Traumatic Spondylolisthesis of the Axis without Fracture: Case Report and Literature Review
Article Information
Lívio Pereira de Macêdo1, João Batista Monte Freire1, Arlindo Ugulino Netto1, Kauê Franke1, Pierre Vansant Oliveira Eugenio1, Glaudir Donato Pinto Júnior2, Renan Furtado de Almeida Mendes2, Saul Cavalcanti de Medeiros Quirino3, Juliano Rodrigues Chaves3, Deoclides Lima Bezerra Júnior3, Geraldo de Sá Carneiro Filho4, Nivaldo S. Almeida1, Hildo Rocha Cirne Azevedo-Filho1,
1Department of Neurosurgery, Hospital da Restauração, Recife, Pernambuco, Brazil
2Centro de Ciências Médicas, Universidade Federal da Paraíba, João Pessoa, Paraíba, Brazil.
3Department of Neurosurgery - Spine Surgery, Hospital da Restauração, Recife, Pernambuco, Brazil
4Chief of Spine Section - Departament of Neurosurgery, Hospital da Restauração, Recife, Pernambuco, Brazil
*Corresponding Author: Lívio Pereira de Macêdo, Department of Neurosurgery, Hospital da Restauração, Recife, Pernambuco, Brazil.
Received: 08 September 2023; Accepted: 14 September 2023; Published: 19 September 2023
Citation: Lívio Pereira de Macêdo, MD, João Batista Monte Freire, MD, Arlindo Ugulino Netto, MD, Kauê Franke, MD, Pierre Vansant Oliveira Eugenio, MD, Glaudir Donato Pinto Júnior, MD, Renan Furtado de Almeida Mendes, MD, Saul Cavalcanti de Medeiros Quirino, MD, Juliano Rodrigues Chaves, MD, Deoclides Lima Bezerra Júnior, MD, Geraldo de Sá Carneiro Filho, MSc, Nivaldo S. Almeida, MD, Hildo Rocha Cirne Azevedo-Filho, MSc, PhD, FRCS. Traumatic Spondylolisthesis of the Axis without Fracture: Case Re- Port and Literature Review. Journal of Spine Research and Surgery. 5 (2023): 82-87.
View / Download Pdf Share at FacebookAbstract
Introduction:
Traumatic spondylolisthesis of the axis is a recurrent up-per cervical spine injury. Axis spondylolisthesis is a broader term, related to when one vertebra slips forward on another, which may in-clude fractures of other vertebral elements and even dislocations not associated with fractures.
Case Presentation:
A 26-year-old male pa-tient was admitted with a report of axial load followed by neck pain and fall from standing height. In the neurological examination, he had no motor, sensory or sphincter deficits. A cervical spine computed to-mography scan with three-dimensional reconstruction was performed, showing spondylolisthesis of C2-C3, without associated fracture, with left facet dislocation and axis lower right facet joint locked. The patient was submitted to a surgical management and he was discharged with cervical collar to ambulatorial follow-up, presenting no neurological complaints.
Discussion:
The absence of fracture in cases of traumatic spondylolisthesis between the C2 and C3 vertebrae is something that is still little reported in the literature, considering its rarity. The classification of these pictures is elementary to define the treatment. Considering the scientific records to date, the stratification proposed by AO Spine can fit the case described. However, there are few studies that discuss the conduct in these cases, probably due to its rarity.
Acknowledgements:
We report an atypical case of C2-C3 traumatic spondylolisthesis, without fracture and without neurological impairment. Due to the low occurrence of cases, the scientific discussion regarding the treatment for such cases is scarce, requiring further stud-ies on the subject.
