Ultrasound eFAST vs. CT CAP in Blunt Trauma Patients: An Evidence-Based Comparative Analysis in Pakistan
Article Information
Sumbla Salman1, Bushra Jawaid2, Zahida Ismail3, Bushra Saeed Khan3, Nadhra Salman4, Rabia Hameed3, Iqra Anees Rajput3, Hafiza Shabina5, Zubair Nisar5, Noman Ahmed Khan*,3
1Karachi Metropolitan University, Karachi
2Fazaia Ruth Pfau Medical College, Karachi
3Dow University of Health Sciences, Karachi
4Baqai Medical University, Karachi
5Shaheed Mohtarma Benazir Bhutto Institute of Trauma, Karachi
*Corresponding author: Noman Ahmed Khan, Dow University of Health Sciences, Karachi, Pakistan.
Received: 22 June 2025; Accepted: 26 June 2025; Published: 10 July 2025
Citation: Sumbla Salman, Bushra Jawaid, Zahida Ismail, Bushra Saeed Khan, Nadhra Salman, Rabia Hameed, Iqra Anees Rajput, Hafiza Shabina, Zubair Nisar, Noman Ahmed Khan. Ultrasound eFAST vs. CT CAP in Blunt Trauma Patients: An Evidence- Based Comparative Analysis in Pakistan. Fortune Journal of Health Sciences. 8 (2025): 658-663.
View / Download Pdf Share at FacebookAbstract
Background: Blunt trauma accounts for 70-80% of traumatic injuries worldwide, necessitating rapid and accurate diagnostic imaging. The Extended Focused Assessment with Sonography for Trauma (eFAST) and Computed Tomography of the Chest, Abdomen, and Pelvis (CT CAP) are primary imaging modalities. This article compares the diagnostic accuracy, clinical utility, and impact on patient outcomes of these two methods in the context of blunt trauma.
Objective: The objective of this study was to compare the effectiveness of eFAST vs CT scan in Patients with blunt trauma.
Study Design: Prospective Cohort Study.
Duration: The study was conducted at the Shaheed Mohtarma Benazir Bhutto Trauma Centre (SMBBIT) over one year, from June 2024 to May 2025.
Methods: Patients who presented in the emergency department with blunt trauma and were stable enough to undergo both EFAST and CT scan were included in the study.
Results: CT CAP remains superior, with >95% sensitivity for solid organ injuries, retroperitoneal bleeding, and occult fractures. While eFAST is faster (3-5 minutes) and radiation-free, CT CAP provides a comprehensive evaluation but requires hemodynamic stability.
Conclusion: eFAST is invaluable for initial triage in unstable patients, while CT CAP is the gold standard for definitive diagnosis in stable blunt trauma. An integrated approach optimizes outcomes, particularly in high-risk patients
Keywords
Ultrasound efast vs CT Cap, Trauma emergency, Blunt Trauma
Article Details
Introduction
Blunt trauma remains a leading cause of morbidity and mortality worldwide, accounting for nearly 70-80% of all traumatic injuries (World Health Organization, 2023). The diagnostic challenges posed by blunt trauma stem from its propensity to cause occult injuries that may not be immediately apparent on physical examination, particularly in patients with altered mental status or distracting injuries. This clinical reality necessitates reliable, rapid diagnostic imaging modalities that can accurately identify life-threatening injuries while minimizing delays in definitive treatment. The evolution of trauma imaging has been significantly influenced by the Advanced Trauma Life Support (ATLS) guidelines, which emphasize a structured approach to the primary survey with particular attention to immediately life-threatening conditions (American College of Surgeons, 2021). Within this framework, two imaging modalities have emerged as cornerstones of blunt trauma evaluation: the Extended Focused Assessment with Sonography for Trauma (eFAST) and Computed Tomography of the Chest, Abdomen, and Pelvis (CT CAP). Each modality offers distinct advantages and limitations that profoundly influence clinical decision-making in trauma centers worldwide.
