|
|
MELD Na |
18 |
0.991 |
88.2 |
89.3 |
89.1 |
65.2 |
97.1 |
|
|
3 month |
CPT |
10.5 |
0.903 |
66.7 |
93.9 |
90.7 |
60.0 |
95.4 |
|
MELD |
19 |
0.974 |
77.8 |
93 |
90.9 |
63.6 |
96.4 |
|
|
MELD Na |
18 |
0.992 |
88.9 |
93.7 |
93.1 |
66.7 |
98.3 |
|
|
6 month |
CPT |
11.5 |
0.09 |
62.5 |
94.8 |
90.9 |
62.5 |
94.8 |
|
MELD |
18.5 |
0.918 |
87.5 |
89.7 |
89.4 |
53.8 |
98.1 |
|
|
MELD Na |
18 |
0.951 |
87.5 |
92.6 |
91.9 |
63.6 |
98.0 |
AUC=Area under the ROC curve, PPV= Positive predictive value, NPV= Negative predictive value
For 1 month mortality cut-off value of CTP score is 10.5 with a sensitivity 64.7%, specificity 93.3%. cut-off value of MELD score is 20 with a sensitivity 76.5%, specificity 90.7%; the cut-off value of MELD Na score is 18 with a sensitivity 88.2%, specificity 89.3%. MELD Na had the highest AUC (0.991) followed by MELD (0.978), CTP (0.922). For 3 month mortality cut-off value of CTP score is 10.5 with a sensitivity 66.7%, specificity 93.9%; cut off value of MELD score is 19 with a sensitivity 77.8%, specificity 93%; cut off value of MELD Na score is 18 with a sensitivity 88.9%, specificity 93.7%. MELD Na had the highest AUC (0.992) followed by MELD (0.974), CTP (0.903). For 6 month mortality cut-off value of CTP score is 11.5 with a sensitivity 62.5%, specificity 94.8%; cut-off value of MELD score is 18.5 with a sensitivity 87.5%, specificity 89.7%, cut off value of MELD Na score is 18 with a sensitivity 87.5%, specificity 92.6%. MELD Na had the highest AUC (0.951) followed by MELD (0.918), CTP (0.09). The positive predictive value was low and negative predictive value was high at 1 month, 3 month and 6 month.
5. Discussion
Predicting the survival of patients with cirrhosis is essential because LT is considered when the anticipated mortality without transplantation exceeds 50% at 1 year [19]. However, transplantation is not always fully successful because of adverse effects or complications after transplantation. The reported 1-year survival rate is 70%-80%. So, it is the important to be able to predict precisely the natural course of liver cirrhosis and to compare the risks and benefits of LT with those of the natural disease course. Proper timing of transplantation increases the success rate of the procedure. According to Organ Procurement and Transplantation Network (OPTN) database, in United States, the median MELD score was 15 (range 6 to 40) in patients who were registered on the waiting list for LT. In Japan, a significant survival benefit of LDLT was observed in patients with MELD score ≥15 (P=0.0181) and significantly more risk with transplantation was observed in those with MELD score <15 compared with that of patients in whom the disease followed its natural course (P =0.0168) [20]. Accurate prediction of short term mortality by different prognostic models can also reduce 15% mortality on waiting list candidates21 and facilitate equal access of organs across all transplant centers.
In this study, total 92 patients with liver cirrhosis were enrolled with mean age of 48.7±12.3 yrs and range 18-68 yrs. Half (55.4 %) of patients were in the age range of 31-50 yrs. It was consistent with another prospective study where the mean age of the patients was 46.97±12.96 years and 50% of patients were in the age range of 41-60 yrs [22]. A study conducted in Bangladesh showed that most cirrhotic patients were in the age group 41-50 years, comprising 31% of cases [23]. In a large population-based cohort study showed that cirrhosis was highest at the ages of 40-60 years [24]. In another cohort study, the median age was 54.3 years (range 31-72) [16].
