Therapeutic and Diagnostic Challenge of Idiopathic Granulomatous Mastitis: A Case Report and Review of the Literature
Article Information
Alpha Boubacar Conte*, Solène Nyingone, Sofia Jayi, Hadiza Moutari Soule, Fatima Zohra Fdili Alaoui, Hikmat Chaara, Moulay Abdelilah Melhouf
Department of Gynecology - Obstetrics II, Sidi Mohamed Ben Abdellah University, Hassan II Teaching Hospital Fez, Fez, Morocco
*Corresponding author: Alpha Boubacar Conte, Department of Gynecology - Obstetrics II, Sidi Mohamed Ben Abdellah University, Hassan II Teaching Hospital Fez, Fez, Morocco
Received: 19 June 2020; Accepted: 10 July 2020; Published: 16 July 2020
Citation:
Alpha Boubacar Conte, Solène Nyingone, Sofia Jayi, Hadiza Moutari Soule, Fatima Zohra Fdili Alaoui, Hikmat Chaara, Moulay Abdelilah Melhouf. Therapeutic and Diagnostic Challenge of Idiopathic Granulomatous Mastitis: A Case Report and Review of the Literature. Journal of Women’s Health and Development 3 (2020): 158-166.
View / Download Pdf Share at FacebookAbstract
Idiopathic Granulomatous mastitis (IGM) is a chronic benign inflammatory disease of the breast that may mimic breast cancer. It is most common in parous young fertile women, although it can occur in nulliparous. It affects mostly women of childbearing age with a history of breastfeeding. IGM is an idiopathic disease due to the influence of some environmental factors in genetically predisposed subjects. Several pathogenic hypothesis have been proposed in the last years (autoimmune, hormonal, infective genesis). Because the clinical presentation can mimic infectious mastitis or inflammatory carcinoma, the disease course is often protracted. The diagnosis is made by histopathology. Ultrasound, mammography, and magnetic resonance imaging are not specific; however, ultrasound and mammography should be done to exclude other pathologies. There is no universal treatment of GM. We report in this manuscript one case of IGM through which we mention a therapeutic and diagnostic challenge with a brief review of the literature. The management was successful despite the long way made by the patient before she acceded to a proper treatment.
Keywords
Granulomatous mastitis; Therapeutic; Diagnostic; Challenge
Granulomatous mastitis articles Granulomatous mastitis Research articles Granulomatous mastitis review articles Granulomatous mastitis PubMed articles Granulomatous mastitis PubMed Central articles Granulomatous mastitis 2023 articles Granulomatous mastitis 2024 articles Granulomatous mastitis Scopus articles Granulomatous mastitis impact factor journals Granulomatous mastitis Scopus journals Granulomatous mastitis PubMed journals Granulomatous mastitis medical journals Granulomatous mastitis free journals Granulomatous mastitis best journals Granulomatous mastitis top journals Granulomatous mastitis free medical journals Granulomatous mastitis famous journals Granulomatous mastitis Google Scholar indexed journals Therapeutic articles Therapeutic Research articles Therapeutic review articles Therapeutic PubMed articles Therapeutic PubMed Central articles Therapeutic 2023 articles Therapeutic 2024 articles Therapeutic Scopus articles Therapeutic impact factor journals Therapeutic Scopus journals Therapeutic PubMed journals Therapeutic medical journals Therapeutic free journals Therapeutic best journals Therapeutic top journals Therapeutic free medical journals Therapeutic famous journals Therapeutic Google Scholar indexed journals Diagnostic articles Diagnostic Research articles Diagnostic review articles Diagnostic PubMed articles Diagnostic PubMed Central articles Diagnostic 2023 articles Diagnostic 2024 articles Diagnostic Scopus articles Diagnostic impact factor journals Diagnostic Scopus journals Diagnostic PubMed journals Diagnostic medical journals Diagnostic free journals Diagnostic best journals Diagnostic top journals Diagnostic free medical journals Diagnostic famous journals Diagnostic Google Scholar indexed journals Challenge articles Challenge Research articles Challenge review articles Challenge PubMed articles Challenge PubMed Central articles Challenge 2023 articles Challenge 2024 articles Challenge Scopus articles Challenge impact factor journals Challenge Scopus journals Challenge PubMed journals Challenge medical journals Challenge free journals Challenge best journals Challenge top journals Challenge free medical journals Challenge famous journals Challenge Google Scholar indexed journals inflammatory articles inflammatory Research articles inflammatory review articles inflammatory