Thoracic Aortic Mural Thrombus, an Unusual Source of Peripheral Thromboembolism: A Report of two cases
Article Information
Michalis Gionis1*, Vasiliki Manaki1, Georgia Kaiafa2, Elisavet Psoma3, Christos Savvopoulos2, Kiriakos Ktenidis1
1Department of Vascular Surgery, AHEPA University Hospital, Thessaloniki, Greece
2First Propedeutic Department of Internal Medicine, AHEPA University Hospital, Thessaloniki, Greece
3Department of Clinical Radiology, AHEPA University Hospital, Thessaloniki, Greece
*Corresponding Author: Michalis Gionis, Department of Vascular Surgery, AHEPA University Hospital, Thessaloniki, Greece
Received: 23 November 2022; Accepted: 05 December 2022; Published: 12 January 2023
Citation: Michalis Gionis, Vasiliki Manaki, Georgia Kaiafa, Elisavet Psoma, Christos Savopoulos, Kiriakos Ktenidis. Thoracic Aortic Mural Thrombus, an Unusual Source of Peripheral Thromboembolism: A Report of two cases. Journal of Surgery and Research 6 (2023): 04-09.
View / Download Pdf Share at FacebookAbstract
Background: Mural aortic thrombus with absence of aneurysmatic or atherosclerotic lesion is a rare finding which usually leads to peripheral embolization and visceral damage. Due to a lack of specific guidelines, the optimal therapeutic treatment remains a controversial topic in the literature.
Case Reports: 1st Case: A 79-year-old man presented with thromboembolism to the left kidney, pancreas, spleen, left popliteal and anterior tibial artery from a 5 cm long thrombus of the descending aorta. He was treated conservatively with therapeutic doses of low molecular weight heparin,antiplatelets and iloprost and continued his treatment at home with therapeutic doses of rivaroxaban and cilostazol. Three and six months later during his follow-up there was a significant regression of the thrombus in the patient’s imaging examination, while his clinical condition was ameliorated.He deceased nine months later after being diagnosed with a brain tumor. 2nd Case: A 70-year-old man presented with mural thrombus of the thoracic aorta, pulmonary thromboembolism, splenic and pancreatic infarcts. He received conservative treatment with therapeutic doses of low molecular weight heparin and antiplatelets.He was transferred in the Cardiologic ICU of our Hospital where his clinical condition was ameliorated.
Conclusion: Thoracic aortic thrombosis in a normal non-atherosclerotic aorta is a rare condition that may present with peripheral thromboembolism. An underlying cause should be identified in all cases, as the condition may indicate a hypercoagulable state associated with underlying malignancy. Conservative treatment can offer good therapeutic outcomes in cases where endovascular repair is not suitable.
Keywords
<p>Thromboembolism, Thrombus, Atherosclerosis, Aortic disease, Hypercoagulability</p>
Thromboembolism articles; Thrombus articles; Atherosclerosis articles; Aortic disease articles; Hypercoagulability articles
Thromboembolism articles Thromboembolism Research articles Thromboembolism review articles Thromboembolism PubMed articles Thromboembolism PubMed Central articles Thromboembolism 2023 articles Thromboembolism 2024 articles Thromboembolism Scopus articles Thromboembolism impact factor journals Thromboembolism Scopus journals Thromboembolism PubMed journals Thromboembolism medical journals Thromboembolism free journals Thromboembolism best journals Thromboembolism top journals Thromboembolism free medical journals Thromboembolism famous journals Thromboembolism Google Scholar indexed journals Thrombus articles Thrombus Research articles Thrombus review articles Thrombus PubMed articles Thrombus PubMed Central articles Thrombus 2023 articles Thrombus 2024 articles Thrombus Scopus articles Thrombus impact factor journals Thrombus Scopus journals Thrombus PubMed journals Thrombus medical journals Thrombus free journals Thrombus best journals Thrombus top journals Thrombus free medical journals Thrombus famous journals Thrombus Google Scholar indexed journals Atherosclerosis articles Atherosclerosis Research articles Atherosclerosis review articles Atherosclerosis PubMed articles Atherosclerosis PubMed Central articles Atherosclerosis 2023 articles Atherosclerosis 2024 articles Atherosclerosis Scopus articles Atherosclerosis impact factor journals Atherosclerosis Scopus journals Atherosclerosis PubMed journals Atherosclerosis medical journals Atherosclerosis free journals Atherosclerosis best journals Atherosclerosis top journals Atherosclerosis free medical journals Atherosclerosis famous journals Atherosclerosis