The Use of A Buccal Free Fat Tissue Graft to Enhance Primary Soft Tissue Closure during Socket Preservation and Improve Ridge Contour at the extraction site: Presentation of the Technique, and Report of Case Series
Article Information
Fares Kablan1*, Abir Abu Subeh2, Ofer Moses3
1Department of Oral and Maxillofacial Surgery, Galilee College of Dental Sciences, Gililee Medical Center, Nahariya 2210001, Israel
2Periodontology (CAGS/DScD) Candidate, Boston university Department of Periodontology Massachusetts, USA
3Department of Periodontology and DentalImplantology School of Dental Medicine, Tel Aviv University, Israel
*Corresponding Author: Dr. Fares Kablan, The Galilee Medical Center, Nahariya 2210001, Israel
Received: 17 July 2023; Accepted 26 July 2023; Published: 18 August 2023
Citation: Fares Kablan, Abir Abu Subeh, Ofer Moses. The use of a buccal free fat tissue graft to enhance primary soft tissue closure during socket preservation and improve ridge contour at the extraction site: Presentation of the Technique, and Report of Case Series. Dental Research and Oral Health. 6 (2023): 40-51.
View / Download Pdf Share at FacebookAbstract
Objectives: The aim of this clinical case series is to present a new technique that utilizes a buccal free fat tissue graft (BFFG) harvested from the buccal fat pad (BFP) for socket preservation, and provides primary closure and socket sealing at the extraction site.
Materials and Methods: Twelve patients (9 women, 3 men; mean age 37) with 28 extraction sites were treated using BFFG for socket preservation and were followedup over 12-60 months post operatively. Ten patients received 22 implants in 25 treated sockets, and 2 patients were treated by conventional fixed partial dentures over 3 treated sockets. BFFG was placed over different bone grafting materials in fresh extraction sockets without the use of a membrane. Patients were examined clinically and radiographically at 2weeks, 4weeks, and at 2 months and 4 months post procedure. Computed tomography was performed after 4 months to evaluate the dimensions of the osseous tissue in the treated sites. Implants were placed 4-5 months post operatively.
Results: Healing following BFFG grafting was uneventful, with minimal morbidity. Follow-up revealed preservation of socket volume compared to the original dimensions before extraction. Soft tissue healing displayed a perfect color match to the surrounding tissue.
Conclusions: Harvesting BFFG from BFP is a simple procedure with only minor complications that can be used to enhance primary soft tissue closure of an extraction site. This technique improves the development of long-term ridge contour and soft tissue thickness, and the BFFG blends with the neighboring attached gingiva.
Keywords
Extraction site, Socket preservation, Free fat graft, Buccal fat pad, Soft tissue grafts, Soft tissue management
Extraction site articles; Socket preservation articles; Free fat graft articles; Buccal fat pad articles; Soft tissue grafts articles; Soft tissue management articles
Extraction site articles Extraction site Research articles Extraction site review articles Extraction site PubMed articles Extraction site PubMed Central articles Extraction site 2023 articles Extraction site 2024 articles Extraction site Scopus articles Extraction site impact factor journals Extraction site Scopus journals Extraction site PubMed journals Extraction site medical journals Extraction site free journals Extraction site best journals Extraction site top journals Extraction site free medical journals Extraction site famous journals Extraction site Google Scholar indexed journals Socket preservation articles Socket preservation Research articles Socket preservation review articles Socket preservation PubMed articles Socket preservation PubMed Central articles Socket preservation 2023 articles Socket preservation 2024 articles Socket preservation Scopus articles Socket preservation impact factor journals Socket preservation Scopus journals Socket preservation PubMed journals Socket preservation medical journals Socket preservation free journals Socket preservation best journals Socket preservation top journals Socket preservation free medical journals Socket preservation famous journals Socket preservation Google Scholar indexed journals Free fat graft articles Free fat graft Research articles Free fat graft review articles Free fat graft PubMed articles Free fat graft PubMed Central articles Free fat graft 2023 articles Free fat graft 2024 articles Free fat graft Scopus articles Free fat graft impact factor journals Free fat graft Scopus journals Free fat graft PubMed journals Free fat graft medical journals Free fat graft free journals Free fat graft best journals Free fat graft top journals Free fat graft free medical journals Free fat graft famous journals Free fat graft Google Scholar indexed journals Buccal fat pad articles Buccal fat pad Research articles Buccal fat pad review articles Buccal fat pad PubMed articles Buccal fat pad PubMed Central articles Buccal fat pad 2023 articles Buccal fat pad 2024 articles Buccal fat pad Scopus articles Buccal fat pad impact factor journals Buccal fat pad Scopus journals Buccal fat pad PubMed journals Buccal fat pad medical journals Buccal fat pad free journals Buccal fat pad best journals Buccal fat pad top journals Buccal fat pad free medical journals Buccal fat pad famous journals Buccal fat pad Google Scholar indexed journals Soft tissue grafts articles Soft tissue grafts Research articles Soft tissue grafts review articles Soft tissue grafts PubMed articles Soft tissue grafts PubMed Central articles Soft tissue grafts 2023 articles Soft tissue grafts 2024 articles Soft tissue grafts Scopus articles Soft tissue grafts impact factor journals Soft tissue grafts Scopus journals Soft tissue grafts PubMed journals Soft tissue grafts medical journals Soft tissue grafts free journals Soft tissue grafts best journals Soft tissue grafts top journals Soft tissue grafts free medical journals Soft tissue grafts famous journals Soft tissue grafts Google Scholar indexed journals Soft tissue management