The Use of Latissimus Dorsi Mini-Flap in Partial Breast Reconstruction
Article Information
Maher H. Ibraheem1, Mina MG Youssef1,2, Youhanna Abdalla3, Rimoun Boutrus4, Amr Farouk5, Ahmed Morsi6
1Department of Surgical Oncology Department, National Cancer Institute, Cairo University, Giza, Egypt
2Department of Breast surgery, Norfolk and Norwich University hospital, Norwich, UK
3Department of Surgical Oncology, National Cancer Institute, Cairo University, Giza, Egypt
4Department of Radiation Oncology, National Cancer Institute, Cairo University, Giza, Egypt
5Department of Diagnostic and Interventional Radiology, National Cancer Institute, Cairo University, Giza, Egypt
6Department of Surgical Oncology, National Cancer Institute, Cairo University, Giza, Egypt
*Corresponding Author: Maher H Ibraheem, Department of Surgical Oncology, National Cancer Institute, Cairo University, Giza, Egypt
Received: 09 October 2019; Accepted: 12 October 2019; Published: 22 October 2019
Citation: Maher H. Ibraheem, Mina MG Youssef, Youhanna Abdalla, Rimoun Boutrus, Amr Farouk, Ahmed Morsi. The Use of Latissimus Dorsi Mini-Flap in Partial Breast Reconstruction. Journal of Cancer Science and Clinical Therapeutics 3 (2019): 240-250.
View / Download Pdf Share at FacebookAbstract
Introduction: The cosmetic drawbacks of breast conserving surgery are asymmetry, nipple or skin retraction, and volume loss with unsatisfactory cosmetic outcome. The principle of Latissimus dorsi mini-flap (LDMF) is to use part of the Latissimus dorsi (LD) muscle as volume replacement to large breast defect up to 20 -30 % of the breast volume.
Purpose: To evaluate (LDMF) as a volume replacement to large breast defect after wide local excision in different breast quadrants and the benefit of using this procedure regarding the cosmetic outcomes, patient satisfaction, procedure-related complications.
Materials and Methods: The study was carried out at the National Cancer Institute, Cairo University, Egypt, from September 2017 to December 2018. Fifteen patients were selected. Wide local excision with post-resection defects of 20%-30% of breast volume were done. An inferolateral incision was done for both tumor resection and LDMF harvesting without any back scar. The patients were scheduled for regular follow up.
Results: All the resection margins were negative. Mean Operative time was 176.6 minutes, the mean hospital stay was 2.47 days. The mean score for sensory preservation was 7.66. The mean of visual analogue score VAS was 8.33 with a score range from 8 to 9. The mean of the surgeon evaluation was 8.53. The median ranged from 8 to 9.
Conclusion: LDMF makes BCS possible to a group of patients who are classically required mastectomy. It is particularly benefical to patients that responds poorly to neoadjuvant chemotherapy or with wide spreading DCIS.