PubMed articles inflammatory PubMed Central articles inflammatory 2023 articles inflammatory 2024 articles inflammatory Scopus articles inflammatory impact factor journals inflammatory Scopus journals inflammatory PubMed journals inflammatory medical journals inflammatory free journals inflammatory best journals inflammatory top journals inflammatory free medical journals inflammatory famous journals inflammatory Google Scholar indexed journals breast articles breast Research articles breast review articles breast PubMed articles breast PubMed Central articles breast 2023 articles breast 2024 articles breast Scopus articles breast impact factor journals breast Scopus journals breast PubMed journals breast medical journals breast free journals breast best journals breast top journals breast free medical journals breast famous journals breast Google Scholar indexed journals radiographically articles radiographically Research articles radiographically review articles radiographically PubMed articles radiographically PubMed Central articles radiographically 2023 articles radiographically 2024 articles radiographically Scopus articles radiographically impact factor journals radiographically Scopus journals radiographically PubMed journals radiographically medical journals radiographically free journals radiographically best journals radiographically top journals radiographically free medical journals radiographically famous journals radiographically Google Scholar indexed journals antibiotic articles antibiotic Research articles antibiotic review articles antibiotic PubMed articles antibiotic PubMed Central articles antibiotic 2023 articles antibiotic 2024 articles antibiotic Scopus articles antibiotic impact factor journals antibiotic Scopus journals antibiotic PubMed journals antibiotic medical journals antibiotic free journals antibiotic best journals antibiotic top journals antibiotic free medical journals antibiotic famous journals antibiotic Google Scholar indexed journals ultrasound articles ultrasound Research articles ultrasound review articles ultrasound PubMed articles ultrasound PubMed Central articles ultrasound 2023 articles ultrasound 2024 articles ultrasound Scopus articles ultrasound impact factor journals ultrasound Scopus journals ultrasound PubMed journals ultrasound medical journals ultrasound free journals ultrasound best journals ultrasound top journals ultrasound free medical journals ultrasound famous journals ultrasound Google Scholar indexed journals cystic articles cystic Research articles cystic review articles cystic PubMed articles cystic PubMed Central articles cystic 2023 articles cystic 2024 articles cystic Scopus articles cystic impact factor journals cystic Scopus journals cystic PubMed journals cystic medical journals cystic free journals cystic best journals cystic top journals cystic free medical journals cystic famous journals cystic Google Scholar indexed journals
Article Details
1. Introduction
Granulomatous mastitis is a rare, benign inflammatory breast disease of unknown etiology, mainly affecting women of childbearing age. Although it presents with features of an abscess, it can be mistaken for breast cancer [1]. The importance of recognizing this disease is because its presentation can clinically and radiographically mimic breast cancer [2], leading to a diagnostic challenge, as well as anxiety during the evaluation [3]. The diagnosis of granulomatous mastitis (GM) is often established after excluding inflammatory breast cancer, autoimmune breast disease and other etiologies such as tuberculosis, fungal or parasitic breast infections. A definitive diagnosis requires a histopathological confirmation of multinucleated giant cell granulomas with micro abscesses [4]. It is thought to be caused by either infectious agents or foreign material, which triggers the immune response system, leading to granuloma formation. Some of the known inflammatory etiologies of GM are tuberculosis (most common, caused by Mycobacterium tuberculosis), sarcoidosis, fungal infection, and autoimmune disease, such as Granulomatosis with Polyangiitis and giant cell arteritis. These entities are clinically, pathologically, and radiographically indistinguishable from idiopathic granulomatous mastitis (IGM) [5]. Different treatment modalities have been reported, with varying success and recurrence rates, but no consensus currently exists as to the ideal treatment regimen [6]. We report through this case our experience in term of clinical, biological and pathological finding and management.