Keywords
Upper cervical spine injury; Spinal cord injury; Spondylolisthesis of the Axis without fracture; case report
Upper cervical spine injury articles Upper cervical spine injury Research articles Upper cervical spine injury review articles Upper cervical spine injury PubMed articles Upper cervical spine injury PubMed Central articles Upper cervical spine injury 2023 articles Upper cervical spine injury 2024 articles Upper cervical spine injury Scopus articles Upper cervical spine injury impact factor journals Upper cervical spine injury Scopus journals Upper cervical spine injury PubMed journals Upper cervical spine injury medical journals Upper cervical spine injury free journals Upper cervical spine injury best journals Upper cervical spine injury top journals Upper cervical spine injury free medical journals Upper cervical spine injury famous journals Upper cervical spine injury Google Scholar indexed journals Spinal cord injury articles Spinal cord injury Research articles Spinal cord injury review articles Spinal cord injury PubMed articles Spinal cord injury PubMed Central articles Spinal cord injury 2023 articles Spinal cord injury 2024 articles Spinal cord injury Scopus articles Spinal cord injury impact factor journals Spinal cord injury Scopus journals Spinal cord injury PubMed journals Spinal cord injury medical journals Spinal cord injury free journals Spinal cord injury best journals Spinal cord injury top journals Spinal cord injury free medical journals Spinal cord injury famous journals Spinal cord injury Google Scholar indexed journals Spondylolisthesis of the Axis without fracture articles Spondylolisthesis of the Axis without fracture Research articles Spondylolisthesis of the Axis without fracture review articles Spondylolisthesis of the Axis without fracture PubMed articles Spondylolisthesis of the Axis without fracture PubMed Central articles Spondylolisthesis of the Axis without fracture 2023 articles Spondylolisthesis of the Axis without fracture 2024 articles Spondylolisthesis of the Axis without fracture Scopus articles Spondylolisthesis of the Axis without fracture impact factor journals Spondylolisthesis of the Axis without fracture Scopus journals Spondylolisthesis of the Axis without fracture PubMed journals Spondylolisthesis of the Axis without fracture medical journals Spondylolisthesis of the Axis without fracture free journals Spondylolisthesis of the Axis without fracture best journals Spondylolisthesis of the Axis without fracture top journals Spondylolisthesis of the Axis without fracture free medical journals Spondylolisthesis of the Axis without fracture famous journals Spondylolisthesis of the Axis without fracture Google Scholar indexed journals Spondylolisthesis articles Spondylolisthesis Research articles Spondylolisthesis review articles Spondylolisthesis PubMed articles Spondylolisthesis PubMed Central articles Spondylolisthesis 2023 articles Spondylolisthesis 2024 articles Spondylolisthesis Scopus articles Spondylolisthesis impact factor journals Spondylolisthesis Scopus journals Spondylolisthesis PubMed journals Spondylolisthesis medical journals Spondylolisthesis free journals Spondylolisthesis best journals Spondylolisthesis top journals Spondylolisthesis free medical journals Spondylolisthesis famous journals Spondylolisthesis Google Scholar indexed journals case report articles case report Research articles case report review articles case report PubMed articles case report PubMed Central articles case report 2023 articles case report 2024 articles case report Scopus articles case report impact factor journals case report Scopus journals case report PubMed journals case report medical journals case report free journals case report best journals case report top journals case report free medical journals case report famous journals case report Google Scholar indexed journals spinal injury articles spinal injury Research articles spinal injury review articles spinal injury PubMed articles spinal injury PubMed Central articles spinal injury 2023 articles spinal injury 2024 articles spinal injury Scopus articles spinal injury impact factor journals spinal injury Scopus journals spinal injury PubMed journals spinal injury medical journals spinal injury free journals spinal injury best journals spinal injury top journals spinal injury free medical journals spinal injury famous journals spinal injury Google Scholar indexed journals vertebral articles vertebral Research articles vertebral review articles vertebral PubMed articles vertebral PubMed Central articles vertebral 2023 articles vertebral 