Ultrasonic and Laboratory Predictors of Pregnancy Loss in Patients with Threatened Miscarriage: A Three-Year Observational Study
Article Information
Abd-Elhaseib Salah*
Department of Obstetrics and Gynecology, Menoufia University, Menoufia governorate, Egypt
*Corresponding Author: Abd-Elhaseib Salah, Department of Obstetrics and Gynecology, Menoufia University, Shibin El-Kom City, Menoufia governorate, Egypt
Received: 01 October 2019; Accepted: 12 October 2019; Published: 21 October 2019
Citation:
Abd-Elhaseib Salah. Ultrasonic and Laboratory Predictors of Pregnancy Loss in Patients with Threatened Miscarriage: A Three-Year Observational Study. Obstetrics and Gynecology Research 2 (2019): 080-087.
View / Download Pdf Share at FacebookAbstract
Objectives: The aim of this study was to assess the relation between different abnormalities of the yolk sac, serum level of Cancer Antigen 125 (CA-125) and serum level of Beta Human Chorionic Gonadotropin (β –HCG) as early predictors of first trimester pregnancy loss in patients with threatened miscarriage.
Methods: This prospective observational study was conducted on 292 pregnant women between six to 13 weeks of gestation who were suffered threatened miscarriage. Visualization of yolk sac and diameter were recorded by transvaginal ultrasound . Maternal serum CA-125 and β HCG were also measured. Pregnancy outcome was the main outcome measure. Data was collected and tabulated.
Results: There was highly Significant relation between YS size and pregnancy outcome (P<0.001). CA-125 and β-HCG were good predictors of miscarriage with accuracy 88%and 81.5% respectively.
Conclusions: Yolk sac size and maternal serum CA-125 and β-HCG are good predictors of pregnancy outcome in first trimester threatened miscarriage.
Keywords
Miscarriage; Cancer Antigen 125 (CA-125); Yolk sac; Beta Human Chorionic Gonadotropin (β-HCG)
Miscarriage articles Miscarriage Research articles Miscarriage review articles Miscarriage PubMed articles Miscarriage PubMed Central articles Miscarriage 2023 articles Miscarriage 2024 articles Miscarriage Scopus articles Miscarriage impact factor journals Miscarriage Scopus journals Miscarriage PubMed journals Miscarriage medical journals Miscarriage free journals Miscarriage best journals Miscarriage top journals Miscarriage free medical journals Miscarriage famous journals Miscarriage Google Scholar indexed journals Cancer Antigen 125 articles Cancer Antigen 125 Research articles Cancer Antigen 125 review articles Cancer Antigen 125 PubMed articles Cancer Antigen 125 PubMed Central articles Cancer Antigen 125 2023 articles Cancer Antigen 125 2024 articles Cancer Antigen 125 Scopus articles Cancer Antigen 125 impact factor journals Cancer Antigen 125 Scopus journals Cancer Antigen 125 PubMed journals Cancer Antigen 125 medical journals Cancer Antigen 125 free journals Cancer Antigen 125 best journals Cancer Antigen 125 top journals Cancer Antigen 125 free medical journals Cancer Antigen 125 famous journals Cancer Antigen 125 Google Scholar indexed journals Yolk sac articles Yolk sac Research articles Yolk sac review articles Yolk sac PubMed articles Yolk sac PubMed Central articles Yolk sac 2023 articles Yolk sac 2024 articles Yolk sac Scopus articles Yolk sac impact factor journals Yolk sac Scopus journals Yolk sac PubMed journals Yolk sac medical journals Yolk sac free journals Yolk sac best journals Yolk sac top journals Yolk sac free medical journals Yolk sac famous journals Yolk sac Google Scholar indexed journals Beta Human Chorionic Gonadotropin articles Beta Human Chorionic Gonadotropin Research articles Beta Human Chorionic Gonadotropin review articles Beta Human Chorionic Gonadotropin PubMed articles Beta Human Chorionic Gonadotropin PubMed Central articles Beta Human Chorionic Gonadotropin 2023 articles Beta Human Chorionic Gonadotropin 2024 articles Beta Human Chorionic Gonadotropin Scopus articles Beta Human Chorionic Gonadotropin impact factor journals Beta Human Chorionic Gonadotropin Scopus journals Beta Human Chorionic Gonadotropin PubMed journals Beta Human Chorionic Gonadotropin medical journals Beta Human Chorionic Gonadotropin free journals Beta Human Chorionic Gonadotropin best journals Beta Human Chorionic Gonadotropin top journals Beta Human Chorionic Gonadotropin free medical journals Beta Human Chorionic Gonadotropin famous journals Beta Human Chorionic Gonadotropin Google Scholar indexed journals gestational articles gestational Research articles gestational review articles