articles Soft tissue management Research articles Soft tissue management review articles Soft tissue management PubMed articles Soft tissue management PubMed Central articles Soft tissue management 2023 articles Soft tissue management 2024 articles Soft tissue management Scopus articles Soft tissue management impact factor journals Soft tissue management Scopus journals Soft tissue management PubMed journals Soft tissue management medical journals Soft tissue management free journals Soft tissue management best journals Soft tissue management top journals Soft tissue management free medical journals Soft tissue management famous journals Soft tissue management Google Scholar indexed journals perio-endo lesions articles perio-endo lesions Research articles perio-endo lesions review articles perio-endo lesions PubMed articles perio-endo lesions PubMed Central articles perio-endo lesions 2023 articles perio-endo lesions 2024 articles perio-endo lesions Scopus articles perio-endo lesions impact factor journals perio-endo lesions Scopus journals perio-endo lesions PubMed journals perio-endo lesions medical journals perio-endo lesions free journals perio-endo lesions best journals perio-endo lesions top journals perio-endo lesions free medical journals perio-endo lesions famous journals perio-endo lesions Google Scholar indexed journals tooth extraction articles tooth extraction Research articles tooth extraction review articles tooth extraction PubMed articles tooth extraction PubMed Central articles tooth extraction 2023 articles tooth extraction 2024 articles tooth extraction Scopus articles tooth extraction impact factor journals tooth extraction Scopus journals tooth extraction PubMed journals tooth extraction medical journals tooth extraction free journals tooth extraction best journals tooth extraction top journals tooth extraction free medical journals tooth extraction famous journals tooth extraction Google Scholar indexed journals dental implants articles dental implants Research articles dental implants review articles dental implants PubMed articles dental implants PubMed Central articles dental implants 2023 articles dental implants 2024 articles dental implants Scopus articles dental implants impact factor journals dental implants Scopus journals dental implants PubMed journals dental implants medical journals dental implants free journals dental implants best journals dental implants top journals dental implants free medical journals dental implants famous journals dental implants Google Scholar indexed journals
Article Details
Abbreviations
BFP; Buccal Fat Pad
FFG: Free Fat Graft
PBFPF: Pedicle Buccal Fat Pad Flap
BFFG: Buccal Free Fat Graft
1. Introduction
The decrease in hard and soft tissue associated with the physiological healing process following tooth extraction may lead to ridge contour deformation, and jeopardize potential treatments using dental implants or conventional prostheses [1-4]. The indications for tooth extraction are varied, and include severe periodontal disease, root fracture, and advanced perio-endo lesions. Most of these situations lead to bone destruction and soft tissue deficit. Socket preservation is a procedure designed to maintain or enlarge the post extraction socket volume, increase bone formation, and prevent soft tissue collapse [5-8]. There are a number of bone substitute materials that can be used to graft an extraction site [9-12], and various soft tissue techniques and materials may be employed to close and seal the socket. A variety of intraoral donor sites including the buccal fat pad are commonly used for soft tissue augmentation [13-20]. The use of a pedicled buccal fat pad flap (PBFPF) as a graft for intraoral defects has become a common procedure since its first publication by Egyedi in 1977 [20]. Reports of using this flap for closure of intraoral defects have been encouraging. The success of the PBFPF has been attributed to the simplicity of the procedure, the rich vascular supply, minor donor site morbidity, and fast epithelialization over 3 to 6 weeks [21-24]. Minor complications associated with PBFPF include distant dehiscence and necrosis, restrictions to mouth opening, mild obliteration of the vestibule, and problems of trans location on through dentate areas that may compromise blood supply. There may also be difficulties with large defects and lesions in the anterior regions of the oral cavity [21].
The use of autogenous fat as a free graft is a common technique in general cosmetic surgery [25], and the long term clinical behavior, characteristics, and healing process are well known in this field of medicine. Fibrosis is considered the main healing mechanism of such autologous free fat grafts (FFGs) [26]. A review of dental and maxillofacial surgery literature reveals only a few publications concerning the use of BFFGs. Neder reported the use of BFFG for oral lesion reconstruction in two patients [27]. Later, Kablan and Laster were the first to report the clinical and histological healing stages of a BFFG, which was used to cover bone augmentation in order to obtain and maintain primary closure [28,29]. Kablan described a case series involving the use of BFFG in the treatment of peri-implantitis [30]. The results indicated that, the use of BFFG improved the clinical attachment level of soft tissue around the affected implants and promoted survival, with excellent functional and esthetic outcomes of the treated implants. A subsequent report by Kablan described the use of BFFG in the closure of defects in the hard palate, and demonstrated the simplicity of harvesting the graft and the good survival as a free graft. This success was confirmed in variety of hard palate defects [31]. A case reported by de Castro, described the use of a BFFG for closure of an oronasal fistula and suggested this technique as a treatment option for some cases of anterior maxillary defects [32]. The current case series study was designed to introduce and evaluate the use of a BFFG as a packing material for bone substitutes grafting of fresh extraction sockets without the use of a barrier membrane.
