Utilization of Cervical Cancer Screening and Its Associated Factors among Women aged 25-49 Years in Kaloleni Sub-County, Kilifi County
Article Information
Emmanuel Moffat Onduko1*, George Makalliwa1, Caroline Musita1
1School of Public Health, Department of Environmental Health and Disease Control, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
*Corresponding author: Mr. Emmanuel Moffat Onduko, BSc in Medical Laboratory Sciences MSc. Public health student at the School of Public Health, , Department of Environmental Health and Disease Control, Jomo Kenyatta University of Agriculture and Technology, Nairobi, Kenya
Received: February 01, 2025 Accepted: February 10, 2025 Published: February 28, 2025
Citation:
Emmanuel Moffat Onduko, George Makalliwa, Caroline Musita. Utilization of Cervical Cancer Screening and Its Associated Factors among Women aged 25-49 Years in Kaloleni Sub-County, Kilifi County. Journal of Cancer Science and Clinical Therapeutics 9 (2025): 27-41.
View / Download Pdf Share at FacebookAbstract
Background: Cervical cancer causes a significant number of deaths and morbidity among women. The aim of the study was to determine utilization of cervical cancer screening and its associated factors among women in Kaloleni Sub-County of Kilifi County aged between 25 and 49 years. Methods: A health facility-based descriptive cross-sectional study in five medical facilities was undertaken in Kaloleni Sub-County. 217 women filled the questionnaire, in depth interviews was done on 20 healthcare workers and health facility assessment. Descriptive statistics and chi-square analysis were utilized to explore the relationship between cervical cancer screening rates and various factors, including individual and healthcare facility characteristics. Content analysis was applied to identify important themes arising in qualitative data. Results: In a study of 217 women aged 25-49 in Kaloleni Sub-County, only 23% had undergone cervical cancer screening. Significant associations were found between screening utilization and geographical location residential area (p = 0.008), awareness of cervical cancer screening (p < 0.001), knowledge of symptoms (p < 0.001), and cost of screening (p < 0.001). Source of income (p = 0.021), while insurance cover (p = 0.030). In addition, health facility factors, such as service promotion (p < 0.001) and staff training adequacy (p < 0.001), significantly affected utilization. Health facility-level assessments determined a lack of advanced cervical cancer services. Conclusion: Cervical cancer screening rates are considerably low. Therefore, it is essential to introduce awareness initiatives, enhance access to screening via outreach activities, subsidize prices, strengthen the healthcare system, and offer patient centered training for healthcare professionals.
Keywords
Cervical cancer screening, Women, HPV, Kenya.
Cervical cancer screening articles; Women articles; HPV articles; Kenya articles
Article Details
Introduction
Cervical cancer is the fourth most leading cancer in women worldwide, indicating a serious public health concern, particularly in low- and middle- income countries. The 2022 GLOBOCAN report indicated there were 348,874 deaths and 662,301 new cases of cervical cancer in the year 2022 [1]. Cervical cancer screening rates in high-income European countries are notably high, varying between 80% and 98.4%, and in the United States, the rate is 72.4% [2, 3]. In contrast, countries in Africa exhibit alarming statistics, with 125,699 new cases and 80,614 deaths reported in 2022, alongside low screening rates across sub-Saharan Africa, from 0.7% in Benin to 45.9% in Namibia [4]. In Kenya, cervical cancer poses a major challenge, with 5,845 new cases and 3,591 deaths reported in 2022. This results in significant incidence and mortality rates of 32.8 and 21.4 per 100,000 women, respectively, making it the second most prevalent cancer among women [1]. Currently, 7.2 million women in Kenya within the ages of 25 to 49 are deemed at risk, yet only 17% of women of childbearing age have been reported to undergo cervical cancer screening [5]. Kenya's national cancer guidelines recommend that 70% of eligible women visiting medical facilities for routine care should be screened [6]. In Kaloleni Sub-County, there is a lack of reliable data on utilization of cervical cancer. This gap in screening adherence exacerbates the risk of late diagnosis, subsequently escalating treatment costs and mortality. Factors contributing to this low uptake include inadequate healthcare infrastructure, socioeconomic and sociocultural barriers, and individual perceptions of screening [7]. Cervical cancer arises from uncontrolled growth of abnormal cells in the cervix, caused by persistent Human Papillomavirus (HPV) infections. These high risk HPV persistent infections can ultimately lead to cervical intraepithelial neoplasia and cervical cancer [8]. HPV is mainly transmitted through sexual contact and risk factors include multiple sexual partners, high parity, the use of long-term hormonal contraceptives, HIV/ AIDS immunosuppression, and tobacco use [9]. Through widespread screening, vaccination, and treatment initiatives, the World Health Organization's 90-70-90 strategy seeks to considerably lower the prevalence of cervical cancer by 2030 [10]. This study aimed to explore these factors and barriers in Kaloleni Sub-County, and to provide insights into the individual level characteristics and health facility factors that hinder effective utilization cervical cancer screening and inform on suitable interventions required.
Materials and Methods
Study design and population
The purpose of this study was to examine the utilization of cervical cancer screening and its associated factors among women in Kaloleni Sub-County, Kilifi County, Kenya, using a health facility-based descriptive cross-sectional design. The period of data gathering in 2024 was June–August. Women were the intended audience. Who had been residing in Kaloleni Sub-County for a minimum of six months and were attending selected health facilities for outpatient services. Eligible participants were women willing to provide informed consent, in their first trimester of pregnancy. Women were excluded if they were unable to give consent, those diagnosed with cervical cancer, and those who underwent complete hysterectomy.