gestational PubMed articles gestational PubMed Central articles gestational 2023 articles gestational 2024 articles gestational Scopus articles gestational impact factor journals gestational Scopus journals gestational PubMed journals gestational medical journals gestational free journals gestational best journals gestational top journals gestational free medical journals gestational famous journals gestational Google Scholar indexed journals fetal membrane articles fetal membrane Research articles fetal membrane review articles fetal membrane PubMed articles fetal membrane PubMed Central articles fetal membrane 2023 articles fetal membrane 2024 articles fetal membrane Scopus articles fetal membrane impact factor journals fetal membrane Scopus journals fetal membrane PubMed journals fetal membrane medical journals fetal membrane free journals fetal membrane best journals fetal membrane top journals fetal membrane free medical journals fetal membrane famous journals fetal membrane Google Scholar indexed journals ultrasound articles ultrasound Research articles ultrasound review articles ultrasound PubMed articles ultrasound PubMed Central articles ultrasound 2023 articles ultrasound 2024 articles ultrasound Scopus articles ultrasound impact factor journals ultrasound Scopus journals ultrasound PubMed journals ultrasound medical journals ultrasound free journals ultrasound best journals ultrasound top journals ultrasound free medical journals ultrasound famous journals ultrasound Google Scholar indexed journals Biomedical articles Biomedical Research articles Biomedical review articles Biomedical PubMed articles Biomedical PubMed Central articles Biomedical 2023 articles Biomedical 2024 articles Biomedical Scopus articles Biomedical impact factor journals Biomedical Scopus journals Biomedical PubMed journals Biomedical medical journals Biomedical free journals Biomedical best journals Biomedical top journals Biomedical free medical journals Biomedical famous journals Biomedical Google Scholar indexed journals Maternal articles Maternal Research articles Maternal review articles Maternal PubMed articles Maternal PubMed Central articles Maternal 2023 articles Maternal 2024 articles Maternal Scopus articles Maternal impact factor journals Maternal Scopus journals Maternal PubMed journals Maternal medical journals Maternal free journals Maternal best journals Maternal top journals Maternal free medical journals Maternal famous journals Maternal Google Scholar indexed journals complete pregnancy articles complete pregnancy Research articles complete pregnancy review articles complete pregnancy PubMed articles complete pregnancy PubMed Central articles complete pregnancy 2023 articles complete pregnancy 2024 articles complete pregnancy Scopus articles complete pregnancy impact factor journals complete pregnancy Scopus journals complete pregnancy PubMed journals complete pregnancy medical journals complete pregnancy free journals complete pregnancy best journals complete pregnancy top journals complete pregnancy free medical journals complete pregnancy famous journals complete pregnancy Google Scholar indexed journals
Article Details
1. Introduction
Miscarriage is defined as pregnancy loss before 20 weeks’ gestation and remains the most common complication of early pregnancy [1]. The yolk sac appears at the fifth week of gestation and the diameter increases steadily (0.1 mm/d) until the end of the 10th week. The upper limit of a normal yolk sac diameter in pregnancies with a gestational age of 5 to 10 weeks was defined as 5.6 mm [2, 3].Typically, when the 10th or 11th week of gestation is completed; the yolk sac starts to degenerate and rapidly shrinks [4]. Cancer antigen-125 (CA-125) is derived from embryonic coelomic epithelium and was used as a predictive marker for spontaneous abortion or subsequent pregnancy outcome particularly in women with threatened miscarriage [5, 6]. Disruption of the epithelial basement membrane of the fetal membrane or of the decidua could theoretically lead to a rise in the maternal CA-125 level; this increase may be a predictor of subsequent spontaneous miscarriage [6]. Beta subunit human chorionic gonadotropin (β-HCG) is produced during pregnancy. It is made by cells that form the placenta. A low β-HCG level could indicate: miscalculation of pregnancy dating, possible miscarriage, blighted ovum or ectopic pregnancy. A high β-HCG level can indicate miscalculation of pregnancy dating, molar pregnancy or multiple pregnancy [7].