Google Scholar indexed journals Aortic disease articles Aortic disease Research articles Aortic disease review articles Aortic disease PubMed articles Aortic disease PubMed Central articles Aortic disease 2023 articles Aortic disease 2024 articles Aortic disease Scopus articles Aortic disease impact factor journals Aortic disease Scopus journals Aortic disease PubMed journals Aortic disease medical journals Aortic disease free journals Aortic disease best journals Aortic disease top journals Aortic disease free medical journals Aortic disease famous journals Aortic disease Google Scholar indexed journals Hypercoagulability articles Hypercoagulability Research articles Hypercoagulability review articles Hypercoagulability PubMed articles Hypercoagulability PubMed Central articles Hypercoagulability 2023 articles Hypercoagulability 2024 articles Hypercoagulability Scopus articles Hypercoagulability impact factor journals Hypercoagulability Scopus journals Hypercoagulability PubMed journals Hypercoagulability medical journals Hypercoagulability free journals Hypercoagulability best journals Hypercoagulability top journals Hypercoagulability free medical journals Hypercoagulability famous journals Hypercoagulability Google Scholar indexed journals Thoracic aortic thrombosis articles Thoracic aortic thrombosis Research articles Thoracic aortic thrombosis review articles Thoracic aortic thrombosis PubMed articles Thoracic aortic thrombosis PubMed Central articles Thoracic aortic thrombosis 2023 articles Thoracic aortic thrombosis 2024 articles Thoracic aortic thrombosis Scopus articles Thoracic aortic thrombosis impact factor journals Thoracic aortic thrombosis Scopus journals Thoracic aortic thrombosis PubMed journals Thoracic aortic thrombosis medical journals Thoracic aortic thrombosis free journals Thoracic aortic thrombosis best journals Thoracic aortic thrombosis top journals Thoracic aortic thrombosis free medical journals Thoracic aortic thrombosis famous journals Thoracic aortic thrombosis Google Scholar indexed journals antiplatelets articles antiplatelets Research articles antiplatelets review articles antiplatelets PubMed articles antiplatelets PubMed Central articles antiplatelets 2023 articles antiplatelets 2024 articles antiplatelets Scopus articles antiplatelets impact factor journals antiplatelets Scopus journals antiplatelets PubMed journals antiplatelets medical journals antiplatelets free journals antiplatelets best journals antiplatelets top journals antiplatelets free medical journals antiplatelets famous journals antiplatelets Google Scholar indexed journals visceral damage articles visceral damage Research articles visceral damage review articles visceral damage PubMed articles visceral damage PubMed Central articles visceral damage 2023 articles visceral damage 2024 articles visceral damage Scopus articles visceral damage impact factor journals visceral damage Scopus journals visceral damage PubMed journals visceral damage medical journals visceral damage free journals visceral damage best journals visceral damage top journals visceral damage free medical journals visceral damage famous journals visceral damage Google Scholar indexed journals
Article Details
Introduction
Thoracic aortic mural thrombus (TAMT) in an aorta, without aneurysmalor atherosclerotic occlusive lesion, is a rare pathologic disorder [1]. Regarding to pathogenesis, several risk factors have been described in the literature including smoking, hypercoagulability due to malignancy or coagulation disorders, use of steroids, connective tissue disorders and vasculitis expressing with endothelial damage, and iatrogenic causes [1]. Descending aorta is the commonest site of aortic mural thrombi and although rare, represents a potential source of non-cardiogenic peripheral embolization, with challenging diagnosis and high morbidity in case of acute limb ischemia and organ infarction [1]. The differential diagnosis should also include aortic endoluminalmalignancy [2]. Most patients initially present with symptoms of acute peripheral embolization or visceral dysfunction. However, there are also extremely rare cases in which the aortic thrombus is discovered accidentally [1,3,4]. Due to the small number of reported cases in the literature, optimal treatment remains a major challenge1. Therapeutic strategies vary from conservative treatment with anticoagulation to open repair or endovascular treatment (TEVAR) [1,3]. This report is of two cases of thrombus in the normal descending thoracic aorta from a vascular center in Greece.