2. Case Report
30-year-old patient who consulted for a hardening of the right breast evolving for two years. Pauciparous with no particular history and no notion of oral contraception. History of the disease: The beginning was marked by the occurrence of a hardening of the right breast in the post-partum during breastfeeding with collection of fluid fistulized to the skin having motivated several consultations in different tertiary structures during which fluid drainages were carried out after realization of breast ultrasound showing multiple lesions classified ACR2 with treatment based on antibiotic and local care without success for a period of one year. In view of the persistence of the symptoms, another breast ultrasound was performed and came in favor of solido cystic tissue lesions of the upper internal quadrant and the external quadrant classified ACR4b. Following this result, ultrasound guided biopsies were proposed. During the biopsy, the sonographer describes fluid collections with no visible tissue. Samples of fluid were taken and the results was in favor of an absence of germs with a negative culture. As the treatment was not successful, she decided to seek for care in our department. At her arrival in our department, the examination found an apyretic patient with asymmetrical breasts; left breast without particularity and right breast having a bumpy appearance seat of several scars of fistulization without inflammatory signs (Figure 1). On palpation, we noted in the inner upper quadrant the presence of a hard, irregular, painless and mobile mass compared to the 2 planes measuring 4 / 3cm and in the outter upper quadrant another hard, irregular, painless and mobile mass compared to 2 planes measuring 10 / 8cm with retraction of the mammal without pressure flow. The axillary areas were free. The rest of the clinical examination was unremarkable.
We decided to repeat a mammography coupled with an ultrasound. The mammography found the presence of 04 opacities interesting the different quadrants of the right breast of variable size and tone, well limited measuring for the largest 5 cm of long axis, absence of suspected micro calcification focus, respect for subcutaneous fatty tissue with a fine and regular skin line (Figure 2 ). The ultrasound breast exploration shows the presence of 04 interesting collections respectively the upper outer quadrant, upper internal and junctions of the upper and inner quadrants. Well limited with heterogeneous thick content with cystic masses of the internal upper quadrant without tissue lesion with free axillary areas. All in favor of liquid collections of the upper quadrants of the right breast with a cystic cluster classified ACR3. A biopsy was thus carried out. The study of the biopsy carrots found a mammary parenchyma seat of an epithelioid and gigantocellular granulomatous reaction joined to a polymorphic inflammatory infiltrate made of lymphocyte grouped in place in lymphoid follicles, of plasma cells and neutrophils in favor of mastitis epithelioid and gigantic-cell granulomatous without caseous necrosis and without tumor lesions. Etiological assessments were made: a normal face pulmonary X-ray, search for BK by PCR and in sputum were negative, ANCA, C3 and C4 without particularity, kidney function (urea, creatine and proteinuria of 24h) normal HIV and Syphilis serologies were also negatives. We concluded to an idiopathic granulomatous mastitis. Patient benefit of medical treatment based on oral corticosteroid for 6 weeks and oral antibiotics (clavulanic amoxicillin: 1g per 8h for 14 days and metronidazole 500mg per 8h for 10 days). The corticosteroid posology was as followed prednisolone 20mg: 60 mg per day for 15 days, after 40 mg per day for 15 days followed by 20 mg per day for 15 other days. The patient was monitored every 15 days by breast clinical examination. At the end of the treatment, she had a good clinical response.
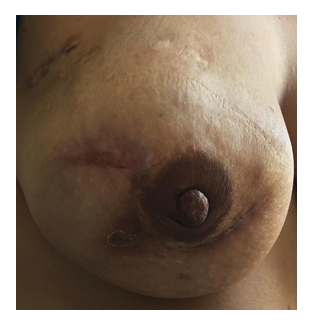
Figure 1: Right breast bumpy appearance seat of several scars of fistulization without inflammatory signs.

Figure 2: Opacities of the breast at the mammography.
