The Use of Clinical Scores to Predict Intensive Care Admission and Mortality in Patients with Covid-19 Disease
Article Information
Simone Zanella1*, Mancosu Alena2, Brugnolli Anna3, Franceschi Francesco4, Carrara Alessandro1, Claudio Ramponi5, Bevilacqua Anita3, Marinelli Elisa3, Ricci Nicola5 and Francesco Buccelletti5
1Department of Surgery, S. Maria del Carmine Hospital, Corso Verona 4, 38068 Rovereto, Italy
2Nurse, 38068 Trento, Italy
3Nursing School of Trento, University of Verona, Verona, Italy
4Institute of Internal Medicine, Catholic University of Rome, Rome, Italy
5Department of Emergency Medicine, S. Chiara Hospital, Largo Medaglie d’oro 9, 38122 Trento, Italy
*Corresponding author: Simone Zanella, General Surgery, S. Maria del Carmine Hospital, Corso Verona 4, 38068 Rovereto, Italy.
Received: 11 September 2022; Accepted: 21 September 2022; Published: 05 October 2022
Citation: Simone Zanella, Mancosu Alena, Brugnolli Anna, Franceschi Francesco, Carrara Alessandro, Claudio Ramponi, Bevilacqua Anita, Marinelli Elisa, Ricci Nicola and Francesco Buccelletti. The Use of Clinical Scores to Predict Intensive Care Admission and Mortality in Patients with Covid-19 Disease. Archives of Clinical and Biomedical Research 6 (2022): 836-843.
View / Download Pdf Share at FacebookAbstract
Introduction: The SARS-Cov2 pandemic worldwide has to date caused 270,000,000 cases and 5,000,000 deaths. Many clinical scores are available for patients who arrive at the Emergency Department with Covid-19 disease and many studies carried out prospectively and retrospectively have demonstrated their effectiveness. In literature no study and no metaanalysis have been performed to evaluate the admission to intensive care unit (ICU) and mortality rates and to establish the best score to be used.
Materials and Methods: The keywords used for the investigation were clinical scores, risk stratifications, Covid patients and Emergency Department. Ultimately the selected articles were entirely found using the PubMed database. In our meta-analysis we evaluated scores obtained studying patients with Covid-19 disease and also scores already known in clinical practice and subsequently used in Covid pandemic. Sensitivity, specificity, positive (PPV) and negative predicting value (NPV), diagnostic accuracy, the Receiver Operating Characteristic (ROC) curve and the Area Under the Curve (AUC) were calculated for each score. We assessed the homogeneity of all studies covered by our meta-analysis and at the end we created a Funnel Plot diagram in order to compare the scores.
Results: A total of 8 studies, 5 retrospective observational and 3 prospective, were analyzed. When considering meta-analyzes the highest value, LR + 9.1 (4.76 - 17.5), refers to NEWS. When considering ICU admission and mortality, the AUC values referring to NEWS are 0.9 (0.9 - 1.00) and 0.9 (0.72 - 1.00) respectively. The LR +, AUC values for intensive care and mortality are 3.3 (2.4-4.3), 0.8 (0.72-0.88) and 0.8 (0.72-0.88) for NEWS2. Evaluating the fixed effect, the LR + value of q-SOFA is 2.816. The AUC value is 0.8 (0.76 - 0.85) for mortality and 0.8 (0.64
Keywords
Covid-19; Clinical Scores and Emergency Department; Risk Stratification; SARS-Cov2
Covid-19 articles; Clinical Scores and Emergency Department articles; Risk Stratification articles; SARS-Cov2 articles
Article Details
1. Introduction
SARS-Cov2, a new coronavirus which causes COVID-19 illness, was initially identified in Wuhan, China, in December 2019 [1] and quickly spread, causing a pandemic that has been one of the most significant health, social and economic problems worldwide. The virus has caused more than 370,000,000 confirmed cases worldwide and more than 6,000,000 deaths [2]. SARS-Cov2 is the seventh coronavirus to date that is known to infect humans. In the recent past other two pandemics caused by two Coronaviruses [3,4] occurred. The Severe Acute Respiratory Syndrome and the Middle Est Respiratory Coronaviruses [3,4] were discovered in China (2002) and in the Middle East (2012) respectively. The mortality rates were approximately 