Patients and methods
The study included patients that were treated over a period of 4 years, and followed up for 1-5 years. After signing an informed consent, a BFFG was used as a coating for particulate bone substitute in a fresh extraction socket, without the use of a barrier membrane. Patients were informed about the innovative treatment modality and alternative treatments. The BFP was surgically exposed to obtain the free fat graft. Following an atraumatic tooth extraction, the fresh sockets were packed with allograft particulate bone; and then a BFFG was positioned to cover the bone graft in the socket. The margins of the BFFG were secured beneath the extraction site flap with 4/0 vicryl by horizontal mattress sutures. Follow-up visits were scheduled for the second and fourth weeks and at 2 and 4 months after surgery. Four months after surgery, treated sites were evaluated clinically, by assessing soft tissue color, ridge contour, volume, and vestibular depth. Bone at the recipient site was assessed radiographically by periapical X-ray and in some cases by cone beam computer tomography (CBCT). Dental implants were placed in the majority of the treated sites at 4 to 5 months post extraction: 22 implants were inserted in 25 extracted-grafted sites. Patients were then referred back to their dentist for prosthetic rehabilitation. Following completion of the prosthetic work, treated sites were periodically evaluated clinically using esthetic and functional parameters such as; ridge volume and contour, and soft tissue architecture and color. The Marginal bone levels around the implants were evaluated by periapical X-ray images.
|
Patients |
Gender |
Age |
Teeth |
Number of sockets |
Implants |
Follow-up months |
|
1 |
F |
58 |
24,25 |
2 |
2 |
60 |
|
2 |
M |
56 |
11, 21 |
2 |
2 |
60 |
|
3 |
F |
47 |
14,15 |
5 |
5 |
36 |
|
4 |
F |
42 |
21 |
1 |
0* |
58 |
|
5 |
F |
44 |
21 |
1 |
1 |
51 |
|
6 |
F |
51 |
22-11 |
3 |
2 |
24 |
|
7 |
F |
44 |
12-21 |
3 |
2 |
42 |
|
8 |
F |
38 |
26 |
1 |
0* |
42 |
|
9 |
M |
51 |
43,22 |
2 |
2 |
40 |
|
10 |
M |
46 |
12,11 |
2 |
2 |
52 |
|
11 |
F |
28 |
45,47 |
2 |
2 |
49 |
|
12 |
F |
21 |
12,11,21,22 |
4 |
2 |
28 |
*Conventional bridge
Table 1: Patients and treated sites (teeth), implants, rehabilitation and follow- up.
Socket volume was evaluated by two ways;
- Socket measurement by CBCT; Planmeca Romexis software (Planmeca ProMax Helsinki Finland), before and 4 months after the surgery (Figure 1a and 1b).
- Images. DICOM files obtained by CBCT were exported to professional segmentation software (D2P, 3D systems), and regions of interest (the socket and defect area and augmented bone area) were segmented and converted to 3D design software(Geomagic Free Form plus) in order to qualify the volume (Figure 1c-1d).
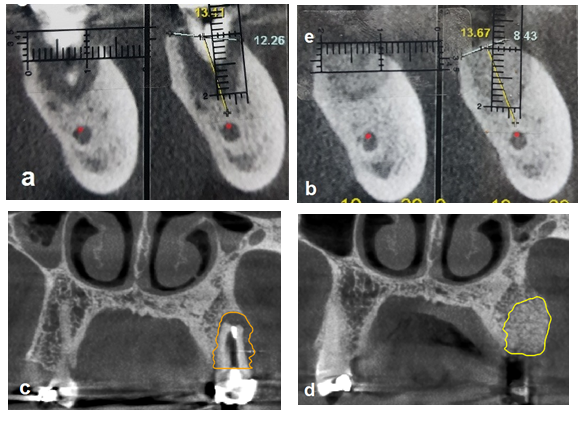
Figure 1: Socket volume
Figure 1a and 1b: Bone dimensions measured by CBCT before, and 4 months after the surgery; Figure 1c and 1d: Socket volume measurements obtained by D2p, 3D systems using DICOM - CBCT before and 4 months after the surgery.
BFFG Harvesting Technique
The donor site
The BFFG was harvested from the BFP (Figure 2), which was accessed through a small horizontal incision in the free mucosa above the second and third maxillary molars (Figure 2a). The fat tissue was reached and easily transformed to the oral cavity by progressive blunt dissection (Figure 2b). Once sufficient BFFG had been harvested ([Figure 2c), the base of the BFP was pushed back into place, and the incision was sutured (figure 2d).
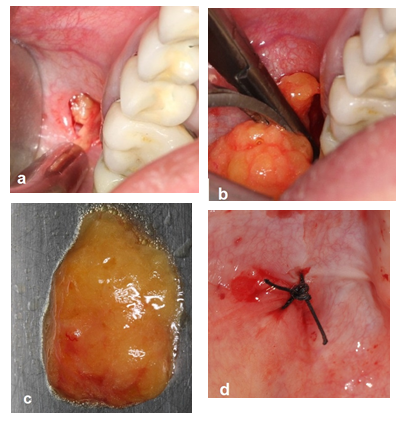
Figure 2: Harvest of the BFFG.
Figure 2a: Small horizontal incision above the second and third maxillary molars, the fat tissue is accessed by blunt dissection; Figure 2b: The fat tissue is easily mobilized to the oral cavity and the desired fat tissue volume is harvested; Figure 2c: The BFFG; Figure 2d: Suturing the donor site incision.