3. Discussion
Idiopathic granulomatous mastitis (IGM) is a benign chronic inflammatory condition of the breast of unknown etiology and characterized by the presence of noncaseating granulomas with micro-abscess formation confined to the breast lobule [7, 8]. The etiology of IGM remains elusive with most cases labeled ‘idiopathic’ and having no identifiable causative factor. Several mechanistic theories have been proposed including an autoimmune reaction to extravasated protein secretions from mammary ducts secondary to trauma, infection or chemical irritation, elevated prolactin levels and use of the oral contraceptive pill (OCP) [2, 9]. The common lesion would be an attack on the ductal epithelium causing extravasation glandular secretions in the connective tissue of the lobule responsible for granulomatous inflammatory lesions [10, 11]. According to some authors, IGM is almost always seen in women of childbearing age. The findings in multiple studies [12, 13] indicate that IGM is almost always seen in women of childbearing age. The patient of our study was in childbearing age. The symptomatology of the patient started two months after the onset of the breastfeeding. A strong association between IGM and history of pregnancy and lactation is reported, with most patients reporting having a pregnancy within 5 years before the diagnosis [14-16] or being diagnosed with IGM within 2 months to 20 years after a pregnancy [17]. Clinical presentation of IGM is most commonly as a firm, ill-defined mass in the upper outer quadrant of the breast The mass is usually unilateral and can occur in any quadrant of the breast but is more frequent in the aforementioned and subareolar regions [18]. The mass is tender and may be associated with erythema of the overlying skin, peau d’orange and indrawing of the nipple. More advanced cases may present with ulcerated areas and sinus tracts or fistulae [19]. Our patient reported episode of fistulas and ulcerations of the breasts skins before she came to us for proper management. The mass may clinically mimic a bacterial abscess and/or breast cancer by inducing skin or nipple retraction. Lymphadenopathy is present in up to 15% of patients [20].Synchronous bilateral breast findings is also reported in some studies [12, 21, 22], isolated skin induration is reported to be as less common clinical manifestations [12]. Its been reported by Wilson and al. that some patients have extramammary signs and symptoms, while others have disease confined to the breast(s). IGM patients could develop repeated abscesses over weeks to months. These findings may be confused with breast abscess or malignancy [23]. Our case was treated repeatedly for recurrent breast abscesses. Based on our experience, it’s likely to be that there’s no specific signs at the imagery neither the mammography and neither the ultrasound nor the MRI could give proper idea for the diagnosis of IGM. Although it can mimic breast cancer, there is no pathognomonic sign for GM on US, mammography, and MRI [1]. Irregular tubular hypoechoic lesions, lobulated hypoechoic masses, parenchymal irregularities without a mass, fistulization to skin or axillary lymphadenopathies, could be recognized on US. Typically, US examination demonstrates a solid mass, often with one or more abscesses. According to Yildiz S and al. [16] multiple irregular hypoechoic masses and collections with tubular connections with fingerlike aspects and skin fistulae in patients with breastfeeding history, suggests IGM rather than carcinoma. In all the two cases of our observations, ultrasound described the aspect in favor of several collections. A focal asymmetric opacity, enhancement of density, diffuse enhancement of fibroglandular mass density, an irregular mass, ellipsoid mass, retraction and heterogeneity of breast parenchyma, could be identified on mammography [1]. The mammographic features of GM have also been reported as normal or as an ill?defined mass suspicious of carcinoma [24]. However the mammography could have the unique interest of eliminating some malignancies aspects. Its also to be noted that mammography’s interpretation is more difficult in young women, whose breasts are dense. MRI can be complementary to US and mammography, showing an irregular mass with parenchymal distortion, but it is not possible to differentiate GM from breast carcinoma based on this MRI finding [25]. These imaging modalities should be used initially in the workup of GM. Microcaclifications suspicious of malignancy, architectural distortion or intraductal mass should warrant appropriate histological diagnosis and subsequent management. [26, 27]. In front of any suspicion of masses inside the breast or suspicion of abscesses, it’s