10% for the SARS-Cov illness and 35% for MERS. The new coronavirus-2019 is an enveloped RNA genomic virus whose nucleocapsid is surrounded by a phospholipid bilayer consisting of the spike protein and the hemagglutinin-esterase. To date it is thought that bats were probably the initial hosts and pangolins the intermediate ones as reported in previous studies [5]. The COVID-19 illness primarily involves the lower respiratory tract. The virus, using the angiotensin-converting enzyme 2 (ACE2) receptor, binds to epithelial cells in the oral and nasal cavities and can migrate down into the lower respiratory tract. The virus transforms the cell into a "virus factory" and uses it to replicate the RNA and all the viral proteins which will subsequently be assembled inside the cell to cause its death through the release of new viral particles of SARS-Cov2. Patients may arrive at the Emergency Department (ED) in critical condition due to severe pneumonia requiring ICU admission or develop worsening symptoms that could lead to death. In most cases COVID-19 is like a typical seasonal flu [6]. Recent studies [7] identified as mortality related risk factors smoke, old age, cancer, diabetes, Body Mass Index > 30. The incubation period is 4-5 days after exposure but in some cases it can be as high as 14 days. The most common symptoms are fever (88%), a cough (67%), fatigue (38%), shortness of breath (33%), gastrointestinal symptoms (5%), anosmia and dysgeusia. Most cases are classified as mild (81%), 14% as severe and 5% as critical [6]. The US National Institutes of Health (NIH) has formulated a classification of the 5 clinical stages of COVID-19 [8]:
- Asymptomatic or pre-symptomatic infection: the patient diagnosed with SARS-CoV-2 is completely asymptomatic.
- Mild illness: the patient has mild symptoms (fever, cough, headache, fatigue), no dyspnea and no radiologically detectable alterations.
- Moderate disease: the patient has an oxygen saturation of ≥ 94% and there is clinical or radiological evidence of pneumonia.
- Severe disease: the patient shows a change in a number of parameters such as oxygen saturation ≤ 93% and PaO2/FiO2≤ 300 mmHg.
- Critical illness: respiratory failure, septic shock and/or failure of one or multiple organs.
Virus transmission occurs through droplets and the virus can remain on surfaces up to several days (plastic) and up to a few hours in the air [9]. The high transmissibility caused a rapid increase in cases initially in China, where the pandemic originated and from where it quickly spread to the rest of the world. In Italy and in Europe strict measures such as lockdowns were adopted to limit the diffusion of the virus [10]. Increased case numbers and clinical experiences allowed doctors to increase their knowledge of the disease, but many more studies are required to improve the treatment of these patients. To date no meta-analysis has ever been performed nor have all the clinical scores analyzed been compared. The aim of our study was to analyze and to compare the various clinical scores usable in patients with Covid-19 and to detect which of these are reliable in predicting mortality and ICU admission.
2. Materials and Methods
Are there clinical scores that are more effective than others in predicting mortality and ICU admission of patients with Covid-19 in an ED or in the first phase of Covid-19 disease management? This is the main focus of this research paper.
PICO QuestionPopulation: Patients over 18 years of age with symptoms and confirmed COVID-19 disease who had been admitted to hospital
Intervention: Clinical scores and scales
Comparison: Clinical assessment
Outcomes: ICU admission and hospital mortality
2.1 Data Source, Search Strategy
The PubMed, the Cochrane Database of Systematic Re-view and the Cumulative Index of Nursing and Allied Health Literature Database (CINAHL) were used to search articles and to perform the review of the literature. Clinical scores, risk stratifications, Covid patients and Emergency Department were the key words searched. The PubMed database was used to find the definitive articles.