Keywords
<p>Mini Ld Flap; Partial Mastectomy Defect</p>
Mini Ld Flap articles, Partial Mastectomy Defect articles
Mini Ld Flap articles Mini Ld Flap Research articles Mini Ld Flap review articles Mini Ld Flap PubMed articles Mini Ld Flap PubMed Central articles Mini Ld Flap 2023 articles Mini Ld Flap 2024 articles Mini Ld Flap Scopus articles Mini Ld Flap impact factor journals Mini Ld Flap Scopus journals Mini Ld Flap PubMed journals Mini Ld Flap medical journals Mini Ld Flap free journals Mini Ld Flap best journals Mini Ld Flap top journals Mini Ld Flap free medical journals Mini Ld Flap famous journals Mini Ld Flap Google Scholar indexed journals Partial Mastectomy Defect articles Partial Mastectomy Defect Research articles Partial Mastectomy Defect review articles Partial Mastectomy Defect PubMed articles Partial Mastectomy Defect PubMed Central articles Partial Mastectomy Defect 2023 articles Partial Mastectomy Defect 2024 articles Partial Mastectomy Defect Scopus articles Partial Mastectomy Defect impact factor journals Partial Mastectomy Defect Scopus journals Partial Mastectomy Defect PubMed journals Partial Mastectomy Defect medical journals Partial Mastectomy Defect free journals Partial Mastectomy Defect best journals Partial Mastectomy Defect top journals Partial Mastectomy Defect free medical journals Partial Mastectomy Defect famous journals Partial Mastectomy Defect Google Scholar indexed journals Latissimus dorsi articles Latissimus dorsi Research articles Latissimus dorsi review articles Latissimus dorsi PubMed articles Latissimus dorsi PubMed Central articles Latissimus dorsi 2023 articles Latissimus dorsi 2024 articles Latissimus dorsi Scopus articles Latissimus dorsi impact factor journals Latissimus dorsi Scopus journals Latissimus dorsi PubMed journals Latissimus dorsi medical journals Latissimus dorsi free journals Latissimus dorsi best journals Latissimus dorsi top journals Latissimus dorsi free medical journals Latissimus dorsi famous journals Latissimus dorsi Google Scholar indexed journals cosmetic outcome articles cosmetic outcome Research articles cosmetic outcome review articles cosmetic outcome PubMed articles cosmetic outcome PubMed Central articles cosmetic outcome 2023 articles cosmetic outcome 2024 articles cosmetic outcome Scopus articles cosmetic outcome impact factor journals cosmetic outcome Scopus journals cosmetic outcome PubMed journals cosmetic outcome medical journals cosmetic outcome free journals cosmetic outcome best journals cosmetic outcome top journals cosmetic outcome free medical journals cosmetic outcome famous journals cosmetic outcome Google Scholar indexed journals breast conserving surgery articles breast conserving surgery Research articles breast conserving surgery review articles breast conserving surgery PubMed articles breast conserving surgery PubMed Central articles breast conserving surgery 2023 articles breast conserving surgery 2024 articles breast conserving surgery Scopus articles breast conserving surgery impact factor journals breast conserving surgery Scopus journals breast conserving surgery PubMed journals breast conserving surgery medical journals breast conserving surgery free journals breast conserving surgery best journals breast conserving surgery top journals breast conserving surgery free medical journals breast conserving surgery famous journals breast conserving surgery Google Scholar indexed journals autologous flap articles autologous flap Research articles autologous flap review articles autologous flap PubMed articles autologous flap PubMed Central articles autologous flap 2023 articles autologous flap 2024 articles autologous flap Scopus articles autologous flap impact factor journals autologous flap Scopus journals autologous flap PubMed journals autologous flap medical journals autologous flap free journals autologous flap best journals autologous flap top journals autologous flap free medical journals autologous flap famous journals autologous flap Google Scholar indexed journals thoracodorsal bundle articles thoracodorsal bundle Research articles thoracodorsal bundle review articles thoracodorsal bundle PubMed articles thoracodorsal bundle PubMed Central articles thoracodorsal bundle 2023 articles thoracodorsal bundle 2024 articles thoracodorsal bundle Scopus articles thoracodorsal bundle impact factor journals thoracodorsal bundle Scopus journals thoracodorsal bundle PubMed journals thoracodorsal bundle medical journals thoracodorsal bundle free journals thoracodorsal bundle best journals thoracodorsal bundle top journals thoracodorsal bundle free medical journals thoracodorsal bundle famous journals thoracodorsal bundle Google Scholar indexed journals breast volume articles breast volume Research articles breast volume review articles breast volume PubMed articles breast volume PubMed Central articles breast volume 2023 articles breast volume 2024 articles breast volume Scopus articles breast volume impact factor journals breast volume Scopus journals breast volume PubMed journals breast volume medical journals breast