2024 articles vertebral Scopus articles vertebral impact factor journals vertebral Scopus journals vertebral PubMed journals vertebral medical journals vertebral free journals vertebral best journals vertebral top journals vertebral free medical journals vertebral famous journals vertebral Google Scholar indexed journals Back Pain articles Back Pain Research articles Back Pain review articles Back Pain PubMed articles Back Pain PubMed Central articles Back Pain 2023 articles Back Pain 2024 articles Back Pain Scopus articles Back Pain impact factor journals Back Pain Scopus journals Back Pain PubMed journals Back Pain medical journals Back Pain free journals Back Pain best journals Back Pain top journals Back Pain free medical journals Back Pain famous journals Back Pain Google Scholar indexed journals ligamentous injury articles ligamentous injury Research articles ligamentous injury review articles ligamentous injury PubMed articles ligamentous injury PubMed Central articles ligamentous injury 2023 articles ligamentous injury 2024 articles ligamentous injury Scopus articles ligamentous injury impact factor journals ligamentous injury Scopus journals ligamentous injury PubMed journals ligamentous injury medical journals ligamentous injury free journals ligamentous injury best journals ligamentous injury top journals ligamentous injury free medical journals ligamentous injury famous journals ligamentous injury Google Scholar indexed journals neurosurgery articles neurosurgery Research articles neurosurgery review articles neurosurgery PubMed articles neurosurgery PubMed Central articles neurosurgery 2023 articles neurosurgery 2024 articles neurosurgery Scopus articles neurosurgery impact factor journals neurosurgery Scopus journals neurosurgery PubMed journals neurosurgery medical journals neurosurgery free journals neurosurgery best journals neurosurgery top journals neurosurgery free medical journals neurosurgery famous journals neurosurgery Google Scholar indexed journals
Article Details
INTRODUCTION
In the current context, automobile accidents, falls and diving in shallow water can be cited as potential etiologies[1-9] for spinal injuries. Among such lesions, there is traumatic spondylolisthesis of the axis, an injury of significant recurrence in cervical spinal injury cases [2],[4],[5],[10-18]. This condition is often treated as a synonym for the “hangman’s fracture” - a term introduced by Schneider et al.[7] -, whose first descriptions are attributed to Wood-Jones[19], in 1913, who reported cases of hanging by judicial conviction with this traumatic repercussion of consistent feature. Nevertheless, the concept of hang- man’s fracture is specifically linked to situations of bilateral fracture in the pars interarticularis of the axis, with or without vertebral translation [1],[5-7],[14],[16],[18],[20-22]. Thus, spondylolisthesis of the axis is a broader term, related to when one vertebra slips forward on another - which can also include fractures of other vertebral elements[1],[23] and even dislocation not associated with fractures. This report presents an atypical case of traumatic spondylolisthesis of the axis, in which there was unilateral dislocation not linked to the fracture, with C2 lower right facet locked, conducted by surgical management.
CASE PRESENTATION
A 26-years-old male patient, with no comorbidities, was admitted to our emergency department with an axial load report followed by neck pain and fall from standing height. On physical examination, he showed good general condition, with hemodynamic stability, referring only a neck pain with no others complaints. In the neurological exam, he obtained the maximum score on the Glasgow Coma Scale, with photoreactive and isochoric pupils, and did not present motor, sensory or sphincter deficits, therefore being classified with ASIA Impairment Scale (AIS) Grade E and Frankel’s classification Grade E. [24-27]. In view of the clinical conditions, a cevical spine computed tomography (CT) scan and cervical spine magnetic resonance imaging (MRI) were performed, also with the aid of three-dimensional digital reconstruction of the vertebrae on CT scan. On image evaluation, C2-C3 spondylolisthesis was found, with no associated fracture, with a left facet dislocation and a locked right lower facet joint of the axis. Moreover, it was found an hyperintense signal in T2/STIR of posterior band in upper cervical, suggesting ligamentous injury and instability. (figure 1 and 2) Based on AO Spine Upper Cervical Injury Classification System, the case corresponds to a C2 and C2-3 Joint Type C, N0.
