Type of Delivery and Functional Constipation at 48 Months of Age: Cohort Study
Article Information
Analida Pinto Buelvas1*, Bianca Del Ponte2, Alicia Matijasevich3, Denise Marques4, Rita Mattiello1, Iná S Santos2
1Post-graduate Program in Pediatrics and Child Health, School of Medicine, Pontifical Catholic University of Rio Grande do Sul, RS, Brazil
2Post-graduate Program in Epidemiology, Faculty of Medicine, Federal University of Pelotas, RS, Brazil
3Department of Preventive medicine, Faculty of Medicine FMUSP, University of São Paulo, SP, Brazil
4Department of Materno-Infantil, Faculty of Medicine, Federal University of Pelotas, RS, Brazil
*Corresponding Author: Analida Pinto Buelvas. Post-graduate Program in Pediatrics and Child Health, School of Medicine, Pontifical Catholic University of Rio Grande do Sul, Rua Josemaria Escriva, 669, apartamento 623, Central Park, Porto Alegre, RS, 91410-470, Brazil
Received: 25 February 2022; Accepted: 09 March 2022; Published: 13 April 2022
Citation:
Analida Pinto Buelvas, Bianca Del Ponte, Alicia Matijasevich, Denise Marques, Rita Mattiello, Iná S Santos. Type of Delivery and Functional Constipation at 48 Months of Age: Cohort Study. Journal of Pediatrics, Perinatology and Child Health 6 (2022): 219-232.
View / Download Pdf Share at FacebookAbstract
Background: Several factors have been associated with childhood functional constipation; more recently, the type of delivery has been investigated. This study examined the association between cesarean section and constipation at 48 months of age in the 2004 birth cohort conducted in the city of Pelotas in Brazil.
Methods: Information on type of delivery (vaginal or cesarean) was extracted from medical records at the hospital of birth. Functional constipation was assessed by interviewing the mother in a 48-month follow-up assessment and was defined as the combination of at least two of the following symptoms in the last month: bowel movements ≤ 2 days/week, hard/scybalous stools, and difficult bowel movements. The prevalence of constipation according to delivery type was calculated. Crude and adjusted relative risks (95% confidence interval) were obtained by Poisson regression with robust variance.
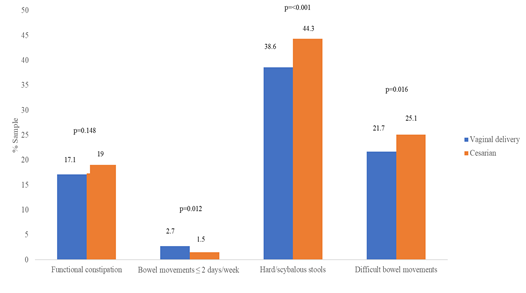
Results: A total of 3,720 children were analyzed, 44.5% of whom were born via caesarean section. The prevalence of functional constipation was 17.1% (15.5-18.8%) among those born vaginally and 19.0% (17.2-21.0%) among those born via caesarean section. Reports of bowel movements ≤ 2 days/week were more frequent among those born vaginally (2.7% vs. 1.5%), while hard/scybalous stools (38.6% vs. 44.3%) and difficult bowel movements (21.7% vs. 25.1%) were more frequent among those born via cesarean section. In the adjusted analysis, there was no association between type of delivery and intestinal constipation (RR = 0.98; 0.84-1.15).
Conclusions: The prevalence of functional consti-pation was high at 48 months of age, and cesarean sections were not related to its occurrence.