volume free journals breast volume best journals breast volume top journals breast volume free medical journals breast volume famous journals breast volume Google Scholar indexed journals breast defect articles breast defect Research articles breast defect review articles breast defect PubMed articles breast defect PubMed Central articles breast defect 2023 articles breast defect 2024 articles breast defect Scopus articles breast defect impact factor journals breast defect Scopus journals breast defect PubMed journals breast defect medical journals breast defect free journals breast defect best journals breast defect top journals breast defect free medical journals breast defect famous journals breast defect Google Scholar indexed journals widened scars articles widened scars Research articles widened scars review articles widened scars PubMed articles widened scars PubMed Central articles widened scars 2023 articles widened scars 2024 articles widened scars Scopus articles widened scars impact factor journals widened scars Scopus journals widened scars PubMed journals widened scars medical journals widened scars free journals widened scars best journals widened scars top journals widened scars free medical journals widened scars famous journals widened scars Google Scholar indexed journals
Article Details
1. Introduction
The cosmetic drawbacks of breast conserving surgery are asymmetry, nipple or skin retraction, and volume loss which resulted in an unsatisfactory cosmetic outcome [1]. The latissimus dorsi (LD) flap is an essential reconstruction option due to its stability and versatility as an autologous flap [2]. The disadvantage of the latissimus dorsi (LD) flap is related to the creation of an additional donor site with scarring and potential morbidity [3]. Drawbacks of autologous LD flap are seroma, widened scars, which occurs at the donor site secondary to increased tension on the healing dermis and poor wound healing which occur at the donor site if too much soft tissue is harvested [4]. The principle of LD mini-flap is to use part of the LD muscle as volume replacement of large breast defect up to 20 -30 % of the breast volume. The LD mini-flap is harvested based on thoracodorsal bundle [5].
2. Purpose
This study had been done to evaluate the Latissimus dorsi mini-?ap (LDMF) as a volume replacement to large breast defect after wide local excision in different breast quadrants and the benefit of using this procedure regarding the cosmetic outcomes, patient satisfaction, procedure-related complications.
3. Materials and Methods
This is a cohort study that was carried out after approval of the ethical committee of the National Cancer Institute of Cairo University in a period of time from September 2017 to December 2018. The research was carried out at the breast surgery unit of the National Cancer Institute of Cairo University. Fifteen female patients with a pathologically proven breast cancer were selected for the study. All patients underwent WLE as a part of BCT with post-resection defects of 20%-30% of breast volume, i.e. the defect is almost the size of one quadrant. We excluded patients who are not a candidate of BCT as Patients with Multi-centric disease or cannot tolerate radiotherapy. Subsequent to history and physical examination, patients underwent bilateral digital mammography and breast ultrasound. We used core biopsy to assess the histology, grade, biological markers as estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (Her2/ neu) and nuclear protein associated with cell proliferation (Ki67). The candidates were counselled preoperatively by the operating surgeons in order to obtain informed consents. Operative time included the time waiting for frozen section results was recorded. The patients were scheduled for weekly follow up for the first 2 months, then once monthly until 3 months after completion of radiotherapy. During these visits, postoperative photographs were taken in anterior and lateral views and any complications were recorded.
Three months after completion of radiotherapy patients’ satisfaction and Sensory preservation were assessed using simplified questionnaire based on Visual Analogue Scale (VAS). Final pictures were assessed by three independent surgeons and the medians were used for statistical analysis.
3.1 Surgical techniques
3.1.1 Wide local excision (WLE) of the tumor and margin assessment: The procedure started with the patient in supine position, an oblique S-shaped incision extended from infra-mammary fold toward the axilla. The incision was deepened to the subcutaneous tissue. Alternative approach was to do WLE through circumareolar incision. A skin flap was raised in subcutaneous tissue then wide local excision of the tumor with a safety margin. The margins were oriented and the specimen was sent for the frozen section for assessment. Axillary staging was done according to the clinical status with either sentinel L.N dissection or traditional axillary dissection. After confirmation of the negativity of the margins, the next step was to harvest the LD-mini flap.