In this study, 73 (79.3 %) patients were male and 19 (20.7 %) were female. It is consistent with another prospective study where 75% of the patient was male [22]. In another study in Bangladesh, there were 258 (88%) males and 35 (12%) females [23]. Cirrhosis was approximately twice as high for men than for women of all ages [24]. Male was also predominant in another cohort study with 201(78.5%) men and 55 (21.5%) women [16]. In this study the viral hepatitis was the most common aetiology (HBV 59.8 %, HCV 10.9%). In China HBV (61.3% ), HCV (15.2%) [16], in Japan HBV ( 70% ), HCV ( 30 % ) [17]. This differs from the aetiology in western country where alcoholic cirrhosis is the commonest cause; 79% in Denmark [24], 86.4% in France [18], 60.9% in South Asian non-Moslem male [25], 50% in Mumbai [22].
In this study, the mean CTP was significantly lower in patients who survived compared to those who died at 1-month, 3-month and 6-month follow-up (e.g., CTP 8.55±1.85 Vs 11.76±1.52 at 1-month, 8.08±1.69 Vs 11.11±1.45 at 3-month and 7.97±1.68 Vs 11.11±1.07 at 6-month (P<0.001). This is consistent with another study where the mean CTP score was significantly lower in patients who survived (8.3±2.3) compared to those who died (10.9± 1.8) (P<0.05) [22]. In another study also showed that mean CTP among those who survived (7.5± 1.8) and those who died (9.4±2.4) was also statistically significantly different (P=0.002) [26].
In this study, the mean MELD scores were significantly lower in patients who survived compared to those who died at 1-month, 3-month and 6-month follow-up (e.g., MELD 13.84±3.55 Vs 23.71±6.03 at 1-month, 13.29±2.92 Vs 22±4.24 at 3-month and 13.43±2.56 Vs 21.88±2.59 at 6-month (P<0.001). This is consistent with another study where the mean MELD score was also significantly lower in those who survived (14.9±6.4) than in those who died (22.0±7.7) (P<0.05) [22]. In another study, a similar result was found with the mean MELD score among those who survived and died was 13.2±5.9 Vs 17.2±7.4 (P=0.002) [26]. In patients with alcoholic hepatitis, the median MELD score (29.5 Vs 22.0 P=.001) was higher in patients who died within 6 months [27].
In this study, the mean MELD Na scores were significantly lower in patients who survived compared to those who died at 1-month, 3-month and 6-month follow-up (e.g. MELD Na 15.76±5.21 Vs 34.37 ± 12.09 at 1-month, 13.98 ± 3.25 Vs 35.07 ± 10.15 at 3-month and 14.25±3.34 Vs 36.78±9.06 at 6-month (P<0.001). In patients with alcoholic hepatitis, the mean MELD Na score (34.0 Vs 24.5; P=0.03) were higher in patients who died within six months [27]. Accurate prognostic indicators for the survival of cirrhotic patients are essential and helpful in guiding clinical decisions. In our study, by measuring the area under the ROC curve, we compared the predictive accuracy among the CTP, MELD, and MELD Na systems for 1-month, 3-month and 6-month mortality in cirrhotic patients. Using the most discriminative cut-off value from the ROC curve for different models, the chance of survival over a certain period of time (3 or 6 months) can be predicted. For patients with a score lower than the selected cut-off, survival is quite high even without transplantation.
In this study, for 1-month mortality, the cut-off value of the CTP score was 10.5, with a sensitivity of 64.7% and specificity of 93.3%. In another study for 1 month mortality, the CTP cut-off value was 9.5, with a sensitivity of 68.9% and a specificity of 69.2% [16]. Here for 1 month mortality the cut-off value of the MELD score was 20, with a sensitivity of 76.5% and specificity of 90.7%. In another study, for 1 month mortality, the cut-off value for MELD was 17, with a sensitivity of 72.1 and specificity of 83.1%. [16] The cut-off value of the MELD Na score was 18, with a sensitivity of 88.2% and specificity of 89.3%.