Case Reports
Case 1
A 79-year-old man, smoker, presented with thromboembolism to the left kidney, pancreas, spleen, left popliteal and anterior tibial artery from a 5 cm long thrombus of the descending aorta. He presented with abdominal pain, nausea and vomiting, edemas, and renal dysfunction with oliguria. Laboratory results revealed hyperkalemia (K: 6.1 mmol/l), metabolic acidosis, anemia,haematuria, amylase levelsat 2.658 U/dl and blood lipase at 264 U/dl. Renal function biomarkers were also elevated with Urea at 384 mg/dL and Creatinineat 8.6 mg/dL. The patient was first treated conservatively with poor success regarding hyperkalemia,and urgently underwent hemodialysis, while at the same time a gastroenterologist consultation took place. Imaging exams included MRCP and Computed Tomography Angiogramof thorax andabdomen with the last ones revealing a big mural thrombus (5cm x 1cm) of the descending aorta with absence of atherosclerotic plaques or aneurysmal lesion (figure 1). Further findings included signs of acute pancreatitisbecause of large pancreatic infarction, as well as multiple renal and spleen infarctions, but no signs of malignant tumors were detected (figures 2,3). MRCP showed no signs of malignancy, or biliary tractcholelithiasis. The 24-hour Holter monitoring was negative to cardiac atrial fibrillation.No further investigation of thrombophilia and malignancy took placeas the patient was older than 70 geras old and due to absence of malignancy in thorax and abdomen imaging exams.pANCA, cANCA markers were also negative. The patient was admitted to the Internal Medicine Department because of multiple organ failure and received adequate conservative treatment. Additionally to aortic mural thrombus and according to his anamnesis, the patient claimed of left limb severe claudication with symptoms initiation three months before hospital admission, and an urgently Vascular Surgeon’s consultation requested. Despite clinical examination findings regarding to left limb (pailness, popliteal and tibial pulselessness, and coldness of the left limb when confronted to contralateral), the patient did not suffer a limb-threatening condition, probably because of his acute-on-chronic ischemia. Patient’s comorbidities and current clinical status did not establish open repair of the descending aorta as an inviting therapeutic option, while TEVAR procedure with insertion of stiff guidewires and aortic endograft deployment inside a pulsing descending aorta with a large, long and unstable mural thrombus, raised serious concerns about massive and hazardous life-threatening peripheral embolization.Previous experience of our Department regarding a thoracic aortic mural thrombus case which ended in massive and hazardous peripheral embolization during TEVAR because of a large descending aorta symptomatic thrombus, led us to proceed with conservative treatment of the patient.The therapeutic schema included high doses of Low Molecular Weight Heparin (tinzaparin 14.000 IU), antiplatelets (aspirin 100mg x 1) and Iloprost (12 ml/h).Duration of Iloprost administration was twenty-one days, after which it was substituted with cilostazol 100mg x 2. Tinzaparin was bridged to therapeutic doses of Rivaroxaban (20 mg x1) after the 21th day, and the schema was completed with the permanence of the antiplatelet agent (aspirin 100 mg x 1). The patient was dismissed in the 25th day of hospitalization in good clinical condition. There was a regression of his visceral pathology clinically as well as regarding to laboratory markers (Urea: 60 mg/dl, Creatinine: 1.43 mg/dl, SGOT: 21 U/I, SGPT: 22 U/I, WBC: 5.55 K/μL). Diuresis was improved and hemodialysis was not required any more. Regarding his left limb acute-on-chronic ischemia, the patient had presence of pulses in his left femoral and popliteal artery, absence of clinical signs and symptoms of acute or severe chronic limb ischemia, and an ankle-brachial index of the left limb equal to 0, 7, with no more claudication. Follow-up in three (Figure 4) and six months (Figure 5) revealed further signs of improvement regarding his aortic pathology, with almost complete recanalization of the descending aorta, significant regression of visceral and renal infarcts and patency of left femoro-popliteal arterial tract. Nevertheless, eight months after his first hospitalization and while still in his triple therapeutic schema, the patient was readmitted to the Neurological Department of our hospital because of equilibrium disorders and diagnosed of a brain tumor and the patient’s hypercoagulable state and aortic thrombus was attributed to malignancy. He was deceased one month later.
