Utility of P57 Immunohistochemistry in Differentiating Complete Mole from Partial Mole
Article Information
Dr. Dilruba Ferdous1*, Prof. Dr. Sabera Khatun2, Dr. Lutfa Begum Lipi3, Dr. Sayada Fatema Khatun4, Dr. Shahana Rahman5, Dr. Rogina Amin6, Dr. Khadija Rahman Shilpi7, Dr. Mirza Md. Asaduzzaman8, Dr. Nilufer Yasmin9
1Senior Consultant, Department of Gynecological Oncology, Maternal and Child Health Training Institute, Lalkuthi Mazar Road, Mirpur, Dhaka, Bangladesh.
2Professor & Founder Chairman, Department of Gynaecology Oncology, Bangladesh Medical University, Dhaka, Bangladesh.
3Assistant Professor, Department of Gynecological Oncology, Dhaka Medical College Hospital, Dhaka, Bangladesh.
4Assistant Professor, Department of Gynecological Oncology, Bangladesh Medical University, Dhaka, Bangladesh.
5Medical Officer (Gynecological Oncology), Bandarban Sadar Hospital, Bandarban, Bangladesh.
6Junior Consultant, Department of Obstetrics and Gynaecology, Kurmitola General Hospital, Dhaka, Bangladesh.
7Junior Consultant, Department of Obstetrics and Gynaecology, Shaheed Suhrawardy Medical College and Hospital (SSMCH), Dhaka, Bangladesh.
8Junior Consultant, Department of Gynecological Oncology, Dhaka Medical College Hospital, Dhaka (DMCH), Dhaka, Bangladesh.
9Junior Consultant, National Institute of Cancer Research & Hospital (NICRH), Dhaka, Bangladesh.
*Corresponding author: Dr. Dilruba Ferdous, Senior Consultant, Department of Gynecological Oncology, Maternal and Child Health Training Institute, Lalkuthi Mazar Road, Mirpur, Dhaka, Bangladesh.
E-mail ID: ferdousdilruba@gmail.com
Received: 24 February 2025; Accepted: 10 March 2025; Published: 16 July 2025
Citation: Dr. Dilruba Ferdous, Prof. Dr. Sabera Khatun, Dr. Lutfa Begum Lipi, Dr. Sayada Fatema Khatun, Dr. Shahana Rahman, Dr. Rogina Amin, Dr. Khadija Rahman Shilpi, Dr. Mirza Md. Asaduzzaman, Dr. Nilufer Yasmin. Utility of P57 Immunohistochemistry in Differentiating Complete Mole from Partial Mole. Obstetrics and Gynecology Research. 8 (2025): 103-109.
View / Download Pdf Share at FacebookAbstract
Background:
Molar pregnancy is basically a gestational trophoblastic neoplasia that is a complication of pregnancy. Depending on the balance of chromosome in the egg, molar pregnancy is divided into two main subtypes; complete and partial.
Objectives:
To find out the utility of p57 IHC in differentiating complete more from partial mole.
Methods:
This was a cross sectional study. The study was conducted in the Department of Gynecological Oncology, Dhaka Medical College Hospital, Dhaka, Bamgladesh. At July, 2019 to June, 2020. All patients who were diagnosed as molar pregnancy were selected by purposive sampling. Thereafter, they were scrutinized according to eligibility criteria and 50 patients were finalized. A pre-tested, observation based, peerreviewed data collection sheet was prepared before study. An informed written consent was taken after explanation regarding the study procedure. Molar tissue was obtained by suction and evacuation of uterus from all the cases. Then the sample was sent for HPR & IHC. Immunohistochemistry evaluation of all cases was performed from molar tissue & also from endometrium. Data regarding clinical, biochemical and surgical profile were recorded. Data were compiled, edited, analyzed. Data analysis were expressed in frequency, mean, standard deviation, percentages and ratio.