Case description
This case had a poor prognosis for the upper two centrals teeth, and the left lateral incisor (Figures 3a and 3b), which were scheduled for extraction and replacement with dental implants. The teeth were gently removed while preserving the soft and hard tissues, followed by curettage of soft tissue remnants and lesions within the socket (Figure 3c). A minimal envelop flap of 2-4 mm was elevated at both the buccal and the palatal sides to allow fixation of a BFFG in the recipient site (Figure 3d). No internal periosteal releasing incisions were attempted. The sockets were filled with allogenic particulate bone substitute, and sculpted to replicate the previous architecture of the ridge (Figure3e). The BFFG (Figure 3f) was harvested from the right BFP, and its size was adjusted to the dimensions of the extraction site. The BFFG was spread over the recipient site directly over the bone particles (Figure 3g), and then secured with two horizontal mattress sutures in the inner aspect of the flap in the buccal aspect (mesial and distal), and another two in the lingual/ palatal aspect (mesial and distal), followed by interrupted sutures from the buccal side through the BFFG to the lingual side to provide complete closure of the flap (Figure 3h). The use of the BFFG was primarily designed to seal the fresh socket and to secure the bone particles in order to prevent exfoliation of the graft material.
This technique enables tension free closure of the extraction site, and simultaneous augmentation of the soft and hard tissue. The BFFG was left partially exposed to the oral cavity. The patient was prescribed an antibiotic regimen for 7 days and postoperative oral hygiene instructions included mouth rinsing twice daily with chlorhexidine 0.12 for 2 weeks followed by topical application of chlorhexidine gel at the surgical site for an additional 2 weeks. Healing was uneventful, with BFFG visible in the recipient site without dehiscence of the wound at the 2 week follow up visit (Figure 3i). Thereafter the patients were examined once a month for 4 months (Figure 3j). CBCT was performed 4 months after augmentation (Figure 3k), two implants were inserted and two healing abutments were immediately engaged (Figure 3l and 3m). The final restoration was completed 3 months later (Figure 3n). The site was carefully followed for 42 months in order to demonstrate the stability of the soft tissue (Figure 3n).
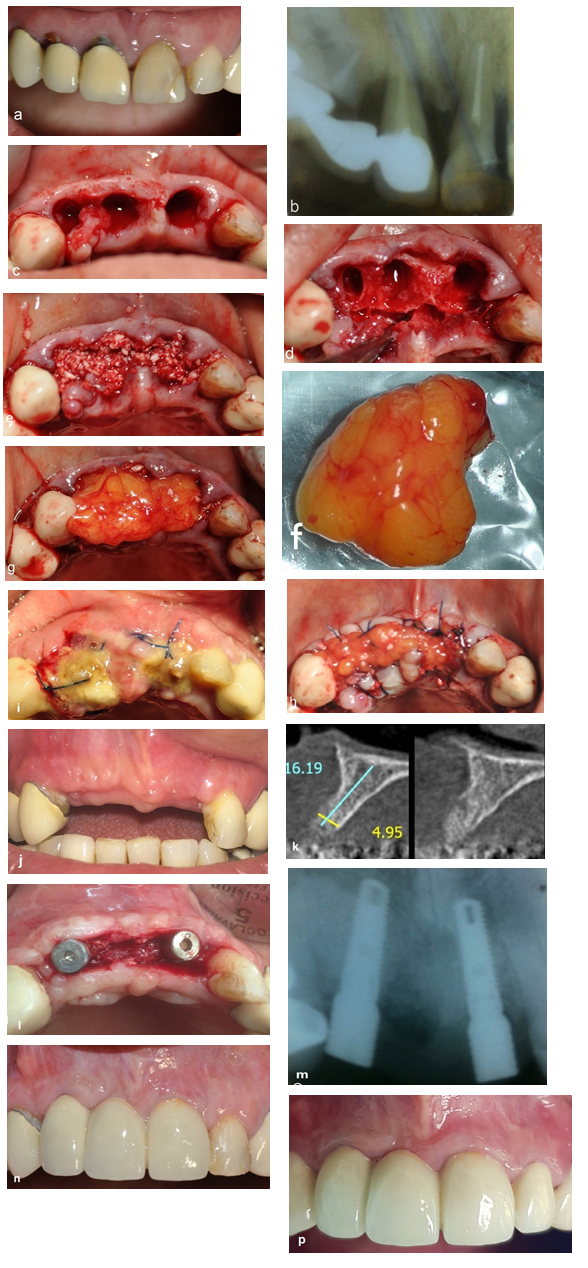
Figure 3: Socket preservation with BFFG. Figure 3a and 3b: Clinical and radiographic views; Figure 3c: Gentle extractions of three anterior maxillary teeth; Figure 3d: Elevation of a minimal buccal, and palatal flap; Figure 3e: Sockets grafted with particulate bone substitute; Figure 3f: The BFFG; Figure 3g: The BFFG is placed over the bone-grafted sockets; Figure 3h: Suturing of the BFFG at the recipient site, the sockets are sealed with partially exposed BFFG; Figure 3i: Follow-up at 2 weeks post- surgery: the BFFG is still visible in the recipient site without wound dehiscence; Figure 3j: Clinical view 4 months after the surgery; Figure 3k: CBCT view 4 months after the surgery; Figure 3l and 3m: Reentry at 4 months and implant placement; Figure 3n: Fixed prosthesis over the implants; Figure 3p: Situation at 42 months follow up.