2.2 Study Selection
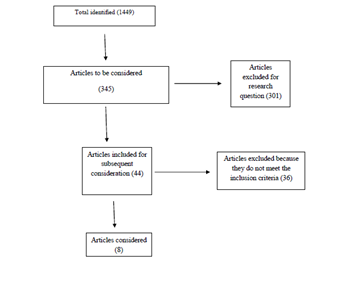
Two investigators (SZ and MA) conducted the study selection and evaluated the titles and the abstracts. A third investigator (BF) resolved any discrepancies. The inclusion criteria were adult patients (18+) with symptoms and diagnosed Covid-19 disease who had accessed the ED or who had been admitted directly to hospital, all studies regarding Covid-19 disease such as clinical trials and meta-analyses and articles published in English in the last two years. The exclusion criteria were articles regarding patients < 18 years old, articles that did not consider ICU admission or mortality in Covid-19 patients and articles that did not analyze the effectiveness of a score or a scale. The meta-analysis was conducted using the Preferred Reporting Items for Systematic Reviews and Meta-analysis statement (PRISMA statement) and its related items [11] and the significance level was set at 5%. I2 statistics were used to assess heterogeneity, with a value between 0-25% considered indicative of negligible heterogeneity, a value between 25%-75% indicative of moderate heterogeneity, and a value ≥75% of substantial heterogeneity.
2.3 Scores Analyzed
This study evaluated all the following scores:
- CURB-65 [11]
- MEWS [12]
- NEWS and NEWS2 [13-15]
- POINT OF MORTALITY 4C [16]
- PSI [17]
- SIRS [18]
- q-SOFA [17-18]
- REMS [19]
- RISE UP [20]
- TRPNCLP and STPCAL [21]
2.4 Statistical Analysis
The Diagnostic Test Calculator was used to obtain likelihood ratios (LR) both positive and negative and to define the interval of confidence for each score analyzed. Sensitivity, specificity, positive (PPV) and negative predicting value (NPV), diagnostic accuracy, Receiver Operating Characteristic (ROC) curve and the Area Under the Curve (AUC) were all calculated. The values of the area below the ROC curve were evaluated using the classification proposed by Swets [19].
2.5 Funnel Plot Diagram
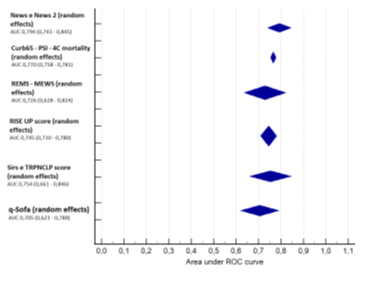
All score analyzed were compared the homogeneity of the studies verified creating a Funnel Plot diagram. RevMan5 was used to create graphs and conduct a meta-analysis. Meta-analyses were also performed using the “random effect” model. The p-value (*) as reported in Fig 1 was always <0.001 for each score. It was necessary to merge the SIRS and TRPNCLP scores because only one value was available.
2.6 Meta-Analysis
A Forest Plot diagram representing each score (or group of scores) is represented in Figure 1.
3. Results
A search was performed using Pubmed, Cochrane Database of Systematic Re-view and Cumulative Index to Nursing and Allied Health Literature (CINAHL) Database. We identified 1449 articles. Only 345 articles were assessed for eligibility and 301 were excluded from research topic. At the end 44 articles were included for further consideration and 36 were excluded after screening title and abstract. Only 8 articles (5 retrospective and 3 prospective) were included [14-17,19-20,21,23]. A flow chart is presented in Figure 2. The likelihood ratio, both positive and negative, and the AUC for each score analyzed and for each study considered are shown in Table 1 and Table 2. Regarding the AUC values, if not specified, we considered both the ICU admission and mortality and the p-value (*) was always <0.001 for each score. Considering the meta-analyzes it can be observed that the highest value, LR + 14 (1.64-113) refers to q-SOFA (95% CI: 81.2 to 94.8, p<0.0001, I2: 90.1 %). The second one, LR + 9.1 (4.76-17.5), refers to NEWS (95% CI: 94.8 to 97.4, p<0.0001, I2: 96.3 %). Analyzing the study of Jang et al. [17] the NEWS score has an AUC value of 0.9 (0.9 – 1.00) for ICU admission and 0.9 (0.72 – 1.00) for mortality. Considering mortality and ICU admission the q-SOFA score has a value of 0.8 (0.76 - 0.85) and 0. 8 (0.64 - 0.93) respectively and both very diagnostically very accurate. SIRS (95% CI: 65.5 to 92.8, p< 0.0001, I2: 83.8 %), CURB-65 (95% CI: 0 to 81.1, p=0.03, I2: 56.1 %) and MEWS (95% CI: 94 to 98.1, p<0.0001, I2: 96.7 %) are less effective as demonstrated by their AUC values < 0.8. When we evaluate mortality and ICU admission with REMS score values > 6 (95% CI: 94 to 98.1, p<0.0001, I2: 96.7 %) the AUC values are 0.9 (0.8-0.9) and 0.74 (0.69-0.79) respectively. Huang et al. [21] in their study presented a TRPNCLP score (95% CI: 63.5 to 92.8, p= 0.0001, I2: 83.8 %) to evaluate duration of hospitalization and disease progression in moderate and severe patients with COVID-19. We found in our meta-analysis an AUC value of 0.9 (0.8 - 0.9) and an LR + of 4.9 (4.0 - 5.9). The RISE UP (95% CI: 0 to 94.4, p= 0.08, I2: 66.7 %) score by van Dam et al. [20] and the 4C mortality score (95% CI: 0 to 81.1, p=0.03, I2: 56.1 %) by Knight et al. [16] also showed excellent results with an LR + maximum value of 2.6 (2.1-3.3) and AUC values of 0.8 (0.73-0.81) and 0.79 (0.78-0.81) for mortality and ICU admission respectively.