Sample size and sampling procedure
Fisher et al.'s method was used to determine the sample size of 217 in order to estimate the prevalence of cervical cancer screening among women aged 25–49 years in Kaloleni Sub-County, as well as to investigate factors associated with screening utilization. Purposive sampling was used to select five high-volume health facilities in Kaloleni Sub-County, ensuring diverse representation. A total of 41 health facilities were initially assessed, identifying those that had consistently high patient attendance. The final selected facilities included: Mariakani Sub-County hospital, Gotani health Centre, Mabati Medical Centre, Vishakani and Tsangatsini dispensaries. Systematic sampling was implemented to select 217 women attending outpatient services at these facilities, utilizing an interval of 16 and randomized starting points.
Data collection procedure
Data were collected using a semi-structured questionnaire adapted from previous studies [11-18]. The questionnaire comprised 50 items structured into two sections: Individual- level characteristics (predisposing, enabling, and need factors) and Health facility-level factors. Pre-testing was conducted with 10% of the sample size to validate the questionnaire’s clarity and relevance. The questionnaire and interview materials were translated into Kiswahili by bilingual experts, and back-translation was used for quality assurance. Three qualified research assistants collected the data by conducting in-person interviews and administered questionnaires. Each session lasted approximately 30 minutes and was conducted in either English or Kiswahili. Qualitative data were gathered from 20 healthcare workers, utilizing a key informant interview guide with 10 open-ended questions that it concentrated on knowledge and experiences related to cervical cancer screening. Purposively, four medical staff members from each of the five selected hospitals and interviewed for approximately 30 minutes. The selected sites were assessed using a health facility assessment tool, adapted from the WHO Harmonized Health Facility Assessment (HHFA) and aligned with Kenya’s National Cancer Control Strategy (2023-2027) and National Cancer Screening Guidelines (2018). Data were collected through interviews with the healthcare staff responsible for screening services.
Data management and analysis
Quantitative data were entered into Microsoft Excel 2021 and analyzed using SPSS Version 27. Descriptive statistics including (frequencies, percentages, and measures of central tendency) were calculated to summarize the data. The relationship between cervical cancer screening rates and various factors, including individual and healthcare facility characteristics, was assessed using chi-square. A p-value of less than 0.05 indicated a statistically significant association. Qualitative data transcripts were coded and analyzed using content analysis to identify trends and insights related to screening utilization. For health facility assessment simple statistics using Microsoft excel was used determine the number of cervical cancer screening services available at the selected health facilities. Key quotes from respondents and services availability were incorporated to support quantitative findings.
Ethical considerations
Ethical approval was obtained from the Institutional Ethics Review Committee at Jomo Kenyatta University of Agriculture and Technology (Reference number JKU/ ISERC/02317/1289), National Commission for Science, Technology, and Innovation (NACOSTI) (Reference number NACOSTI/P/24/35129) and Kilifi County (Reference number KLF/DOH/RESEARCH/VOL.1/142). Informed consent was secured from all participants, ensuring confidentiality by anonymizing responses.
Results
General characteristics of the study participants
The study's participation rate was 100%, with 217 women. Table 1 provides an overview of sociodemographic traits and awareness about cervical cancer and screening. The majority of participants in the research were from Mariakani Cervical cancer screening can detect (32.7%) and Christians (79.3%). The common age group

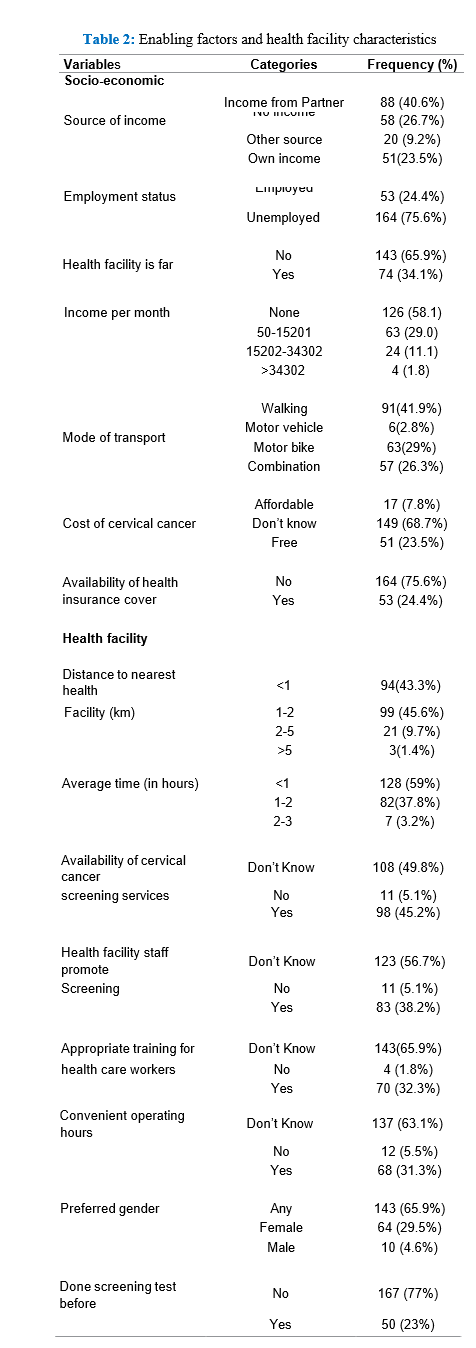
were between ages 25 and 29 (54.8%), and 54.8% had only completed primary school. Most participants (55.3%) knew what cervical cancer screening was, yet a significant portion (77%) had not yet undergone screening, despite 93.1% supporting regular screenings. Regarding enabling factors, most participants were unemployed (75.6%), relied on income from a partner (40.6%), and lived within 1-2 km of health facilities (45.6%) (Table 2). A large majority indicated the importance of regular screening for women's health (84.3%) (Table 3), as 49.8% were uninformed about cervical cancer availability at health facilities (Table 2).