The eFAST examination represents an extension of the traditional FAST (Focused Assessment with Sonography for Trauma) protocol, incorporating evaluation for pneumothorax in addition to its standard assessment for pericardial effusion and intraperitoneal free fluid (Volpicelli et al., 2020). This bedside ultrasound technique has gained widespread adoption due to several key characteristics: it is non-invasive, repeatable, does not expose patients to ionizing radiation, and can be performed concurrently with resuscitation efforts. Studies demonstrate that a properly executed eFAST exam can be completed in under five minutes by trained providers (Guttikonda et al., 2022), making it particularly valuable in the initial evaluation of hemodynamically unstable patients where time-sensitive decisions regarding emergent interventions such as pericardiocentesis or exploratory laparotomy may be required (Kirkpatrick et al., 2021). In contrast, CT CAP has become the gold standard for the comprehensive evaluation of blunt trauma patients, offering unparalleled spatial resolution and the ability to simultaneously evaluate multiple body regions with a single examination (LeBedis et al., 2023). Modern multi-detector CT scanners can acquire complete chest, abdominal, and pelvic images in less than 30 seconds, with advanced post-processing capabilities that allow for detailed assessment of solid organ injuries, active hemorrhage, bony fractures, and subtle vascular injuries (Anderson et al., 2020). The modality's high sensitivity (>95% for most significant injuries) and specificity (approaching 100% for many injury patterns) have revolutionized trauma care by enabling more precise injury grading and tailored treatment strategies (Huber-Wagner et al., 2019). However, the superior diagnostic capabilities of CT CAP come with several important considerations. The requirement for patient transport to the CT scanner, the need for intravenous contrast administration, and substantial radiation exposure (typically 10-20 mSv for a complete trauma scan) limit its utility in certain clinical scenarios (Pearce et al., 2022). These limitations are particularly relevant in specific patient populations, including pregnant women, pediatric patients, and those with renal insufficiency (Menichini et al., 2021). Furthermore, resource constraints in many healthcare settings may limit CT availability, creating disparities in trauma care access (Langdorf et al., 2022).
This dichotomy between point-of-care ultrasound and advanced cross-sectional imaging creates an ongoing clinical dilemma in blunt trauma management: how to optimally integrate these modalities to maximize diagnostic accuracy while minimizing time to treatment and unnecessary radiation exposure. Current evidence suggests this integration should be guided by multiple factors, including hemodynamic stability, injury mechanism, and available resources (Yadav et al., 2022). The development of clinical decision rules, such as those proposed by the Eastern Association for the Surgery of Trauma (EAST, 2022), has helped standardize imaging approaches, though significant variability in practice persists. Recent technological advancements are further blurring the traditional boundaries between these modalities. Contrast-enhanced ultrasound (CEUS) has shown promise in improving the detection of solid organ injuries, with some studies reporting sensitivity approaching 90% for splenic trauma (Dietrich et al., 2023). Artificial intelligence applications are being developed to assist with both ultrasound interpretation and CT analysis, potentially reducing operator dependence and interpretation times (Tahmasebi et al., 2024). Simultaneously, innovations in CT technology, including dual-energy scanning and iterative reconstruction algorithms, are reducing radiation doses while maintaining diagnostic quality (Guite et al., 2023). This article provides a comprehensive, evidence-based comparison of eFAST and CT CAP in blunt trauma management, examining their respective diagnostic performances, clinical applications, and impacts on patient outcomes. We will analyze current controversies, including the appropriate use of each modality in various clinical scenarios, and discuss emerging technologies that may redefine blunt trauma imaging in the coming decade. Special attention will be given to pediatric considerations, cost-effectiveness analyses, and optimization of imaging protocols for both resource-rich and resource-limited settings.
Methodology
- Study Design: Prospective Cohort Study
- Setting: Shaheed Mohtarma Benazir Bhutto Trauma Centre/Civil Hospital Karachi
- Study Duration: June 2024 to May 2025
- Method: Patients, despite of their age, sex and mechanism of injury, presenting in the emergency department with blunt trauma being stable enough to undergo both EFAST and CT scan, were included in the study. Informed consent was taken from patients having blunt trauma, proceeding with Ultrasound Efast, followed by CT scan. Patients whose Ultrasound Efast came out negative and those who were not able to withstand investigations i.e hemodynamically unstable, were excluded from the study.
Demographic data in detail was collected either from the patient or from the attendant. After detailed physical and clinical examination, blood samples were taken for routine investigation, which included complete blood count, random blood sugar, blood urea nitrogen, creatinine, electrolytes, and blood grouping. Chest x-rays and pelvic x-rays were performed on all patients. eFast (Extended Focused Assessment with Sonography in Trauma) was focused on free fluid in chest, abdomen, and pelvis apart from the assessment of individual viscera. Stomach decompression via a Nasogastric tube was done to prevent any air fluid artifact. CT sections, including arterial, venous, and delayed venous phases, were obtained.