Results:
Among 50 patients, the highest 27(54%) belonged to 26-35 years, which was subsequently followed by 21(42%) patients belonged to 19-25 year’s age group. Rest 2(4%) were from 36-40 year’s group. The mean age of the patients was 27.36±2.79 (age range: 19-40) years. The highest 35(70%) were in 2nd gravida. Besides 8(16%) and 6(12%) were in their 1st and 33rd gravida. Rest 11(2%) was on her 4th gravida. Out of 50 patients, the highest 23(46%) patients presented at 12-16 week of gestational age, 13(26%) and 10(20%) patients presented at <12 weeks and 17-20 weeks of gestational age respectively. Only 4(8%) patients present of 21-24 weeks of gestational age. Out of 50 patients, 39(78%) were complete mole and rest 11(22%) were diagnosis as partial mole on the basis of HPR diagnosis. Out of 39 CM diagnosis by HPR, 79.84% were correct diagnosis determined by p57 immunohistochemistry. On the contrary, among 11 confirmed PM diagnosis by HPR only 27.27% were reconfirmed as correct diagnosis by p57 immuhohistochemistry. Extra villous trophoblast in p57 IHC expressed highest percentages in both CM and PM (84% vs 100%). Likewise, cytotrophoblast shows the highest in PM (100%) though it had the lowest expression in CM (6%). Vilous stromal cells had 82% expression in PM whereas 10% expression in CM, Decidua expression was 60% and 78% in CM and PM respectively.
Conclusion:
The effectiveness of p57 IHC test may reliably identify CM and may be used in association with the histological findings to distinguish CM from its mimics.
Keywords
Molar pregnancy; Chromosome; p57 IHC; Gestational age HPR diagnosis; PM diagnosis.
Article Details
I. INTRODUCTION
Gestational trophoblastic neoplasia is a pregnancy related disorder that has been applied to describe the different pathological appearance of trophoblastic tissue. It includes hydatidiform mole (HM), invasive mole, placental site trophoblastic tumors and choriocarcinoma. Among them HM is the most common. It is, actually, a benign tumour that develops in the uterus. It is also known as molar pregnancy. It begins when an egg is fertilized but normal viable pregnancy not occurs, rather than the placenta develops into an abnormal mass of cyst. A normal pregnancy contains 46 chromosomes half of it comes from mother and rest half from the father. Depending on the balance of chromosome in the egg, molar pregnancy is divided into two main subtype :- (1) complete mole (2) partial mole [1]. A partial mole contains 69 chromosome instead of normal 46, one third of the chromosome (23) comes from the maternal side and others (46) from the paternal side [2]. It consists of an abnormal embryo and some normal placental tissue. As the embryo is malformed it cannot survive. The egg of complete mole contains only 23 paternal chromosome, here amniotic sac or embryo is absent. As soon as the egg is fertilized by the sperm trophoblastic cell behave abnormally and this results in a mass of abnormal cells that can grow fluid filled sac (cysts) with the appearance of white grapes [3]. The exact etiology is yet unknown but it seems to be related with ovular defect, abnormality within the uterus or nutritional deficiencies. Several epidemiological risk factors are identified for the development of molar pregnancy; the most important one is geographical factor. The highest incidence is seen in Philippines being 1 in 80 pregnancy and lowest in European countries 1 in 752 cases. Incidence in USA being about 1 in 2000 and in our neighbor country India it is about 1 in 400 pregnancies (D.C. Dutta Text Book; 215). It develops from the placental tissue during early pregnancy in which the embryo fails to develop normally. Microscopically mole may be identified by three classic findings [4] 1. Edema of villous 2. Avascular villi. 3. Nest of proliferating syncytotrophoblast and cytotrophoblast element surrounding villi. Hydatidiform mole (HM) was first described by Hippocrates around 400 B.C. as "dropsy of the uterus." Since that time, HM (also referred to as molar pregnancy or mole) has been of clinical and research interest. Molar pregnancy is part of a group of diseases classified as gestational trophoblastic disease (GTD), which originate in the placenta and have the potential to locally invade the uterus and metastasize. The pathogenesis of GTD is unique because the maternal tumor arises from gestational rather than maternal tissue (Berkowitz and Goldstein, 2013). HM is made up of two distinct entities, complete HM and partial HM. These differ on the basis of chromosomal pattern, gross and microscopic histopathology, clinical presentation, and outcome [5]. Molar pregnancies, although benign but considered to be premalignant because they have the potential to develop into a malignancy. Basically, morphologic