Proportion of women aged 25-49 years utilizing cervical cancer screening
The study had 217 female participants in total. Table 4 shows that just 23% of respondents had ever undergone a cervical cancer screening. Healthcare workers have seen a worrying pattern in the low percentage of women in Kaloleni Sub-County who use cervical cancer screening programs. As one Healthcare worker stated, "Many women do not see the need for screening unless they have symptoms" (HCW 3).
Individual-level characteristics associated with the utilization of cervical cancer screening Predisposing Factors
Regarding the geographical location mentioned in Table 4, the high uptake witnessed at Mariakani can be explained by how close medical facilities are. There was correlation between geographical location and the use of cervical cancer services (p = 0.008). The availability of supplies and equipment contributes to high uptake. One HCW explained:

“In Mariakani sub-county hospital, we have most of the basic things that we normally use for screening” (HCW 19)
There was no correlation between the use of cervical cancer services and education, marital status, or religion (Table 4). Age groups and cervical cancer usage are significantly correlated at 5% level of significance (p = 0.003). Utilization is higher among older women. Women within the age groups of 35-39 have the highest proportion of those utilizing cervical cancer services at 47.8%.
The participants’ awareness of cervical cancer led to screening utilization (Table 5). This suggests that cervical cancer screening and knowledge of the disease's existence are significantly correlated. A p value of 0.000 supports the

assumption that there is correlation between being aware of cancer screening and utilization of screening services. According to some medical providers they had concerns on poor knowledge. This could be inferred from the following statement by a healthcare worker:
"Mostly knowledge gap, most women are not aware about cervical cancer, how they can be screened and what is the prevention strategy." (HCW 10)
There is a significant association between those aware about symptoms of cervical cancer and screening for cervical cancer at 5% level of significance (p < 0.001) (Table.5). Respondents who recognize foul vaginal smell as a symptom for cervical cancer are more 3 times likely to go screening compared to those who recognize vaginal bleeding as a symptom for cervical cancer (odds ratio of 3.704). Healthcare workers have emphasized on the lack of education regarding the risks associated with sexual behavior and its link to cervical cancer. The following statement was made by one HCW:
"Illiteracy, neglect. Unless they are sick and have a pelvic inflammatory disease, then you tell them and then they will do it. But they are not ready to come to hospital. I think they are not ready to take up screening of diseases." (HCW 8)
There was significant association between knowing if HPV causes cervical cancer and going for cervical cancer screening. Participants unaware of this relationship revealed an 81.7% non-utilization rate (p = 0.001, odds ratio of 0.224) (Table 5). Health care workers pointed that women who don’t know that HPV causes cervical cancer and those who don’t believe that HPV causes cervical cancer are less likely to go cervical cancer screening. One healthcare worker stated:
"They don't know that having more sexual partners is a risk factor in influencing or is a risk factor of getting the cervical cancer, whereby they don't know that men are the carriers of this HPV virus, thus they just engage in sexual activity without knowing that men are the carriers of this HPV virus." (HCW 19)

Knowledge about the ability of cervical cancer screening to detect cancer decreased the likelihood of non-utilization. Among those unaware, 92.2% did not utilize screening compared to 71.6% of those who acknowledged its efficacy (p = 0.005, odds ratio of 0.215) (Table 5). The healthcare workers indicated that most women are ignorant about cervical cancer screening. One healthcare worker remarked:
“I would say a bigger percentage of the women our community are not well educated per se. I would say maybe we have still a very big percentage of people who do not know cervical cancer screening.”(HCW 11)
Enabling Factors
There was a substantial correlation (p = 0.021) between screening use and income source (Table 5). Medical professionals noted that one of the reasons women were not screening for cervical cancer was financial restrictions. According to one healthcare worker,
“Many women in Kaloleni cannot afford the transport costs to reach the health facilities and also the services associated with cervical cancer screening due to high levels of poverty.” (HCW 2)
Employed categories are twice more likely to seek out cervical cancer screening services than jobless respondents (odds ratio of 2.12) (Table 5). Healthcare professionals emphasized how employment stability might affect health goals and service access. According to one HCW,
"Women in stable employment tend to do regular health screenings into their routines." (HCW 16)
The perceived cost of screening and its usage were shown to be significantly correlated (p < 0.001) (Table 5). According to the medical professionals, many women, particularly with very little income will not participate. A HCW confirmed this:
“They're thinking about the children rather than thinking about themselves. So, you realize that when it's time for them to come, maybe they take their time to come to the clinic. They start complaining, oh this is transport, this is money that I can buy food for my kids instead of just coming to the facility to check up on their health” (HCW 20)
Health insurance availability was significantly correlated with cervical cancer screening usage (p = 0.030) (Table 5). Many women do not utilize cervical cancer screening because of the costs lack health insurance. As one HCW worker explained,
“So, in my opinion, I think one of the main issues is lack of health insurance. Most patients are poor, as you know in this region poverty levels are very high, and therefore when they are told to pay for cervical cancer screening they will forgo the service” (HCW 14)
Need Factors
The perceptions of screening providing peace and uptake of cervical cancer screening was statistically significant (p = 0.003). The health workers highlighted that some women don’t want to do cervical cancer screening because they fear the results. The following statement was made by one HCW,
“Some of them are scared of the results, the outcome. What if they get cancer? Then what is next? And then you know, cancer has been associated with more of like a death sentence. So, they would rather not learn about it. They live with it, not knowing that they had cancer rather than they're told they have cancer and they cannot be able to take care of themselves when it comes to treatment.” (HCW 16)