3.1.2 Flap harvest: The patient position was changed to lateral decubitus. The key difference between this technique and autologous LD flap is that in this technique we used the same inferolateral incision to harvest the LD muscle without a back scar. Therefore, this technique is called scarless LD flap. The posterior axillary fold was identified then a flap elevated in the subcutaneous plane over the LD muscle toward the lumbosacral fascia. The thoracodorsal vessels could be identified entering the latissimus dorsi about 3 cm medial to the lateral edge of the muscle. At this level, 1 or 2 branches come from the thoracodorsal to the serratus anterior muscle; these could be traced proximally to identify the thoracodorsal artery. The neurovascular pedicle was then followed superiorly to its junction with the subscapular artery; the circumflex scapular artery arises near this junction. This artery should be preserved if possible, but if additional pedicle length was needed, the circumflex scapular vessels could be divided. The length of muscle needed to fill the defect was estimated by measuring from the apex of the axilla to the lower limit of the breast defect and adding few centimeters to this length. This extra length was added so that the muscle could be folded to create a satisfactory shape and volume. Later on, the Serratus anterior branches were divided to allow maximum mobility of the flap. The posterior edge of the LD muscle was then freed, and the deep perforators from the intercostal arteries were identified and ligated. The muscle could then be transected distally at a level determined by the amount of tissue required. The muscle was then elevated from distal to proximal and its insertion was divided at a level proximal to the entry of the thoracodorsal vessels. The flap was then based solely on its vascular pedicle and could be rotated and transferred to the surgical defect. The pedicle had to be inspected to assure that no torsion or kinking of the vessels then the flap was shaped to match the defect using interrupted absorbable suture. According to the site of the wide local excision, a tunnel was created from the axillary wound into the breast defect. In some patients this required removal of breast tissue to ensure that the flap sited comfortably without tension and without bulging. The tension on the pedicle was minimized by suturing the muscle to the superolateral edge of the pectoralis major muscle or to adjacent breast tissue. The muscle was then secured in the breast defect using absorbable sutures to fold the muscle to produce a shape and size required to fill the defect.
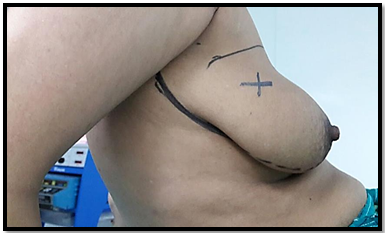
Figure 1: Preoperative image Shows incision planning. Figure x indicates the site of the tumor.

Figure 2: Intraoperative image shows the incision and flap elevation also x indicates the site of the tumor.

Figure 3: Intraoperative image shows the site of the defect after the resection.

Figure 4: Intraoperative image shows delivery of the flap through axillary incision.

Figure 5: Intraoperative image shows the flap pedicle. The flap is on the site of the defect superficially.
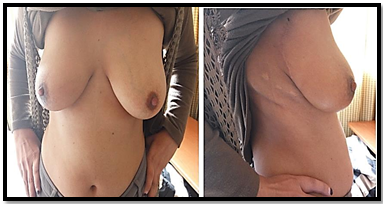
Figure 6: Anterior and lateral view of the same patient who had UOQ tumor at 7 months postoperatively.