In this study, for 3-month mortality, the cut-off value of the CTP score was 10.5, with a sensitivity of 66.7% and specificity of 93.9%. This is consistent with another study where for 3-month mortality, the CTP cut-off value was 9.5 with a sensitivity of 67.1% and specificity of 69.4%.16 The cut-off value of the MELD score was 19, with a sensitivity of 77.8% and specificity of 93%. This is consistent with another study where for 3-month mortality, the cut-off value of the MELD score was 18.6 with a sensitivity of 71% and specificity of 82% [17]. Similar result was found the in another study, the cut-off value of MELD score was 17.5 with a sensitivity 71.1%, specificity 87.2%.16 The cut-off value of the MELD Na score was 18, with a sensitivity of 88.9% and specificity of 93.7%. This is consistent with another study where for 3-months mortality, the cut-off value of MELD Na score was 18.6 with a sensitivity of 83% and specificity of 70% [17].
According to table 6, at 3 month of follow up, there is a significant difference in the MELD score between surviving (13.29±2.92) and the patients who died (22±4.24) and that of MELD Na score (13.98±3.25 Vs 35.07±10.15). Here we find that there was a significant difference in mortality rate in patients with MELD score >19 and MELD Na score > 18 as compared to that in patients with MELD score <19 and MELD Na score < 18.
In this study, for 6-month mortality cut-off value of the CTP score was 11.5, with a sensitivity of 62.5% and a specificity of 94.8%. In another study, the best cut-off for the prediction of 6-month mortality was 10 for the CTP [18]. The cut-off value of the MELD score was 18.5, with a sensitivity of 87.5% and specificity of 89.7%. This is consistent with another study where for 6-month mortality, the cut-off value of the MELD score was 18.6 with a sensitivity of 57% and specificity of 85% [17]. In another study, the best cut-off for MELD was 17.9 for 6-month mortality [18]. The cut off value of MELD Na score was 18 with a sensitivity of 87.5% and specificity of 92.6%. This is consistent with another study where for 6 months mortality with the cut off value of MELD Na score was 18.6 with a sensitivity of 75% and a specificity of 75% [17]. In another study the best cut-off for the MELD Na was 19.0 [18].
In this study, these models typically had a consistently low positive predictive value (53.8-68.8 %) but high negative predictive value (92.1-98.3%), this might be a useful strategy in selecting transplant candidates. This finding implicates that chance to survive over a certain period of time (1, 3 or 6 months) for patients with a score lower than the selected cut off is quite high even without transplantation. In this study, a patient with CTP <15 would have a 94.8% chance of survival at 6 month without a LT. This finding is close to findings of another study with the cut-off value of CTP (<10); there is 94.4% chance of survival at 6 month without a LT [18].
In this study, a patient with a MELD score of <19 would have a 96.4 % chance of survival at 3-month and MELD score of 18 (<18.5) have 98.1 % chance of survival at 6-month without a LT. These findings are consistent with other findings where a patient with a MELD score of 18 (< 18.6) would have a 96% and 89% chance of survival at 3 and 6 months respectively [17]. In another study MELD (<17.9) has 87.9% chance of 6-month survival without LT [18].
In this study, a patient with MELD Na score of <18 would have a 98.3 % and 98% chance of survival at 3 and 6 months, respectively, without LT. A similar result was found in another study with MELD Na score of 18 (<18.6) would have a 97% and 92% chance of survival at 3 and 6 months, respectively, without a LT [17]. In another study, without LT, 6-month survival for MELD Na (<19) was 92.6 %. [18]. This information is crucial for transplant physicians in making decisions to avoid futile LT.
In this study, MELD Na had the highest AUC at 1-month, 3-month and 6-month. At 1-month, MELD Na had the highest AUC (0.991), followed by MELD (0.978) and CTP (0.922). In another study using 1-month mortality as the end-point, the AUC was 0.819 for the MELD score and 0.722 for the CTP score [16]. In this study, for 3-month mortality MELD Na had the highest AUC (0.992), followed by MELD (0.974) and CTP (0.903). In another study, at three months, the AUC was 0.820 for the MELD score and 0.721 for the CTP score [16]. AUC was also higher for MELD Na (0.801), followed by MELD (0.773) for three months of mortality [17]. In this study, for 6-month mortality MELD Na had the highest AUC (0.951) followed by MELD (0.918) and CTP (0.09). In another study, at six months AUC for MELD-Na (0.778) was higher than MELD (0.735) [17].