For the belief that regular screening is important, those who responded "Don’t know" had a very high rate of non- utilization (97.1%) compared to those who recognized its importance (73.2%), and this difference was statistically significant (p = 0.002) (Table 5).The perspective shared by a healthcare provider sheds light on a common mindset regarding health screening behaviors. A healthcare provider noted that,
“In my experience in this health facility, most women, of course, are scared of cancer diagnosis. And it is common for people to say ignorance is bliss. And so, they would rather not know their diagnosis, because they fear it, because of what is the stigma associated with cancer. So, a lot of them would not voluntarily come.” (HCW 19)
Husband approval for screening was also significantly associated with utilization, as 88% of those uncertain about their husbands’ stance did not utilize screening, in contrast to only 63.5% of those whose husbands approved (p < 0.001) (Table 5). In light of cultural sensitivities surrounding gender and healthcare, it is essential for healthcare workers to approach patient interactions thoughtfully. They added that some women would be embarrassed no matter the sex of the health personnel. A response from healthcare provider emphasizes this:
“Women believe that you're not supposed to show your vaginal parts to any other person apart from your husband. So, they wait until the husband gives them a go ahead to go for cancer screening because they feel if they go against it, it's more like cheating to them because someone else has been able to see their private parts. And then it's even becoming worse when they come to the facilities and they get maybe the person attending to them is a male health care worker. So, it even becomes dificult for them to want to go ahead and do the test. So, for me, that is hindering them from getting the test” (HCW 15)
Health facility-level factors that affect the utilization of cervical cancer screening
There was a significant correlation (p < 0.001) between the availability of cervical cancer screening services in medical facilities and utilization of cervical cancer screening (Table 6). Health facility assessment as shown in table 7 indicates that there is access to VIA screening method in all the selected healthcare facilities; however, there is significant variation in cervical cancer services availability across healthcare facilities. Healthcare workers expressed their concerns regarding inadequate resources at screening facilities, highlighting the gap between available infrastructure and necessary medical equipment. One healthcare worker stated.
“I would say facility-based hindrances to screening services like shortage of supplies, shortage of equipment that is used in screening like speculums, examination tables, and examination lamps. We also have a knowledge gap for the providers. Not everyone has been trained on cervical cancer screening. So, I would say those are some of the facility- based and then availability of space too to provide such.” (HCW 15)
The convenience of operating hours was also significantly associated with screening utilization (p < 0.001) (Table 6). While 9.5% of individuals who did not know about the operating hours utilized this service, a statistically noteworthy 52.9% did when they were deemed convenient (OR = 0.093). Healthcare workers in Kaloleni Sub-County highlighted the challenges that limit access to care. One HCW reported,
"An example in hand is actually where I work, we have the equipment, the speculums and the brushes but we close at 5pm." (HCW 5)
According to table 6, the promotion of screening services by health facility staff significantly influenced utilization (p < 0.001). Only 8.1% of those who were unaware of this promotion utilized the services, while 45.8% of patients promoted by staff availed themselves of the screenings (OR = 0.105). Healthcare workers highlighted the importance of educational resources in promoting health awareness among women in communities. One HCW emphasized:
"Availability of educational posters is not adequate. So, if we have adequate educational posters, most women in communities can be aware of it and they come for screening themselves to the nearest facility." (HCW 18)
There was a statistically significant association between the perceived adequacy of health worker training and screening utilization (p < 0.001) as shown in table 6. A mere 9.1% of respondents who were uncertain about training adequacy used screening services, compared to 51.4% of those who perceived the training as adequate (OR = 0.094). Health facility assessment found that four out of five healthcare facilities had trained their staff on VIA in the past 2 years. Healthcare workers pointed out significant challenges in providing consistent care due to staffing issues such as lack of training. One healthcare worker stated,
“The trained personnel are an issue because not everyone is conversant with how the screening is done.” (HCW 4) Women of reproductive age who had done cervical cancer screening before had a profound impact on utilization (p < 0.001). Healthcare workers observed that prior experiences with health screenings significantly influence women's future screening behaviors. One HCW stated,
“Once they get a negative result they normally leave the facility when they are happy and you can tell that the patients would want to come on every other alternate time that they will be needed because the first result was a negative.” (HCW 17)

Health Facility Assessment
As indicated in summary table 7, the examination of the availability of cervical cancer services at the five selected medical facilities reveals significant patterns in the delivery of healthcare services. Although the five health institutions provide HPV vaccines and VIA screening, only one provides PAP smears, and only two provide cervical cancer treatment services, suggesting some limitations in access. Notably, there is no access to advanced services such as cervicography, HPV testing, LEEP treatment and colposcopy.

Discussion
Cervical cancer screening is a critical preventive measure that remains underutilized in many low-resource settings, as evidenced by alarming statistics from Kaloleni Sub- County, where only 23% of women aged 25-49 have used these services. Research findings reveal a complex landscape of barriers hindering access to cervical cancer, including individual-level characteristics and health facility-level constraints. Comparisons with other regions underscore a widespread issue of low screening uptake that reflects broader challenges in promoting preventive care. By identifying and discussing specific predisposing, enabling, and need factors that influence women's health-seeking behaviors, this analysis emphasizes the urgent need for targeted educational campaigns, systemic improvements in healthcare accessibility, and culturally sensitive strategies to enhance cervical cancer screening rates and strengthening healthcare infrastructure.