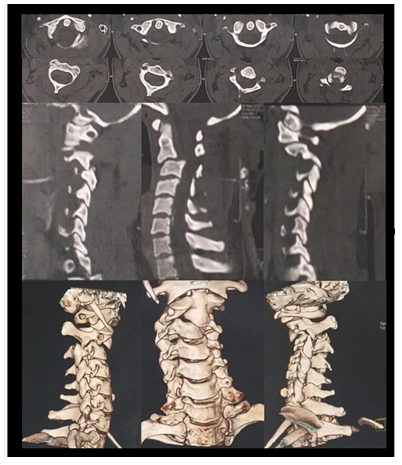
Figure 1: Cevical spine CT scan with 3D reconstruction showing a C2-C3 spondylolisthesis with no fracture associated. with a left facet dislocation and axis lower right facet joint locked.
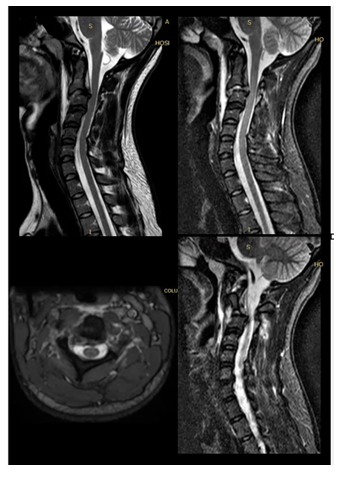
Figure 2: Cevical spine MRI showing an hyperintense signal in T2/STIR of C2-C3 posterior band, suggesting ligamentous injury.
The spine neurosurgery team led to the reduction of spondylolisthesis, initially by posterior approach, exposing the posterior elements of the skull to the third cervical vertebra and obtaining amplitude for the un-locking of the right lower facet joint by drilling. Then, we tried to complete the reduction, at first, using a manual maneuver, stabilizing C2 and C3 with the use of a steel wire, tying the spinous processes of the vertebrae. With the failure of the first attempt, C1-C3 posterior arthrodesis was performed, using lateral mass screws fixation technique. (figures 3 and 4) On the postoperative control image, it was observed that spondylolisthesis had not been completely reduced. Therefore, four days after the first surgery, a second surgical procedure was performed, using an anterior approach. In this procedure, a C2-C3 discectomy with bone graft and interbody fusion (ACDF) was performed (figure 5), obtaining a 360 degree cervical fusion. [31]
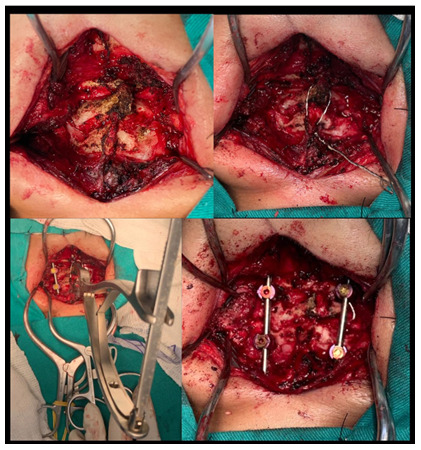
Figure 3: Upper Left: Intraoperative view, posterior approach, exposing posterior elements of the skull to the third cervical vertebra and obtaining amplitude for the unlocking of the right lower facet joint by drilling. Then, we tried to complete the reduction, at first, using a manual maneuver, stabilizing C2 and C3 with the use of a steel wire, tying the spinous processes of the vertebrae. With the failure of the first attempt, C1-C3 posterior arthrodesis was performed, using lateral mass screws fixation technique.
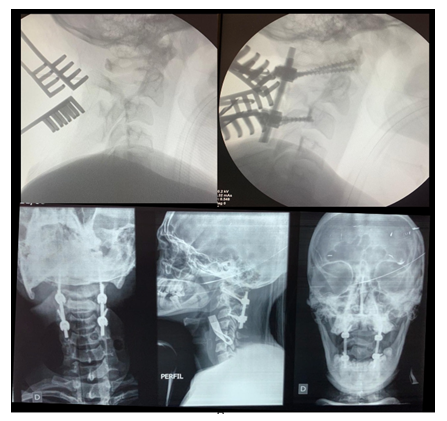
Figure 4: Upper Left: Pre-operative fluoroscopy image showing C2-C3 spondylolisthesis. Upper Right: Intraoperative fluoroscopy after C1-C3 posterior arthrodesis, Lower Left and Lower right: Post-operative X-ray showing C1-C3 posterior arthrodesis, showing that spondylolisthesis had not been completely reduced.