|
Severe disease (ICU admission or mortality), non-severe disease |
||||
|
LR + |
LR - |
AUROC |
||
|
NEWS >= 5 |
||||
|
-Covino et al. [19] |
4.4 (3.1 - 6.1) |
0.4 (0.3 - 0.6) |
0.8 (ICU 0.8 – 0.9) |
|
|
-Covino et al. [19] |
2.8 (2.0 - 3.9) |
0.3 (0.1 - 0.9) |
0.8 (mortality 0.7 – 0.8) |
|
|
-Jang et al. [17] |
9.1 (4.76 - 17.5) |
0.18 (0.03 - 1.10) |
0.9 (ICU 0.9 – 1.00) |
|
|
-Jang et al. [17] |
0.9 (mortality 0.72 – 1.00) |
|||
|
- Knight et al. [16] |
0.65 (mortality 0.65 – 0.66) |
|||
|
NEWS2 >=5 |
||||
|
-Holten et al. [23] |
2.06 (1.59 - 2.66) |
0.31 (0.15 - 0.60) |
0.80 (0.72 – 0.88) |
|
|
-Covino et al. [19] |
3.3 (2.4 – 4.3) |
0.4 (0.3 – 0.6) |
0.78 (ICU 0.73 – 0.82) |
|
|
-Covino et al. [19] |
2.7 (1.8 – 4.0) |
0.4 (0.1 – 1.0) |
0.75 (mortality 0.70 – 0.80) |
|
|
-Myrstad et al. [14] |
2.95 (1.84 – 4.71) |
0.19 (0.05 – 0.69) |
0.79 (0.66 – 0.91) |
|
|
-Gidari et al. [15] |
2.6 (1.7 – 4.1) |
0.2 (0.1 – 0.5) |
0.75 (ICU 0.63 – 0.85) |
|
|
SIRS >= 2 |
||||
|
-Holten et al. [23] |
1.64 (1.29 - 2.09) |
0.41 (0.21 - 0.77) |
0.70 (all 0.61 – 0.80) |
|
|
-Myrstad et al. [14] |
1.80 (1.02 – 3.17) |
0.60 (0.31 – 1.15) |
0.63 (all 0.47 – 0.80) |
|
|
-Jang et al. [17] |
0.639 (mortality 0.42 – 0.86) |
|||
|
-Jang et al. [17] |
0.79 (ICU 0.66 – 0.93) |
|||
|
CURB-65 >=2 |
||||
|
- Holten et al. [23] |
2.8 (1.82 - 4.33) |
0.53 (0.36 - 0.78) |
0.75 (all 0.65 – 0.84) |
|
|
-Myrstad et al. [14] |
2.72 (0.83 – 8.87) |
0.81 (0.59 – 1.12) |
0.58 (all 0.41 – 0.76) |
|
|
-Knight et al. [16] |
0.76 (mortality 0.74 – 0.79) |
|||
|
QSOFA >=2 |
||||
|
-Holten et al. [23] |
4.9 (2 - 12) |
0.78 (0.64 - 0.95) |
0.70 (0.61 – 0.79) |
|
|
-Covino et al. [19] |
1.7 (1.1 – 2.6) |
0.80 (0.7 – 1.0) |
0.56 (ICU 0.51 – 0.62) |
|
|
-Covino et al. [19] |
4.0 (2.8 – 5.7) |
0.2 (0.1 – 0.8) |
0.8 (mortality 0.76 – 0.85) |
|
|
-Myrstad et al. [14] |
14 (1.64 – 113) |
0.75 (0.55 – 1.02) |
0.62 (0.45 – 0.81) |
|
|
-Knight et al. [16] |
0.62 (mortality 0.615 – 0.630) |
|||
|
-Jang et al. [17] |
0. 8 (mortality 0.60 – 0.96) |
|||
|
- Jang et al. [17] |
0.8 ( ICU 0.64 – 0.93) |
|||
Table 1: Likelihood ratio and AUROC.