Proportion of women utilizing cervical cancer screening
Kaloleni Sub-County's results show that only 23% of women between the ages of 25 and 49 had utilized cervical cancer screening, reflecting a concerning trend that is consistent with similar studies in Kenya and across the region. For instance, a study in central Kenya reported that 25.6% of women had undergone cervical cancer screening, while national data indicated that only 17% of women of childbearing age were screened [13, 5]. In other countries; studies in South Africa, Ethiopia, Uganda, Nigeria, Ghana and Ethiopia respectively reported cervical cancer screening uptake rates of 35.5%, 22.9%, 20.6%, 18.4%, 24.6%, and 24% respectively, highlighting a persistent challenge in promoting preventive care among women [19-23, 17]. These figures demonstrate that low screening uptake is a prevalent issue across low- and middle-income countries. High-income countries, such as New Zealand and Australia, screening rates
reach as high as 95% [9], highlighting the stark disparity in cervical cancer prevention efforts. The healthcare worker's observation that many women only seek screening when symptomatic further supports global patterns, such as lack of awareness, cultural beliefs, and inadequate access to healthcare services hinder proactive health behaviors. This finding aligns with the studies examining barriers to cervical cancer screening [24, 25]. As a result, the low uptake in Kaloleni underscores the critical need for focused educational campaigns and community outreach initiatives that not only educate women about the value of routine screenings regardless of symptoms but also address particular societal and cultural barriers that prevent them from accessing these essential services.
Individual-level characteristics associated with the utilization of cervical cancer screening Predisposing Factors
The research reveals significant disparities in the use of cervical cancer screenings across women residing in the different administrative wards, with a marked contrast between areas like Kaloleni, where 83.9% of participants did not utilize screening, and Mariakani, with a utilization rate of 36.6% due to higher service availability. This finding aligns with existing literature that emphasizes the importance of geographic accessibility in health care, particularly in rural areas where healthcare resources are often limited [26]. The analysis showed that marital status did not have impact on utilization of cervical cancer screening, a finding that corroborates a study in Ghana [27]. There is correlation between age groups and utilization of cervical cancer where utilization is higher among older women above 39 years at 40% compared to women below 39 years at 20.8%, this is consistent with a studies in Ethiopia [18] and Nigeria [28] where the younger women do not identify themselves as at risk and do not take up the services. A study in Kenya [29] found that cervical cancer screening was higher among older women than young women. One possible explanation for this could be, women in this age range have a higher possibility of giving birth, having more gynecological exams, and they may have more frequent visits to healthcare facilities for antenatal and postnatal care. Religion was not statistically significant to utilization of cervical cancer screening. The utilization of cervical cancer screening was not correlated with the level of education. The results supported research conducted in Egypt and Nigeria that found no correlation between education level and use of cervical cancer screening [30]. Awareness about cervical cancer and its screening correlates strongly with screening rates; participants unaware of cervical cancer exhibited a 96.2% non-utilization rate, consistent with findings from Cameroon [31], respectively showing that knowledge gaps hinder engagement in preventive health behaviors. Moreover, understanding the link between HPV and cervical cancer significantly impacted attitudes towards screening, as those unaware reflected an 81.7% non-utilization rate, echoing a study which found that one of the main factors influencing screening acceptance was awareness [20].
Since 89.9% of non-users were not aware of the signs of cervical cancer, knowledge on about cervical cancer is crucial. This aligns with a study in Nigeria that indicated non-usage of cervical cancer screening was mostly among women who were ignorant on the symptoms and risk factors of cervical cancer. This emphasizes the need for targeted educational interventions [24].
Enabling factors
The screening rate was lower for women who depended on their partners' income (20.5%) compared to those with independent income sources (45%). This finding aligns with a past study on economic barriers to healthcare services [33]. The lower screening rates among women dependent on partners indicate that financial autonomy may empower women to prioritize their health. Financial constraints emerged as a significant barrier to screening, with many healthcare workers noting that high poverty levels hinder access to services. This observation resonates with findings, which identified inadequate health insurance as a primary impediment to timely cervical cancer screening [34]. Many women are kept away by the expenses associated with cervical cancer screening [16, 18]. The perceived affordability of screening influenced participation, where participants who found costs manageable had a significantly higher utilization rate (58.8%) compared to those who were unaware of costs (8.1%). This finding reflects similar concerns articulated in research highlighting that economic barrier can lead to advanced-stage diagnoses among underprivileged women [35]. Employment status also played a crucial role in screening utilization, with employed women exhibiting higher rates of participation (34.0%) compared to unemployed counterparts (19.5%). The positive correlation between job stability and health-seeking behavior aligns with findings in studies conducted in four sub-Saharan countries and Japan [36, 37], which indicated that employed women are more likely to engage in preventive health measures due to access of information about health issues from their employers. Stable employment allows women to incorporate health screenings into their routines and makes healthcare access more feasible [27].
Health insurance coverage was significantly associated with screening rates, revealing that women lacking insurance utilized screening services far less frequently (19.5%) compared to their insured peers (34.0%). This highlights a consistent theme from the literature, where a lack of insurance is identified as a critical barrier to accessing preventive healthcare services. Healthcare workers' insights reflect the apprehension many women feel about expenses associated with screenings, echoing findings which noted that financial concerns often deter women from seeking preventive care [38] The analysis of monthly income confirmed its relationship with screening uptake, revealing that women with no income had a utilization rate of only 13.8%. This resonates with studies showing that low-income status significantly impacts women's access to cervical cancer screening [4]. As articulated by healthcare workers, many women prioritize basic necessities over health screenings, reflecting broader socio-economic challenges faced by women in lower-income brackets [39]. The findings of this study highlight the significant role socio-economic factors play in influencing cervical cancer screening utilization in Kaloleni. Improving access to these vital health treatments requires addressing obstacles relating to insurance coverage, economic empowerment and budgetary limitations. to cervical cancer screening programs.
