The Role of Nursing in Ruptured Gastrointestinal Stromal Tumor in Adolescents and Young Adults: A Case Report
Article Information
Riham Saud Alhazmy1, Ayman Baghdadi2*
1Master student in Medical-Surgical Nursing, Jeddah, Kingdom of Saudi Arabia, King Abdulaziz University
2Consultatnt in General Surgery, Rabigh General Hospital, Rabigh city, Kingdom of Saudi Arabia, Minstar of Health
*Corresponding Author: Ayman Baghdadi, Consultatnt in General Surgery, Rabigh General Hospital, Rabigh city, Kingdom of Saudi Arabia, Minstar of Health.
Received: 27 November 2023; Accepted: 08 December 2023; Published: 14 February 2024
Citation: Riham Saud Alhazmy, Ayman Baghdadi. The Role of Nursing in Ruptured Gastrointestinal Stromal Tumor in Adolescents and Young Adults: A Case Report. Archives of Clinical and Medical Case Reports. 8 (2024): 26-29.
View / Download Pdf Share at FacebookAbstract
Gastrointestinal stromal tumors (GISTs) are rare life-threatening forms of cancer representing 0.1%-3% of all gastrointestinal (GI) malignancies. Nursing has become a critical component in handling patients with gastrointestinal tumors. This case report investigates the role of nursing in ruptured GISTs in adolescents and young adults (AYA). It focuses on a 17-year-old female who was admitted to the emergency department (ER) due to the sudden onset of generalized abdominal pain, nausea, and vomiting. After an initial examination, the patient underwent an urgent laparotomy. During this procedure, an unexpected ruptured cystic outgrowth was found originating from the distal ileum. Resection and an anastomosis of the affected section were performed, and a pelvic drain was inserted. GISTs are malignant mesenchymal tumors of the gastrointestinal tract. In rare cases, the tumor may rupture and result in hemoperitoneum; thus, it is challenging for healthcare workers to detect and manage it.
Keywords
Case report; Gastrointestinal stromal tumor; Small intestine; Nursing; Cancer
Case report articles; Gastrointestinal stromal tumor articles; Small intestine articles; Nursing articles; Cancer articles.
Case report articles Case report Research articles Case report review articles Case report PubMed articles Case report PubMed Central articles Case report 2023 articles Case report 2024 articles Case report Scopus articles Case report impact factor journals Case report Scopus journals Case report PubMed journals Case report medical journals Case report free journals Case report best journals Case report top journals Case report free medical journals Case report famous journals Case report Google Scholar indexed journals Syndrome articles Syndrome Research articles Syndrome review articles Syndrome PubMed articles Syndrome PubMed Central articles Syndrome 2023 articles Syndrome 2024 articles Syndrome Scopus articles Syndrome impact factor journals Syndrome Scopus journals Syndrome PubMed journals Syndrome medical journals Syndrome free journals Syndrome best journals Syndrome top journals Syndrome free medical journals Syndrome famous journals Syndrome Google Scholar indexed journals Gastrointestinal stromal tumor articles Gastrointestinal stromal tumor Research articles Gastrointestinal stromal tumor review articles Gastrointestinal stromal tumor PubMed articles Gastrointestinal stromal tumor PubMed Central articles Gastrointestinal stromal tumor 2023 articles Gastrointestinal stromal tumor 2024 articles Gastrointestinal stromal tumor Scopus articles Gastrointestinal stromal tumor impact factor journals Gastrointestinal stromal tumor Scopus journals Gastrointestinal stromal tumor PubMed journals Gastrointestinal stromal tumor medical journals Gastrointestinal stromal tumor free journals Gastrointestinal stromal tumor best journals Gastrointestinal stromal tumor top journals Gastrointestinal stromal tumor free medical journals Gastrointestinal stromal tumor famous journals Gastrointestinal stromal tumor Google Scholar indexed journals tumor articles tumor Research articles tumor review articles tumor PubMed articles tumor PubMed Central articles tumor 2023 articles tumor 2024 articles tumor Scopus articles tumor impact factor journals tumor Scopus journals tumor PubMed journals tumor medical journals tumor free journals tumor best journals tumor top journals tumor free medical journals tumor famous journals tumor Google Scholar indexed journals Small intestine articles Small intestine Research articles Small intestine review articles Small intestine PubMed articles Small intestine PubMed Central articles Small intestine 2023 articles Small intestine 2024 articles Small intestine Scopus