Case 1
A 58-year-old woman was referred for extraction of her first and second left maxillary premolars (Figure 4a) followed by insertion of two implants. This was accomplished by a two stage approach. After obtaining written informed consent, the first stage involved the extraction of the two premolars and preservation of the sockets. Following atraumatic extraction of the teeth (Figure 4b), the sockets were grafted with particulate allograft bone substitute and packed with BFFG harvested from the left BFP. This serves as primary closure of the treated site and prevents loss of bone particles from the grafted socket. The BFFG was easily spread over the augmentation site, and secured by sutures (Figure 4c). Healing over the next 4 months of follow-up was uneventful. A clinical evaluation of the recipient site 4 months after the surgery revealed a good ridge contour with adequate volumes of hard and soft tissue (Figure 4d). CBCT imaging demonstrated osseous dimensions that were suitable for implant placement (Figures 4e and 4f) and accordingly, two implants (3.75mm diameter, and 13 and 16 mm in length) respectively were inserted (Figure 4g). Implants exposure 4 months after their insertion revealed thick soft tissue, good bone volume, and a successful osseointegration of the implants (Figure 4h). The patient was referred to her dentist for implant borne prosthetic reconstruction. The final esthetic and functional outcomes were satisfactory (Figure 4i and Figure 4j). This patient was followed for 60 months (Figure k).
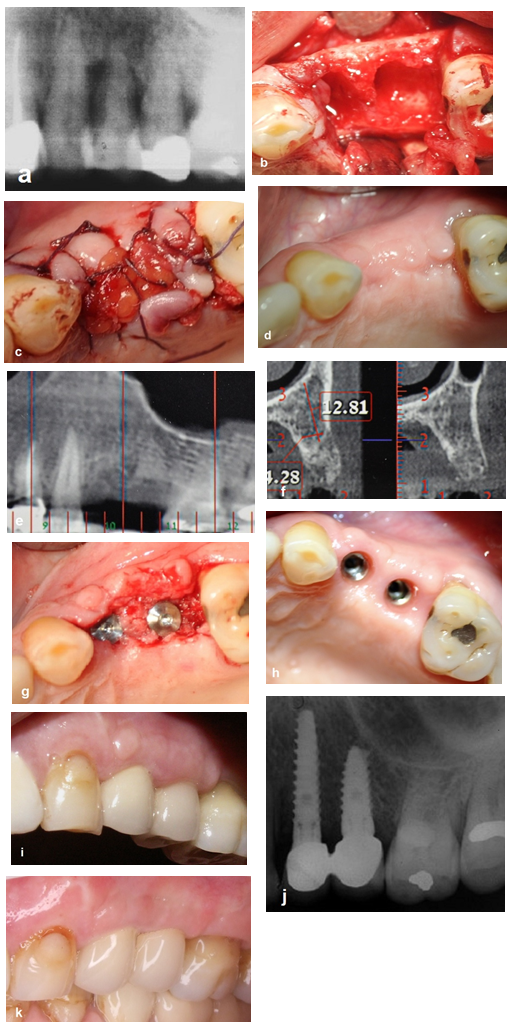
Figure 4: Case 1
Figure 4a: Radiographic view; Figure 4b: The extraction sites; Figure 4c: The BFFG can be readily spread over the sockets, and sutured to seal the sockets; Figure 4d: Follow- up at 4 months post-surgery; Figure 4g: Reentry, and placement of 2 implants with good soft tissue volume; Figure 4h: Follow-up 4 months after placement of the implants, thick soft tissue can be seen around the implants with an excellent color match; Figure 4i and 4j: Follow-up 12 months post- surgery; clinical and radiographic views; Figure 4k: Follow-up 60 months post -surgery; excellent ridge contour and color match, and stable outcomes.
Case 2
A 44-year-old woman, with high esthetic demands was referred for extraction of her left maxillary central tooth (#21) (Figures 5a and 5b). Since the patient presented with a high smile line, a meticulous treatment plan was needed with respect to the exact shape and size of the tooth to be extracted. An esthetic temporary bridge over the maxillary incisors, including a pontic over the extracted tooth, was planned for the healing period of bone grafting of the socket and simultaneous BFFG. The treatment sequence included prefabrication of an acrylic temporary bridge, and preparation of teeth 22, 11, and 12. The next step involved the extraction of the submerged root (Figures 5c), followed by grafting the extraction site with bone particles (Figure 5d). The BFFG was harvested from the left BFP, and used to seal the socket (Figure 5e). A temporary bridge was cemented immediately following BFFG suturing (Figure 5f). After 4 months, a full ceramic bridge was placed with satisfactory results (Figure 5g). Follow up at 60 months, revealed stability of the esthetic results (Figure 5h and Figure 5i).
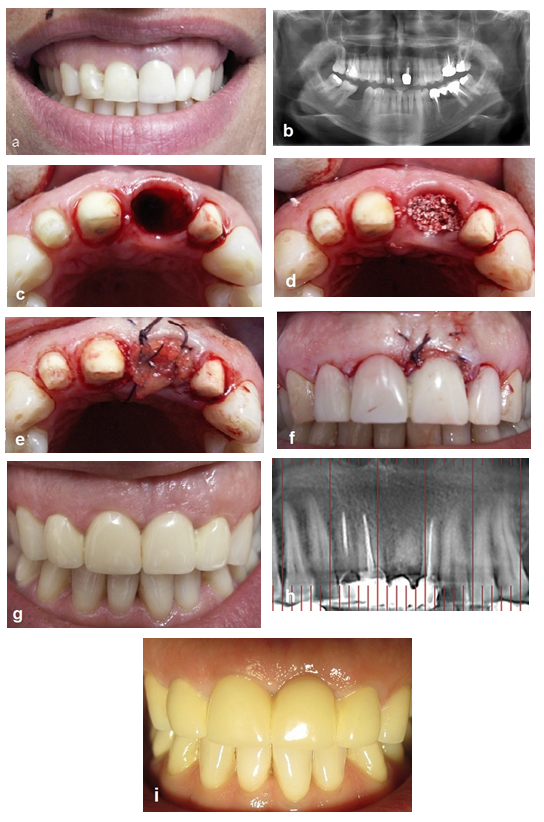
Figure 5: Case 2
Figure 5a and 5b: Clinical and Radiographic View; Figure 5c: Atraumatic extraction; Figure 5d: Grafting of the socket; Figure 5e: Soft tissue augmentation and socket seal by the BFFG; Figure 5f: Cementation of the temporary bridge immediately after suturing of the BFFG at the recipient site; Figure 5g: Follow up 12 months post- surgery; Figure 5h: Follow up 60 months post - surgery, radiographic view; Figure 5i: Follow up 60 months post- surgery.