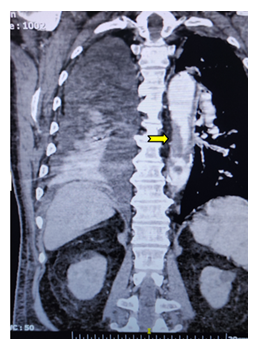
Figure 1: Descending aortal mural thrombus depiction via Computed Tomography
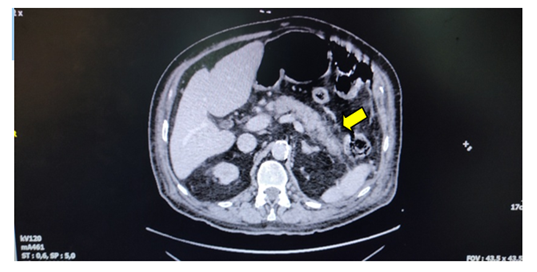
Figure 2: Pancreatic margins changes indicating of acute pancreatitis

Figure 3: Splenic infarction due to peripheral embolization
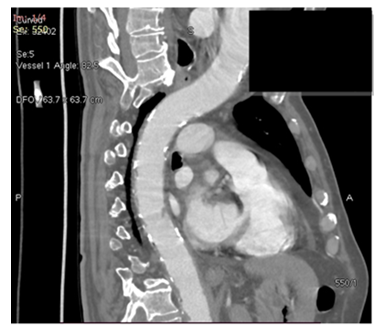
Figure 4: Three months follow-up. Total regression of aortic mural thrombus
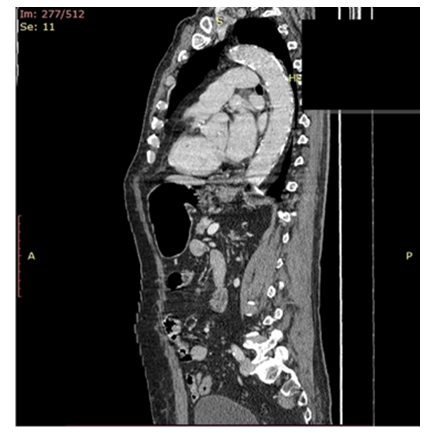
Figure 5: Six months follow-up. Total regression of aortic mural thrombus, no recurrence.
Case 2
A 70 years old male with an anamnesis of smoking, hypertension, and type II diabetes mellitus but no intermittent claudication, presented to Emergency Department of our hospital, with chest and abdominal pain, Transit Ischemic Attack, and dyspnea. Urgent imaging test with Computed Tomography Angiogram revealed an all along the Thoracic Aorta Mural Thrombus (figure 6), Pulmonary Embolism of both lungs, splenic and pancreatic infarcts and a tumor of the right lung (figures 7- 9). He was admitted to the Cardiology ICU, where Vascular Surgeons performed a clinical examination and consultation. The presence of palpable pulses were detected in all levels of clinical examination (neck, arms and limbs), and the patient was free of symptoms and signs of acute or chronic peripheral arterial occlusive disease. Despite imaging signs, no symptoms of abdominal pathology were present and his clinical condition was good. pANCA, cANCA markers were also negative. Further investigation for thrombophilia was not performed due to patient’s age and hypercoagulability was attributed to malignancy. The patient received conservative medical treatment with therapeutic doses of low molecular weight heparin and antiplatelets (aspirin 100 mgx1), after Neurologic consultation and since there were no haemorrhagic signs in Imaging control with CT of the cerebrum parenchyma. Further investigation tests are still to be performed regarding the malignancy findings of the right lung, as well as findings regarding pancreatic parenchyma and duct. Three days after his admission in the Coronary ICU, the patient was ameliorated, with complete regression of dyspnea, chest and abdominal pain, and symptoms free regarding neurological, abdominal and peripheral arterial occlusive disease. The patient was also dismissed symptoms free. During his one and three month follow-up there was total regression of the thrombus.