articles Small intestine impact factor journals Small intestine Scopus journals Small intestine PubMed journals Small intestine medical journals Small intestine free journals Small intestine best journals Small intestine top journals Small intestine free medical journals Small intestine famous journals Small intestine Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals CT articles CT Research articles CT review articles CT PubMed articles CT PubMed Central articles CT 2023 articles CT 2024 articles CT Scopus articles CT impact factor journals CT Scopus journals CT PubMed journals CT medical journals CT free journals CT best journals CT top journals CT free medical journals CT famous journals CT Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals Sepsis articles Sepsis Research articles Sepsis review articles Sepsis PubMed articles Sepsis PubMed Central articles Sepsis 2023 articles Sepsis 2024 articles Sepsis Scopus articles Sepsis impact factor journals Sepsis Scopus journals Sepsis PubMed journals Sepsis medical journals Sepsis free journals Sepsis best journals Sepsis top journals Sepsis free medical journals Sepsis famous journals Sepsis Google Scholar indexed journals Cancer articles Cancer Research articles Cancer review articles Cancer PubMed articles Cancer PubMed Central articles Cancer 2023 articles Cancer 2024 articles Cancer Scopus articles Cancer impact factor journals Cancer Scopus journals Cancer PubMed journals Cancer medical journals Cancer free journals Cancer best journals Cancer top journals Cancer free medical journals Cancer famous journals Cancer Google Scholar indexed journals
Article Details
Key Clinical Message:
This study describes one of the rare cases that may occur around the world. In this case, we reviewed the sign and symptoms that the patient may present with. In addition to the diagnostic test that may help in early detection, and how to deal with it.
1. Background
Gastrointestinal stromal tumors (GISTs) are typically discovered in the gastrointestinal tract and arise in the interstitial cells of Cajal [1]. The disease mainly affects the stomach (60%-70%) and the small intestines (20%-25%). Its estimated incidence is 10-15 per million [2], with a median age of 65 years at the time of diagnosis. Less than 10% of individuals are diagnosed prior to age 40 [3, 4]. GISTs rarely occur in children and adolescents; they account for only 1.4% to 2.7% of all GIST cases [5]. For the clinical presentation, many GISTs are asymptomatic and identified incidentally. Symptoms depend on the size and location of the tumor [6]. In adolescents and young adults (AYA), some patients have chronic anemia (hemoglobin: <8 g/dl) and associated symptoms such as fatigue and paleness, as well as abdominal pain, vomiting, and abdominal distention [7]. In rare cases, the patient has a ruptured GIST and spontaneous hemoperitoneum, requiring immediate intervention [8]. Adolescents and young adults (AYA) have different characteristics, treatment responses, and psychosocial needs, and these aspects should be addressed in research [9]. Moreover, a ruptured cyst is a life-threatening circumstance that requires immediate attention [10]. However, research related to AYA with GISTs is limited. To fill in this gap in the literature, this case report focuses on ruptured gastrointestinal stromal tumors in AYA from a nursing perspective.
2. Case Presentation
A 17-year-old female arrived in an emergency department (ED) with the sudden onset of generalized abdominal pain. She was experiencing aching; its frequency was intermittent, and its severity was moderate but aggravated by walking. The pain score was 6 out of 10 on the numerical pain scale. She was also experiencing nausea and vomiting, both of which began in the morning. The patient was single, a high school student, and unemployed. She had a history of recent anemia detected in another clinic and was prescribed an iron tablet (100mg/day). However, she stopped taking it six months ago and did not follow-up on her condition. Her vital signs, the body temperature was 37C, blood pressure was 95/60 mmHg, respiratory rate was 25 breaths/min, and the radial pulse was 100 beats/min and regular. She weighed 47 kg, and her height was 156 cm. She did not know her previous weight. During the examination, she was conscious, oriented. The abdominal examination showed generalized abdominal tenderness mainly in the lower abdominal area with guarding with decreased bowel sounds. The patient’s skin was pale and somewhat cold. The early diagnosis for the patient was a ruptured ovarian cyst versus a ruptured viscus.