4. Results
The mean age of the participants was 41.4 year with a median was 41 year. Eleven patients had the tumor in upper outer quadrant (UOQ). Two out of the 11 had a multifocal disease in the UOQ. Of the rest, 2 patients had a tumor in the upper inner quadrant (UIQ), one patient had a tumor in the central quadrant, and one patient had a tumor in LOQ. Eight patients had T3N1M0 tumors at the presentation. Five patients had T2N0M0 tumors & two patients had T3N0M0. All patients with locally advanced tumors received neoadjuvant chemotherapy. Seven patients had an axillary stage of N1 at paraffin section, five patients had N0 stage, two had N2 stage, and only one had N3 stage. Out of the ten locally advanced tumors at initial presentation, 8 had a partial clinical response and two had almost no response at all. 7 cases had Miller-Payne grade 2 (up to 30 % tumor cell loss), one case had Miller-Payne grade 3 (between 30% and 90% tumor cell loss). Two cases had Miller-Payne grade 1 (no reduction in overall cellularity). All the cases had satisfactory resection margins with the narrowest margin ranges from 8 to 30 mm. The results of the frozen section were almost identical to the results of the paraffin section. Because there were no significant differences between the results of frozen and paraffin sections, no single patient was re-operated on to obtain sufficient margins. The mean hospital stay was 2.47 days ranging from 2 to 5 days according to the post-operative course. Only 2 patients stayed for 5 days while 12 stayed for only 2 days. One patient stayed for 3 days. Mean Operative time was 176.6 minutes ranging from 160 to 195 minutes.
4.1 Complications
For the purpose of clarification, we divided the postoperative complications into major complications that required reoperation and minor complications that managed conservatively. We considered the major complications to be, flap necrosis and major.
bleeding that required operative intervention. Minor complications are Shoulder stiffness, prolonged seroma, minor bleeding, and infection. In all of the 15 cases, there were no major complications that required reoperation. Four patients reported Shoulder stiffness with limited abduction after 150 degrees. Shoulder stiffness was managed with physiotherapy with promising results. All patient suffered from Seroma. The mean of the duration of Seroma was 2.87 weeks ranging from 2 weeks in mild cases to 5 weeks in severe cases. Only one case from the 15 participants suffered from minor post-operative bleeding that was managed conservatively. This patient was on aspirin pre-operatively. Single case suffered from post-operative infection which was successfully managed with antibiotics for 2 weeks. Therefore, the infection rate in this study is only 6.6%.
4.2 Sensory preservation of breast skin in general
Sensory preservation was assessed by giving the patient a simple questionnaire we designed and the participants were asked to give a score in a scale from (1-10). The mean score for sensory preservation was 7.66. The patients gave a score ranging from 7 to 9.
4.3 Patient satisfaction
Patient satisfaction was assessed by Visual Analogue Scale (VAS). A simple questionnaire was designed and the participants were asked to give a score in a scale from (1-10). The mean of VAS was 8.33 with a score range from 8 to 9. For the purpose of statistical analysis, we considered a score of 8 meant significant result and a score of 9 highly significant.
4.4 Surgeon evaluation
Surgeon evaluation was done by three surgeons assessment score. In this method, three independent surgeons evaluated the same post-operative picture. Each surgeon received a questionnaire and was asked to give a score in a scale from (1-10). The median of the three evaluations was used in the statistical analysis. The mean of the surgeon evaluation was 8.53. The median ranged from 8 to 9.
4.5 Statistical analysis
Spearman correlation coefficient (r) was used to delineate the correlations between the results. There was a significant negative correlation between postoperative pain (in weeks) and VAS scores with a p-value of 0.023 and r of -0.580. This means that the patients with a greater post-operative pain reported less overall satisfaction than the patients with well-controlled postoperative pain. Therefore, postoperative pain is a psychological factor that affects patient satisfaction.
The surgeon, assessment score has a negative correlation with the volume of resection (defined by area x 10~3 in mm). This was signified by r- value of -0.588 and p- value of 0.021. This means there was a decrease of the surgeon satisfaction score with the increase in the volume of resection. However, the mean surgeon satisfaction score was high in general (8.5). Therefore, this procedure has a high overall surgeon satisfaction regarding the cosmetic outcome. There was a positive correlation between operative time and sensory preservation. This may indicate that in order to achieve more sensory preservation, the surgeon should be more meticulous and careful in handling the tissues in order to preserve as many cutaneous nerves as possible. Moreover, The procedure is not time-consuming so careful technique will not cause much delay in the operative time. There was a positive correlation between the operative time and Surgeons assessment score. This may signify the importance of intra-operative planning and meticulous handling of tissue. Post-operative pain duration (in weeks) was found to have a negative correlation with the sensory preservation score. Spearman correlation coefficient (r) was -0.632 and p-value was 0.012. This may be explained by that cutting of sensory nerves could both increase post-operative pain and affect negatively sensory preservation.