The aim of this study was to assess the relation between different abnormalities of the yolk sac, serum level of Cancer Antigen 125 (CA-125) and serum level of Beta Human Chorionic Gonadotropin (β –HCG) as early predictors of first trimester pregnancy loss in patients with threatened miscarriage.
2. Materials and Methods
This prospective observational study was conducted on 292 women who attended the Antenatal clinic or Emergency room at the Department of Obstetrics and Gynecology, Menoufia University Hospital during the period between the beginnings of August 2016 and August 2019. The study protocol was formally reviewed and approved by the local review board and ethics committee at Menoufia Faculty of Medicine with all patients signed the informed consent for prior to conducting the study. Patients presented with threatened miscarriage after thorough history taking, clinical examination and transvaginal ultrasound were included in the study. Patients with missed miscarriage, multiple pregnancies and with any type of medical disorders as diabetes mellitus and hypertension were excluded from the study.
All enrolled patients underwent the followings:
- Transvaginal ultrasound (Sonata Plus 2009-02, IBE Technology, International Biomedical Engineering Technologies; with vaginal probe multi frequency four to nine MHZ) to measure yolk sac size and diameter in addition to crown rump length. Scanning was done in both coronal and sagittal planes.
- Blood sampling: Maternal venous blood samples were collected in plain blood collection tubes containing EDTA as anticoagulant.β-HCG and CA-125 were measured using immune assay system. The ARCHITECT Total β-HCG and CA-125 assay is a two-step immunoassay to determine the presence of β-HCG and CA-125 in human serum and plasma using Chemiluminescent Microparticle Immunoassay (CMIA) technology with flexible assay protocols, referred to a Chemiflex.
Serial follow up visits of patients (twice weekly) was adopted if patients declined to be admitted to hospital till the 14th week of gestation or pregnancy loss has occurred; whatever earlier.
2.1 Statistical analysis
Results were statistically analyzed by SPSS version 22 (SPSS Inc., Chikago, IL, USA). Non paired t test was used for parametric data. Mann-Whitney test was used for non-parametric data. Chi-Squared (χ2) and Fisher's exact tests were used for qualitative variables. Receiver operating characteristic (ROC curve) is a graphical plot of the sensitivity, vs. false positive rate (one minus the specificity). P value was considered significant if ≤0.05.
3. Results
Maternal characteristics including age, parity, body mass index and parity were depicted in table [1]. Βeta Human Chorionic Gonadotropin was significantly lower in the group (YS size >5 mm) than the group (YS size ≤≤5 mm) (P< 0.001), while CA-125 was significantly higher in the group (YS size >5 mm) than the group (YS size ≤ 5 mm) (P< 0.001). There was highly Significant relation between YS size and pregnancy outcome (P<0.001) as demonstrated in table [2] and figures [1]. Gestational age and HCG were significantly lower in abortion group than complete pregnancy group (P=0.015 and < 0.001 respectively). But YS size, CA-125 and threatened abortion were significantly higher in abortion group than complete pregnancy group (P <0.001, <0.001 and 0.002) respectively as shown in table [3]. Yolk Sac size, CA-125 and β-HCG were a good detector of miscarriage with accuracy 70.6%, 88% and 81.5% respectively as shown in table [4] and figure [2].
|
General characteristics |
Study group (n=292) |
|
Age (Years) Mean ± SD Range |
25.19 ± 5.64 17.0-42.0 |
|
Body mass index (kg/ m²) Mean ± SD Range |
29.12 ± 5.34 20.30-45.40 |
|
Gestational age (weeks) Mean ± SD Range |
7.06 ± 1.22 5.0-10.0 |
Table 1: Maternal characteristics.