2.1 Diagnostic test
An abdominal ultrasound showed that the right adnexal soft tissue mass measured 5.5 x 4.5 cm, indicating a mild to moderate free pelvic abdominal turbid collection. Based on the ultrasound, the patient underwent an urgent expletory laparotomy. During the laparotomy, an unexpected ruptured cystic outgrowth was found that originated from the distal ileum (Figure 1). It had an indurated bowel wall area underneath it as well as a moderate amount of blood-free fluid. Consequently, resection and an anastomosis of the affected segment were performed, and a pelvic drain was inserted. The ruptured cyst was sent to the histopathology lab, and its examination revealed a gastrointestinal stromal tumor (GIST) and a mixed tumor of ileum. The tumor size was 6.5 x 3.5 x 2 cm. For the unifocal tumor, the mitotic rate was 36/5 MM2, with a tological grade 2, which is a high grade. The mitotic rate was >5/5MM2 with a risk assessment of high risk. The mucosal resection margins were free of tumors. However, tumor cells were seen on the ruptured cyst’s wall, and the cyst contents indicated pathological stage 3. The lab investigation is shown in (Tale 1) [11].
Table 1: lab Investigation
|
Test |
Result |
Normal range |
|
white blood cell (WBC) |
9.67X10^3/ul |
3.7-10.1X10^3/ul [11] |
|
hemoglobin concentration (HGB) |
5.9g/dl |
12.9-14.2g/dl [11] |
|
Platelet |
708 X10^3/ul |
155-366X10^3/ul [11] |
|
blood urea nitrogen (BUN) |
3 mg/dl |
7-18mg/dl [11] |
|
creatinine level |
0.46mg/dl |
0.55-1.3mg/dl [11] |
|
C reactive |
lower than 6 mg/L |
less than 10 mg/L [11] |
2.2 Treatment
The treatment of the case involved many aspects. In the ER, the patient received intravenous fluids to prevent hypovolemic shock. She was given two units of packed RBCs to correct her hemoglobin level prior to the operation. Intra-operation, because of the ruptured tumor, the hemoperitoneum was managed through laparotomy via resection, an anastomosis, and the placement of a surgical drain. On the first day post-operation, the patient received two units of packed RBCs while in intensive care. To prevent complications related to wound infection, she was given antibiotic prophylaxis–specifically, ceftriaxone 1g, a daily IV for five days, and analgesics including pethidine 50 mg, IM, 12 hours for the first 24 hours and paracetamol 1,000 mg, IV, eight hours for the first seven days. Since the patient was a teenager and had a serious and rare illness, she was provided with good professional psychosocial support from healthcare workers and her family, and this aspect was an important part of her treatment.
2.3 Outcome and Follow-up
The patient had a sudden GIST rupture, surgical intervention was necessary. A multidisciplinary approach was used to achieve optimal care and to reach the desirable outcomes. First, immediately after the operation, the patient was shifted to the intensive care unit (ICU) for close monitoring. The plan was to continue replenishing the blood volume with two units of packed RBCs, but a hypokalemia occurred as a complication of dehydration. It was given intravenous fluids (Dextrose 5% normal saline with 40 mcq of KCL 100ml/hr) for 24 hours. A Foley’s catheter was attached pre-operation to monitor her kidney functions; after 24 hours, the output was 2,400 ml of clear, yellow, and the catheter was disconnected. Thereafter, the patient was moved to the surgical ward to continue her management which included monitoring surgical drain outcomes, which were as follows: 300 ml bloody exudate on the first day, 250 ml serous on the second day, 300 ml serous on the third day, 100 ml serous on the fourth day, 80 ml on the fifth day, 50 ml serous on the sixth day, and less than 20 ml on the seventh day, when the device was disconnected.