Keywords
Constipation, Cesarean Section, Microbiota, Mode of Delivery
Article Details
1. Introduction
Functional constipation is a functional disorder of the gastrointestinal tract and considered a growing health problem worldwide, particularly in children. It can negatively affect children’s emotional, social, and physical well-being considerably as well as increase healthcare costs [1, 2]. A recent meta-analysis showed that the prevalence of functional constipation in children ranged from 0.5% to 32.2%, with an estimated global pooled prevalence of functional constipation of 9.5% (95%CI 7.5-12.1%) [3]. The wide variation in prevalence may arise from several factors such as genetic, lifestyle, and socioeconomic conditions [3]. This meta-analysis also showed a low prevalence in Asia and the highest prevalence in Europe and the Americas. In Central and South America, the pooled prevalence was 13.3% (95%CI 11.2-15.8%). Studies in Brazil among children aged 1 to 18 years old showed prevalence rates ranging from 10% to 38% [4-8].
In recent decades, there has been an increase in the number of studies exploring the association between cesarean births and the development of diseases in childhood, including functional gastrointestinal disorders [9-18]. A possible justification for this is that cesarean births differ from vaginal births in the process by which microbes are passed from the mother to her infant. During and after passage through the birth canal, vaginal delivery exposes the neonate to a wide variety of microbes from the vaginal fora and intestinal microbiota. The microbiota can impact the health status of the host through modulation of energy harvesting, the immune system, metabolic and hormonal signaling, and xenobiotic metabolism. Through these mechanisms the gut microbiota has been related with a large variety of health disorders, including functional constipation [19]. Despite there being biological plausibility for the association between the type of delivery and intestinal constipation in childhood, few studies have explored this association and their results are not consistent [14-16]. Evidence regarding risk factors related to functional constipation in early childhood can offer critical clues to its etiology and help guide the development of preventive strategies. Thus, this study aimed to investigate the association between the type of delivery and functional constipation at 48 months of age, among children belonging to a birth cohort.
2. Material and Methods
2.1 Participants
The 4,263 children born between January 1st and December 31st of 2004, of mothers living in the urban zone of the municipality of Pelotas or in Jardim América – a neighborhood bordering Pelotas and belonging to the neighboring municipality of Capão do Leão – were identified and their mothers were invited to form part of the 2004 Pelotas Birth Cohort. Pelotas is a city of 328,275 inhabitants, located in the south of Brazil. Only 32 mothers (0.8%) refused to participate in the study and so 4,231 children were included in the cohort. In the first 24 hours after delivery, the mothers were interviewed by trained interviewers, using a previously tested structured questionnaire to collect information about socio-economic, demographic, reproductive, and behavioral characteristics. The newborns were weighed and measured. After the child’s enrollment at the hospital of birth (perinatal study), six follow-ups were carried out (at 3, 12, 24, and 48 months and at 6 and 11 years of age), with follow-up rates of 95.7%, 94.3%, 93.5%, 92.0%, 90.2%, and 86.6%, respectively. The mean age (standard deviation) of the children in these follow-ups was 3.1 (0.1), 11.9 (18.1), 23.9 (0.6), and 50.3 (1.8) months and 6.7 (0.2) and 10.9 (0.3) years old. Methodological details of the cohort can be obtained in another publication [20]. This study included the children born from single gestations.
2.2 Outcome
The presence of functional intestinal constipation was defined as the combination of at least two of the following symptoms in the last month: bowel movements ≤ 2 days/week, a history of hard or scybalous stools, and difficult bowel movements. The questions used to construct the outcome were applied to the person responsible for the child: “In the last month, how many days a week did <CHILD> poop?”; “In the last month, was <CHILD’s> poop in little balls?”; “In the last month, did <CHILD> have difficulty pooping?”
2.3 Exposure of interest
The exposure of interest was the type of delivery. Those children who had a surgical delivery were considered as born via cesarean (exposed), according to information extracted from the medical records during the perinatal assessment.