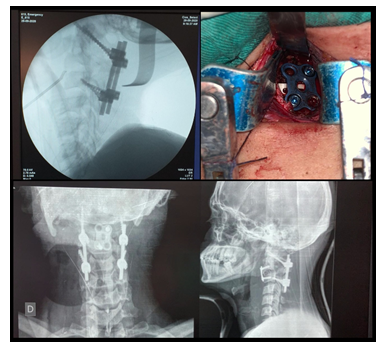
Figure 5: Upper Left: On the second surgical procedure, pre-operative fluoroscopy image showing the level. confirmation Upper Right: C2-C3 ACDF Intraoperative view.
After this intervention, it was possible to conclude the reduction and the stability of the cervical spine. The patient was discharged with cervical collar to ambulatorial follow-up, presenting no neurological complaints (figure 6).
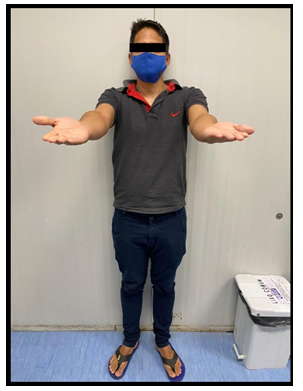
Figure 6: The patient on ambulatorial follow-up with no neurological complaints.
Discussion
The term spondylolisthesis refers to the slipping/dislocation of one vertebral body over the other (from the Greek spondylos, which means vertebra, and listhisis, which refers to slip). Usually, when it occurs due to a traumatic cause, it has been established as a synonym of "hangman's fracture", a cervical lesion in which there is a fracture of the pars interarticularis [1],[5-7],[14],[16],[18],[20-22], whose name known that the major cause of traumatic cervical injury is related to traffic accidents, corresponding alludes to the damages observed in hanging victims [19]. Nonetheless, despite this expression, it is to about 39.5 to 55% of cases28. Other frequent etiologies include shallow water dives and falls [1-9].
The absence of fracture in cases of traumatic spondylolisthesis between C2 and C3 vertebrae is still poorly reported in the literature, considering its rarity. In a retrospective study of 258 patients with high cervical spine trauma, Fujimura et al. reported only 3 cases of C2-C3 dislocation without fracture, which represents approximately 1% of cases [29]. Moreover, among cervical spine traumas, about 50% occur between C5 and C7, which reinforces the lower frequency of upper cervical spine injuries.
Considering the anatomical site, it is expected that patients with upper cervical injuries presents severe neurological deficits, given the proximity of important neural structures. However, the absence of clinical neurological signs can be explained by the greater diameter of the vertebral canal above C3 in comparison to the diameter of the spinal cord, which decreases the chance of compressive myelopathy. In this context, patients who survive to a upper cervical injury tend to course without neurological deficits [1],[5],[18],[29].
Imaging exams are essential in order to delimit the topography and severity of cervical injuries in an adequate therapeutic planning. Ra-diography and CT scan should be done to evaluate bone integrity and the presence of fractures, besides examining the alignment and position of bone structures, in search of displaced facets joints, for example [4],[18],[32]. The mandatory use of magnetic resonance imaging (MRI) is questionable28. Although a good analysis of the discoligament complex can be made from his images, Hart et al. concluded that, for unilateral facet displacement, awake and cooperative patients can have their treatment safely initiated even without MRI [33].
The classification of the injury is elementary for the management. In this framework, AO Spine proposed a method for stratification of patients with high cervical trauma, based on the lesional topography, type of injury, neurological status and modifiers. Considering the scientific records up to now, the AO Spine Upper Cervical Injury Classification System is the only capable of framing the case reported. Moreover, there are few studies that discuss the conduct for such cases, most probably due to their rarity.