|
Severe disease (ICU admission or mortality), non-severe disease |
||||
|
LR + |
LR - |
AUROC |
||
|
PSI >=3 |
||||
|
-Holten et al. [23] |
2,39 (1.71 - 3.33) |
0,41 (0.25 - 0.69) |
0,75 (mix 0.65 – 0.84) |
|
|
-Knight et al. [20] |
0,736 (mortality 0.68 – 0.79) |
|||
|
REMS > 6 |
||||
|
-Covino et al. [18] |
2,4 (1.8 – 3.2) |
0,5 (0.3 – 0.7) |
0,74 (ICU 0.69 – 0.79) |
|
|
-Covino et al. [18] |
3.2 (2.5 – 4.2) |
0.1 (0.1 – 0.8) |
0,9 (mortality 0.8 – 0.9) |
|
|
MEWS >5 |
||||
|
-Covino et al. [18] |
2,0 (1.6 – 2.5) |
0,50 (0.3 – 0.7) |
0,65 (ICU 0.60 – 0.70) |
|
|
-Covino et al. [18] |
1,6 (1.0 – 2.6) |
0,60 (0.3 – 1.0) |
0,63 (mortality 0.58 – 0.68) |
|
|
TRPNCLP |
||||
|
- Huang et al. [21] |
4,9 (4.0– 5.9) |
0.21 (0.14 – 0.31) |
0,9 (all 0.8 – 0.9) |
|
|
RISE UP SCORE |
||||
|
- van Dam et al. [19] |
2.49 (2.04 – 3.02) |
0,51 (0.42 – 0.62) |
0,8 (mortality 0.73 – 0.81) |
|
|
- van Dam et al. [19] |
2.6 (2.1 – 3.33) |
0.08 (0.04 – 0.14) |
0,79 (all 0.78 – 0.81) |
|
|
4C mortality score |
||||
|
- R. Knight et al. [20] (validation court) |
1,51 (1.48 – 1.53) |
0,19 (0.18 – 0.21) |
0,767 (mortality 0.760 – 0.773) |
|
|
- R. Knight et al. [20] (derivation court) |
0,786 (0.781 – 0.807) |
|||
Table 2: Likelihood ratio and AUROC.
4. Discussion
In our work we analyzed RISE-UP, 4C mortality, TRPNCLP scores studied for patients with Covid-19 disease and scores such as NEWS, MEWS, q-SOFA, CURB-65, SIRS, REMS and PSI used every day to evaluate the patients in ED and during pandemic also in patients with Covid-19 illness. When looking at the meta-analyzes we can observe that the highest value, LR + 9.1 (4.76-17.5), refers to NEWS. Considering the same study [19] we found AUC values of 0.8 (0.8-0.9) and 0.8 (0.7-0.8) regarding ICU admission and mortality. Analyzing the study of Jang et al. [17] we obtained the highest AUC values, respectively of 0.9 (0.9-1.00) for admission to intensive care and 0.9 (0.72 - 1.00) for mortality. The random effect value of q-SOFA is 3.707 (1.675 - 8.203) but its high value is mainly determined by Myrstad et al. [12] with an LR + of 14 (1.64 - 113). The study of Holten et al. [23] presents a positive likelihood ratio of 4.9 (2 - 12), the third high value in our meta-analysis. Myrstad et al. [12] performed a prospective cohort study based on 66 patients and for this reason it has a little impact on the meta-analisys. Evaluating the fixed effect, the LR+ would be 2.816, which is largely positive value considering the research question. The q-SOFA score, as demonstrated also in other previous studies, is the second-best useable score for patients with Covid-19. When considering the study of Jang et al. [14], we obtained an AUC value of 0.8 both for intensive care unit admission and mortality. When considering q-SOFA we observed that other studies had AUC values of less than 0.70. CURB-65, MEWS and SIRS are less usable. The highest positive likelihood ratio is 2.8 (1.82-4.33) referred to CURB-65 and considering ICU admission and mortality the AUC values are always less than 0.80 for all scores. Covino et al. [18] evaluated with a retrospective study the REMS score. Mortality has an AUC value of 0.9 (0.8-0.9) and a positive likelihood ratio of 3.2 (2.5 - 4.2) when the REMS score is greater than 6. Other studies are necessary to evaluate this score because the only study considered in our meta-analysis is a retrospective study and refers to a specific population. Huang et al. [21] created a score to predict the risk of hospitalization and disease progression in patients with Covid-19. The TRPNCLP is probably the most useable score; when considering ICU admission and mortality, the AUC values are 0.9 (0.8-0.9) and a positive likelihood ratio of 4.9 (4.0-5.9). The score was evaluated in a recent study [21], it could therefore also be used across Europe and the United States, but it has some limitations due to values obtained only through a blood test. Other two scores could be interesting to use. Van Dam et al. [19] and Knight et al. [20] developed the RISE