2.4 Potential confounders
The potential confounding variables included characteristics of the family, mother, and of the child. Regarding the family, monthly income was used, corresponding to the sum of the values perceived for all residents of the household, in the month prior to the child’s birth, subsequently grouped in quintiles. The maternal characteristics included full years of schooling (subsequently categorized as 0-4, 5-9, or > 9 years), marital status (lives with a husband or partner; yes or no), pre-gestational body mass index (BMI) (later categorized as < 18.5, 18.5-24.9, 25.0-29.9, or ≥ 30 kg/m2) [21], smoking during pregnancy (one or more cigarettes a day, every day, in any trimester of the pregnancy; yes or no), age at the time of delivery (subsequently categorized as < 20, 20-25, 26-30, 31-35, or > 35 years old), and parity (0, 1, or ≥ 2 deliveries prior to that of 2004). Regarding the child’s characteristics at birth, the following variables were used: sex (female or male), skin color self-reported by the mother (white, brown, or black, which also included yellow and indigenous), birth weight (subsequently categorized as < 2000, 2000-2499, 2500-2999, or ≥ 3000 grams), and gestational age (later classified as < 32, 32-33, 34-36, 37-38, or 39-41 weeks).
2.5 Ethical aspects
The perinatal study and 48-month follow-up of the cohort were approved by the Ethics Committee of the School of Medicine of the Federal University of Pelotas (approval protocols 40601116 and 012/07, respectively). The mother or legal guardian signed a free and informed consent form before the data collection.
2.6 Analysis
The general prevalence of functional intestinal constipation and of each one of the constipation symptoms in the last month (bowel movement frequency ≤ 2 days/week, history of hard or scybalous stools, or history of difficult bowel movements) were calculated. Afterwards, the general prevalence of constipation and of each one of the constipation symptoms were calculated, according to the delivery type. The difference in the prevalence of functional intestinal constipation according to delivery type was analyzed by Chi-squared test. The strength of the association between cesarean section and functional intestinal constipation and between cesarean section and each one of the constipation symptoms was analyzed using crude and adjusted Poisson regression, with robust variance, obtaining relative risks (RR), with the respective 95% confidence intervals (95%CI). The analyses were first adjusted for family income and maternal characteristics (first level), and then for variables of the child at birth (second level). In each level, the adjustment variables were removed one by one using the backward stepwise method (from the highest to the lowest p value), and those that were associated with the outcome at p ≤ 0.20 were kept in the model. A two-tailed p < 0.05 was set as significant. A sensitivity analysis was run after excluding children with a history of diarrhea in the 15 days prior to the interview, since symptoms of irritable bowel syndrome, which is characterized by alternating periods of constipation and diarrhea [22, 23], were not investigated. All the analyses were conducted using the Stata 12.0 statistical package.
3. Results
Altogether, 3,720 children with available information on delivery type and the outcome of interest were included in the analyses. The distribution of the children according to family income and maternal characteristics is shown in Table 1. Due to the methodology used, around 20% of the families belonged to each one of the income quintiles. More than 40% of the mothers (43.5%) had more than nine years of schooling, the majority (84.3%) lived with their husband or partner, 12.3% had a pre-gestational BMI ≥ 30 kg/m2, and 27.2% smoked during the pregnancy. Regarding age, 18.9% were under 20 and 8.1% were over 35 years old. Around 40% were primiparas and 44.5% had a caesarian delivery.
Table 2 shows the distribution of the sample according to characteristics of the child at birth. Most of the children were male (52.0%) and were reported as having white skin (66.5%). The prevalence of LBW and preterm births was 8.1% and 13.7%, respectively. Among all of the children, 81 (2.2%) presented a bowel movement frequency of ≤ 2 days/week, 1,527 (41.0%) had a history of hard or scybalous stools, and 863 (23.2%) had difficult bowel movements in the previous month, with a general prevalence of functional intestinal constipation of 17.9% (16.7-19.2%). The prevalence of functional intestinal constipation and of constipation symptoms, according to delivery type, is shown in Figure 1. There was no difference in the prevalence of functional intestinal constipation according to delivery type: 17.1% (15.5-18.8%) among those born vaginally and 19.0% (17.2-21.0%) among those born via cesarean section. Reports of bowel movements ≤ 2 days a week were more frequent among children born vaginally (2.7%; 2.0-3.4%) than among those born via cesarean (1.5%; 0.9-2.1%). Reports of hard/scybalous stools (44.3%; 41.9-46.7%) and difficult bowel movements (25.1%; 23.0-27.1%) were more frequent among children born via cesarean than among those born vaginally, for whom the prevalence was 38.6% (36.5-40.7%) and 21.7% (19.9-23.5%), respectively.