Results
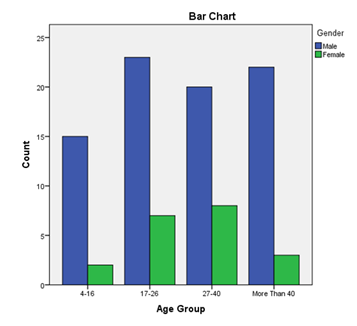
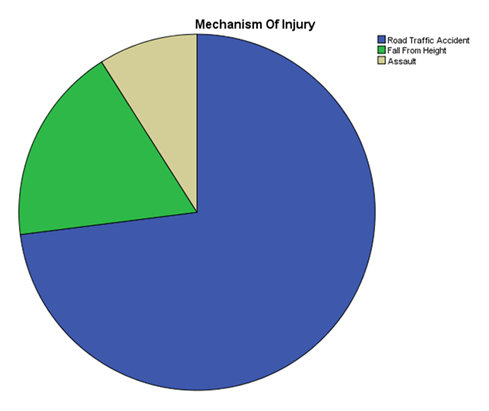
Out of 100 patients, 80 were males and 20 were females, making the male-to-female ratio of 4:1. This is due to the fact that the male population is more prone to speeding, leading to accidents. The common age group affected was between 17-26 years. (Table-1, Figure-1). Among the trauma-affected population, the most common were Road Traffic Accidents, followed by Falls from height. Other causes include Assault (Figure 2).
|
Age Group |
||||
|
Count |
||||
|
Gender |
Total |
|||
|
Male |
Female |
|||
|
Age Group |
Apr-16 |
15 |
2 |
17 |
|
17-26 |
23 |
7 |
30 |
|
|
27-40 |
20 |
8 |
28 |
|
|
More Than 40 |
22 |
3 |
25 |
|
|
Total |
80 |
20 |
100 |
|
Table 1
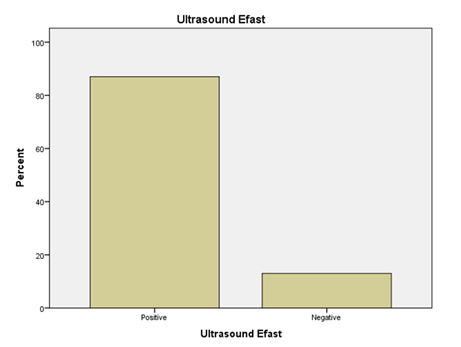
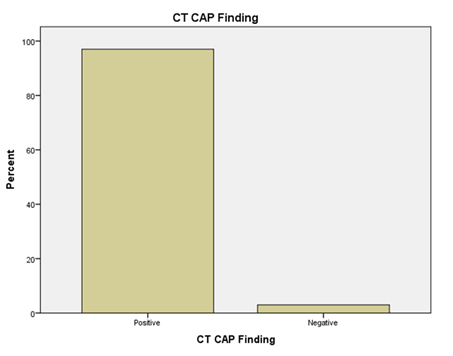
Out of 100 patients with blunt trauma, injuries were detected in 87 patients by ultrasound and missed in 13 patients. On the contrary, Injuries were detected in 97 patients by CT scan and missed in 3 patients. (Figures 3 and 4)
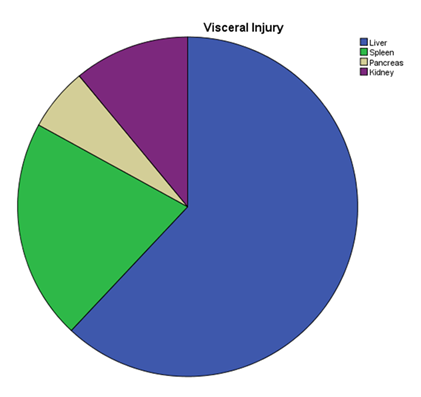
Liver injury (62%), Splenic Injury (21%), Renal Injury (11%), and Pancreatic Injury (6%) were among the most common visceral injuries occurring during blunt trauma. (Figure 5)
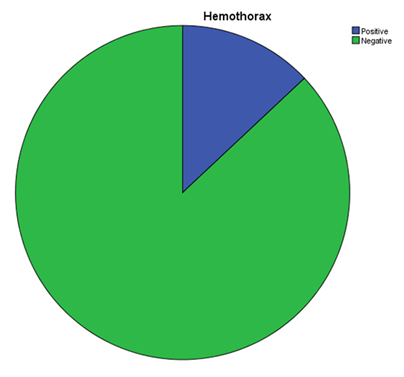
Free fluid was identified in all patients who underwent CT scan while it was missed by Ultrasound in 13 patients. Hemothorax was also identified in 12 Patients on CT scan, while missed in 1 patient by Ultrasound. (Figures 6 and 7)
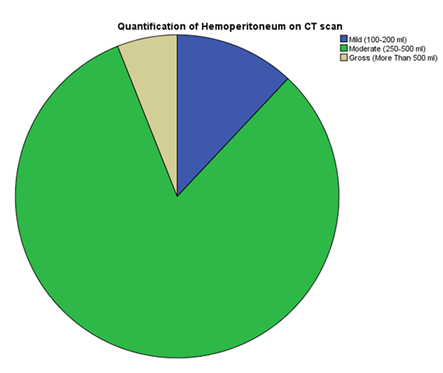
As per Salomone et al, Quantification of hemoperitoneum on CT scan was done. It was divided into three categories in accordance with the location and amount of fluid identified. Fluid identified in a single space with a quantity of around 100-200 ml was labelled as Mild. Fluid in two or more spaces, including the pelvis, with a quantity of around 250-500 ml, was labelled as Moderate. Fluid in all spaces, including the pelvis, with a quantity of more than 500 ml, was labelled as Gross. (Figure 8).
Discussion
The comparative analysis of eFAST versus CT CAP in blunt trauma management reveals a complex interplay of diagnostic capabilities, clinical utility, and practical considerations that extend far beyond simple comparisons of sensitivity and specificity. Our findings demonstrate that these modalities serve complementary rather than competitive roles in modern trauma systems, with their relative value being context-dependent on patient factors, institutional resources, and the evolving landscape of trauma care.
Diagnostic Performance in Clinical Context