mandatory to lead investigation so that to have a proof of malignancies, or infections or any other etiology of the symptoms presented by the patient. In the search of diagnosis it’s important to note that liquids from our patient breast was removed for etiologic purpose and the samples were sterile and free from any presence of bacteria. Biopsy of tissue components was done and the diagnosis of GM was obtained. GM is diagnosed by histopathology only. The disease is characterized by the formation of a non-necrotizing granuloma in combination with a localized infiltrate of multi-nucleated giant cells, epithelioid histiocytes, lymphocytes, and plasma cells. Sometimes, organized sterile micro-abscesses occur with neutrophilic infiltrates. Inflammation that extends into adjacent lobules can indicate a higher severity. The involved parenchyma mostly shows loss of acinar structures and damaged ducts [28, 29]. The histological describe a mammary parenchyma site of a granulomatous epithelioid and giganto-cellular reaction associated with a polymorphic infiltrate made of lymphocytes grouped by place in lymphoid follicles of plasma cells and neutrophils describing a granulomatous epithelioid and giganto-cellular mastitis without caseous necrosis and absence of tumor lesion. The differential diagnosis of MGI arises clinically with carcinomatous mastitis and mastitis, infectious or not (lipophagic granuloma, cysteoadenonecrosis, sarcoidosis, Wegener's disease, etc.). Histological examination helps differentiate these pathologies [30]. The etiological and immunological assessment includes the C3, C4, C50, anti-nuclear antibody, anti-DNA, antistreptolysin dosage and syphilitic serology. This balance was negative in our patient [31]. In our habit we add to those exams the research of BK in sputum and by PCR, HIV serology, front chest x-ray, evaluation of renal function by urea, creatine and proteinuria of 24h. All these examinations were negative in our patient. There is a general lack of consensus and clarity in the treatment of GM [32]. Our patient benefited first initially from pus drainage as required by the clinical picture followed by antibiotic therapy based on amoxi plus clavulanic acide and metronidazol. This treatment was unsuccessful due to the fact that the patients kept the same clinical pictures. The same attitude is made by some authors due to the fact that the clinical presentation of the disease is typical for mastitis, most patients get antibiotics in the beginning of their therapy cascade in the form of a blind antibiotic therapy without any microbiological proof of a bacterial infection. GM is per definition a sterile inflammatory disease; therefore, antibiotic therapy usually fails [32, 33]. Which lets us say that we should not be relentless on a treatment of recurrent abscess of the breast whose bacteriological sample is negative without thinking of doing a biopsy to have a diagnosis and start an adequate treatment. However, the main therapeutic approaches include surgery, steroids, immunosuppressant drugs or a combination of two or more modalities [34, 35]. It also include conservative measures such as close regular surveillance [11]. Up to half of cases may develop a chronic course and surgical intervention should be employed judiciously as complications from surgery can be worse than the primary lesion [23, 36]. Some authors recommend a corticosteroid regimen of 30 mg prednisolone twice a day for 2 weeks, tapering gradually based on clinical findings. Every-2-week visits should take place to evaluate treatment response and possible side effects. Corticosteroids should be administered for a minimum of 8 weeks and a maximum of 6 months to minimize possible side effects [37]. Methotrexate is a treatment option for patients who have relapsed or who do not tolerate high-dose corticosteroid therapy. A low-dose regimen similar to those recommended for patients suffering from chronic rheumatoid diseases: 7.5–25 mg methotrexate as a weekly dose combined with folic acid applied daily or once a week [38].
4. Conclusion
This case is a learning lesson about the challenge with the diagnosis and the management of IGM and it illustrates that this entity is not well known by the clinicians and the radiologist.
Conflicts of Interest
None
Contribution of the Authors
All the authors participated to the management of the patient and the writing of the manuscript.
References
- Korkut E, Akcay MN, Karadeniz E, Subasi ID, Gursan N. Granulomatous mastitis: a ten?year experience at a university hospital. Eurasian J Med 47 (2015): 165?173.
- Kessler E, Wolloch Y. Granulomatous mastitis: a lesion clinically simulating carcinoma. Am J Clin Pathol 58 (1972): 642-646.