Need factors
The results demonstrate a significant association between women's perceptions of screening providing peace of mind and their actual utilization of screening services. Specifically, a notable difference was found between those who were uncertain about the reassurance provided by screening 2.8% participated in screening and those who believed it offered reassurance, 26.3% utilized cervical cancer screening. This aligns with a meta-analysis done on 72 studies spanning 34 countries, which indicated that women's decisions around cervical cancer screening are heavily influenced by their attitudes and beliefs [40] The data revealed that fear of cancer diagnoses remains a primary barrier to screening, echoing sentiments expressed by healthcare workers where patients often perceive it as a death sentence. Similarly, according to research conducted in Kenya, significant individual- level hindrances to cervical cancer screening were the fear and anxiety surrounding pelvic exams [41]. As highlighted in previous studies the negative societal labels attached to cervical cancer significantly deter women from engaging in prevention strategies [42, 7]. The positive belief in value of regular cervical cancer screening was critical. A startling 97.1% of respondents who were unsure of the significance of routine screening did not utilize the services, as opposed to 73.2% who acknowledged its significance. A study in Kenya found that women who had visited a medical institution during the previous 12 months were more likely to use cervical cancer screening [29]. This highlights the necessity of preventative health education initiatives at the medical facilities Husband approval emerged as a critical influencing factor, demonstrating a direct correlation with screening utilization rates. The analysis indicated that 88% of women who were unsure about their husbands’ stance on screening did not participate; contrasting sharply with the 63.5% of those whose husbands supported the idea. This is in line with studies conducted in low and middle countries that shows cervical cancer was viewed as private and taboo and lack of peer support [7].
The healthcare practitioners demonstrated how cultural perceptions of women's health decisions have a substantial impact on utilizing cervical cancer screening, making it important to navigate these cultural dynamics carefully. This finding reflects similar concerns articulated in research highlighting the effects of socio-cultural norms, gender prejudice, and partner and family influence also play a role in hindering healthcare choices [43]. In some studies cervical cancer screening has been associated with sexual transmission, with women attending screening assumed to be engaged in infidelity or promiscuity [7]. The discomfort surrounding the examination process remains a significant obstacle. Many women express embarrassment and anxiety about exposing themselves during screening, and this barrier is not easily surmountable. However, public health education can play a pivotal role in addressing these misconceptions and discomforts [39].
The study reveals significant gaps in understanding women’s decision-making and the critical role of male partner support. Further research is necessary to create effective strategies that respect cultural sensitivities while increasing screening rates.
Health facility-level factors that affect the utilization of cervical cancer screening
Awareness of services availability and health facilities correlates with utilization of cervical cancer screening (p < 0.001). This highlights the crucial role of awareness in promoting health-seeking behaviors, as noted in research findings where the proximity of healthcare facilities to screened households was significantly correlated with screening uptake [44]. The healthcare providers pointed out lack of educational materials concerning cervical cancer and importance of screening in the medical facilities. The promotion of screening services by health facility staff is another significant factor influencing utilization. Only 8.1% of those who were unaware of promotional efforts engaged in screening, contrasting sharply with 45.8% in those receiving active encouragement (p < 0.001). This is consistent with findings which pointed to healthcare provider attitudes as critical in patients decision-making processes regarding screenings [45]. This also aligns with a study in Uganda which found that women who received relevant information from their health providers had higher odds of having ever been screened [21]. The adequacy of health worker training also surfaced as a determinant of screening utilization. The study found that 51.4% of respondents who perceived training as adequate utilized services, whereas only 9.1% of those unsure about staff training engaged in screening (p < 0.001). This is in line with findings which emphasized that inadequate knowledge among healthcare workers contributes to poor screening rates [46]. A study in Kenya posited that clinics which reported cervical cancer screening results were much more likely to have at least one practitioner with the necessary training [47]. The healthcare workers raised concerns about the knowledge gap among medical practitioners, underscoring the need for systematic training programs that standardize knowledge across healthcare facilities to enhance service delivery.
Convenience of operating hours emerged as a critical factor in the decision to undergo screening. Only 9.5% of respondents unaware of operating hour’s utilized services, while 52.9% took advantage of convenient hours (p < 0.001). This finding aligns with which found that geographical and logistical barriers significantly affect screening uptake [48].The healthcare workers revealed that service hours of many facilities do not accommodate patients’ needs. Thus, optimizing the operating hours of health facilities can potentially improve access and service utilization. The impact of past experiences with cervical cancer screening is significant, as evidenced by the overwhelming 97.9% utilization rate among women who had previously participated (p<0.001). This suggests that positive initial experiences can create a reinforcing cycle of participation in screening programs. Similarly, research findings emphasize that building positive relationships and satisfactory experiences with women undergoing screenings could contribute substantially to increased follow-up screenings [49]. This finding is also consistent with other studies done in Africa that demonstrated a correlation between desire to accept screening and previous screening history [41, 50]. This study highlights the need to enhance awareness, staff engagement, training for healthcare personnel, operational hours, and good screening experiences to improve cervical cancer screening uptake.
Conclusion
Cervical cancer screening utilization in Kaloleni Sub- County is alarmingly low, with only 23% of women aged 25-49 accessing these vital services. This reflects broader patterns in low-resource settings and underscores the need for targeted interventions to enhance awareness, accessibility, and acceptance. The study reveals that individual-level factors, including knowledge of cervical cancer and its symptoms, socioeconomic status, and health perceptions, significantly influence screening behaviors. Additionally, socio-cultural barriers, such as social norms and partner support, further complicate health-seeking habits. Health facility factors, including trained personnel and accommodating operating hours, are also crucial. To improve outcomes and reduce cervical cancer morbidity and mortality, stakeholders must address identified barriers through collaborative efforts among government, healthcare providers, and communities. Future research should explore the unique cultural and institutional challenges faced by women in various contexts to inform tailored interventions that resonate with their specific experiences.