Postoperative instructions
Patients were informed about the importance of strict adherence to instructions that included consumption of a soft diet for two weeks, a carful tooth brushing to avoid surgical area, and mouth rinsing with chlorhexidine digluconate 0.2% twice daily for two weeks. Amoxycillin 500mg was prescribed every 8 h for 7 days. This was replaced by clindamycin 300 mg every 8 h for 7 days for patients who are allergic to penicillin. Sutures were removed 14 days post operatively. Follow-up visits were scheduled every 2 to 4 weeks for 4 months.
Results
Twenty-eight extraction sites in 12 patients were treated using BFFGs for socket preservation. Clinically, the healing process at both donor and recipient sites was completed uneventful in all cases. The BFP healed very well without any cosmetic compromise. Sings of epithelialization at the grafted area were visible from the second week in all patients and there was complete cover at 4 weeks post-surgery. There was no dehiscence of the wound, and particulate bone grafts remained in place within the sockets without migration or loss of the preserved volume. Long term follow up demonstrated excellent ridge contour of the treated extraction sites with a good color match. Radiographs obtained after the surgery demonstrated that the packed sockets maintained the initial volume at the surgery. The 22 implants inserted in this study had good length and diameter, and thick soft tissue. Two grafted sites employed pontics in conjunction with conventional crown and bridge work. Follow-up of these implants revealed thick peri-implant attached gingiva with satisfactory esthetic and functional rehabilitation outcomes. The followup period was 12-60 months (average 43 months).
Discussion
Most teeth that require extraction have compromised hard and soft tissue quality and volume, and a localized ridge deformity which may be particularly severe in the buccal alveolar of bone damaged either by disease or the trauma of extraction. This deformity is usually clinically significant and the difficulties created for conventional bridge or implant placement may become esthetically problematic. Grafting in a fresh socket in order to enhance the esthetics is therefore recommended for the relevant areas. Accordingly, the present study examined the effects of preserving alveolar ridge dimensions by using BFFG to cover a particulate bone graft packed in fresh extraction sockets, without the use of barrier membrane. The BFP has been extensively used as a pedicle flap (PBFPF) in oral and maxillofacial reconstruction procedures since its first publication in 1977, and its wide applications are well documented in the literature. The predictable outcomes, the ease of graft harvest, and the low rate of complications make the PBFPG an attractive flap to close small to medium sized lesions in the posterior regions of the oral cavity [20,21]. Graft healing has been widely investigated, and mainly occurs by fibrosis and fast epithelialization [22,24]. During the last 10 years, the PBFPG has become a popular method for covering different bone grafts in the posterior maxilla [33,34]. The two cited studies reported the use of PBFPG to cover the window in the lateral wall of the sinus during maxillary sinus bone augmentation. The authors concluded that a PBFPG might be a substitute for resorbable barrier membranes. Liversedge et al. noted that the PBFPG protected maxillary bone grafts, and suggested that this autograft may be left exposed to the oral cavity without any risk of infection [35]. The main disadvantage of this flap is that it cannot reach the anterior regions of the oral cavity, and its use is therefore limited to the posterior oral areas [33-35]. The use of an autologous free fat graft to correct contour deformities and to enhance the volume of the recipient sites is very familiar from cosmetic surgery [25,26]. Following several years of using free fat grafts in various clinical applications in the maxillofacial field, it is now established that fat tissue from the BFP can survive and heal well, and can therefore serve as an excellent tissue graft for various defects in the oral cavity [27-32]. The author (FK) was the first to investigate and report the clinical and histologic healing process of a BFFG after maxillofacial surgery. BFFG was shown to heal by fast epithelialization of the exposed regions and simultaneous fibrosis of the graft that proceeds from immature fibrosis to full maturation after 4 months [28,29].