- Barreto DS, Sedgwick EL, Nagi CS, Benveniste AP. Granulomatous mastitis: etiology, imaging, pathology, treatment, and clinical findings. Breast Cancer Research and Treatment 171 (2018): 527-534
- Schelfout K, Tjalma WA, Cooremans ID, Coeman DC, Colpaert CG, Buytaert PM. Observations of an idiopathic granulomatous mastitis, Eur J Obstet Gynecol Reprod Biol 97 (2001): 260-262.
- Bakaris S, Yuksel M, Ciragil P, Guven MA, Ezberci F, Bulbuloglu E. Granulomatous mastitis including breast tuberculosis and idiopathic lobular granulomatous mastitis. Can J Surg 49 (2006): 427?430.
- Alrayes A, Almarzooq R, Abdulla HA. Surgical treatment of granulomatous mastitis: Our experience in Bahrain. Breast J (2019): 1-5.
- Gurleyik G, Aktekin A, Aker F, Saglamc A. Medical and surgical treatment of idiopathic granulomatous lobular mastitis: a benign inflammatory disease mimicking invasive carcinoma. J. Breast Cancer 15 (2012): 119-123.
- Baslaim MM, Khayat HA, Al-Amoudi SA. Idiopathic granulomatous mastitis: a heterogeneous disease with variable clinical presentation. World J. Surg 31 (2007): 1677-1681.
- Bani-Hani KE, Yaghan RJ, Matalka II, Shatnawi NJ. Idiopathic granulomatous mastitis: time to avoid unnecessary mastectomies. Breast J 10 (2004): 318-322.
- Lee JH, Oh KK, Kim EK, Kwack KS, Jung WH. Radiologic and clinical of idiopathic granulomatous lobular mastitis mimicking advanced breast cancer. Yonsei Med J 28 (2006): 431-415.
- Lai EC, Chan WC, Ma TK, Tang AP, Poon CS. The role of conservative treatment in idiopathic granulomatous mastitis. Breast J 11 (2005): 454-456.
- Manouchehr Aghajanzadeh, Rasool Hassanzadeh, Soheila Alizadeh Sefat, Ali Alavi, Hossein Hemmati, Mohammad Sadegh Esmaeili Delshad, et al. Granulomatous mastitis: presentations, diagnosis, treatment and outcome in 206 patients from the north of Iran. Breast 24 (2015): 456-460.
- Oztekin PS, Durhan G, Nercis Kosar P, Erel S, Hucumenoglu S. Imaging findings in patients with granulomatous mastitis. Iran J Radiol 13 (2016): e33900.
- Al-Khaffaf B, Knox F, Bundred NJ. Idiopathic granulomatous mastitis: a 25-year experience. J Am Coll Surg 206 (2008): 269-273.
- Al-Khawari HA, Al-Manfouhi HA, Madda JP, Kovacs A, Sheikh M, Roberts O. Radiologic features of granulomatous mastitis. Breast J 17 (2011): 645-650.
- Seyma Yildiz, Ayse Aralasmak, Huseyin Kadioglu, Huseyin Toprak, Huseyin Yetis, Zuhal Gucin, et al. Radiologic findings of idiopathic granulomatous mastitis. Med Ultrason 17 (2015): 39-44.
- Fatih Altintoprak, Engin Karakece, Taner Kivilcim, Enis Dikicier, Guner Cakmak, Fehmi Celebi, et al. Idiopathic granulomatous mastitis: an autoimmune disease?. Sci World J 2013 (2013): 148727
- Naraynsingh V, Hariharan S, Dan D, Harnarayan P, Teelucksingh S. Conservative management for idiopathic granulomatous mastitis mimicking carcinoma: case reports and literature review. Breast Dis 31 (2010): 57-60.
- Benson JR, Dumitru D. Idiopathic granulomatous mastitis: presentation, investigation and management. Future Oncol 12 (2016): 1381-1394.
- Calis H, Karabeyoglu SM. Follow-up of granulomatous mastitis with monitoring versus surgery. Breast Dis 37 (2017): 69-72.
