The Role of Emergency Medicine for Postgraduate Year One Undifferentiated Physician: A Qualitative Analysis of Trainees' Perspective
Article Information
Weide Tsai1, 2*, Ching-Yi Shen1, 2, Chih-Chun Huang1, 3, Chen-Hao Liao1, NaiHui Lin1, Kuan-Chih Kuo1, Chih-Chun Hsu1
1Department of Emergency Medicine, MacKay Memorial Hospital, Taipei, Taiwan
2Department of Medicine, MacKay Medical College, New Taipei City, Taiwan
3Yuanpei University of Medical Technology, Hsinchu, Taiwan
*Corresponding author: Weide Tsai, Department of Emergency Medicine, MacKay Memorial Hospital, Chung-san North Road, Section 2, No 92, Taipei, Taiwan
Received: 05 December 2021; Accepted: 16 December 2021; Published: 03 January 2022
Citation:
Weide Tsai, Ching-Yi Shen, Chih-Chun Huang, Chen-Hao Liao, NaiHui Lin, Kuan-Chih Kuo, Chih-Chun Hsu. The Role of Emergency Medicine for Postgraduate Year One Undifferentiated Physician: A Qualitative Analysis of Trainees' Perspective. Archives of Internal Medicine Research 5 (2022): 005-017.
View / Download Pdf Share at FacebookAbstract
Background: PGY program was initiated in 2003 for undifferentiated physicians in Taiwan, the program aimed to improve physicians’ general competency gap exposed during the SARS epidemic breakout. Many published studies discussed the effectiveness of the program. We were interested in the learning impacts gained from the physicians' perspectives during EM rotation in the PGY program, and little was known regarding this subject.
Methods: This retrospective study used grounded theory data analysis methods. 201 PGY physicians rotated in the emergency department from August 2014 to July 2017 answered three open-ended post-rotation survey questions resulting in a dataset of 603 comments. A three-member team for code develop-ment reviewed all comments and established the code themes with the consensus of the team members. A four-member coding team coded applicable comments accordingly.
Results: We coded 563 (96%) comments and sorted 32 themes essential to characterize the clinical exper-iences into two categories. Twenty-six codes were relevant to professional development; 6 were related to the emotional issue. In the professional develop-ment category, patient care (33%) was the most frequently coded domain in the sub-level of six core competencies, followed by system-based practice (25%) and interpersonal and communication skills (19%). Senses of growth and improvement were the most frequently coded themes in the emotional issue category, followed by pressure at the workplace and on-the-spot-feedback. The top 3 lessons learned by physicians' perception were decision-making, team and patient communication, and prioritizing tasks.
Conclusions: EM rotation had a productive role in professional development for undifferentiated physic-ians before receiving specialty discipline training. Gaining experiences in clinical judgment and communication were the strengths
Keywords
PGY, Undifferentiated Physician, Emergency Medicine Rotation, Professional Development, General Competency Training, Decision-Making, Clinical Judgement, Communication, Physician Perception
PGY articles; Undifferentiated Physician articles; Emergency Medicine Rotation articles; Professional Devel-opment articles; General Competency Training articles; Decision-Making articles; Clinical Judgement articles; Communication articles; Physi-cian Perception articles
Article Details
1. Background
The SARS epidemic outbreak in 2003 exposed a deficiency in the general competency among physicians. In response to this issue, postgraduate-year (PGY) general competency training, also known as the PGY program, was initiated in 2003 nation-wide in Taiwan for all physicians before receiving specialty discipline training. The program's duration was only three months long at the beginning, expanded into six months in 2006, and extended to a one-year term in 2011. A newly revised two-year program was initiated in 2019 as the first class of physicians graduated from a reformed system of six-year term medical schools, aimed to have more integrity of school education and general medicine training for all physicians. This one-year PGY program consisted of clinical rotations in internal medicine, general surgery, pediatrics, obstetrics and gynecology, emergency medicine (EM), community medicine, and elective rotations of other disciplines.