Table 3 shows the crude and adjusted associations between delivery type and both functional constipation and symptoms of functional constipation at 48 months of age. In the crude and adjusted analyses there was no association between the type of delivery and functional intestinal constipation. Regarding the symptoms of constipation, there was a statistical association in the crude analyses: bowel movements ≤ 2 days/week were 44% less likely to be reported by children born by cesarean section, whereas hard/scybalous stools and difficult bowel movements were 15% more likely to be reported by children born via cesarean section. However, all the associations lost significance after adjusting for confounders. The results of the sensitivity analyses are shown in Table 4. A total of 314 (8.4%) children were excluded from these analyses. The values for the likelihood of functional intestinal constipation or of its symptoms in isolation were very similar to those obtained in the previous analysis.
|
N |
% |
|
|
Family income (quintile) |
||
|
1st |
737 |
19.8 |
|
2nd |
747 |
20.1 |
|
3rd |
740 |
19.9 |
|
4th |
780 |
21.0 |
|
5th |
716 |
19.2 |
|
Schooling (years completed) |
||
|
0-4 |
556 |
15.2 |
|
5-9 |
1527 |
41.4 |
|
> 9 |
1602 |
43.5 |
|
Marital status |
||
|
With a partner |
3137 |
84.3 |
|
Pre-gestational BMI (kg/m2) |
||
|
< 18.5 |
76 |
3.5 |
|
18.5-24.9 |
1253 |
57.2 |
|
25.0-29.9 |
592 |
27.0 |
|
≥ 30 |
272 |
12.3 |
|
Smoked during pregnancy |
||
|
Yes |
1013 |
27.2 |
|
Age (years) |
||
|
< 20 |
702 |
18.9 |
|
20-25 |
1171 |
31.5 |
|
26-30 |
816 |
22.0 |
|
31-35 |
725 |
19.5 |
|
> 35 |
304 |
8.1 |
|
Parity |
||
|
0 |
1469 |
39.5 |
|
1 |
984 |
26.5 |
|
≥ 2 |
1266 |
34.0 |
|
Delivery type |
||
|
Vaginal |
2064 |
55.5 |
|
Cesarean |
1656 |
44.5 |
Table 1: Distribution of the sample according to family income and maternal characteristics (N=3,720).
|
|
N |
% |
|
Sex |
||
|
Male |
1934 |
52.0 |
|
Female |
1825 |
48.0 |
|
Skin color |
||
|
White |
2520 |
66.5 |
|
Brown |
459 |
16.2 |
|
Black |
470 |
17.3 |
|
Weight at birth (grams) |
||
|
< 2000 |
78 |
2.1 |
|
2000-2499 |
222 |
6.0 |
|
2500-2999 |
960 |
25.8 |
|
≥ 3000 |
2459 |
66.1 |
|
Gestational age (weeks) |
||
|
< 32 |
38 |
1.1 |
|
32-33 |
48 |
1.4 |
|
34-36 |
390 |
11.2 |
|
37-38 |
1132 |
32.6 |
|
39-41 |
1866 |
53.7 |
Table 2: Distribution of the sample according to characteristics of the child at birth (N= 3,720).