examination of products of conception (POC) forms the main diagnostic tool in the differential diagnosis of complete mole (CM) and partial mole (PM). However, the criteria are subjective and show considerable inter-observer variability [6]. With early diagnosis and evacuation of molar pregnancies, the differentiation from early non-molar placentation, especially hydropic abortus (HA), is difficult. The p57KIP2 gene encoding for p57, a cell cycle inhibitor, is strongly paternally imprinted and expressed from the maternal allele. Molar pregnancy occur most frequently in South East Asia like Malaysia, Singapore, Hong Kong, Indonesia, Philippines and China [7]. Incidence in Philippines is 1 in 80, in India is1 in 400 [8]. The exact etiology of the disease is yet unknown, but it appears to be related to the ovular defect as it sometimes affects one ovum of a twin pregnancy. There is an increased risk in teenagers and woman over 35 years. The rate rises to 10 fold after the age of 40 years [4]. Patients with higher parity are at higher risk in under developed countries [9]. HM occurs once in every 1000 pregnancies in the US, with much higher rates in Asia (e.g. up to one in 100 pregnancies in Indonesia) [10]. The symptom which most often calls attention to the abnormality is recurrent uterine bleeding. Nausea, vomiting have been reported in 14-32 % of patients of hydatidiform mole and may be confused with nausea and vomiting of early pregnancy. In over 80% of cases the first evidence of hydatidiform mole is the passage of vesicular tissue, bleeding and brown discharge. The uterus is too large for the period of amenhorrea. is present in only 50% of cases. Sometimes the uterus is smaller than normal, especially if the mole dies. Enlargement of both ovaries seen in 25-30% of molar pregnancy. The genetic basis of hydatidiform moles was established in the 1970’s [11]. All CHM have a diandric paternal only genome; there is no maternal contribution. The majority of CHM are therefore homozygous and arise from an anuclear empty ovum that has been fertilised by a haploid 23, X sperm (monospermy), which then replicates its own chromosomes resulting in a 46, XX karyotype (uniparental paternal isodisomy). A minority involve the fertilisation of an anuclear empty ovum with two sperm (dispermy) simultaneously, which can result in a 46, XX or 46, XY karyotype (uniparental paternal heterodisomy). A very rare form of CHM involves tetraploidy [12]. It has also been reported that diploidization may follow from a triploid conceptus; a CHM would result if the maternal haploid contribution was lost. The abnormality in fetal-placental development in CHM is essentially due to abnormal genomic imprinting effects. Loss of the maternal epigenetic imprint and gain of paternally imprinted gene expression together result in global genome demethylation and abnormal gene expression that result in abnormal placental trophoblast development [13]. Most cases of CHM are sporadic, however a very small minority of moles are recurrent and often familial, usually being diploid and biparental (having both sets of parental chromosomes). Rare recurrent hydatidiform moles (RHM) involve at least two molar pregnancies. Maternal homozygous and compound heterozygous recessive gene mutations have been reported in some families. Two such genes are NLRP7 and KHDC3L [14]. NLRP7 (NLR family, pyrin domain containing 7) located at 19q13.4 is a member of the NLR family of proteins with a role in inflammation and apoptosis. It was the first identified recessive gene involved in RHMs and mutations have been reported in 48-80% of patients with more than 50 mutations identified to date [15]. KHDC3L (KH domain containing 3-like) located at 6q13 is a member of the KHDC1 protein family. It was the second recessive gene identified responsible for RHM, however only five mutations have been identified to date [16]. The exact causal mechanisms involving these two genes in RHM families is not fully understood, however deregulation of imprinted genes contributes to pathogenesis, resulting in aberrant cell proliferation and differentiation [14]. Immunohistochemical marker P57KIP2 is used recently in the diagnosis of HM, p57KIP2 is the protein product of the paternally imprinted but maternally expressed gene CDKN1C located on chromosome 11 p15.5. Because CHM lack a maternal genomic component, they are not expected to express imprinted genes that are normally expressed by the maternal allele, and immunohistochemical analysis for p57 has been shown to be a valuable tool in the diagnosis of a CHM. Considering the above mentioned facts and figures, the present study is aimed to find out the utility of p57 immunohostochemistry in differentiating complete mole from partial mole.