|
|
Yolk sac size |
Mann-Whitney test
|
P value |
|||
|
>5mm No.=32 |
≤5 mm No.=260 |
|||||
|
Mean ± SD |
Mean ± SD |
|||||
|
β HCG Median Interquartile range |
17417.75 ± 6742.75 17301.0 11751.50-21380.0 |
31098.62 ± 15975.51 28334.50 19178.0-40092.25 |
3.60 |
<0.001** |
||
|
CA 125 Median Interquartile range |
43.85 ± 13.87 44.0 33.0-54.77 |
27.93 ± 10.74 29.05 19.70-32.80 |
4.23 |
<0.001** |
||
|
Outcome -Abortion -Ongoing pregnancy |
no |
% |
no |
% |
Fisher’s exact |
P value |
|
24 8 |
75.0 25.0 |
18 242 |
6.9 93.1 |
53.61 |
<0.001** |
|
Table 2: Distribution of the studied yolk sac group regarding β HCG, CA 125 and the pregnancy outcome.
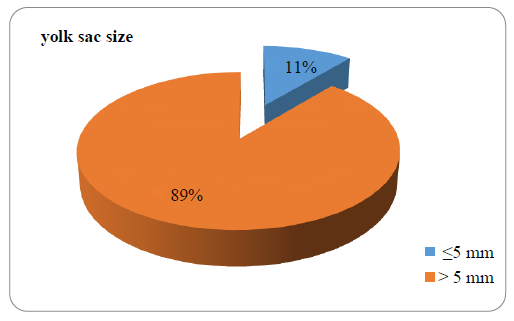
Figure 1: Distribution of the studied group regarding the size of yolk sac.
|
Age (Y) |
Outcome |
Test of sig |
P value |
|||
|
Abortion No.=21 |
Complete pregnancy No.=125 |
|||||
|
Mean ± SD |
Mean ± SD |
|||||
|
25.19 ± 6.41 |
25.20 ± 5.53 |
t= 0.01 |
0.994 |
|||
|
BMI (kg/ M2) |
28.69 ± 4.23 |
29.19 ± 5.52 |
t= 0.01 |
0.995 |
||
|
Gestational age (w) |
6.47 ± 0.74 |
7.16 ± 1.25 |
Mann-Whitney 2.44 |
0.015* |
||
|
Yolk sac size (mm) |
0.61 ± 0.30 |
0.34 ± 0.10 |
Mann-Whitney 6.36 |
<0.001** |
||
|
β HCG (mIU/ml) |
12983.52 ± 3742.94 |
32390.80 ± 15350.59 |
Mann-Whitney 7.31 |
<0.001** |
||
|
CA 125 (U/ml) |
52.61 ± 9.76 |
25.82 ± 7.28 |
Mann-Whitney 7.09 |
<0.001** |
||
|
Threatened abortion Yes No |
13 8 |
61.9 38.1 |
35 90 |
28.0 72.0 |
χ2 9.37 |
0.002* |
|
History of abortion Yes No |
18 3 |
85.7 14.3 |
105 20 |
84.0 16.0 |
Fisher’s exact 0.04 |
1.0 |
BMI =Body mass index; CA-125 =Cancer antigen 125; β HCG= Beta Human Chorionic Gonadotropin
Table 3: Comparison between results of the studied outcome regarding general and obstetric characteristics.
|
Variable |
AUC |
Cutoff point |
Sensitivity % |
Specificity % |
Accuracy % |
PPV % |
NPV % |
|
Yolk sac size |
0.81 |
≥ 0.42 |
67 |
82 |
70.6 |
39 |
94 |
|
β HCG |
0.93 |
≤ 20830 |
90.5 |
80 |
81.5 |
43 |
98 |
|
CA 125 |
0.98 |
≥ 33.25 |
95 |
87 |
88 |
55.5 |
99 |
Table 4: Validity of yolk sac size, B HCG and CA 125 regarding the outcome of pregnancy.