The wound dressing was changed on the second and seventh days. The wound was clean, with no signs of infection. The patient was referred to a social worker to give appropriate support to the patient and her family. Another type of medication was mentioned during the treatment part. An abdominal CT scan with contrast was performed on the fourth day to check metastasis. The scan revealed a multiple hepatic focal soiled lesion visible on the right lobe hepatic segment, though bowel thickening was not detected. On the ninth day, the patient was discharged, and no surgical complications were perceived. The patient instructed to follow-up in the tertiary center that specialized in oncology and to have a CT scan every four months for two years.
3. Discussion
In the current case report, we discussed the rare case of ruptured gastrointestinal stromal tumors in adolescents and young adults. Specifically, we detailed the case of a 17-year-old female who was admitted to the ER with simple nausea, vomiting, and generalized abdominal pain. Based on the patient’s history as well as an examination and an ultrasound, the working diagnosis was a ruptured ovarian cyst versus a ruptured viscus. A surgical intervention occurred to manage the hemoperitoneum. Post-surgery, the patient had no complications and was discharged on the ninth day post-operation. To manage the same cause, an experienced multidisciplinary team is necessary. This team should include histopathologists, radiologists, surgeons, and oncologists, as well as gastroenterologists, nuclear medicine specialists, and clinical nurse specialists, who play a vital role.
The role of nursing in GISTs case:
The nursing role starts with the arrival of patients in the ER (Table 2); the symptoms vary depending on the patient, the size of the tumor, and the location of the tumor. Patients may have non-specific symptoms, including upper gastrointestinal bleeding, anemia, abdominal pain/discomfort, and a palpable mass [12]. In some adolescents and young adults (AYA), fatigue and weakness may occur due to iron deficiency anemia. Moreover, if the tumor originates in the intestine, constipation may occur [7].
Table 2: The role of Nursing
|
In emergency department |
|
|
1 |
Immediate application of an intravenous fluid to prevent shock and the observation of the patient’s condition [13]. |
|
2 |
Prepare the patient for diagnostic procedures, such as an abdominal B-ultrasound or a CT scan [13]. |
|
3 |
Prepare for an emergency operation [13]. |
|
Post-operative period |
|
|
1 |
Monitor the circulatory, respiratory and urinary systems of the patient for the early detection of life-threatening complications [14]. |
|
2 |
Monitor a patient’s pain and anxiety levels after surgical procedures [14]. |
|
3 |
Prevent complications related to a compromised immune system as well as hospitalization due to illnesses such as pneumonia [14]. |
|
4 |
Early mobilization and help with the incision treatment [14]. |
|
5 |
Help the patient to restore the body functions such as self-adherence to a diet and medications [14]. |
|
6 |
Monitoring a patient’s behavior [14]. |
|
7 |
Providing a health education seminar [14]. |
|
8 |
Offer appropriate psychosocial support [14]. |
Regarding treatment, based on the literature, the basic method and the best way to manage GISTs is complete surgical resection [10, 15]. Research conducted in the United States on 392 AYA diagnosed with GISTs showed that when 332 (84%) of the AYA population underwent surgical management, their GIST-specific survival (GSS) and overall survival (OS) rates improved [9]. Other research has shown that Imatinib, which is a drug that inhibits the kinase enzyme activity of a Kit, is an effective first-line medical therapy for post-operative therapy, malignant metastasis, and recurrent GISTs [13, 14, 16]. Imatinib improves the survival rate; thus, the median survival rate was seven years, and the lowest survival rate was less than one year [17].
Conclusion
In conclusion, a ruptured GIST in adolescents and young adults is an emergency situation that requires immediate intervention from expert nursing staff and a physician. An active examination, diagnosis, and treatment may help increase the AYA’s chance of survival. Further studies are needed to focus on the risk factors, early detection of the disease, and long-term follow-up.