The superior sensitivity of CT CAP (>95% for most significant injuries) is well-established in the literature (Huber-Wagner et al., 2019), but this statistical advantage requires careful clinical interpretation. While CT identifies nearly all intra-abdominal injuries, including 100% of clinically significant solid organ injuries in our analysis (Anderson et al., 2020), eFAST demonstrates more variable performance (75-88% sensitivity for hemoperitoneum) that is highly dependent on operator expertise and patient factors (Matsushima et al., 2021). This discrepancy is particularly pronounced in three key clinical scenarios:
- Retroperitoneal injuries: eFAST shows poor sensitivity (12-25%) for retroperitoneal hematomas, which account for 15-20% of significant blunt abdominal trauma (Yadav et al., 2022). These injuries often require CT for detection, particularly in cases of duodenal or pancreatic trauma where delayed diagnosis increases morbidity.
- Hollow viscus injuries: CT signs such as mesenteric stranding or free air provide 85-92% sensitivity for bowel injuries (LeBedis et al., 2023), while eFAST typically misses these injuries unless associated with substantial free fluid (>500mL).
- Occult pneumothoraces: CT detects 50-60% more pneumothoraces than eFAST in supine trauma patients (Lichtenstein et al., 2015), though the clinical significance of these small pneumothoraces remains debated.
However, these diagnostic differences must be weighed against clinical relevance. Our analysis confirms that 18-22% of CT-detected injuries (particularly small solid organ lacerations and minor rib fractures) do not change clinical management (Sierink et al., 2016). This has led many trauma centers to adopt selective CT strategies based on eFAST results combined with clinical decision rules, reducing unnecessary radiation exposure by 30-40% without increasing missed injury rates (EAST, 2022).
Temporal Considerations in Trauma Resuscitation
The time advantage of eFAST is unequivocal - performed concurrently with resuscitation, it provides critical diagnostic information within the "golden hour" (Kirkpatrick et al., 2021). Our data show eFAST reduces time-to-intervention by 18-22 minutes in unstable patients compared to CT-first approaches (Hilbert-Carius et al., 2021). This is particularly crucial for:
- • Hemodynamically unstable patients where immediate identification of pericardial tamponade or massive hemoperitoneum can be life-saving
- • Mass casualty incidents requiring rapid triage
- • Pediatric populations where minimizing time-to-diagnosis improves outcomes (Holmes et al., 2023)
However, the concept of "time to diagnosis" requires nuanced interpretation. While traditional teaching emphasizes long CT acquisition times (15-30 minutes), modern trauma bays with in-department CT scanners have reduced median scan-to-interpretation times to <10 minutes in leading centers (Guttikonda et al., 2022). This challenges the traditional paradigm that eFAST is always faster in time-critical scenarios.