|
Relative risk |
95%CI |
p |
|
|
Intestinal constipation |
|||
|
Crude model: |
0.159 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.12 |
0.96-1.30 |
|
|
Adjusted model:1 |
0.796 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.98 |
0.84-1.15 |
|
|
Bowel movements ≤ 2 days/week |
|||
|
Crude model: |
0.015 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.56 |
0.35-0.89 |
|
|
Adjusted model:2 |
0.068 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.63 |
0.39-1.03 |
|
|
Hard/scybalous stools |
|||
|
Crude model: |
0.007 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.15 |
1.04-1.27 |
|
|
Adjusted model:3 |
0.434 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.04 |
0.94-1.16 |
|
|
Difficult bowel movements |
|||
|
Crude model: |
0.036 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.15 |
1.01-1.32 |
|
|
Adjusted model: 4 |
0.557 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.04 |
0.91-1.20 |
|
1 Adjusted for family income, maternal age, and sex of the child
2 Adjusted for maternal schooling and birth weight
3 Adjusted for family income, maternal age, maternal schooling, parity, sex of the child, and skin color of the child
4 Adjusted for family income, maternal age, parity, and sex of the child
Table 3: Crude and adjusted relative risk, with 95% confidence interval (95%CI), for the associations between delivery type and both functional intestinal constipation and symptoms of functional intestinal constipation, at 48 months of age.
|
Odds Ratio |
CI 95% |
p |
|
|
Intestinal constipation |
|||
|
Crude model: |
0.094 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.15 |
0.98-1.34 |
|
|
Adjusted model:1 |
0.882 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.99 |
0.83-1.17 |
|
|
Bowel movements ≤ 2 days/week |
|||
|
Crude model: |
0.013 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.53 |
0.32-0.87 |
|
|
Adjusted model:2 |
0.055 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
0.60 |
0.36-1.01 |
|
|
Hard/scybalous stools |
|||
|
Crude model: |
0.004 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.16 |
1.05-1.29 |
|
|
Adjusted model:3 |
0.338 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.06 |
0.95-1.18 |
|
|
Difficult bowel movements |
|||
|
Crude model: |
0.010 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.20 |
1.04-1.38 |
|
|
Adjusted model:4 |
0.258 |
||
|
Vaginal delivery |
1.00 |
||
|
Cesarean |
1.09 |
0.94-1.26 |
|
1 Adjusted for family income, maternal age, parity, sex of the child, and gestational age
2 Adjusted for maternal schooling and birth weight
3 Adjusted for family income, maternal schooling, maternal age, and parity
4 Adjusted for family income, maternal age, parity, and sex of the child
Table 4: Crude and adjusted relative risk, with 95% confidence interval (95%CI), for the associations between delivery type and both intestinal constipation and symptoms of intestinal constipation, at 48 months of age, after excluding the children with a history of diarrhea in the 15 days prior to the interview.
4. Discussion
This study showed a high frequency of functional intestinal constipation among children aged 48 months in our setting. Almost one in every five children presented at least two of the symptoms of functional intestinal constipation investigated. Reports of hard or scybalous stools and of difficult bowel movements had a high prevalence in the sample (41.0% and 23.2%, respectively), whereas the history of ≤ 2 days/week with bowel movements was a rare event (2.2%). Contrary to the original hypo-thesis, this study did not identify any association between the delivery type and functional intestinal constipation at 48 months of age. This finding differs from that of a cross-sectional study conducted in Mexico in 2015 with 300 children aged 1-5 years old, in which those born via cesarean section had 7.8 times more chance of presenting intestinal consti-pation than those born vaginally [14]. However, the authors did not report the definition of constipation used in the study. A cohort study conducted in Japan (Japan Environment and Children’s Study – JECS) with 83,019 children aged one year old found a prevalence of intestinal constipation in the whole cohort of 1.4%, with no difference in the crude and adjusted risk ratios among children born via cesarean and those born vaginally [15].