Objectives
General objective:
To find out the utility of p57 IHC in differentiating complete more from partial mole.
Specific objectives:
• To find out complete mole by using p57 IHC.
• To find out partial mole by using p57 IHC.
Materials and Methods
This was a cross-sectional study. The patients were selected purposively. A total of 50 patients were included in this study. The study was conducted in the Department of Gynecological Oncology, Dhaka Medical College & Hospital (DMCH), Dhaka, Bangladesh. At July 2019 to June 2020.
Inclusion Criteria
• Diagnosed cases molar pregnancy by ultrasonography and S. BhcG
Exclusion Criteria
• PGTN
• Choriocarcinoma
• PSTT
• Invasive mole.
• Incomplete abortion
• Missed abortion
• H/O previous chemotherapy.
Procedures of Collecting Data
Data was collected from the sample. Already Diagnosed cases of molar pregnancy are included in my study only after obtaining the informed consent of the patient. Detailed history and thorough clinical examination, BHCG and USG was performed following a pre tested questionnaire but only after obtaining the informed consent of the patient.
Procedures of Data Analysis and Interpretation
Statistical analyses were carried out by using the Statistical Package for Social Sciences version 23.0 for Windows (SPSS Inc., Chicago, Illinois, USA). The mean values were calculated for continuous variables. The qualitative observations were indicated by frequencies and percentages. Chi-square test was used to compare categorical data like clinical signs and symptoms. A “p” value <0.05 was considered as significant.
Ethical clearance
Ethical clearance of the study had been taken from the Ethical Review Committee of Dhaka Medical College Hospital.
Table 1: Distribution of patients according to age (N=50).
|
Age group (in years) |
Frequency (%) |
|
19-25 Yrs. |
21 (42%) |
|
26-35 Yrs. |
27 (54%) |
|
36-40 Yrs. |
2 (4%) |
|
Mean age ±SD (in years) |
27.36±2.76 |
|
Age range (in years) |
19-40 |
Table 1 shows that among 50 patients, the highest 27(54%) belonged to 26-35 years, which was subsequently followed by 21(42%) patients belonged to 19-25 years’ age group. Rest 2(4%) were from 36-40 years’ group. The mean age of the patients was 27.36±2.79 (age range: 19-40) years.
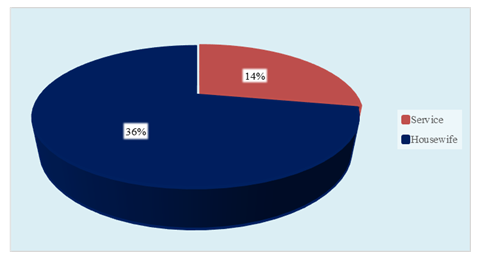
Table 2: Distribution of patients according to socioeconomic status (N=50).
|
Socioeconomic status |
Frequency (%) |
|
Low ( £6821) |
18 (36%) |
|
Lower middle (6828-26852) |
27 (54%) |
|
Higher middle (26852-83018) |
4 (8%) |
|
High (³83024) |
1 (2%) |
Table 2 shows that among 50 patients, 27(54%), 18(36%) and 4(8%) were from low (6821), lower middle (6828-26852) and higher middle (26859-83018) socioeconomic status respectively. Rest 1(2%) came from high (³83024) socioeconomic status.