UP and the 4C mortality scores. Based on a large population both of them maintain AUC values slightly lower than 0.8 and likelihood positive values higher than 1. NEWS and NEWS2 are the most usable score to evaluate disease progression with an ICU admission and mortality in patients with Covid-19 illness. These scores, among all considered, are the easiest to use for all healthcare professionals. Other studies will be necessary to evaluate the use of these scores especially during the first phase of the disease when patients are at home and must monitor themselves. q-SOFA is probably the second best score to use because considering few values it give us an exhaustive information of the patient. The score created for Covid-19 pandemic such as TRPNCLP, 4C mortality and RISE-UP are probably more accurate but not usable at home and when patients is in ER department require a long time to obtain all the informations to evaluate clinical situation of the patients.
5. Conclusions
NEWS and NEWS2 have proven to be, according to our study, the most useful scores to predict disease progression with intensive care admission or mortality. These scores are very easy to use; healthcare professionals as well as the patients themselves could use them from home in the first phase of the disease. Furthermore, the values of the scores could be communicated at any time to a third person such as a family doctor or a nurse. Meta-analysis is important because even today the first phase of Covid-19 disease management is a “Wait and see” approach, which essentially means monitoring at home. The positive case is recorded, the parameters and clinical conditions of the infected person are monitored, but basically there is no treatment. The person is expected to fight the virus through their own immune system. The clinical picture and the symptoms (severe pneumonia and respiratory distress) of the patient will need to get worse for him/her to be admitted to hospital. In our opinion targeted monitoring using clinical scores that are highly reliable in predicting worsening and mortality could be an effective strategy.
Limitations
It is necessary to report a number of important limitations regarding the drafting of this literature review. Firstly, the sample of articles taken into consideration is not particularly high. In some cases, in fact, it was not possible to calculate certain parameters (likelihood ratio). Secondly, all the articles are observational retrospective cohort studies, therefore significant "gold standard" elements for evidence-based research are not included: randomized assignment, the presence of a control group (only one article performed the study with a second control group - R. Knight et al. [20], blindness and masking or blinding). Hierarchically stronger studies such as meta-analysis or RCT were therefore not included. Furthermore, as this is an extremely current topic, the data is constantly changing and there will undoubtedly be an evolution of the virus, the disease related to it and the relative treatment of the patients by healthcare professionals. New scores, methods and risk stratification strategies are therefore currently under development and could give completely different results compared to the data and protocols currently in use.
Ethics Approval
This research work is a meta-analysis of published data and does not contain any direct involvement of human participants.
Informed Consent Statement
Not applicable.
Data Availability Statement
All the data retrieved have been included in the manuscript.
Contributors
All the authors defined the intellectual content, conducted literature research, acquired data, and participated in the manuscript preparation, editing and critical review. SZ is the named guarantor.
References
- Chan JF, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 395 (2020): 514-523.
- Coronavirus disease 2019 (COVID-19). Situation Report (2019).
- Zhou P, Yang XL, Wang XG, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579 (2020): 270-273.