Several studies have published and discussed the achievement of objectives goals assessed through various methods [1-3]. Further research on the effectiveness of specific rotations like community medicine in the program was discussed in the literature [4, 5]. Experience in EM is considered a critical part of medical education [6], EM rotation provides excellent primary care training opportunities by encountering a significant breadth of the patient population and managing a diversity of clinical presentation. Although PGY physicians have EM clerkships, the clerkship experiences vary in rotation block time, total hours worked, shift length, and use of teaching modalities. Not all PGY trainees had the same level of exposure to the primary care experi-ence [7, 8]. The PGY program functions as an enhancement tool filling the insufficiency gap of the primary care training in clerkship. One study showed that PGY physicians' performance scores signify-cantly increased in all six core competencies after training in the emergency department and ward [9]. Narrative comments are evaluation tools commonly used to assess trainees' clinical performance [10]. The popular qualitative analytical tool, like Workplace-based narrative assessment (WBNA), represents the faculty's viewpoint.
However, the subjective experiences of trainee physicians were rarely discussed in the literature. One previous research has analyzed the comments of medical students on EM rotation that showed positive impacts on learning and clearing information for improving the training course [11]. Nevertheless, we know little about PGY physicians' thoughts and feelings about this compulsory rotation. Reflection is an essential capacity in core ACGME competencies [12], reflective practices as a teaching modality have been reported in a few specialty training [13, 14]. In our department, we have hosted a review session focused on trainees' self-reflection and feedback since the program's initiation. The information received during the meeting helped improve the program and get a more in-depth understanding of trainee feelings.
1.1 Objective
The study’s objective was to extend our regular review session, explore PGY physicians' perception through a scientific reflection-oriented approach, and analyze respondents' self-assessed impacts from their EM rotation experience. The analyzed data could be used as supporting evidence to justify the role and highlight the areas of strength of EM rotation in the PGY program.
1.2 EM rotation in PGY course
EM rotation in PGY course implemented in an ED staffed with board-certified EM attending physicians on-site 24 hours for patients' medical service and trainees' supervision. The compulsory EM rotation for PGY was a one-month block time, consisted of three crucial sections: an orientation, work shifts, and a review session. The full-day clinical-driven orien-tation incorporated an extensive range of learning modalities, including interactive didactics of avoiding common EM pitfalls, administrative and commu-nication skills; simulation workshops on handover; the practice of the electronic medical system on simulated cases, and a group of simulated case-based discussion. The practical training included 14 twelve-hour shifts in clinical service, equally distributed between day and overnight shifts. While working on clinical shift, all trainee physicians were assigned an attending physician for on-the-spot feedback and supervision to ensure adequate quality of the trainees' procedural skills and medical service. The patient care duties for PGY physicians were 20 patients on average per shift. The trainees' self-reflection and feedback are three-hour sessions that the PGY program director gathered with all trainees, comm-ented on the problems encountered during the training, listened to their self-reflections, and received verbal feedback from trainees.
2. Method
Subjects for this retrospective analysis were PGY physicians who completed EM rotation from August 2014 to July 2017 in an urban hospital accredited as a medical center-level institution with an annual census of more than 130,000 emergency department (ED) patient visits. We wanted to focus on trainees' thoughts, specifically on the role of the EM rotation within the overall experience context, so the survey asked trainees to respond to three open-ended questions. The open-ended questions allowed an in-depth exploration of the trainees' perception of the rotation. The purpose of multiple inquiries was not to constrain physicians in their thinking about what they considered appropriate EM rotation objectives from a single perspective or question. We included these open-ended questions on the existing post-rotation questionnaire survey that was part of the EM course requirement. Our analysis process involved both quantitative and qualitative research methods. The study design received approval from the Invest-igational Review Board of the hospital. The theme and retrospective nature of the study did not require a formal consent process. We completely de-identified all data before analysis.
2.1 Data
201 PGY physicians completed the survey within five days after the rotation. We implemented prompt reply instruction within five days to take advantage of the recent EM rotation's fresh and explicit memory. The responding rate was 100%; the trainees answered all three questions and generated a dataset of 603 comments.