This study defined intestinal constipation by the presence of a single criterion (chronic fecal retention, defined as a defecation frequency of < 3 times/week) [24, 25]. Besides the age group of the participants, the use of a different criterion for identifying intestinal constipation makes any comparison with our findings difficult. Recently, this group found a weak association between cesarian sections and functional constipation in 3-year-old Japanese child-ren (odds ratio = 1.06; 1.00-1.12) [16]. In this study, functional constipation was evaluated using the Rome III criteria. A possible explanation for the weak or no association described is that other factors such as genetics, lifestyle, socioeconomic status, educational level, and psychological and environm-ental factors (such as having to use sanitary facilities at school) [26, 27] may have a more significant impact than type of delivery on functional consti-pation. This reinforces the importance of studying the association in different populations. Nevertheless, it remains difficult to draw strong conclusions regarding factors that might be associated with functional constipation, considering that most of the current evidence is from cross-sectional studies.
C-sections are considered an important risk factor for a number of immune and metabolic diseases. How-ever, C-sections have increased worldwide over the last decades. Currently, South America is the region with the highest cesarian section rate (42.9%). This peculiarity may be due to a number of factors, such as: low maternal self-efficacy, a fear of childbirth and labor pains, and a predisposition by the medical team to perform the surgery. Unfortunately, it could be said that C-sections have become a part of the current motherly lifestyle [28]. In Brazil, cesareans have become more common than vaginal deliveries [29]. A total of 11,774,665 live births were reported in Brazil in the period from 2014 to 2017, most of which were delivered via cesarean (55.8%). The difference in the gut microbial composition and diversification resulting from cesarean births may contribute to an increase in calorie capture by the intestine, which would favor the development of obesity [30].
Atypical neonatal colonization in the intestine can persist for several years [31] and influence the intestinal immune response [32], as well as mucosal barrier function. That altered mucosal barrier function can be important in the pathogenesis of autoimmune entities, such as celiac disease, as the translocation of gliadin peptides through the intes-tinal epithelium is a key element in that mechanism [32]. The theory of the hypothalamic-pituitary-adrenal (HPA) axis suggests that the increase in cortisol concentrations at the moment of vaginal delivery would stimulate the HPA axis, which would have a negative feedback effect over inflammatory and immune reactions [33]. The results of the studies that have evaluated these associations, however, are controversial, with some finding a risk association and others finding no association [10, 15, 34-37].
This study has strengths and limitations. Among the strengths is the fact that it is the first study to investigate the association between delivery type and functional constipation among preschoolers in Latin America [22, 23]. Moreover, information was collected about various potential maternal and child-related confounders, which were considered in the adjusted analyses. In addition, the symptoms sugg-estive of functional intestinal constipation were also analyzed separately and a sensitivity analysis was conducted, to exclude possible cases of irritable bowel syndrome. Furthermore, the cohort design, the large sample size, and the follow-up rate of more than 90% at the age at which the outcome was evaluated are positive methodological aspects of the study.
The main limitation of the study was the absence of information on the other symptoms and signs of functional constipation proposed by international guidelines [22, 23]. We had no information on fecal incontinence, history of retentive posturing or excessive volitional stool retention, the presence of a large fecal mass in the rectum, or history of large diameter stools that can obstruct the toilet. Another limitation was the lack of information about family history of intestinal constipation, a factor previously identified as being associated with functional intestinal constipation in childhood [25]. Moreover, the fact that the child’s intestinal habit was obtained through information from the mother may be subject to information bias. It is worth noting that in a previous study with the same cohort at four years of age the prevalence of functional constipation was 31.0%, [24] as defined following the modified Rome II criteria according to the presence of two of the following symptoms: hard stools, scybalous stools, evacuations with blood, difficulty in evacuating, interval between successive evacuations >72 hours, and the use of laxatives during the last 30 days. This difference highlights the importance of the criteria for calculating the prevalence of functional constipation in childhood.
- Conclusion
In our study, the prevalence of functional intestinal constipation among children aged 48 months was high. After controlling for confounding factors, no association was found between delivery type and functional intestinal constipation or with its symptoms.