- Zhu N, Zhang D, Wang W, et al. A novel coronavirus from patients with pneumonia in China. New England Journal of Medicine 382 (2020): 727-733.
- LiY,HaiTaoZ,JorgeG,et al.A machinelearning-based model for survival prediction in patients with severe COVID-19 infection.MedRxiv (2020): 1-25.
- Chams N, Chams S, Badran R, et al. COVID-19: A Multidisciplinary Review. Front Public Health 8 (2020): 1-20.
- Alizadehsani R, Alizadeh Sani Z, Behjati M, et al. Risk factors prediction, clinical outcomes and mortality in COVID-19 patients. Journal of Medical Virology 93 (2021): 2307-2320.
- National Institutes of Health. COVID-19 Treatment Guidelines. Management of persons with COVID-19. Bethesda, MD NIH (2020).
- Bhardwaj R, Agrawal A. Likelihood ofsurvivalof coronavirus in a respiratorydropletdeposited on a solidsurface. Physics of Fluids 32 (2020): 1-6.
- Ji D, Zhang D, Xu J, et al. Prediction forProgressionRisk in Patients withCOVID-19Pneumonia: The CALLScore. Clinical Infectious Diseases 71 (2020): 1393-1399.
- Myint PK, Sankaran P, Musonda P, et al. Performance of CURB-65 and CURB-age in community-acquired pneumonia. International Journal of Clinical Practice 63 (2009): 1345-1350.
- Patel S. Calculated decisions: PSI/PORT score: pneumonia severity index for community-acquired pneumonia. Emergency Medicine Practice (2021): 23.
- Kostakis I, Smith GB, Prytherch D, et al. Portsmouth Academic Consortium For Investigating COVID-19 (PACIFIC-19). The performance of the National Early Warning Score and National Early Warning Score 2 in hospitalised patients infected by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). Resuscitation 159 (2021): 150-157.
- Myrstad M, Ihle-Hansen H, Tveita AA, et al. National Early Warning Score 2 (NEWS2) on admission predicts severe disease and in hospital mortality from Covid-19 - a prospective cohort study. Scandinavian Journal of Trauma, resuscitation and emergency medicine 28 (2020): 66.
- Gidari A, De Socio GV, Sabbatini S, et al. Predictive value of National Early Warning Score 2 (NEWS2) for intensive care unit admission in patients with SARS CoV-2 infection. Infectious Diseases 52 (2020): 698-704.
- Knight SR, Ho A, Pius R, et al. ISARIC4C investigators. Risk stratification of patients admitted to hospital with covid-19 using the ISARIC WHO Clinical Characterisation Protocol: development and validation of the 4C Mortality Score. British Medical Journal 371 (2020): 1-12.
- Jang JG, Hur J, Hong KS, et al. Prognostic Accuracy of the SIRS, qSOFA, and NEWS for Early Detection of Clinical Deterioration in SARS-CoV-2 Infected Patients. Journal of Korean Medical Science 35 (2020): 234.
- Raith EP, Udy AA, Bailey M, et al. Australian and New Zealand Intensive Care Society (ANZICS) Centre for Outcomes and Resource Evaluation (CORE). Prognostic Accuracy of the SOFA Score, SIRS Criteria, and qSOFA Score for In-Hospital Mortality among Adults with Suspected Infection Admitted to the Intensive Care Unit. JAMA 317 (2017): 290-300.
- Covino M, Sandroni C, Santoro M, et al. Predicting intensive care unit admission and death for COVID-19 patients in the emergency department using early warning scores. Resuscitation 156 (2020): 84-91.
- van Dam PM, Zelis N, Stassen P, et al. Validating the RISE UP score for predicting prognosis in patients with COVID-19 in the emergency department: a retrospective study British Medical Journal Open 11 (2021): 1-7.
- Huang J, Xu Y, Wang B, et al. Risk stratification scores for hospitalization duration and disease progression in moderate and severe patients with COVID-19. BMC Pulmonary Medicine 21 (2021): 120.
- Swets JA, Getty DJ, Pickett RM, et al. Enhancing and evaluating diagnostic accuracy. Medical Decision Making. 11 (1991): 9-18.
- Holten AR, Nore KG, Tveiten CEVWK, et al. Predicting severe COVID-19 in the Emergency Department. Resuscitation Plus 4 (2020): 1-7.