Therapeutic Approach with PCSK9 Inhibitors for Effective Cardiovascular Risk Reduction in Diabetes
Article Information
Francisco Arrieta1, Pedro Iglesias2, Manuel Aguilar3, Pedro Mata4, Juan Pedro-Botet5*
1Department of Endocrinology and Nutrition, Hospital Universitario Ramón y Cajal, Madrid, Spain
2Department of Endocrinology and Nutrition, Hospital Universitario Puerta de Hierro. Madrid, Spain
3Department of Endocrinology and Nutrition, Hospital Universitario Puerta del Mar, Department of Medicine, Universidad de Cádiz, Cádiz, Spain
4Fundación Hipercolesterolemia Familiar, Madrid, Spain
5Lipid and Vascular Risk Unit, Hospital del Mar; Department of Medicine, Universitat Autònoma de Barcelona, Barcelona, Spain
*Corresponding Authors: Dr. Pedro-Botet J, Hospital del Mar. Passeig Marítim, 25-29. 08003 Barcelona, Spain
Received: 04 November 2020; Accepted: 16 November 2020; Published: 03 December 2020
Citation: Francisco Arrieta, Pedro Iglesias, Manuel Aguilar, Pedro Mata, Juan Pedro-Botet. Therapeutic Approach with PCSK9 Inhibitors for Effective Cardiovascular Risk Reduction in Diabetes. Cardiology and Cardiovascular Medicine 4 (2020): 736-742.
View / Download Pdf Share at FacebookKeywords
Cardiovascular prevention; Diabetes mellitus; Hypercholesterolaemia; Lipid-lowering drugs; Low-density lipoprotein cholesterol; PCSK9 inhibitors
Article Details
Introduction
Type 2 diabetes mellitus (T2DM) is a recognised risk factor for cardiovascular disease, being the main cause of death in this specific population. As the direct and indirect healthcare burden attributable to T2DM is notably increasing, patients with diabetes will represent a growing percentage of the population with established cardiovascular disease. Hypercholesterolaemia is a causal factor for the development and progression of atherosclerotic vascular injury [1, 2]; consequently, the awareness of lipid profile is crucial in subjects with diabetes, especially T2DM, both at the time of diagnosis and in the clinical follow-up, in order to achieve therapeutic goals with greater precision [1, 3]. Furthermore, delay in the management of hypercholesterolaemia is associated with a rise in vascular risk and a high recurrence of cardiovascular events, a fact that undoubtedly entails unacceptable health and social costs [1, 4]. Therefore, it is paramount to optimise the use of pharmacological therapies with proven efficacy in reducing cardiovascular risk in patients with diabetes.
Currently-available lipid-lowering drugs such as statins, ezetimibe and proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitors enable us a priori to achieve strict therapeutic objectives regarding low-density lipoprotein cholesterol (LDL-C) [5]. Different studies and meta-analyses have shown the beneficial effects of an additional reduction in LDL-C levels when statins are combined with ezetimibe or PCSK9 inhibitors, thus confirming the greater reduction in LDL-C concentration and the greater efficacy in cardiovascular prevention [6, 7].
The recommendations of the Cardiovascular Risk Group of the Spanish Diabetes Society (SED) 2018 [8], the European Society of Cardiology (ESC)/European Atherosclerosis Society (EAS) 2019 [9], the American College of Cardiology (ACC)/American Heart Association (AHA) in primary prevention of cardiovascular disease 2019 [10] and the most recent from the American Diabetes Association (ADA, 2020) [11] and the Endocrine Society 2020 [12] highlight the need to reduce cardiovascular risk in T2DM with proper use of the available therapeutic strategies. The therapeutic goals for the diabetic population according to risk category, time since diagnosis and type of diabetes are shown in Table 1 [9]. Very recently, in the DA VINCI study [13], an 18-European country, cross-sectional, observational study among patients receiving lipid-lowering therapies, fewer than half of high/very high-risk primary and secondary prevention patients achieved 2016 ESC/EAS LDL-C goals, with approximately one-fifth achieving the lower 2019 ESC/EAS goals. Therefore, in the real world, a huge gap exists between the achieved and recommended LDL-C goals by the guidelines for patients at the highest risk.