Table 3: Distribution of patients according to Gravida (N=50)
|
Gravida |
Frequency (%) |
|
1st |
8 (16%) |
|
2nd |
35 (70%) |
|
3rd |
6 (12%) |
|
4th |
1 (2%) |
Table 3 shows that among 50 patients, the highest 35(70%) were in 2nd gravida. Besides 8(16%) and 6(12%) were in their 1st and 33rd gravida. Rest 11(2%) was on her 4th gravida.
Table 4: Distribution of patients according to gestational age (N=50).
|
Gestational age at presentation (in week) |
Frequency (%) |
|
<12 |
13 (26%) |
|
Dec-16 |
23 (46%) |
|
17-20 |
10 (20%) |
|
21-24 |
4 (8%) |
Table 4 shows that out of 50 patients, the highest 23(46%) patients presented at 12-16 week of gestational age, 13(26%) and 10(20%) patients presented at <12 weeks and 17-20 weeks of gestational age respectively. Only 4(8%) patients presents of 21-24 weeks of gestational age.
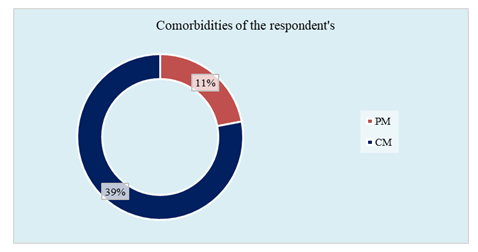
Table 5: Summary of original diagnosis and final diagnosis with p57 immunohistochemistry in complete mole (CM) and partial mole (PM) (N=50).
|
Final Diagnosis |
||||
|
CM |
PM |
|||
|
n=39 |
IHC |
n=11 |
IHC |
|
|
CM |
31 |
30N, 1P |
3 |
3P |
|
PM |
8 |
8N |
8 |
8P |
|
Accuracy |
31/39 |
38/39 |
03-Nov |
11-Nov |
|
-79.84% |
(97.43%N) |
(27.27% |
(100%P) |
|
|
P: Positive N: Negative IHC: Immunohistochemistry |
||||
|
CM: Complete mole PM: Partial Mole |
||||
Table 5 shows that out of 39 CM diagnosis by HPR, 79.84% were correct diagnosis determined by p57 immunohistochemistry. On the contrary, among 11 confirmed PM diagnosis by HPR only 27.27% were reconfirmed as correct diagnosis by p57 immuhohistochemistry.
Table 6: Distribution of histopathological features in CM and PM (n=50).
|
Morphological features |
CM |
PM |
|
Proportion of villi showing edema (range) (%) |
70-95 |
52-70 |
|
Cistern formation (%) |
95 |
62 |
|
Scalloping (%) |
82 |
100 |
|
Villous trophoblastic hyperplasia intensity in majority (%) and location(%) |
Marked: 75 |
Mild: 100 |
|
Extravillous/implementation site hyperplasia – intensity in majority (%) and atypia (%) |
Marked: 60 |
Mild to moderate: 80 |
Table 6 shows the overall morphological features of complete mole and partial mole.
Table 7: IHC with p57 in CM and PM (n=50).
|
p57 IHC |
CM |
PM |
|
Cytotrophoblast (%) |
6 |
100 |
|
Vilous stromal cells (%) |
10 |
82 |
|
Extravillous trophoblast (%) |
86 |
100 |
|
Decidua (%) |
60 |
78 |
Table 7 shows that extravillous trophoblast in p57 IHC expressed highest percentages in both CM and PM (84% vs 100%). Likewise, cytotrophoblast shows the highest in PM (100%) though it had the lowest expression in CM (6%). Vilous stromal cells had 82% expression in PM whereas 10% expression in CM, Decidua expression was 60% and 78% in CM and PM respectively.