2.2 Analysis process
We used grounded theory data analysis methods [15] to gather the ideas and emotions that emerged from the data and were significant enough to deserve their codes, specifically statements that expressed their beneficial impacts on learning from the clinical experience. Three team members formed a code development group and studied the responses; they first suggested code for inclusion independently, reviewed the code application with each other, and resolved disagreements. The final code scheme consisted of two categories, professional develop-ment, and emotional issue. We further sorted professional development codes into one of six core competencies domains by the American College for Graduate Medical Education (ACGME). Each response was reviewed and coded based on the agreed keywords by the coding group. The content of each response was parsed into one or multiple codes. The coding group had four team members working independently. The code was validated and cross-reviewed, reaching a consensus on coding. We analy-zed the data using Google Sheets software. Data from question one, "What were the most valuable lessons you learned from EM rotation?" was also used to assess the importance rank-order of the codes identified, as the question used explicitly priority phrase "the most valuable". The importance rank-order was established based on the number of PGY physicians who expressed priority for each theme.
3. Result
The result is presented in two sections reflecting different overview and conceptual analysis levels. The first section provides a quantitative overview of all coded themes in two categories. The second section focused on the analysis of responses to three individual questions.
3.1 Quantitative overview of all coded themes in two categories
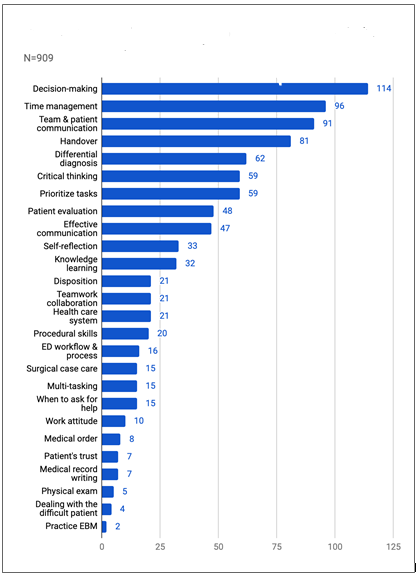
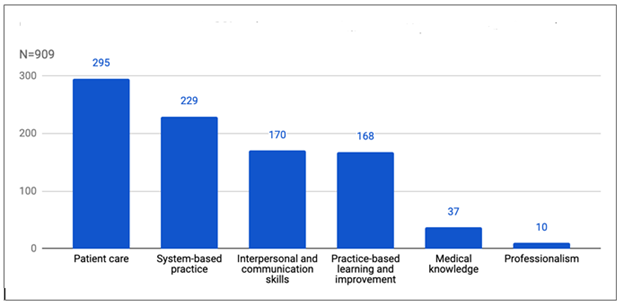
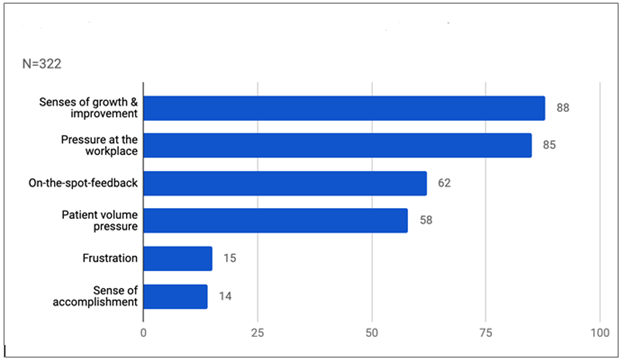
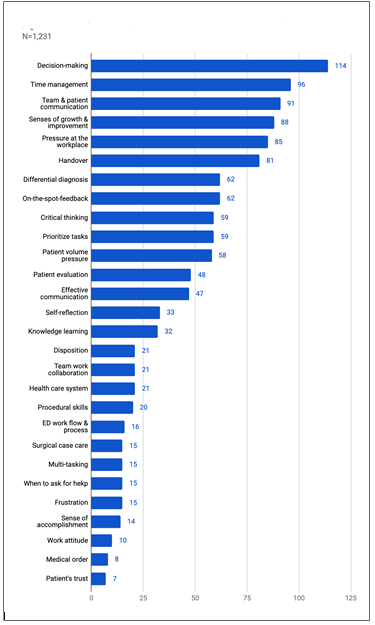
We received a total of six hundred three comments from PGY physicians. Of these, we coded 563 (96%) comments, and 22 (4%) did not match any code themes. We sorted a total of thirty-two themes essential to characterize the clinical experiences during EM rotation into two categories. Twenty-six were clinically relevant to professional development, with an overall code frequency distribution of 74% (Figure 1). We further classified the coded themes based on the six ACGME competency domains in the professional development category. Patient care was the domain with the most frequently coded competency themes (33%), followed by system-based practice (25%) and interpersonal and comm-unication skills (19%) (Figure 2). Among the patient care domain, ACGME competency most salient to PGY, decision-making was the most frequently coded theme (39%). We identified six codes with a coding frequency distribution of 26% in the emotional issue category. The three most common codes were senses of growth and improvement (27%), followed by pressure at the workplace (26%), and on-the-spot-feedback (19%) (Figure 3). We noted that two of the most common codes occupied the fourth and fifth positions in overall frequency counts (Figure 4). This finding indicated that a demanding and stressful EM rotation could be a rewarding learning experience.