6. Conclusion
Most patients were young adult (4th to 5th decade) with male predominance. HBV was the commonest aetiology which differs from the western world.The study result concluded that there is a significant difference in CTP, MELD, and MELD Na scores in patients who survived and who died. The higher score, the higher risk of death. For CTP, MELD and MELD Na score, above the specific cut-off value probability of survival was significantly reduced. For 1 month mortality, cut off value of CTP, MELD, MELD Na score was 10.5, 20, 18 respectively with a sensitivity of 64.7%, 76.5%, 88.2% & specificity 93.3%, 90.7%, 89.3% respectively. For 3 month mortality cut off value of CTP, MELD, MELD Na score was 10.5, 19 and 18 with a sensitivity of 66.7%, 77.8 %, 88.9% and specificity of 93.9%, 93%, 93.7% respectively. For 6 month mortality cut off value of CTP, MELD, MELD Na score was 11.5, 18.5 and 18 with a sensitivity of 62.5%, 87.5%, 87.5% and specificity of 94.8%, 89.7%, 92.6% respectively. CTP, MELD, and MELD Na had the same efficacy and in some cases, even better effectiveness among our population. MELD Na was found to have the highest AUC.
Limitations
- The study period was short.
- Sample size was small.
- Cirrhosis due to Non-alcoholic steatohepatitis (NASH), Alcohol, primary biliary cirrhosis (PBC), primary sclerosing cholangitis (PSC) and haemochromatosis were not found during this study period and were not included in this study.
Ethical issue: This study was approved by institutional review board (IRB) of BSMMU.
References
- Belle SH, Porayko MK, Hoofnagle JH, Lake JR & Zetterman RK. Changes in quality of life after liver transplantation among adults. National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Liver Transplantation Database (LTD). Liver Transplantation and Surgery 3 (1997): 93-104.
- Oellerich M, Burdelski M & Lautz HU. Assessment of pre-transplant prognosis in patients with cirrhosis. Transplantation 51 (1991): 801-6.
- Shrestha R, McKinley C & Showalter R. Quantitative liver function tests define the functional severity of liver disease in early-stage cinhosis. Liver Transplantation and Surgery 3 (1997): 166-73.
- Kamath PS, Wiesner RH & Malinchoe M. A model to predict survival in patients with end-stage liver disease. Hepatology 33 (2001): 464-70.
- Giannini E, Botta F & Testa R. Utility of the MELD score for assessing 3-month survival in patients with liver cirrhosis: one more positive answer. Gastroenterology 125 (2003): 993-4.
- Dunn W, Jamil LH, Brown LS, Wiesner RH, Kim WR & Menon KV. MELD accurately predicts mortality in patients with alcoholic hepatitis. Hepatology 41 (2005): 353-8.
- Cholangitas E, Mareli L & Shusang V. Systemic review of performance of MELD in setting of liver transplantation. Liver Transplantation 12 (2006): 523-529.
- Ruf AE, Kremers WK, Chavez LL., Descalzi VI, Podesta LG & Villamil FG. Addition of serum sodium into the MELD score predicts waiting list mortality better than MELD alone. Liver Transplantation 11 (2005): 336-43.
- Heuman DM, Abou-Assi SG & Habib. A Persistent ascites and low scrum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology 40 (2004): 802-10.
- Biggins SW, Rodriguez HJ, Becchetti P. Bass NM, Roberts JP & Terrault NA. Serum sodium predicts mortality in patients listed for liver transplantation. Hepatology 41 (2005): 32-9.