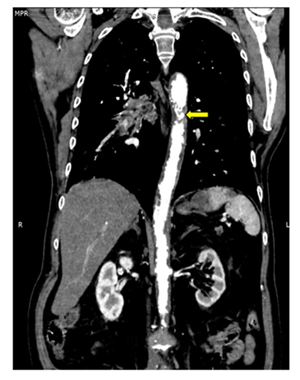
Figure 6: Thoracic aortic mural thrombus, depiction via Computed Tomography
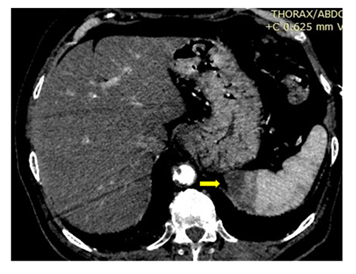
Figure 7: Splenic and Pancreatic lesions due to peripheral embolization
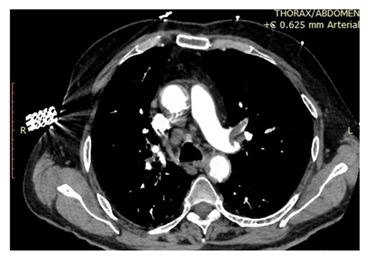
Figure 8: Thoracic Aorta Mural Thrombus and Pulmonary Embolism in both lungs
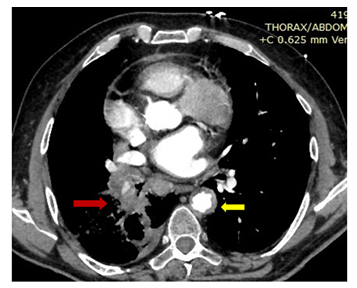
Figure 9: Thoracic aorta mural thrombus, massive pneumonic embolism in both lungs and lung cancer (yellow arrow: aorta, red arrow: lung cancer)
Discussion
Due to a lack of specific guidelines, the optimal therapeutic treatment for aortic floating mural thrombus remains a controversial topic in the literature [1-4]. Therapeutic options vary between open or endovascular aortic repair to conservative therapy [2]. The afore-mentioned cases offer the opportunity to discuss the advantages of conservative treatment over other therapeutic strategies especially in patients with other comorbidities and not good clinical condition. In the last decade, detection of thrombus in the thoracic aorta is more often and easily achieved thanks to the use of advanced imaging methods during investigation of thromboembolic sources [2,4]. In most centers, patients with peripheral embolism receive a 24-hourHolter monitoring, TEE (transesophangeal echocardiogram), CTangiogram, or MRAngiogram of the thoraco-abdominal aorta, and arterial duplex ultrasonography of the vessels proximal to the embolic occlusion as part of the routine procedure during the hospital permanence [2,4]. Due to the small number of reported cases and the absence of clear recommendations [1], the appropriate treatment is widely contested, and many options have been recommended. In their studies, Dougherty et al. and Hausmann et al. both suggest catheter-guided thrombolysis as a therapy for thoracic aortic mural thrombus [5,6] .This therapy, however, has been shown to have a risk of lysing pedunculated lesions, releasing the majority of the thrombus and causing significant embolization [1].
Other studies suggest conservative treatment as a very efficient and safe option. More specifically, when anticoagulant treatment is administered promptly, can lead even to complete thrombus resolution and prevention of recurrent embolization [2,7]. In the literature, there are studies that present complete resolution of the thrombus after anticoagulant treatment with unfractioned heparin or therapeutic doses of low molecular weight heparin and later warfarin alone, resulting in low rates of recurrent peripheral embolization [7]. Duration of the anticoagulant therapy is also controversial. Some patients were treated with anticoagulants until thrombus resolution, while others received lifelong treatment. Since there are no publications in the literature to guide about these issues, regarding either thoracic aortic mural thrombus or in general arterial thrombotic events, the ideal optimal duration and dosage of anticoagulant treatment of thoracic aortic mural thrombus remains unknown [7]. Endovascular repair is an effective therapy for thoracic aortic mural thrombus, characterized by minimally invasive, low risk procedure [2,4]. Criado et al. described the first TEVAR operation with TEE use in 2004, demonstrating the superiority of the endovascular method and the importance of TEE during stent graft implantation [8]. Endovascular treatment of thoracic aortic mural thrombus has been documented in the literature more frequently in this late era [1]. Technically, the thrombus should be completely entrapped between the stent-graft and the aortic wall, and the graft must extend at least 2 cm proximally and 2 cm distally from the thrombus's longitudinal extensionwitha 5-10% stent-graft oversizing [1]. However, there is always risk of distal embolism during guide-wire insertion and stent deployment, which could be discouraging for this approach [9]. This type of treatment may be efficient in recurrent episodes of peripheral embolization from a floating mural thrombus. Furthermore, as Narh-Martey et al mentioned, the ability to use a single incision for both procedures makes endovascular stent grafts attractive during simultaneous thrombectomy of the lower extremities and thoracic aortic mural thrombus repair [10]. Open repair is usually the last option in the management of such cases when conservative and endovascular strategies have failed as well as in case of endoluminal malignancy of the aortic wall. In this case, local resection of the tumor is required [1]. Unlike heart thrombi or other peripheral thrombi that occur due to atherosclerosis, aortic mural thrombus due to the absence of atherosclerotic lesion is a totally different clinical entity with different management and different more complex causes.