Kablan and Laster discussed the disadvantages and limitations of a pedicled BFP as compared to the BFFG [28,29]. According to their experience, the use of a PBFPF presents certain limitations that the use of BFFG as a free graft in the oral cavity avoids. The required dimensions of the BFFG are much smaller than those of the PBFPG. Another justification for the use of BFFG is that there is no restriction to mouth opening after the surgery as frequently occurs when using the PBFPG. Another important difference is that in contrast to a PBFPG, the use of BFFG maintains the vestibular depth with no risk of dental injury to the graft in full arch patients. The main advantages of the BFFG are therefore that there are no anatomical limitations following surgery and that the BFFG can be used in any location of the oral cavity. Kablan and Laster reported the clinical and histological healing staging of the BFFG [28,29]. BFFG has been reported to enhance primary soft tissue closure of augmented bone and to improve the thickness of the soft tissue at the receptor sites when used to cover the augmented bone and obtain and maintain primary soft tissue closure. Kablan reported a case series describing the use of BFFG in the treatment of peri-implantitis [30]. The BFFG improved the clinical attachment of soft tissue around the affected implants and prolonged their survival, with excellent functional and esthetic outcomes of the treated implants. In addition, the fibrotic healing of the BFFG inhibits the recurrence of peri-implant lesions. A year later, Kablan described the use of the BFFG in closure of defects in the hard palate and demonstrated the simplicity of the graft and its ability to survive free transfer. The BFFG successfully covered a variety of hard palate defects [31]. As an alternative, De Castro et al described the use of FFG for closure of oronasal fistula and suggested it as a treatment option for certain anterior maxillary defects [32]. Another recent study reported the use of BFFG for treatment of gingival recessions at various sites in both maxillary and mandibular teeth. A BFFG may represent an option for the treatment of gingival recessions as evidenced by the support thinning and recessed gingiva around exposed teeth in 17 patients. The results of this study emphasized that the major benefit of this treatment modality is the applicability for the anterior maxillary teeth and all the mandibular dentition [36]. The conclusion was that the long-term stability of the exposed teeth coverage obtained makes the BFFG a good choice and an excellent option for the treatment of gingival recessions. Our current study introduces an additional clinical indication since the BFFG was used to cover, pack, and seal fresh extraction sockets without the use of a barrier membrane, and with the fat graft left partially exposed to the oral cavity. The ease of use at the recipient site, and the possibility of secure suturing to the recipient bed produce stable graft with no healing issues noted during the follow up period of up to 5 years. We can therefore conclude that the BFFG represent an excellent and reliable option for covering bone grafts during socket preservation. The clinical healing process was similar to the process reported previously by the author [28-31]. The follow-up revealed consistent healing features characterized by graft epithelialization even at the second week after the operation. This epithelialization started from the borders of the graft at the interface with the recipient site soft tissue. There was no bone graft particle leakage or wound dehiscence observed. The BFFG was completely epithelialized by 4 to 6 weeks after surgery, and the color of the recipient resembled that of the surrounding tissue by the 3-4 month time point. At this stage we previously demonstrated histologically that the BFFG is covered with oral epithelium after the completion of healing and contains fibrotic tissue. These findings may suggest that the BFFG induces rapid formation of epithelium over the socket. The successful treatment outcomes in this case series were maintained throughout the long follow-up period ranging from 2 to 5 years. Our results indicate that the BFFG provides two important functions in the preserved fresh sockets; the first is to provide autologous soft tissue that augments the soft tissue volume of the extraction site, and the second is to pack the particulate bone graft material in the socket and prevent exfoliation. The unique advantage of using BFFG lies in the fibrotic healing of this graft that provides the long term stability of tissue observed at the recipient site. The outcomes from utilizing the BFFG challenged in the present study were highly satisfactory, and demonstrate predictable results of using this graft for a variety of indications requiring soft tissue grafting in the oral cavity.
Conclusions
Harvesting of FFG from a BFP is a simple procedure with minor complications, and the graft is readily manipulated. The BFFG may be used obtain primary soft tissue closure of fresh extraction socket. The fibrous healing of the graft improves the long-term ridge contour and soft tissue thickness, and mimics the attached gingiva. The ability of the BFFG to survive and the similarity of the healing to that of pediculated BFP enables the use as free graft. The major benefits of the BFFG, with the possibility of use in any region in both jaws, and multiple applications in the entire oral cavity, provide this technique with a promising future in maxillofacial surgery.
Author contributions
Conceptualization, Surgeries and follow- up, F.K.; writing A.S.; Review& editing F.K. and O.M.
Acknowledgment
Dr. Zoabi Adeeb; for his assessment in socket volume measurements.
Funding
This study received no external fungings.
Conflicts of interest
The authors declare no conflict of interest
References
- Schropp L, Wenzel A, Kostopoulos L, et al. Bone healing and soft tissue contour changes following single- tooth extraction: A clinical and radiographic 12-month prospective study. Int J Periodontics Restorative Dent 23 (2003): 313-323.
- Mecall RA, Rosenfeld AL. Influence of residual ridge resorption patterns on implant fixture placement and tooth position. 1. Int J Periodontics Restorative Dent 11 (1991): 8.
- Mecall RA, Rosenfeld AL. Influence of residual ridge resorption patterns on implant fixture placement and tooth position. 2. Presurgical determination of prosthesis type and design. Int J Periodontics Restorative Dent 12 (1992): 32.
- Van der Weijden F, Dell'Acqua F, Slot DE. Alveolar bone dimensional changes of post-extraction sockets in humans: A systematic review. J Clin Periodont 36 (2009): 1048-1058.
- Lekov V, Kenney EB, Weinlaender M et al. A bone regenerative approach to alveolar ridge maintenance following tooth extraction.Report of 10 cases. J Periodontol 68 (1997): 563.
- Werbitt MJ, Goldberg PV. Immediate implantation. Preservation of bone volume and osseous regeneration. J Periodontol 10 (1991): 157.
- Nemcovsky CE, Serfaty V. Alveolar ridge preservation following extraction of maxillary anterior teeth. Report of 23 consecutive cases. J Periodontol 67 (1996): 390.
- Lasella JM, Greenwell H, Miller RL, et al. Ridge preservation with freeze-dried bone allograft and collagen membrane compared to extraction alone for implant site development: A clinical and histologic study in humans. J Clin Periodontol 74 (2003): 990-999.
- Artzi Z, Tal H, Dayan D: Porous bovine bone mineral in healing of human extraction sockets. Part I: Histomorphometric evaluations at 9 months. J Periodontol 71 (2000):10-15.