Discussion
In this study the incidence of molar pregnancy was 4.3 per 1,000 deliveries that is 1 in 232 deliveries. A study by Aghababaii et al. (2016) [17] in Iran showed the incidence was 3.70 per 1,000 deliveries that is 1 in 27.1 deliveries. Dinesh et al. (2016) [18] in his study showed the incidence of molar pregnancy was 4.56 per 1000 deliveries that is 1 in 219 deliveries. Study by Akhter (1981) [19] in 1978-1980 at SSMC and Mitford Hospital showed that incidence of molar pregnancy was 1 in 144 deliveries that are 6.9 per thousand. The obtained incidence rate in our study was consistent with other studies except the study of Aghababaii S et al. (2016) [17]. In the study maximum number of patients (54%) were between (26 - 35) years age group that was also supported by a previous Bangladeshi study where they showed that 64% patients were from 20-29 yrs age group [20]. Another study showed that 63.75% patients were in 21-30 yrs age group [4]. Besides, a study of 287 patients was done in Pusan, Korea where the authors showed that highest number patients (70%) were below 30 yrs of age [5]. The findings of these studies are contrast to the previous observations. But interestingly, another previous Bangladeshi study showed the similar results like our findings [21]. In this study, 84% patients were multigravida and 16% patients were primigravida that are supported by a previous study where they showed that in 60% cases hydatidiform mole was associated with multiparity [22]. Another study showed that 70% patient were multigravida [18]. Our study results are consistent with the previous study results. In the study, 36% patients belonged to lower class whereas total 62% were from middle class and rest 2% belonged to affluent society. These results were comparable to a previous study showed that 86% patients were from middle class [18]. Out of 50 patients the highest 46% patients present between 12-16 weeks of pregnancy which is in line to a previous study in FMCH where they showed exact 46% patients present between 12-16 weeks of pregnancy [21]. In another Bangladeshi study 40% patients present with 12-16 week’s gestation that was also agreed to our study findings [23]. On the other hand, 26% patients presented in <12 week’s gestation which were agreed by the findings of another study where 22.97% patients presented at this stage [24]. In this study, we have diagnosed 78% of our cases as complete mole (CM) and rest 22% of our cases as partial mole (PM). These diagnoses were initially diagnosed by histopathology report (HPR) which was subsequently reconfirmed by Immunohistochemistry (IHC). After doing IHC it was revealed that in some cases HPR failed to provide the original diagnosis. IHC with p57 was negative in 96 percent CM and positive in 100 percent PM. The morphologic findings were in conjunction with reported literature [25]. In our study, correct diagnosis on morphology alone was 79.84 percent for CM, 27.27 percent for PM. Although the histopathological criteria for diagnosis of partial and complete molar pregnancy are clearly defined in the literature, unfortunately they are not always present in histological slides, especially in case of early molar pregnancy. For example, in the study of Paul et al. [26], 21 cases of molar pregnancy were reevaluated using flow cytometry and immunohistochemical analysis of p57 marker. It was found that only six of the 21 cases were really molar pregnancies [26]. According to Golfier et al. (2011) [27], there is a significant difference in the accuracy of diagnosis of molar pregnancy if the analysis was performed by an experienced pathologist. Apart from the accumulated experience that allows more accurate determination of the histological criteria, this study found that the experienced pathologists significantly more often (41.0%) use additional immunohistochemical markers such as p57 to confirm the histological diagnosis. In fact, these investigators believe that adequate and relevant clinical differentiation between partial, complete molar pregnancy and hydropic abortion can be achieved if the slides are evaluated by an experienced pathologist in this field, but only if additional immunohistochemical or molecular techniques are used [27]. All cases in this study were evaluated by an experienced pathologist, with the use