In our two recent cases, conservative treatment was the best option due to the patients’ comorbidities and general clinical condition, in combination to the risk of peripheral embolization during stent-graft implantation. It is worth-mentioning that in both cases, pANCA, cANCA markers were negative; patients were older than 70 years old so thrombophilia tests were not investigated. In the first case malignancy was not diagnosed but nine months later as the imaging examinations (thorax and abdomen) that had been at first performed were negative for tumors. In the second case, malignancy was detected promptly, since initial imaging investigation revealed the lung tumor. In both cases, the hypercoagulable state could was attributed to malignancy.
Similar cases have also been reported in the literature [11,12]. In the cases of Habib et al. and Khine et al. patients were managed conservatively with anticoagulant and antiplatelet therapy and during their follow-ups there was full regression of the aortic thrombi.
Conclusions
Thoracic aortic thrombosis in a normal non-atherosclerotic aorta is a rare condition that may present with peripheral thromboembolism. An underlying cause should be identified in all cases, as the condition may indicate a hypercoagulable state associated with underlying malignancy. Anticoagulation treatment remains the primal empirical option since there are no precise guidelines regarding therapeutic strategy. Moreover, it is related with low risk of complications and it is suitable for complex patients with multiple comorbidities, resulting to good final outcomes.
References
- Tsilimparis N, Hanack U, Pisimisis G, et al. Thrombus in the non-aneurysmal, non-atherosclerotic descending thoracic aorta--an unusual source of arterial embolism. Eur J Vasc Endovasc Surg 41 (2011): 450-457.
- Goedemé J, Berzenji L, Nicolay S, et al. Conservative Treatment of a Floating Mural Thrombus in the Descending Aorta. Aorta 9 (2021): 38-40.
- Meyermann K, Trani J, Caputo FJ, et al. Descending thoracic aortic mural thrombus presentation and treatment strategies. J Vasc Surg 66 (2017): 931-936.
- Yang S, Yu J, Zeng W, et al. Aortic floating thrombus detected by computed tomography angiography incidentally: Five cases and a literature review. J Thorac Cardiovasc Surg 153 (2017): 791-803.
- Dougherty MJ, Calligaro KD, Rua I, et al. Idiopathic pedunculated mural thrombus of the nonaneurysmal infrarenal aorta presenting with popliteal embolization: two cases treated with thrombolytic therapy. J Vasc Surg 32 (2000): 383-387.
- Hausmann D, Gulba D, Bargheer K, et al. Successful thrombolysis of an aortic-arch thrombus in a patient after mesenteric embolism. N Engl J Med 327 (1992): 500-501.
- Bowdish ME, Weaver FA, Liebman HA, et al. Anticoagulation is an effective treatment for aortic mural thrombi. J Vasc Surg 36 (2002): 713-719.
- Criado E, Wall P, Lucas P, et al. Transesophageal echo-guided endovascular exclusion of thoracic aortic mobile thrombi. J Vasc Surg 39 (2004): 238-242.
- Filippone G, Barbera GL, Palermo C, et al. Endovascular Repair of Primary Thoracic Aortic Mural Thrombus Following Upper Limb Embolization. Braz J Cardiovasc Surg 36 (2021): 829-833.
- Narh MP, Szuchmacher M, Cicchillo M, et al. Thoracic endovascular aortic repair for thoracic aortic mobile thrombus. J Surg Case Rep 12 (2012): 1767.
- Khine K, Toor A, Khalighi K, et al. Incidental descending thoracic aortic thrombus: the conundrum of medical versus surgical therapy. J Community Hosp Intern Med Perspect 9 (2019): 491-494.
- Habib H, Hsu J, Winchell PJ, et al. Mural thrombus in the normal-appearing descending thoracic aorta of a chronic smoker. Tex Heart Inst J 40 (2013): 619-622.