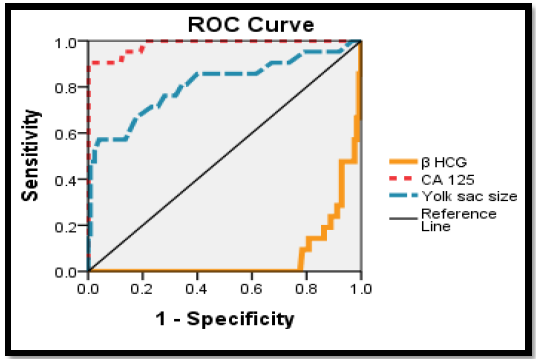
Figure 2: Roc curve for validity of yolk sac size, B HCG and CA 125 regarding the outcome of pregnancy.
4. Discussion
The clinical diagnosis of threatened miscarriage is presumed when any bloody vaginal discharge or bleeding appears during the first half of pregnancy; approximately half of women will abort [8]. In this study, yolk sac size, CA-125 and β-HCG were good predictors of pregnancy loss (spontaneous miscarriage). Yolk sac larger than five mm is a good indication that the probability of abortion will be significantly high [9-12]. A previous study on 305 pregnant women between the 6th to 9th weeks of gestation has revealed that an enlarged yolk sac visualized before the 7th week of gestation is strongly associated with a significantly increased risk for spontaneous miscarriage [10]. Revankar et al. [13] also stated that maternal serum CA-125 measurements appear to be a highly sensitive laboratory marker in patients with viable pregnancy with first trimester threatened miscarriage. The sensitivity, specificity, positive predictive value and negative predictive value of serum CA-125 with a cutoff 60 IU/ml in predicting miscarriage was 43.5%, 100%, 100%, and 67.5% respectively. Also, Maged et al. [14] support our study, they stated that the CA-125 and HCG were significant predictors of miscarriage in their study which done on 250 pregnant women. The sensitivity, specificity, positive predictive value and negative predictive value of serum CA-125 at the level of 80 IU/ml was 80.2%, 78.3%, 69.6% and 82.4% respectively. The sensitivity, specificity, positive predictive value and negative predictive value of serum HCG at the level of 19887 mIU/ml was 66.6%, 81.1%, 75.6% and 89.9% respectively.
More recent studies confirmed that serum β- HCG is a good predictor of miscarriage [15-17]. On the other hand, many other studies disagree with using yolk sac size [18-20] or laboratory markers either CA-125 [21] or β- HCG to be valuable for predicting pregnancy outcome in first trimester threatened miscarriage. These differences may be attributed to different patient populations, different clinical scenarios as well as different ultrasonic and laboratory testing techniques. The large cohort included and uniform protocol of follow up, constitutes the main strength of the current study. Inability to include a control group was unintended limitation of this study secondary to costly laboratory tests. Future research should explore the cost-effectiveness of combined testing for prediction of pregnancy outcome in patients with first trimester threatened miscarriage in a multicentre design.
5. Conclusions
Yolk sac size and maternal serum CA-125 and β-HCG are good predictors of pregnancy outcome in first trimester threatened miscarriage.
Conflict of interest
None declared.
Acknowledgments
The author would like to thank members of the Radiology and Clinical Pathology departments at
Menoufia University hospital for their logistic support.
References
- Faisal Mohammed Basama. The outcome of pregnancies in 182 with threatened miscarriage. Arch Gynecol Obstet 270 (2004): 86-90.
- Nogales FF, Beltran E, Gonzalez F. Morphological changes of the secondary human yolk sac in early pregnancy wastage. In: Nogales FF (ed) Human yolk sac and yolk sac tumor. Springer, Berlin, Heidelberg New York (1993): 174-194.
- Levi CS, Dashefsky SM, Lyons EA, Holt CS, Lindsay DJ.First-trimesterultrasound. In: McGahan JP, Goldberg BB (eds). Diagnostic Ultrasound:A Logical Approach. 1st ed. Philadelphia, PA: Lippincott-Raven (1997): 134-148.
- Gulbis B, Jauniaux E, Cotton F, Stordeur P. Protein and enzyme patterns in the fluid cavities of the first trimester gestational sac: relevance to the absorptive role of secondary yolk sac. Mol Hum Reprod 4 (1998): 857-862.