of additional immunohistochemical analyses. In this way, it was possible to confirm the diagnosis of complete mole using immunohistochemistry even in the case of biparental diploidy. Additional immunohistochemical analyses are often used in the literature to distinguish between partial and complete molar pregnancy. This method is simple and quick and can be performed without the need for expensive equipment [28]. The most useful antibody to confirm a diagnosis of complete mole is p57 [29]. The p57Kip2 protein is a cyclin-dependent kinase inhibitor. It is the protein product of the CDKN1C gene, located on chromosome 11p15.5 and is paternally imprinted and maternally expressed. Thus, since the complete molar pregnancy is missing genetic material from the mother, it is not expected to show CDKN1C gene expression [29]. On the other hand, the cases of hydropic abortions (biparental diploidy) and partial molar pregnancy (diandric triploidy) are expected to show p57 positivity in the cytotrophoblasts and villous stromal cells. However, cases of biparental diploid complete moles also have abnormal, androgenetic pattern of p57Kip2 expression rather than that seen in other types of biparental conceptuses. This is probably due to abnormal imprinting, being a common mechanism underlying the development of biparental diploid complete mole [30]. The immunohistochemical analysis for the p57 marker confirmed all seven cases of androgenetic diploidy as complete molar pregnancies, whereas in the one case of biparental diploidy, the absence of the p57 marker in the cytotrophoblasts and villous stroma was the only back up for the histopathological diagnosis of early complete mole. Other investigators have also been able to differentiate cases of hydropic abortion and partial mole from complete mole cases, based on immunohistochemistry for p57. They have not found p57 positivity in the cytotrophoblasts or villous stroma in any of the complete mole cases tested, unlike partial mole or hydropic abortion [29].
Limitations of The Study
It was a cross-sectional single blinded single centered study with small sample size in short duration. So, this study did not proclaim the scenario of whole of the country.
Recommendations
The multicenter study in whole of the country with multi-disciplinary approach and long duration could be reveal the real picture of the study in this regards.
Conclusion
In conclusion, it could be claimed that the effectiveness of p57 IHC test may reliably identify CM and may be used in association with the histological findings to distinguish CM from its mimics.
References
- Stone M, Bagshawe KD. An analysis of the influences of maternal age, gestational age, contraceptive method, and the mode of primary treatment of patients with hydatidiform moles on the incidence of subsequent chemotherapy. Br J ObstetGynaecol.; 86 (2009): 782-792.
- Berkowitz RS, Goldstein DP. Chorionic tumors. N Engl J Med 335 (1996): 1740-1748.
- Soper JT, Mutch DG, Schink JC. American College of Obstetricians and Gynecologists. Diagnosis and treatment of gestational trophoblastic disease: ACOG Practice Bulletin No. 53. GynecolOncol. 93 (2004): 575-585.
- Decherney, Nathan. Current Obstetrics & Gynecologic Diagnosis & Treatment ,10th edition, McGraw-Hill, (2007): 885-894.
- Melamed, A., Gockley, A.A., Joseph, N.T., et al. Effect of race/ethnicity on risk of complete and partial molar pregnancy after adjustment for age. Gynecologic oncology, 143 (2016): pp.73-76.
- Fukunaga M, Katabuchi H, Nagasaka T, et al. Interobserver and intraobserver variability in the diagnosis of hydatidiform mole. Am J Surg Pathol 29 (2005): 942-947.
- Dutta D.C. Text book of Obstetrics,6th edition, Typesetter andPrinter,28-36 (2007): 385-424
- Kumer, Malhotra, Jeffcoate’s principles of Gynecology, 7th edition. Jaypee Brothers (2008): p.161-169
- Parazzaini F et al., Risk factors for gestational trophoblastic disease, a separate analysis of complete and partial moles. J Obstel Gynaecol, 78 (1991): 1039-1045
- Abbas, R.K. and Al-Khafaji, K.R. Expression of P57 Immunohistochemical marker in complete and partial hydatidiform mole by using tissue microarray technique IOSR Journal of Applied Chemistry (IOSR-JAC) 7 (2014): pp.P 90-95
- Kajii T, Ohama K.. Androgenetic origin of hydatidiform mole. Nature; 268 (1997): 633-634.