Acknowledgments
This article was produced with data from the study “2004 Pelotas Birth Cohort,” conducted by the Post-graduation Program in Epidemiology of the Federal University of Pelotas, with support from the Brazilian Association of Collective Health (ABRASCO). From 2009 to 2013, the 2004 birth cohort was financed by the Wellcome Trust. Previous phases of the study were financed by the World Health Organization, the Support Program for Centers of Excellence (PRONEX), the National Council for Scientific and Technological Development (CNPq), the Ministry of Health, and Pastoral da Criança. The present study was conducted with the support of the Coordination for the Improvement of Higher Education Personnel – Brazil (CAPES) – Financing Code 01. AM, RM, and ISS receive support from the CNPq.
Funding Statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of Interest
None
References
- Liyanarachchi H, Rajindrajith S, Kuruppu C, et al. Association between childhood constipation and exposure to stressful life events: a systematic review. Neurogastro-enterol Motil (2021): 1-9.
- Vriesman MH, Rajindrajith S, Koppen IJN, et al. Quality of Life in Children with Functional Constipation: A Systematic Review and Meta-Analysis. J Pediatr. United States (2019).
- Koppen IJN, Vriesman MH, Saps M, et al. Prevalence of Functional Defecation Disorders in Children: A Systematic Review and Meta-Analysis. J Pediatr. United States 198 (2018): 121-130.e6.
- Costa ML, Oliveira JN, Tahan S, et al. Overweight and constipation in adolescents. BMC Gastroenterol. England 11 (2011): 40.
- Fraga LGA, Sampaio A, Boa-Sorte N, et al. Obesity and lower urinary tract dysfunction in children and adolescents: Further research into new relationships. J Pediatr Urol. England 13 (2017): 387.e1-387.e6.
- Lewis ML, Palsson OS, Whitehead WE, et al. Prevalence of Functional Gastrointestinal Disorders in Children and Adolescents. J Pediatr. United States 177 (2016): 39-43.e3.
- Morais MB de, Maffei HV. Constipação intestinal. J pediatr (Rio J) (2000): 76.
- Ciampo IRL Del, Galvão LC, Ciampo LA Del, et al. Prevalence of chronic constipation in children at a primary health care unit. J Pediatr (Rio J) (2002).
- Kuhle S, Tong OS, Woolcott CG. Association between caesarean section and childhood obesity: A systematic review and meta-analysis. Obes. Rev (2015).
- Kristensen K, Henriksen L. Cesarean section and disease associated with immune function. J Allergy Clin Immunol (2016).
- Bager P, Simonsen J, Nielsen NM, et al. Cesarean section and offspring’s risk of inflammatory bowel disease: A national cohort study. Inflamm Bowel Dis (2012).
- Decker E, Hornef M, Stockinger S. Cesarean delivery is associated with celiac disease but not inflammatory bowel disease in children. Gut Microbes (2011).
- Cardwell CR, Stene LC, Joner G, et al. Caesarean section is associated with an increased risk of childhood-onset type 1 diabetes mellitus: A meta-analysis of observational studies. Diabetologia (2008).
- Zúñiga Carrasco IR, Caro Lozano J, Franco Castañeda P del C. Cesárea como factor condicionante de estreñimiento, dermatitis y alergias en niños de dos unidades del Instituto Mexicano del Seguro Social. Alergia, Asma e Inmunol Pediátrica (2015).
- Yoshida T, Matsumura K, Tsuchida A, et al. Association between cesarean section and constipation in infants: the Japan Enviro-nment and Children’s Study (JECS). BMC Res Notes. England 11 (2018): 882.
- Nakamura M, Matsumura K, Ohnuma Y, et al. Association of cesarean birth with prevalence of functional constipation in toddlers at 3 years of age: results from the Japan Environment and Children’s Study (JECS). BMC Pediatr 21 (2021): 419.
- Moreno-Galarraga L, Romanos Nanclares A, García-Blanco L, et al. Caesarean delivery is associated with an absolute increase in the prevalence of overweight in the offspring: The SENDO project. J Paediatr Child Health 57 (2021): 819-825.