Since 2015, with the approval of the Food and Drug Administration (FDA) and the European Medicines Agency (EMA), the pharmacological armamentarium for the treatment of dyslipidaemia has been expanded with two monoclonal antibodies against PCSK9. These new lipid-lowering agents, with considerable clinical evidence of their cardiovascular benefits, provide significant reductions in LDL-C, specifically in patients with high vascular risk who do not achieve the recommended goals despite modifications in lifestyle and statin treatment in monotherapy at the maximum tolerated dose or in combination with ezetimibe, as well as in those with intolerance or contraindication for the use of statins but who have a high risk of cardiovascular events [14-19].
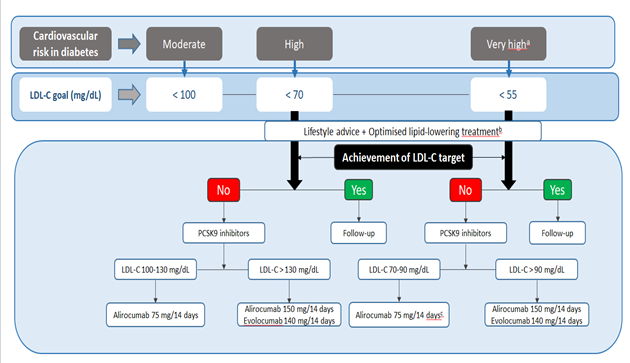
The present report emitted by the Cardiovascular Risk Group of the Spanish Diabetes Society (SED) and the Familial Hypercholesterolemia Foundation (FHF), aimed to facilitate the achievement of therapeutic objectives in LDL-C in the T2DM population through the rational use of lipid-lowering drugs, including PCSK9 inhibitors, evolocumab and alirocumab (Figure 1).
|
Cardiovascular risk categories |
Clinical features |
LDL-C goal |
Non HDL-C goal |
Apo B goal |
|||
|
TODa |
CVRF |
Time since DM diagnosis |
% reduction |
Level (mg/dL) |
Level (mg/dL) |
Level (mg/dL) |
|
|
Very high |
Yes |
≥ 3 |
Individualise T1DM T2DM > 20 years |
> 50 |
< 55 |
< 85 |
< 65 |
|
High |
No |
1-2 |
Individualise T1DM T2DM 10-20 years |
> 50 |
< 70 |
< 100 |
< 80 |
|
Moderate |
No |
0 |
T1DM < 35 years old T2DM < 40 years old and/or duration < 10 years |
30-50 |
< 100 |
< 130 |
< 100 |
Apo, apolipoprotein; CVRF cardiovascular risk factors; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; TOD, target organ damage; CVRF: age, sex, family history, hypertension, smoking, hypercholesterolaemia, overweight/obesity (particularly abdominal obesity) and sedentary lifestyle; *Adapted from the ESC/EAS 2019 guideline [9]. No subject with diabetes is at low cardiovascular risk; aTOD is defined as microalbuminuria, retinopathy or neuropathy
Table 1: Stratification of cardiovascular risk and therapeutic objectives in the population with diabetes*.
Figure 1: Algorithm of therapeutic approach with PCSK9 inhibitors in diabetic patients for effective cardiovascular risk reduction; aCardiovascular risk category and therapeutic objective not considered in the current therapeutic report of the Spanish Association of Medicines and Health Products; bOptimised lipid-lowering treatment leads to a reduction in LDL-C ≥ 50%, either with statin monotherapy or associated with ezetimibe, with adherence of 80%; cThe option to use full starting doses of either of the two PCSK9 inhibitors may also be valid.