- Froum S, Cho SC, Rosenberg E, et al. Histological comparison of healing extraction sockets implanted with bioactive glass or demineralized freeze-dried bone allograft: A pilot study. J Periodontol 73 (2002): 94.
- Carmagnola D, Adriaens P, Berglundh T. Healing of human extraction sockets filled with Bio-oss. Clin Oral Implants Res 14 (2003): 137-143.
- Org'eas GV, Clementini M, Risi VD, et al. Surgical techniques for alveolar socket preservation: A systematic review. Int J Oral Maxillofac Implants 28 (2013): 1049-1061.
- Mardinger O, Chaushu G, Ghelfan O, et al. Intrasocket reactive soft tissue for primary closure after augmentation of extraction sites with severe bone loss before implant placement. J Oral Maxillofac Surg 67 (2009): 1294-1299.
- Mardinger O, Vered M, Chaushu, et al. Histomorphometrical analysis following augmentation of infected extraction sites exhibiting severe bone loss and primarily closed by intrasocket reactive soft tissue. Clin Implant Dent Relat Res 14 (2012): 359-365.
- Tal H. Autogeneous masticatory mucosal grafts in extraction socket seal procedures; a comparison between sockets grafted with demineralized freeze-dried bone and deproteinized bovine bone materials. Clinical Oral Implants Res. 10 (1999): 289-269.
- Fowler S, Breault LG, Rebitski G. Ridge preservation utilizing an acellular dermal allograft and demineralized freeze-dried bone allograft: Part I. A report of 2 cases. J Periodontol 71 (2000): 1353.
- Lansberg C, Bichacho N. A modified surgical/prosthetic approach for optimal single implant supported crown. Part 1- the socket seal surgery. Practical Periodontics and Aesthetic Dentistry 6 (1994): 11-17.
- Nemcovsky CE, Artzi Z, Moses O. Rotated split palatal flap for soft tissue primary coverage over extraction sites with immediate implant placement. Description of the surgical procedure and clinical results. J Periodontol 70 (1999): 926.
- Tal H, Bichacho N, Kornowski Y, et al. Rotated palatal flaps: A functional and aesthetic solution in endentulous sites. Pract Proced Aesthet Dent 16 (2004): 599-606.
- Egyedi P. Utilization of the buccal fat pad for closure of oro-antral and/or oro-nasal communications. J Maxillofac Surg 5 (1977): 241-2414.
- Singh J, Prasad K, Lalitha RM, et al. Buccal pad of fat and its applications in oral and maxillofacial surgery: A review of published literature (February) 2004 to (July) 2009. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 110 (2010): 698-705.
- Tideman H, Bosanquet A, Scott J. Use of the buccal fat pad as a pedicled graft J Oral Maxillofac Surg 44 (1986): 435-440.
- Loh FC, Loh HS. Use of the buccal fat pad for correction of intraoral defects: Report of cases. J Oral Maxillofac Surg 49 (1991): 413-416.
- Martín-Granizo R, Naval L, Costas A, et al. Use of buccal fat pad to repair intraoral defects: Review of 30 cases. Br J Oral Maxillofac Surg 35 (1997): 81-84.
- Shiffan MA (Ed). Autologous fat transfer, Art, science, and clinical practice. Springer-Verlag Berlin Heidelberg (2010); Part I pp. 3-40.
- Nguyen A, Pasyk KA, Bouvier TN, et al. Comparative study of survival of autologous adipose tissue taken and transplanted by different techniques. Plast Reconstr Surg 85 (1990): 378-86.
- Neder A. Use of buccal fat pad for graft. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 55 (1983): 349-350.
- Kablan F, Laster Z. The use of free fat tissue transfer from the buccal fat pad to obtain and maintain primary closure and to improve soft tissue thickness at bone-augmented sites: Technique presentation and report of case series. Oral Craniofac Tissue Enj 2 (2012): 282-293.
- Kablan F, Laster Z. The use of free fat tissue transfer from the buccal fat pad to obtain and maintain primary closure and to prove soft tissue thickness at bone-augmented sites: Technique presentation and report of case series. Int J Oral Maxillofac Implants 29 (2014): e220-231.
- Kablan F. The use of buccal free fat graft in regenerative treatment of peri-implantitis; A new and predictable technique. Ann Maxillofac Surg 5 (2015): 178-185.
- Kablan F. The use of buccal fat pad free graft in closure of soft-tissue defects and dehiscence in the hard palate: A new technique. Ann Maxillofac Surg 6 (2016): 241-245.
- De Castro CH, De Souza LN. Fernandes Santos, et al. Use of the buccal fat pad as free graft for closure of oronasal fistula in cleft palate patient. J Craniofac Surg 26 (2015): e14-16.
- Hassani A, Khojasteh A, Alikhasi M. Repair of the perforated sinus membrane with buccal fat pad during sinus augmentation. J Oral Implantol 34 (2008): 330-333.
- Herna'ndez-Alfaro F, Torradeflot MM, Marti C. Prevalence and management of Schneiderian membrane perforations during sinus lift procedures. Clin Oral Immplants Res 19 (2008): 91-98.
- Liversedge RI, Wong K. The use of the buccal fat pad im maxillary and sinus grafting of the severely atrophic maxilla preparatory to implant reconstruction of the partially or completely edentulous patient:technical note. Int J Oral Maxillofac Implants 17 (2002): 424-428.
- Kablan F. The reliability of free buccal fat graft for treatment of severe gingival recessions at mandibular and maxillary exposed roots. Ann Maxillofac Surg 8 (2018): 281-286.