- Zhang T, Sidorchuk A, Sevilla-Cermeño L, et al. Association of Cesarean Delivery With Risk of Neurodevelopmental and Psychiatric Disorders in the Offspring: A Systematic Review and Meta-analysis. JAMA Netw open (2019).
- Scheithauer TPM, Dallinga-Thie GM, de Vos WM, et al. Causality of small and large intestinal microbiota in weight regulation and insulin resistance. Mol Metab [Internet]. Elsevier GmbH 5 (2016): 759-770.
- Santos IS, Barros AJD, Matijasevich A, et al. Cohort profile update: 2004 pelotas (Brazil) birth cohort study. Body composition, mental health and genetic assessment at the 6 years follow-up. Int J Epidemiol (2014).
- World Health Organization. Obesity: prev-enting and managing the global epidemic. Report of a WHO consultation. World Health Organization technical report series (2000).
- Hyams JS, Di Lorenzo C, Saps M, et al. Childhood functional gastrointestinal disorders: Child/adolescent. Gastroenterology (2016).
- Benninga MA, Nurko S, Faure C, et al. Childhood functional gastrointestinal dis-orders: Neonate/toddler. Gastroenterology (2016).
- Mota DM, Barros AJD, Santos I, et al. Characteristics of intestinal habits in children younger than 4 years: Detecting constipation. J Pediatr Gastroenterol Nutr (2012).
- Kocaay P, Egritas O, Dalgic B. Normal defecation pattern, frequency of constipation and factors related to constipation in Turkish children 0-6 years old. Turk J Gastroenterol. Turkey 22 (2011): 369-375.
- Tam YH, Li AM, So HK, et al. Socio-environmental factors associated with constipation in Hong Kong children and Rome III criteria. J Pediatr Gastroenterol Nutr. United States 55 (2012): 56-61.
- Vernon S, Lundblad B, Hellstrom AL. Children’s experiences of school toilets present a risk to their physical and psychological health. Child Care Health Dev. England 29 (2003): 47-53.
- Magne F, Silva AP, Carvajal B, et al. The elevated rate of cesarean section and its contribution to non-communicable chronic diseases in Latin America: The growing involvement of the microbiota. Front. Pediatr (2017).
- Pesquisa Nacional de Saude 2013: Ciclos da Vida (National Health Survey 2013: Life Cycles). Rio de Janeiro: IBGE (2015).
- Kalliomäki M, Collado MC, Salminen S, et al. Early differences in fecal microbiota composition in children may predict overweight. Am J Clin Nutr (2008).
- Salminen S, Gibson GR, McCartney AL, et al. Influence of mode of delivery on gut microbiota composition in seven year old children (2004).
- Round JL, Mazmanian SK. The gut microbiota shapes intestinal immune responses during health and disease. Nat. Rev. Immunol (2009).
- Magiakou MA, Mastorakos G, Webster E, et al. The hypothalamic-pituitary-adrenal axis and the female reproductive system. Ann N Y Acad Sci (1997).
- Barros FC, Matijasevich A, Hallal PC, et al. Cesarean section and risk of obesity in childhood, adolescence, and early adulthood: Evidence from 3 Brazilian birth cohorts. Am J Clin Nutr (2012).
- Marcotte EL, Thomopoulos TP, Infante-Rivard C, et al. Caesarean delivery and risk of childhood leukaemia: A pooled analysis from the Childhood Leukemia International Consortium (CLIC). Lancet Haematol (2016).
- Goldani HAS, Bettiol H, Barbieri MA, et al. Cesarean delivery is associated with an increased risk of obesity in adulthood in a Brazilian birth cohort study. Am J Clin Nutr (2011).
- Li Y, Tian Y, Zhu W, et al. Cesarean delivery and risk of inflammatory bowel disease: A systematic review and meta-analysis. Scand J Gastroenterol (2014).