First of all, it should be noted that the attainment of LDL-C targets in patients with diabetes must be individualised, and the proposed therapeutic approach algorithm therefore differs from that of other scientific societies [18]. Second, it is important to take into account that according to recent updated reports on the therapeutic positioning of evolocumab and alirocumab in hypercholesterolaemia of the Spanish Agency for Medicines and Health Products (AEMPS) [20, 21], funding of these drugs is limited to patients with familial hypercholesterolaemia and/or established cardiovascular disease (ischaemic heart disease, ischaemic cerebrovascular disease and peripheral arterial disease) with LDL-C > 100 mg/dL despite the maximum tolerated doses of statins. Thus, to obviate the consequences of adding ezetimibe in patients with diabetes treated with statins for of LDL-C concentrations varying between 100 and 130 mg/dL for those at high/very high risk that would imply the non-indication of PCSK9 inhibitors despite not having achieved the respective therapeutic objectives, we selected the term “optimised lipid-lowering treatment”, coined by the Spanish Arteriosclerosis Society (SEA) [22] and defined as one with a relative reduction ≥ 50% in LDL-C with adherence of 80%. In this respect, the difference in the additional reduction in LDL-C compared to baseline with a statin at the maximum tolerated dose or in combination with ezetimibe ranges from 50% to 60%. Therefore, we propose that all high/very high risk patients requiring a > 20% reduction in LDL-C despite receiving the maximum tolerated dose of statin should be additionally treated with a PCSK9 inhibitor. Similarly, since there are two PCSK9 inhibitors with a high LDL-C reduction effect, their choice must also be tailored based on baseline LDL-C and the possibility of dose titration (Figure 1). However, the possibility of using full starting doses with either of the two PCSK9 inhibitors may also be reasonable, particularly in T2DM patients at very high cardiovascular risk.
On the other hand, we must stress two facts: the European guidelines recommend LDL-C < 55 mg/dL with a relative reduction > 50% compared to baseline as a therapeutic goal in patients with very high cardiovascular risk, and very low LDL-C levels can be achieved with the use of PCSK9 inhibitors in combination with statins. Although there does not appear to be a lower limit for plasma LDL-C beyond which no benefits are obtained [23], the lack of long-term safety studies suggests applying appropriate clinical judgement and considering the patient's choice when achieving concentrations of LDL-C < 30 mg/dL [17, 23-26]. Furthermore, in a recent subanalysis of the Odyssey Outcomes trial [27] using a propensity score matching, relative and absolute reductions in major cardiovascular events with alirocumab were similar in patients who achieved LDL-C 25-50 or < 25 mg/dL. These findings do not indicate a clear advantage of targeting LDL-C levels below 25 mg/dL.
In short, it would be desirable to re-review the report by the AEMPS on the therapeutic position of PCSK9 inhibitors and individualise the indications in patients with diabetes at high/very high cardiovascular risk in accordance with the latest clinical practice guidelines. In this respect, the present statement includes, in the therapeutic approach algorithm (Figure 1), a new vascular risk situation not previously contemplated by the AEMPS. The proposed algorithm is simple in design, easy to carry out and eminently practical when the different clinical scenarios of cardiovascular risk in the diabetic population are considered.
Acknowledgements
We thank Miss Christine O’Hara for review of the English version of the manuscript.
Conflicts of Interest
The authors Arrieta, Iglesias, Aguilar, Mata and Pedro-Botet have no conflict of interest regarding the publication of this article.
References
- Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 38 (2017): 2459-2472.
- Borén J, Chapman MJ, Krauss RM, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease: pathophysiological, genetic, and therapeutic insights: a consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J 41 (2020): 2313-2330.
- Boekholdt SM, Hovingh GK, Mora S, et al. Very low levels of atherogenic lipoproteins and the risk for cardiovascular events: a meta-analysis of statin trials. J Am Coll Cardiol 64 (2014): 485-494.
- Pérez de Isla L, Arroyo-Olivares R, Alonso R, et al. Incidence of cardiovascular events and changes in the estimated risk and treatment of familial hypercholesterolemia: the SAFEHEART registry. Rev Esp Cardiol (Engl. Ed) 73 (2020): 828-834.
- Masana L, Ibarretxe D, Plana N. Maximum low-density lipoprotein cholesterol lowering capacity achievable with drug combinations. When 50 plus 20 equals 60. Rev Esp Cardiol (Engl Ed) 69 (2016): 342-343.
- Maki KC, Ridker PM, Brown WV, et al. An assessment by the Statin Diabetes Safety Task Force: 2014 update. J Clin Lipidol 8 (2014): 17-29.
- Murphy SA, Cannon CP, Blazing MA, et al. Reduction in total cardiovascular events with ezetimibe/simvastatin post-acute coronary syndrome: the IMPROVE-IT Trial. J Am Coll Cardiol 67 (2016): 353-361.