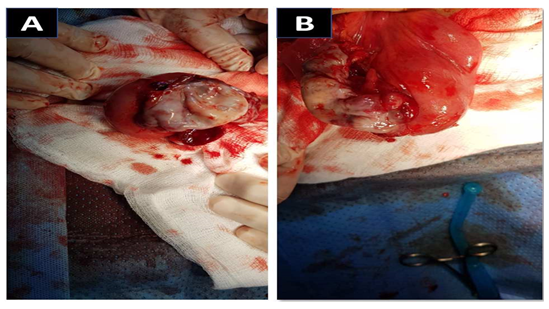
Figure 1(A, B): Ruptured cystic outgrowth from the bowel wall.
Credit contribution
Conceptualization, investigation, project administration, and writing – original Draft preparation: Riham Saud Alhazmy
Investigation, supervision, and writing – review & editing: Ayman Baghdadi.
Consent policy
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
References
- Joensuu H. Gastrointestinal stromal tumor (GIST). Annals of Oncology 17 (2006): 280-286.
- Soreide K, Sandvik O M, Soreide JA, et al. Global epidemiology of gastrointestinal stromal tumours (GIST): A systematic review of population-based cohort studies. Cancer Epidemiology 40 (2016): 39-46.
- Miettinen M, Sobin L H, and Lasota J. Gastrointestinal stromal tumors of the stomach: A clinicopathologic, immunohistochemical, and molecular genetic study of 1,765 cases with long-term follow-up. American Journal of Surgical Pathology 29 (2005): 52-68.
- Nilsson B, Bumming P, Meis-Kindblom JM, et al. Gastrointestinal stromal tumors: The incidence, prevalence, clinical course, and prognostication in the preimatinib mesylate era—A population- based study in western Sweden. Cancer 103 (2005): 821-829.
- Casali PG, and Blay J Y. Gastrointestinal stromal tumours: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Annals of Oncology 21 (2010): 98- 102.
- Cichoz-Lach H, Kasztelan-Szczerbinska B, and Slomka M. Gastrointestinal stromal tumors: epidemiology, clinical picture, diagnosis, prognosis and treatment. Polskie Archiwum Medycyny Wewnetrznej 118 (2008): 216.
- Rink L, and Godwin A K. Clinical and molecular characteristics of gastrointestinal stromal tumors in the pediatric and young adult population. Current Oncology Reports 11 (2009): 314-321.
- Sugawara G, Yamaguchi A, Isogai M, et al. A case of gastrointestinal stromal tumor of the ileum with intraabdominal hemorrhage (in Japanese). Jpn Soc Clin Surg 64 (2003): 3092-3096.
- Fero K E, Coe T M, Fanta P T, et al. Surgical management of adolescents and young adults with gastrointestinal stromal tumors: A US population-based analysis. JAMA Surgery 152 (2017): 443-451.
- Bucher P, Poletti P, Myit S, et al. Spontaneous rupture of a gastrointestinal stromal tumour associated with life-threatening nontraumatic hemoperitoneum. Canadian Journal of Surgery 51 (2008): E38.
- McGhee, Michael F, Caroline A Saxelby, et al. A Guide to Laboratory Investigations. CRC Press (2021).
- Judson I, Bulusu R, Seddon B, et al UK clinical practice guidelines for the management of gastrointestinal stromal tumours (GIST). Clinical Sarcoma Research 7 (2017): 1-10.
- Han L, Shen C, and Tian Y. Clinical treatment and nursing care of gastrointestinal stromal tumor acute abdomen. Journal of Gastroenterology and Hepatology Research 4 (2015): 1821-1825.
- Griffin J M, St Amand M, and Demetri G D. Nursing implications of Imatinib as molecularly targeted therapy for gastrointestinal stromal tumors. Clinical Journal of Oncology Nursing 9 (2005):
- Van der zwan S M, and Dematteo R P. Gastrointestinal stromal tumor: Five years later. Cancer 104 (2005): 1781-1788.
- Cavnar M J, Seier K, Curtin C, et al. Outcome of 1,000 patients with gastrointestinal stromal tumor (GIST) treated by surgery in the pre-and post-Imatinib eras. Annals of Surgery 273 (2021): 128.
- Fauske L, Hompland I, Lorem G, et al. Striving towards normality in daily life: A qualitative study of patients living with metastatic gastrointestinal stromal tumour in long-term clinical remission. Sarcoma 8 (2020): 1814394.