|
VAS score overall satisfaction |
Spearman correlation coefficient (r) |
P value |
|
Postoperative pain duration (weeks) |
-0.580 |
0.023 |
Table 1: Correlation between post-operative pain (in weeks) and VAS score.
|
Surgeons assessment score |
Spearman correlation coefficient (r) |
P value |
|
volume of resection |
-0.588 |
0.021 |
Table 2: Correlation between Surgeons assessment score and volume of resection.
|
P value |
Spearman correlation coefficient (r) |
Sensory preservation score |
|
0.043 |
0.528 |
Operative time |
Table 3: Correlation between the operative time and sensory preservation.
|
Surgeons assessment score |
Spearman correlation coefficient (r) |
P value |
|
Operative time |
0.565 |
0.028 |
Table 4: Correlation between between the operative time and Surgeons assessment score.
|
Sensory preservation score |
Spearman correlation coefficient (r) |
P value |
|
Postoperative pain duration (weeks) |
-0.632 |
0.012 |
Table 5: Correlation between between Sensory preservation score and Postoperative pain duration (weeks).
5. Discussion
Raja M A K et al. [6] founded that the use of the LDMF for breast reconstruction limits the deformity resulting from the loss of breast tissue; moreover, it does not appear to atrophy significantly with time [6]. There are similar results in our study as indicated by the high both patient and surgeon satisfaction scores.They stated that the LDMF does not produce significant scarring within the breast but remains soft and pliable following radiotherapy [6]. In our study, there was high patient satisfaction and sensory preservation even after 7 months follow up. This may indirectly indicate reduced scarring by using this procedure. Raja reported a low rate of complications with this procedure and flap loss with the LDMF appears uncommon, but has been reported [6]. In our study there also, a low rate of complication. Moreover, flap loss had not developed in any of the 15 cases. Dixon et al. [7] has performed this procedure on 30 patients with large breast tumor and reported a low rate of complications. They reported two cases of postoperative bleeding that required reoperation [7]. In our study, only one patient has bled post-operatively and managed conservatively with no need of reoperation. They concluded that a two-stage procedure is better for margin assessment [7]. In our study, none of the patients who had LDMF reconstruction required reoperation for a positive margin which indicates that two-stage procedure is not necessary with the current frozen section techniques.
Gendy et al. [8] performed a retrospective study on 106 patients to compare skin-sparing mastectomy (SSM) and LDMF regarding surgical complications, functional disability, cosmetic result, and psychological morbidity [8]. They concluded that LDMF is a feasible procedure and safe from the oncological point. LDMF can achieve a satisfactory cosmetic outcome when 20%-30% of the breast has to be resected leaving a large resection defect in small to medium sized breasts [8]. In our study, the mean of VAS was 8.33 with a score range from 8 to 9 which indicate high patient satisfaction. They also noted that postoperative surgical complications were less common in LDMF in comparison to skin-sparing mastectomy (SSM) and rarely required reoperation [8] In our study, there was no comparison between SSM and LDMF. However, all the complications in our study were minor and none required reoperation. In our study, there was no single case of skin envelope necrosis. Therefore, this complication is very rare with the LDMF. Gendy et al. [8] concluded that LDMF reconstruction was associated with a minor degree of sensory loss in contrast to skin sparing mastectomy with preservation of nipple-areola complex sensation in the majority of the cases [8]. In our study, there was high overall sensory preservation with a mean score for sensory preservation of 7.66. Gendy et al. [8] concluded that LDMF is a less major procedure than skin-sparing mastectomy (SSM), as it avoids extensive dissection, additional scars and the use of a prosthesis. As a result, it may provide a useful alternative to mastectomy [8]. In our study, we founded that LDMF not to be a time-consuming procedure as the average operative time was generally less than three hours. This time included the time for resection and the time waiting for frozen section results. Gendy et al. [8] stated that the judgment of cosmetic outcome is prone to bias and no single method of assessment is entirely reliable [8]. Our method to take both patient’s satisfaction and surgeons’ assessment into consideration. Both gave comparable results. In our study, shoulder disability affected 26.7 % of the patients. This result is comparable to the result of Gendy et al. [8] (25% shoulder disability affects patient work). This may be related to the volume of the LD muscle harvested during dissection. However, our patients reported improvement with physiotherapy and only a minor impact on daily activity.