Given the lack of studies that guide the conduct specifically for the reported case, it was necessary to evaluate the treatment panorama for similar conditions. In cases of hanging fractures, the classification proposed by Effendi [10] and modified by Levine-Edwards [2] defines the conduct. For this, the mechanism of trauma and the morphological characteristics of the injury are considered. In most cases, conservative treatment is the recommended choice, since they tend to be stable lesions with no neurological impairment, due to spinal canal enlargement and preservation of ligaments [1]. However, in cases of facetary dislocation, an important posterior ligament injury is assumed, which makes the condition significantly unstable and, therefore, fits it as type III, the most severe. Then, surgical management with open reduction and C2-C3 or C1-C3 arthrodesis via posterior access is recommended [34].
Regarding for the definition of management in subaxial injury cases, a classification usefull is the Subaxial Cervical Spine Injury Classification (SLIC), in which morphological characteristics, the state of the discoligamentary complex and the neurological state are considered. In this context, patients with unilateral or bilateral facetary displacement add enough points to be classified as cervical lesions of greater instability, even without neurological impairment, and are therefore candidates for surgery [36].
Acknowledgement
In summary, we reported a case, notably atypical, of traumatic C2-C3 spondylolisthesis, without fracture and neurological impairment. The use of the term "hangman’s fracture" as a synonym for traumatic spondylolisthesis of the axis is imprecise, and, therefore, may cause confusion when treating patients with the described condition. In our center, we have decided on a surgical management for the instability correction. However, due to the low incidence of cases, current discussion regarding the management for such cases is still scarce, requiring new future studies on this subject.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, author- ship, and/or publication of this article.
References
- Ferro FP, Borgo GD, Letaif OB, et al. Traumatic spondylo- listhesis of the axis: Epidemiology, management and outcome. Acta Ortop Bras 20 (2012): 84-87.
- Levine AM, Edwards CC. The management of traumatic spon-dylolisthesis of the axis. J Bone Jt Surg - Ser A 67 (1985): 217-226.
- Machinis TG, Fountas KN, Kapsalaki EZ, et al. A rare case of com- plete C2-C3 dislocation with mild neurological symptoms. Eur Spine J 15 (2006): 585-589.
- Shimamura Y, Kaneko K. Irreducible traumatic spondylolisthesis of the axis: Case report and review of the literature. Injury 39 (2008): 371-374.
- Al-Mahfoudh R, Beagrie C, Woolley E, et al. Management of Typical and Atypical Hang- man’s Fractures. Published online 6 (2016).
- Coric D, Wilson JA, Kelly DL. Treatment of traumatic spondy-lolisthesis of the axis with nonrigid immobilization: A review of 64 cases. J Neurosurg. Published online 85 (1996): 550-554.
- SCHNEIDER RC, LIVINGSTON KE, CAVE AJ, HAMILTON G. “HANGMAN’S FRACTURE” OF THE CERVICAL SPINE. J Neurosurg. Published online 14 (1965): 198-208.
- White AA, Panjabi MM. The clinical biomechanics of the occip-itoatlantoaxial complex. Orthop Clin North Am. Published online 9 (1978): 867-878.
- Li XF, Dai LY, Lu H, et al. A systematic review of the management of hangman’s Eur Spine J 15 (2006): 257-269.
- Effendi B, Roy D, Cornish B, et al. Fractures of the ring of the axis. A classification based on the analysis of 131 cases. J Bone Jt Surg - Ser B. Published online 63 (1981): 319-327.
- Starr JK, Eismont FJ. Atypical hangman’s fractures. Spine (Phila Pa 1976). Published online 18 (1993): 1954-1957.
- Ge C, Hao D, He B, et al. Anterior cervical discectomy and fusion versus posterior fixation and fusion of C2-3 for unstable hangman’s fracture. J Spinal Disord Tech 28 (2015): E61-13-E66.
- Gehweiler JA, Clark WM, Schaaf RE, et al. Cervical spine trauma: The common combined conditions. Ra-diology. Published online 130 (1979).
- Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: Analysis of management and outcome in 340 consecutive cases. Spine (Phila Pa 1976). Published online 22 (1997): 1843-1852.
- Hadley MN, Dickman CA, Browner CM, et al. Acute axis fractures: A review of 229 cases. J Neurosurg. Published online 71 (1989): 642-647.
- Murphy H, Schroeder GD, Shi WJ, et al. Management of Hangman’s Fractures: A Systematic J Orthop Trauma 31 (2017):S90-S95.
- Hadley MN, Browner C, Sonntag VKH. Axis fractures: A com-prehensive review of management and treatment in 107 cases. Neurosurgery. Published online 17 (1985): 281-290.
- Choi WG, Vishteh AG, Baskin JJ, et al. Completely dislocated hangman’s fracture with a locked C2-3 facet: Case report. J Neurosurg 87 (1997): 757-760.
- Wood-Jones F. THE IDEAL LESION PRODUCED BY JUDI-CIAL HANGING. Lancet. Published online (1913).
- Samaha C, Lazennec JY, Laporte C, et al. Hangman’s frac-ture: The relationship between asymmetry and instability. J Bone Jt Surg Ser B. Published online 82 (2000): 1046-1052.
- Bakhsheshian J, Sizdahkhani S, Ohiorhenuan I, et al. Transpedicular lag screw placement in traumatic cervical spondylolisthesis: Case report and systematic review of the literature. J Clin Neurosci 63 (2019): 256-262.
- Patel J, Kundnani V, Kuriya S, et al. Unstable Hangman’s fracture: Anterior or posterior surgery? J Craniover-tebr Junction Spine 10 (2019): 210-215.
- Karthigeyan M, Rangan V, Salunke P. A case of traumatic C2-3 listhesis without pars fracture: Insights from this possible variant of hangman’s fracture. Neurol India 65(2017):209-209. Accessed October 30, 2020.
- Ditunno JF, Young W, Donovan WH, et al. The interna-tional standards booklet for neurological and functional classifi-cation of spinal cord injury. Paraplegia. Published online 32 (1994): 70-80.
- Maynard FM, Bracken MB, Creasey G, et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord. Published online 35 (1997): 266-274.
- Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial man- agement of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. Published online 7 (1969): 179-192.
- Kirshblum SC, Burns SP, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury (revised 2011). J Spinal Cord Med 34 (2011): 535-546.
- Del Curto D, Tamaoki MJ, Martins DE, et al. Surgical approaches for cer- vical spine facet dislocations in adults. Cochrane Database Syst Rev 2 (2014).
- Fujimura Y, Nishi Y, Chiba K, et al. Prognosis of neurological deficits associated with upper cervical spine injuries. Paraplegia 33 (1995): 195-202.
- Joaquim AF, Lawrence B, Daubs M, et al. Eval-uation of the subaxial injury classification system. J Craniover-tebr Junction Spine 2 (2011): 67-72.
- WHOLEY MH, BRUWER AJ, BAKER HL. The lateral roent-genogram of the neck; with comments on the atlanto-odontoid-basion relationship. Radiology 71 (1958): 350-356.
- Munakomi S, M Das J. Cervical Subluxation. StatPearls Publishing. Accessed (2020).
- Hart RA, Vaccaro AR, Nachwalter RS. Cervical facet disloca-tion: When is magnetic resonance imaging indicated? Spine (Phila Pa 1976), 27 (2002): 116-118.
- Divi SN, Schroeder GD, Oner FC, et al. AOSpine—Spine Trauma Classification System: The Value of Modifiers: A Nar-rative Review With Commentary on Evolving Descriptive Principles. Glob Spine J 9 (2019): 77S-88S.
- Ryang YM. Upper cervical spine trauma. Spine Surg A Case-Based Approach. Published online (2019): 253-267.
- de la Rua Julio R, Claudio CG, Tomás VP. The surgical approach to subaxial cervical spine injuries: an evidence-based algorithm based on the SLIC classification system. Spine (Phila Pa 1976), 33 (2008): 2620-2629.