Acknowledgement
I would like to thank all the study participants for their valuable contribution during data collection.
I also acknowledge the work of my supervisors, research assistants, and my mentor, Dr. Kishor Mandaliya.
Conflict of interest
There was no competing interest.
References
- Bray F, Laversanne M, Sung H, et al. Global cancer statistics 2022: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 CA: A Cancer Journal for Clinicians 74 (2024): 229-263.
- Trends at a Glance | Cancer trends progress report. National Cancer Institute (2021).
- Williams J, Rakovac I, Victoria J, et al. Cervical cancer testing among women aged 30–49 years in the WHO European Region. European Journal of Public Health 31 (2021): 884-889.
- Ba D M, Ssentongo P, Musa J, et al. Prevalence and determinants of cervical cancer screening in five sub- Saharan African countries: A population-based study. Cancer Epidemiology 72 (2021):
- KNBS. Kenya Demographic and Health Survey (KDHS) 2022—Kenya National Bureau of Statistics (2022).
- MOH. Ministry of Health, Kenya. Kenya National Cancer Screening Guidelines. 2018. Ministry of Health (2018).
- Petersen Z, Jaca A, Ginindza T G, et Barriers to uptake of cervical cancer screening services in low-and-middle- income countries: A systematic review. BMC Women’s Health 22 (2022): 486.
- WHO. Global Cancer Observatory. Cancer tomorrow: A tool that predicts the future cancer incidence and mortality burden worldwide from the current estimates in 2018 up until 2040. International Agency for Research on Cancer, World Health Organization (2018).
- Bruni L, Serrano B, Roura E, et al. Cervical cancer screening programmes and age-specific coverage estimates for 202 countries and territories worldwide: A review and synthetic The Lancet. Global Health 10 (2022): 1115-1127.
- WHO. Global strategy to accelerate the elimination of cervical cancer as a public health problem (2020).
- Ali-Risasi C, Mulumba P, Verdonck K, et Knowledge, attitude and practice about cancer of the uterine cervix among women living in Kinshasa, the Democratic Republic of Congo. BMC Women’s Health 14 (2014): 30.
- Fitzpatrick M, Pathipati M P, McCarty K, et al. Knowledge, attitudes, and practices of cervical Cancer screening among HIV-positive and HIV-negative women participating in human papillomavirus screening in rural Zimbabwe. BMC Women’s Health 20 (2020): 153.
- Gatumo M, Gacheri S, Sayed A-R, et al. Women’s knowledge and attitudes related to cervical cancer and cervical cancer screening in Isiolo and Tharaka Nithi counties, Kenya: A cross-sectional study. BMC Cancer 18 (2018): 745.
- Mekuria M, Edosa K, Endashaw M, et al. Prevalence of Cervical Cancer and Associated Factors Among Women Attended Cervical Cancer Screening Center at Gahandi Memorial Hospital, Ethiopia. Cancer Informatics 20 (2021): 11769351211068431.
- Morema E N, Atieli H E, Onyango R O, et Determinants of Cervical screening services uptake among 18–49 year old women seeking services at the Jaramogi Oginga Odinga Teaching and Referral Hospital, Kisumu, Kenya. BMC Health Services Research 14 (2014): 335.
- Ndejjo R, Mukama T, Kiguli J, et al. Knowledge, facilitators and barriers to cervical cancer screening among women in Uganda: A qualitative BMJ Open 7 (2017): e016282.
- Tekle T, Wolka E, Nega B, et al. Knowledge, Attitude and Practice Towards Cervical Cancer Screening Among Women and Associated Factors in Hospitals of Wolaita Zone, Southern Ethiopia. Cancer Management and Research 12 (2020): 993-1005.
- Woldetsadik A B, Amhare A F, Bitew S T, et al. Socio- demographic characteristics and associated factors influencing cervical cancer screening among women attending in St. Paul’s Teaching and Referral Hospital, Ethiopia. BMC Women’s Health 20 (2020): 70.
- Akokuwebe M E, Idemudia E S, Lekulo A M, et al. Determinants and levels of cervical Cancer screening uptake among women of reproductive age in South Africa: Evidence from South Africa Demographic and health survey data, 2016. BMC Public Health 21 (2021):
- Belay Y, Dheresa M, Sema A, et al. Cervical Cancer Screening Utilization and Associated Factors Among Women Aged 30 to 49 Years in Dire Dawa, Eastern Ethiopia. Cancer Control 27 (2020):
- Isabirye A, Mbonye M K, and Kwagala Predictors of cervical cancer screening uptake in two districts of Central Uganda. PLOS ONE 15 (2020): e0243281.
- Mafiana J J, Dhital S, Halabia M, et Barriers to uptake of cervical cancer screening among women in Nigeria: A systematic review. African Health Sciences 22 (2022): 295-309.
- Tawiah A, Konney T O, Dassah E T, et al. Determinants of cervical cancer screening uptake among women with access to free screening: A community-based study in peri-urban Ghana. International Journal of Gynaecology and Obstetrics: The Official Organ of the International Federation of Gynaecology and Obstetrics 159 (2022): 513-521.
- Binka C, Nyarko S H, Awusabo-Asare K, et Barriers to the Uptake of Cervical Cancer Screening and Treatment among Rural Women in Ghana. BioMed Research International, 2019 (2019): 6320938.
- Yang L, Boily M-C, Rönn M M, et al. Regional and country-level trends in cervical cancer screening coverage in sub-Saharan Africa: A systematic analysis of population-based surveys (2000-2020). PLoS Medicine 20 (2023): e1004143.