Rainsbury and Paramanathan performed LDMF on 70 patients with tumor diameter up to 40 mm. The age of the patients in their study ranged from 28-60 years (mean 46 year). They reported low complication rate (rate of 11%) [9]. Rainsbury and Paramanathan reported that Cosmetic failure was uncommon following LDMF even with extensive parenchymal resection (>150 g). On the other hand, they reported cosmetic failure of more than one third in those who underwent extensive WLE without reconstruction [9]. Another reliable option for partial breast reconstruction is chest wall perforator ?aps. The main advantage of these techniques is minimizing the donor site morbidity by preserving the underlying muscles. However, these techniques are more challenging for reconstructive surgeons [10]. The pedicled perforator ?aps commonly used for breast or thoracic reconstruction are the thoracodorsal artery perforator (TDAP) ?ap, lateral intercostal artery perforator (LICAP), anterior inter-costal artery perforator (AICAP), and the serratus anterior artery perforator (SAAP) ?ap [10]. Hamdi M et al. [10] described an algorithm by using pedicled perforator ?aps in breast surgery, which spares the LD muscle. They provided indications for the use of pedicled perforator ?aps which include partial breast reconstruction, salvage procedure after signi?cant partial failure of free ?ap for breast reconstruction and reconstruction of large thoracic defects [10]. The contraindications to the pedicled perforator ?aps are the following:
- Damage to the thoracodorsal pedicle is an absolute contraindication to raising a TDAP ?ap.
- Previous surgery to the axilla or lung (lateral thoracotomy)
- 3-radiotherapy to the region may also result in damage to the perforators.
- Large breast defects in thin patients are often dif?cult to reconstruct with pedicled perforator ?aps due to a lack of suf?cient ?ap volume [10].
The TDAP flap is based on the lateral descending branch of the thoracodorsal artery. This is one of the two terminal branches of the thoracodorsal artery [10]. Hamdi M, et al reported that donor-site morbidity was reduced significantly by using the pedicle perforator flaps as the LD muscle is left intact with functional motor innervation. Moreover, they reported a significant decrease in pain and seroma [10]. Another potential advantage for the use of the perforator ?aps is the preservation of the LD muscle for a later use especially in the case of LICAP ?ap where the thoracodorsal pedicle is not disturbed [10]. Adler N et al. [11] conducted a retrospective study on 18 patients to evaluate the use of TDAP flap. Eleven patients had complete breast reconstruction using a TDAP ?ap with simultaneous insertion of an expander or implant. Four cases were partial reconstruction to gain additional volume after previous breast reconstruction and the 3 other cases were reconstruction after lumpectomy [11].
Adler N et al. [11] reported that all the TDAP flaps in their study survived with only two cases required evacuation of hematoma. One case had late extrusion of the expander after expansion in the previously irradiated tissue, requiring expander removal. There were no donor site complications [11]. Recent anatomical studies showed some variation in the location of the branching point and the perforators. This adds to the difficulty of the procedure [11]. Several studies showed that after the transfer of the LD muscle, shoulder strength and/or the range of motion deteriorate. In our study, 26% of the patients reported shoulder stiffness. Therefore, prospective controlled trials comparing both LDMF and perforators flaps should be our focus in the future [12].