- Hui P. Molecular diagnosis of gestational trophoblastic disease. Expert Rev Mol Diagn; 10 (2010): 1023-34.
- Bestor TH, Bourc'his D. Genetics and epigenetics of hydatidiform moles. Nat Genet 38 (2006): 274-276.
- Nguyen NM, Slim R. Genetics and Epigenetics of Recurrent Hydatidiform Moles: Basic Science and Genetic Counselling. Curr Obstet Gynecol Rep 3 (2014): 55-64.
- Estrada H, Buentello B, Zenteno JC, et al. The p. L750V mutation in the NLRP7 gene is frequent in Mexican patients with recurrent molar pregnancies and is not associated with recurrent pregnancy loss. Prenat Diagn; 33 (2013): 205-208.
- Reddy R, Akoury E, Phuong Nguyen NM, et al. Report of four new patients with protein-truncating mutations in C6orf221/KHDC3L and colocalization with NLRP7. Eur J Hum Genet 21 (2013): 957-964.
- Aghababaii S, Shobeiri F, Hosseinipanah SM. Hydatidiformmole: A statistical survey in west of Iran. Postgrad Med Inst. 30 (2016).
- Dinesh K, Singh YA, Singh LS et al. A study of molar pregnancy at tertiary centre of India. (2016): 49-52.
- Akter. Hydatidiform mole. Dissertation, FCPS examination, Dhaka (1981).
- D.C. Text book of Obstetrics, 8th edition, Jaypee Brothers, (2015): p-222.
- Khan JH, Ferdous J, Alam S. Clinical Presentation and Management of Hydatidiform Mole in a Peripheral Tertiary Hospital. Bangladesh J Obstet Gynaecol, Vol. 25 (2010) : 59-64.
- Mungan T, Kuscu E, Dabakoglu T, et al. Hydatidiform mole; clinical analysis of 310 patients. Int J ObstelGynaecol.; 25 (1996): 233-238.
- Nahar. Molar pregnancy Analysis of 50 cases in FMCH & BSMMU, Dissertion FCPS examination, Dhaka (2005).
- Goldstein DP, Berkowitz RS. Current management of complete and partial molar pregnancy. J Reprod Med. 39 (1994): 139-146.
- Dayal S, Chaturvedi V, Singh A, et al. Audit of partial and complete hydatidiform moles in tertiary care hospital in rural inhabitants of India. Indian J Health Sci 7 (2014): 104-107.
- Paul M, Goodman S, Felix J, et al. Early molar pregnancy: Experience in a large abortion service. Contraception. 81 (2010): 150-156.
- Golfier F, Clerc J, Hajri T, et al. Contribution of referent pathologists to the quality of trophoblastic diseases diagnosis. Hum Reprod 26 (2011): 2651-2657.
- Erfanian M, Sharifi N, Omidi AA. P63 and Ki-67 expression in trophoblastic disease and spontaneous abortion. J Res Med Sci. 14 (2009): 375-384.
- Sarmadi S, Izadi-Mood N, Abbasi A, et al. p57KIP2 immunohistochemical expression: A useful diagnostic tool in discrimination between complete hydatidiform mole and its mimics. Arch Gynecol Obstet 283 (2011): 743-748.
- Fisher RA, Hodges MD, Rees HC, et al., The maternally transcribed gene p57(KIP2) (CDNK1C) is abnormally expressed in both androgenetic and biparental complete hydatidiform moles. Hum Mol Genet 11 (2002): 3267-3272.