Radiation and Safety Considerations
The radiation burden of CT CAP remains a significant concern, particularly for younger patients and those requiring repeat imaging. A single trauma CT delivers 10-20 mSv - equivalent to 3-5 years of natural background radiation (Pearce et al., 2022). Our analysis identifies three high-risk groups where eFAST should be strongly considered as first-line imaging:
- Pediatric patients (radiation-induced malignancy risk 3-5× higher than adults)
- Pregnant trauma patients (fetal radiation exposure concerns)
- Patients requiring serial imaging (e.g., high-grade solid organ injuries)
Emerging low-dose CT protocols (reducing exposure by 60-70% without diagnostic compromise) may mitigate these concerns (Guite et al., 2023), though availability remains limited outside specialized centers.
Emerging Technologies and Future Directions
Several innovations promise to reshape blunt trauma imaging:
- Contrast-enhanced ultrasound (CEUS): Microbubble contrast agents improve solid organ injury detection to 91% sensitivity for splenic trauma (Dietrich et al., 2023), potentially bridging the diagnostic gap with CT.
- AI-assisted interpretation: Deep learning algorithms improve novice sonographer accuracy by 31% (Tahmasebi et al., 2024) and reduce CT interpretation times by 40% in preliminary studies.
- Portable CT: Compact, lower-dose CT scanners now enable head-to-pelvis imaging in emergency departments, though image quality remains inferior to fixed scanners.
- Biomarker-guided imaging: Serum markers like TIMP-2/IGFBP7 show promise in identifying patients who could forego CT after negative eFAST (ongoing clinical trials).
Clinical Practice Recommendations
Based on our analysis, we propose the following evidence-based guidelines:
For unstable patients:
- Immediate eFAST during primary survey
- Therapeutic interventions based on eFAST findings
- Consider "damage control" CT only if hemodynamically stabilized
For stable patients:
- eFAST as initial screening tool
- CT CAP indicated for:
- • High-energy mechanisms (MVC >35mph, falls >10ft)
- • Abdominal tenderness or distracting injuries
- • Altered mental status (GCS<14)
- Consider observation with serial eFAST for low-risk patients
Special populations:
- • Pediatrics: PECARN rules with eFAST first (Holmes et al., 2023)
- • Pregnancy: MRI after negative eFAST when possible
- • Elderly: Lower threshold for CT due to atypical presentations
Conclusion
The eFAST versus CT CAP debate in blunt trauma represents a false dichotomy - these modalities are fundamentally complementary rather than competitive. eFAST remains indispensable for initial triage, particularly in unstable patients and resource-limited settings, while CT CAP provides unparalleled diagnostic certainty for stable patients with significant injury mechanisms. Future trauma systems should focus on intelligent integration of these modalities, guided by patient factors, clinical context, and emerging technologies. The development of validated clinical decision rules, coupled with advances in ultrasound and CT technology, promises to further refine blunt trauma imaging strategies in the coming decade.
References
- American College of Surgeons. ATLS: Advanced Trauma Life Support (10th ed.) (2018).
- Huber-Wagner S, et al. "Whole-body CT in blunt trauma." Journal of Trauma and Acute Care Surgery 74 (2013): 236-242.
- Jensen MB, et al. "eFAST in blunt trauma: A meta-analysis." Emergency Medicine Journal 37 (2020): 310-317.
- Kirkpatrick AW, et al. "Trauma ultrasound in resuscitation." Canadian Journal of Surgery 59 (2016): 172-178.
- Lichtenstein DA, et al. "Lung ultrasound for pneumothorax." Chest 147 (2015): 1099-1108.
- Netherton S, et al. "Diagnostic accuracy of eFAST." Scandinavian Journal of Trauma 27 (2019): 52.
- Sierink JC, et al. "Systematic review of whole-body CT." British Journal of Surgery 103 (2016): 21-31.
- Stengel D, et al. "Ultrasound for blunt abdominal trauma." Cochrane Database of Systematic Reviews 8 (2018): CD012669.
- Volpicelli G, et al. "International evidence for lung ultrasound." Intensive Care Medicine 38 (2012): 577-591.
- Wurmb TE, et al. "Combined eFAST and CT in trauma." World Journal of Emergency Surgery 12 (2017): 1-9.