In view of our study, the advantages of the LDMF over perforator flaps are as follow:
- The LDMF provides a larger volume for larger breast defect.
- The LDMF as it is a scarless procedure, it spares the patient a scar that could be disfiguring in contrast to perforator flaps.
- Depending on the main thoracodorsal pedicle theoretically make the rate of flap loss much lower.
- TDAP flap results in a large scar on the patients’ chest which could be disfiguring especially in patients who undergo a conservative procedure such as CBT.
- Moreover, TDAP has limitations in reconstruction defects, especially in the inner quadrants.
Preserving the LD muscle in a certain group of young athletic patients must be considered. Hence the need of comparison and clarification of the indications must be standardized in the future [11]. Harvesting of the LD muscle results in the higher serum rate of the donor site. In our study, all the 15 patients suffered from donor site seromas. In contrast to the study conducted by Adler, Neta et al, they reported none of their 18 patients suffered from donor site seromas [11].
6. Conclusion
LDMF volume replacement makes breast-conserving surgery possible for a group of patients who are classically required mastectomy. This technique is particularly benefical to patients with tumors that responds poorly to neoadjuvant chemotherapy or patient with wide spreading DCIS. This procedure is safe, with a low rate of complications, high patient satisfaction rate and a good cosmetic outcome.
References
- Haloua MH, Krekel NM, Jacobs GJ, et al. Cosmetic Outcome Assessment following Breast-Conserving Therapy: A Comparison between BCCT. core Software and Panel Evaluation. International journal of breast cancer (2014): 716-860.
- Sood R, Easow JM, Konopka G, et al. Latissimus Dorsi Flap in Breast Reconstruction: Recent Innovations in the Workhorse Flap. Cancer control: journal of the Moffitt Cancer Center 25 (2018): 1073274817744638.
- Nelson JA, Lee IT, Disa JJ. The Functional Impact of Breast Reconstruction: An Overview and Update. Plastic and reconstructive surgery. Global open 6 (2018): e1640.
- Fernando Hernanz, Sara Regaño, Carlos Redondo-Figuero, et al. Oncoplastic breast-conserving surgery: analysis of quadrantectomy and immediate reconstruction with latissimus dorsi flap. World J Surg 31 (2007): 1934-1940.
- Rainsbury RM. Breast-Sparing Reconstruction with Latissimus Dorsi Miniflaps. European Journal of Surgical Oncology (EJSO) 28 (2002): 891-895.
- Raja M, Straker V, Rainsbury R. Extending the Role of Breast-Conserving Surgery by Immediate Volume Replacement. British Journal of Surgery 84 (1997): 101-105.
- Dixon JM, Venizelos B, Chan P. Latissimus dorsi mini-flap: a technique for extending breast conservation. Breast 11 (2002): 58-65.
- Gendy RK, Able JA, Rainsbury RM. Impact of skin-sparing mastectomy with immediate reconstruction and breast sparing reconstruction with miniflaps on the outcomes of oncoplastic breast surgery. Br J Surg 90 (2003): 433-439.
- Rainsbury RM, Paramanathan N. Breast Cancer 5 (1998): 139.
- Hamdi M, Van Landuyt K, Monstrey S, et al. Pedicled perforator ?aps in breast reconstruction: a new concept. Br Plast Surg 57 (2004): 531-539.
- Adler N, Seitz IA, Song DH. Pedicled thoracodorsal artery perforator flap in breast reconstruction: clinical experience. Eplasty 9 (2009): e24.
- Adams WP, Lipschitz AH, AnsariM, et al. Functional donor site morbidity following latissimus dorsi muscle ?ap transfer. Ann Plast Surg 53 (2004): 6-11.