- Arrieta F, Iglesias P, Pedro-Botet J, et al. Diabetes mellitus y riesgo cardiovascular: actualización de las recomendaciones del grupo de trabajo de Diabetes y Enfermedades Cardiovasculares de la Sociedad Española de Diabetes (SED, 2018). Clin Investig Arterioscler 30 (2018): 137-153.
- Mach F, Baigent C, Catapano AL, et al; ESC Scientific Document Group. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J 41 (2020): 111-188.
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 140 (2019): 596-646.
- Standards of medical care in diabetes 2020. Diabetes Care 43 (2020): 1-206.
- Newman CB, Blaha MJ, Boord JB, et al. Lipid Management in Patients with Endocrine Disorders: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab 105 (2020): 674.
- Ray KK, Molemans B, Marieke Schoonen W, et al. EU-Wide Cross-Sectional Observational Study of Lipid-Modifying Therapy Use in Secondary and Primary Care: the DAVINCI study. Eur J Prevent Cardiol (2020).
- Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med 376 (2017): 1713-1722.
- Robinson JG, Nedergaard BS, Rogers WJ, et al. Effect of evolocumab or ezetimibe added to moderate- or high-intensity statin therapy on LDL-C lowering in patients with hypercholesterolemia: the LAPLACE-2 randomized clinical trial. JAMA 311 (2014): 1870-1882.
- Scherer N. Alternative treatment regimens with the PCSK9 inhibitors alirocumab and evolocumab: a pharmacokinetic and pharmacodynamic modeling approach. J Clin Pharmacol 57 (2017): 846-854.
- Steg PG, Szarek M, Bhatt DL, et al. Effect of alirocumab on mortality after acute coronary syndromes. Circulation 140 (2019): 103-112.
- Escobar C, Anguita M, Arrarte V, et al. Recommendations to improve lipid control. Consensus document of the Spanish Society of Cardiology. Rev Esp Cardiol (Engl Ed) 73 (2020): 161-167.
- Schwartz GG, Steg PG, Szarek M, et al. ODYSSEY OUTCOMES Committees and Investigators (2018). Alirocumab and Cardiovascular Outcomes after Acute Coronary Syndrome. N Engl J Med 379 (2018): 2097-2107.
- Informe de Posicionamiento Terapéutico de Evolocumab (Repatha®) en hipercolesterolemia. IPT, 12/2020. V2 (2020).
- Informe de Posicionamiento Terapéutico de Alirocumab (Praluent®) en hipercolesterolemia. IPT, 13/2020. V2 (2020).
- Ascaso JF, Civeira F, Guijarro C, et al. Indicaciones de los inhibidores de PCSK9 en la práctica clínica. Recomendaciones de la Sociedad Española de Arteriosclerosis (SEA), 2019. Clin Investig Arterioscler 31 (2019): 128-139.
- Masana L, Girona J, Ibarretxe D, et al. Clinical and pathophysiological evidence supporting the safety of extremely low LDL levels-The zero-LDL hypothesis. J Clin Lipidol 12 (2018): 292-299.
- Dobrzynski JM, Kostis JB, Sargsyan D, et al. Effect of cholesterol lowering with statins or proprotein convertase subtilisin/kexin type 9 antibodies on cataracts: a meta-analysis. J Clin Lipidol 12 (2018): 728-733.
- Ma C, Gurol ME, Huang Z, et al. Low-density lipoprotein cholesterol and risk of intracerebral hemorrhage: a prospective study. Neurology 93 (2019): 445-457.
- Schmidt AF, Carter JL, Pearce LS, et al. PCSK9 monoclonal antibodies for the primary and secondary prevention of cardiovascular disease. Cochrane Database Syst Rev 10 (2020): CD011748.
- Schwartz GG, Szarek M, Bhatt DL, et al. LDL-C < 50 mg/dL (< 1.3 mmol/L) is an appropriate target after acute coronary syndrome: a propensity score-matched analysis of the ODYSSEY OUTCOMES trial. Presented at the European Society of Cardiology Congress. The Digital Experience (2020).