- Kabawat SE, bast RC, Bhan AK, Welch WR, Knapp RC, Colvin RB. Tissue distribution of a coelomic epithelium related antigen recognized by the monoclonal antibodies Ca-125. J Gynecol.Path 2 (1983): 275-285.
- Check JH, Nowrozi k, Winkel CA, Johnson T, Seefried L. Serum CA-125 levels in early pregnancy and subsequent spontaneous abortion,Obstet. Gynecol 75 (1990): 742-744.
- Schmidt T, Rein DT, Foth D, Eibach HW, Kurbacher CM, Mallmann Pchmidt T, et al. Prognostic value of repeated serum CA 125 measurements in first trimester pregnancy. Eur J Obstet Gynecol Reprod Biol 97 (2001): 168-173.
- Hasan R, Baird DD, Herring AH, Olshan AF, Jonsson Funk ML, Hartmann KE. Patterns and predictors of vaginal bleeding in the first trimester of pregnancy. Ann Epidemiol 20 (2010): 524-531.
- Mordan S, forouzeshfar M. Are Abnormal Yolk Sac Characteristic Important Factors in Abortion Rates? Int J Fertil Steril 6 (2012): 127-130.
- Tan S, Gülden N, Kanat-Pektas M , Özcan AS , Keskin H , Akgündüz G, et al. Abnormal sonographic appearances of the yolk sac: which can be associated with adverse perinatal outcome? Med Ultrason 16 (2014): 15-20.
- Berdahl DM, Blaine J, Van Voorhis B, Dokras A. Detection of enlarged yolk sac on early ultrasound is associated with adverse pregnancy outcomes. Fertil Steril 94 (2010): 1535-1537.
- Kumari S, Roy Roychowdhury J, Biswas S. Prediction of early pregnancy failure by use of first trimester ultrasound screening. Int J Reprod Contracept Obstet Gynecol 5(2016): 2135-2140.
- Revankar VM, Aggarwal A, Manohar RG. Comparison of CA-125 levels in threatened abortion and normal pregnancies. World Journal of Pharmacy and Pharmaceutical Sciences 4 (2015): 1357-1364.
- Maged A, Ghada A, Eman E, Rasha B, Dalia A. Correlation of Serum CA-125 and Progesterone Levels with Ultrasound Markers in The Prediction of Pregnancy Outcome in Threatened Miscarriage. Int J Fertil Steril 9 (2016): 506-511.
- Al-Sebai M, Diver M, Hipkinw L. The role of a single free p-human chorionic gonadotrophin measurement in the diagnosis of early pregnancy failure and the prognosis of fetal viability. Hum Reprod 11 (1995): 881-888.
- Osmana?ao?lu MA, Karahan SC, Aran T, Güven S, Turgut E, Mente?e A, et al. The diagnostic value of β-human chorionic gonadotropin, progesterone, and ischemia-modified albumin and their combined use in the prediction of first trimester abortions. Int Sch Res Notices (2014): 1-5.
- Ali H M, Salman ST, Ibrahim HK. Prediction of Pregnancy Outcome Using HCG, CA125 and Progesterone in Cases of Habitual Abortions; Diyala Journal of Medicine 5 (2013): 63-68.
- Cho FN, Chen SN, Tai MH, Yang TL. The quality and size of yolk sac in early pregnancy loss. Aust NZ J Obstet Gynaecol 46 (2006): 413-418
- Makrydimas G, Sebire NJ, Lolis D, Vlassis N, Nicolaides KH. Fetal loss following ultrasound diagnosis of alive fetus at 6 -10 weeks of gestation. Ultrasound Obstet Gynecol 22 (2003): 368-372.
- Maged AM, Al-Mostafa W. Biochemical and ultrasonographic predictors of outcome in threatened abortion. Middle East Fertil Soc J 18 (2013): 177-181.
- Mahdi B. Estimation of CA-125 level in First trimester threatened abortion. Int J Gynaecol Obstet 12 (2009): 1-5.
- Memtsa M, Jauniaux E, Gulbis B, Nyrhinen NC, Jurkovic D. Maternal serum markers in predicting successful outcome in expectant management of missed miscarriage. Reprod Biomed Online 34 (2017): 98-103.