- Biggins SW, Kim WR, Terrault NA, Saab S, Hadan V, Schiano T, et al. Evidence-based incorporation of serum sodium concentration into MELD. Gastroenterology 130 (2006): 1652-1660.
- Srikureja W, Kyulo NL, Runyon BA & Hu KQ. MELD score is a better prognostic model than Child-Turcotte-Pugh score or Discriminant Function score in patients with alcoholic hepatitis. Journal of Hepatology 42 (2005): 700-706.
- Kim SY, Yim HI, Lee J, Lee BJ, Kim DI, Jung SW, et al. Comparison of CTP, MELD, and MELD-Na scores for predicting short term mortality in patients with liver Cirrhosis. Korean Journal of Gastroenterology 50 (2007): 92-100.
- Wong VW, Chim AM, Wong GL., Sung JJ & Chan HL. Performance of the new MELD-Na score in predicting 3-month and 1-year mortality in Chinese patients with chronic hepatitis B. Liver Transplantation 13 (2007): 1228-1235.
- Khan M. 35 mln people suffer from liver disease in Bangladesh. The Independent newspaper 28 (2010): 14.
- Xiao-Hui LV, Hong-Bo L, Ying W. Bing-Yuan W, Min S & Ming-Jun S. Validation of model for end-stage liver disease score to serum sodium ratio index as a prognostic predictor in patients with cirrhosis. Journal of Gastroenterology and Hepatology 24 (2009): 1547-1553.
- Huo TI, Chei Lin H. Hou SC, Lee PC & Wu JC. Comparison of Four Model for End-Stage Liver Disease-Based Prognostic Systems for Cinhosis. Liver tramplantation 14 (2008): 837-844.
- Boursier J,Cesbron E, Tropet AL Pilette C Comparison and Improvement of MELD and Child- Turcotte-Pugh Score Accuracies for the Prediction of 6-month Mortality in Cirrhotic Patients. Journal of Clinical Gastroenterology 43 (2009): 580-585.
- Collier JD & Webster G. Liver and biliary tract disease in N R. Colledge. B R. Walker & S H. Ralston (eds). Davidson's principles and practice of medicine. Churchill Livingstone Elsevier. Edinburgh (2010): 976.
- Ishigami M, Honda T, Okumura A. Ishikawa T, Kobayashi M, Katano Y, et al. Use of the Model for End-Stage Liver Disease (MELD) score to predict 1-year survival of Japanese patients with cirrhosis and to determine who will benefit from living donor liver transplantation. Journal of Gastroenterology 43 (2008): 363-368.
- Wiesner RH, Freeman RB & Mulligan DC. Liver transplantation for hepatocellular cancer: the impact of the MELD allocation policy. Gastroenterology 127 (2004): 261-7.
- Mishra P, Desai N, Alexander J, P-singh D and Sawant P. Applicability of MELD as a short-term prognostic indicator in patients with chronic liver disease: An Indian experience. Journal of Gastroenterology and Hepatology 22 (2007): 1232-1235.
- Islam N, Khan M and Ahmed Z. Cirrhosis of liver. Bangladesh Medical Research Council Bulletin (1981); VII (2).
- Fialla AD. Ove B, Muckadell SD & Lassen AT. Incidence, etiology and mortality of cirrhosis: a population-based cohort study. Scandinavian Journal of Gastroenterology 47 (2012): 702-709.
- Dodus MA. Cox, Iqbal TH and Cooper BT. Ethnic differences in cirrhosis of the liver in a british citty: Alcoholic cirrhosis in south asian man. Alcohol & Alcoholism 38 (2003): 148-150.
- Gotthardt D, Weiss KH & Baumgartner M. Limitation of the MELD score in predicting mortality or need for removal from waiting list in patients awaiting liver transplantation. BMC Gastroenterology 9 (2009): 72.
- Brianna E.V, Asrani SK, Dunn W. Kamath PS and Shah VH. Influence of Serum Sodium on MELD-Based Survival Prediction in Alcoholic Hepatitis. Mayo Clinic Proceedings 86 (2011): 37-42.