- Dickson K S, Boateng E N K, Acquah E, et Screening for cervical cancer among women in five countries in sub- saharan Africa: Analysis of the role played by distance to health facility and socio-demographic factors. BMC Health Services Research 23 (2023): 61.
- Ampofo A G, Adumatta A D, Owusu E, et A cross- sectional study of barriers to cervical cancer screening uptake in Ghana: An application of the health belief model. PloS One 15 (2020): e0231459.
- Rosethe R-J, Golda O Knowledge, Belief and Practice of Cervical Cancer Screening and Prevention among Women of Taraba, North-East Nigeria. Asian Pac J Cancer Prev 20 (2019): 3291-3298.
- Gebreegziabher Z A, Semagn B E, Kifelew Y, et al. Cervical cancer screening and its associated factors among women of reproductive age in Kenya: Further analysis of Kenyan demographic and health survey BMC Public Health 24 (2024): 741.
- Omotoso O, Matariek G, Omotoso E, et al. Practice of Breast Self-Examination and Knowledge of Breast and Cervical Cancer Screening: A bi-national Survey in Africa. AfricArXiv Preprints (2020).
- Donatus L, Nina F K, Sama D J, et al. Assessing the uptake of cervical cancer screening among women aged 25-65 years in Kumbo West Health District, Cameroon. Pan African Medical Journal 33 (2019): Article 1.
- Olubodun T, Balogun M R, Odeyemi A K, et Barriers and recommendations for a cervical cancer screening program among women in low-resource settings in Lagos Nigeria: A qualitative study. BMC Public Health 22 (2022): 1906.
- Tiruneh F N, Chuang K-Y, Ntenda P A M, et Individual- level and community-level determinants of cervical cancer screening among Kenyan women: A multilevel analysis of a Nationwide survey. BMC Women’s Health 17 (2017): 109.
- Olusola P, Banerjee H N, Philley J V, et al. Human Papilloma Virus-Associated Cervical Cancer and Health Disparities. Cells 8 (2019): Article 6.
- Vaccarella S, De Vries E, Sierra M S, et Social inequalities in cancer within countries. In S. Vaccarella, Lortet-Tieulent, R. Saracci, D. I. Conway, K. Straif, & P. Wild (Eds.), Reducing social inequalities in cancer: Evidence and priorities for research. International Agency for Research on Cancer (2019).
- Kaneko N. Factors associated with cervical cancer screening among young unmarried Japanese women: Results from an internet-based survey. BMC Women’s Health 18 (2018): 132.
- Mekonen E G, Gebrehana D A, and Tamir T T. Determinants of cervical cancer screening among women of childbearing age in four sub-Saharan African countries: Insights from large population surveys. BMC Cancer 24 (2024): 1304.
- Twinomujuni C, Nuwaha F, and Babirye J N. Understanding the Low Level of Cervical Cancer Screening in Masaka Uganda Using the ASE Model: A Community-Based Survey. PloS One 10 (2015):e0128498
- Black E, Hyslop F, and Richmond R. Barriers and facilitators to uptake of cervical cancer screening among women in Uganda: A systematic BMC Women’s Health 19 (2019): 108.
- Lau J, Shrestha P, Shaina Ng J, et al. Qualitative factors influencing breast and cervical cancer screening in women: A scoping review. Preventive Medicine Reports 27 (2022b): 101816.
- Adewumi K, Nishimura H, Oketch S Y, et al. Barriers and Facilitators to Cervical Cancer Screening in Western Kenya: A Qualitative Journal of Cancer Education : The Official Journal of the American Association for Cancer Education 37 (2021): 1122.
- Mboineki J F, Wang P, Dhakal K, et al. Predictors of uptake of cervical cancer screening among women in Urban Tanzania: Community-based cross-sectional study. International Journal of Public Health 65 (2020): 1593-1602.
- Mochache V, Wanje G, Lucy Nyagah. Religious, socio- cultural norms and gender stereotypes influence uptake and utilization of maternal health services among the Digo community in Kwale, Kenya: a qualitative study. Reprod Health 17 (2020): 71.
- Barrett B W, Paz-Soldan V A, Mendoza-Cervantes D, et Understanding Geospatial Factors Associated With Cervical Cancer Screening Uptake in Amazonian Peruvian Women. JCO Global Oncology 6 (2020): 1237- 1247.
- Nigussie G, Mamaru A M, Michael M M. Assessment of Suitable Land for Surface Irrigation in Ungauged Catchments: Blue Nile Basin, Water 11 (2019): 1465.
- Odera J O, Odera E, Githang’a J, et Esophageal cancer in Kenya. American Journal of Digestive Disease 4 (2017): 23-33.
- Eastment M C, Wanje G, Richardson B A, et A cross- sectional study of the prevalence, barriers, and facilitators of cervical cancer screening in family planning clinics in Mombasa County, Kenya. BMC Health Services Research 22 (2022): 1577.
- Waiswa P, Namazzi G, Okuga M. Working with community health workers to improve maternal and newborn health outcomes: implementation and scale- up lessons from eastern Uganda. Glob Health Action 10 (2017): 1345495.
- Njuguna E, Ilovi S, Muiruri P, et al. Factors influencing cervical cancer screening in a Kenyan Health Facility: A mixed qualitative and quantitative study. International Journal of Reproduction, Contraception, Obstetrics and Gynecology 6 (2017): 1180-1185.
- Mabelele M M, Materu J, Ng’ida F D, et al. Knowledge towards cervical cancer prevention and screening practices among women who attended reproductive and child health clinic at Magu district hospital, Lake Zone Tanzania: A cross-sectional study. BMC Cancer 18 (2018): 565.