- Gautier N, Lalonde L, Tran-Thanh D, et al. Chronic granulomatous mastitis: imaging, pathology and management. Eur J Radiol 82 (2013): e165-e175.
- Boufettal H, El Hafidy K, Noun M, Hermas S, Samouh N. Mastite granulomateuse idiopathique bilatérale. Imagerie de la Femme 19 (2009): 262-264.
- Wilson JP, Massoll N, Marshall J, Foss RM, Copeland EM, Grobmyer SR. Idiopathic granulomatous mastitis: in search of a therapeutic paradigm. Am Surg 73 (2007): 798-802.
- Kok KY, Telisinghe PU. Granulomatous mastitis: presentation, treatment and outcome in 43 patients. Surgeon 8 (2010): 197?201.
- Akcan A, Aky?ld?z H, Deneme MA, Akgun H, Ar?tas Y. Granulomatous lobular mastitis: a complex diagnostic and therapeutic problem. World J Surg 30 (2006): 1403?1409.
- Freeman CM, Xia BT, Wilson GC, Lewis J D, Khan S, Lee S J, et al. Idiopathic granulomatous mastitis: a diagnostic and therapeutic challenge. Am J Surgery 214 (2017): 701?706.
- Ocal K, Dag A, Turkmenoglu O, Kara T, Seyit H, Konca K. Granulomatous mastitis: clinical, pathological features and management. Breast 16 (2010): 176?182.
- Leyla Ozel, Aysun Unal, Ethem Unal, Melih Kara, Erdal Erdo?du, Osman Krand, et al. Granulomatous mastitis: is it an autoimmune disease? Diagnostic and therapeutic dilemmas. Surg Today 42 (2012): 729-733.
- Jeffery E Illman, Simone B Terra, Allison J Clapp, Katie N Hunt, Robert T Fazzio, Sejal S Shah, et al. Granulomatous diseases of the breast and axilla. Radiological findings with pathological correlation. Insights Imaging 9 (2018): 59-71.
- Salem A, Bennaceur R, Driss M. Imagerie des mastites granulomateuses idiopathiques. Imagerie de la Femme 18 (2008): 46-54.
- Sabate J, Clotet M, Gomez A, De Las Heras P, Torrubia S, Salinas T. Radiologic evaluation of uncommon inflammatory and reactive breast disorders. Radiographics 25 (2005): 411-424.
- Muhammad Umair Bashir, Alexius Ramcharan, Sarah Alothman, Sabine Beaugris, Sarosh Ahmad Khan, Mohammed A Sbeih, et al. The enigma of granulomatous mastitis: a series. Breast Dis 37 (2017): 17-20.
- Islam A Elzahaby, Ashraf Khater, Adel Fathi, Islam Hany, Mohamed Abdelkhalek, Khaled Gaballah, et al. Etiologic revelation and outcome of the surgical management of idiopathic granulomatous mastitis; an Egyptian centre experience. Breast Disease 36 (2016): 115-122.
- Joseph KA, Luu X, Mor A. Granulomatous mastitis: a New York public hospital experience, Ann Surg Oncol 21 (2014): 4159-4163.
- Kayahan M, Kadioglu H, Muslumanoglu M. Management of patients with granulomatous mastitis: analysis of 31 cases, Breast Care (Basel) 7 (2012): 226-230.
- Kaviani A, Noveiry BB, Jamei K, Rabbani A. How to manage idiopathic granulomatous mastitis: suggestion of an algorithm. Breast 20 (2014): 110-112.
- Alper Akcan, A Bahadir Oz, Serap Dogan, Hülya Akgün, Muhammet Akyüz, Engin Ok, et al. Idiopathic granulomatous mastitis: comparison of wide local excision with or without corticosteroid therapy. Breast Care 9 (2014): 111-115.
- Sami Akbulut, Zulfu Arikanoglu, Ayhan Senol, Nilgun Sogutcu, Murat Basbug, Erhan Yeniaras, et al. Is methotrexate an acceptable treatment in the management of idiopathic granulomatous mastitis?. Arch Gynecol Obstet 284 (2011): 1189-1195.