3.2 Quantitative and qualitative analysis of comments on three survey questions
The analysis revealed thirty-one codes from the responses to the first question, "What were the most valuable lessons you learned from EM rotation?", twenty-six of them were relevant to professional development. Five belonged to the emotional issue category. The three most valuable lessons learned were decision-making (n=70), team and patient communication (n=59), and prioritizing tasks (n=48). No themes from the emotional issue category entered the top ten list (Table 1). Furthermore, three out of the ten most important lessons, their coding frequency ranks, were in the same order as the priority list. PGY physicians perceived decision-making as the most valuable theme, consistent with the most frequently coded theme in the patient care domain. Of coding frequency distribution, the themes in the professional development category were dominant, with 94%. Of the dataset from responses to the second question," What were the differences between your anticipated and actual learning experi-ences in EM rotation?", fifty PGY physicians (25%) reported no difference existed for the anticipated and actual rotation experiences, eleven (6%) reported exceeding expectations with valuable experiences, and nine (5%) reported experiences less useful.
Although only seventy trainees (36%) answered directly to the question with comparative description, most of them seized the opportunity to elaborate on other themes in the responses. There were 23 recognized themes in the professional development category. The coding frequency distribution in this category was 59%, less dominant than the result of the first question, and no themes from this category entered the top three most frequently codes on the list. We identified six themes in the emotional issue category, and the three most frequently coded themes were patient volume pressure (n=41), followed by pressure at the workplace (n=30), and senses of growth and improvement (n=30). A complex ER environment contributes to various forms of pressure like patient visit volume pressure, workplace press-ure, or peer pressure. We have frequently noticed the concern of pressure relevant to the rotation from the trainees during our orientation, and some PGY physi-cians were anxious about this issue on their first day.
Nevertheless, the tone of that pressure switched from a negative emotion to a motivation later in the review session. It is worth noting that some PGY physicians felt less useful regarding their clinical experiences did not match closely to the total frequency of the pressure themes in the emotional issue category. This result may suggest that PGY physicians perceived pressure as acceptable and could manage it as a driving force to work and learn during rotation. There were thirty themes identified to the third question" Any afterthoughts regarding your EM rotation experience?". The three most common themes were senses of growth and improvement (n=58), followed by pressure at the workplace (n=48), and two themes tied in third place, on-the-spot-feedback (n=37), and handover (n=37). The emotional issue category dominated the most frequently coded list but had less overall frequency distribution of 41%. The data from the response to this question may suggest a productive and positive role of EM rotation for undifferentiated physicians in the PGY program. The valuable lessons identified by the trainees were the evidence that supported the role.
|
Theme |
number of Trainees (n=201) |
Importance rank-order* |
Overall coding frequency rank-order |
|
Decision-making |
70 |
1 |
1 |
|
Team & patient communication |
59 |
2 |
3 |
|
Prioritizing tasks |
48 |
3 |
7 |
|
Time management |
47 |
4 |
2 |
|
Differential diagnosis |
40 |
5 |
5 |
|
Critical thinking |
34 |
6 |
6 |
|
Effective communication |
32 |
7 |
9 |
|
Patient evaluation |
29 |
8 |
8 |
|
Handover |
17 |
9 |
4 |
|
Disposition |
14 |
10 |
13 |
*Importance rank-order was established based on the number of PGY physicians who expressed priority for each theme in question one.
Table 1: Ten most valuable lessons perceived by PGY physicians.
4. Discussion
EM rotation experience has been discussed extensively in the literature, and EM rotation has a crucial role in medical education, specifically in medical students [7]. Our analysis has demonstrated some unique facts about the EM rotation on the PGY physician level. The most valuable lesson perceived by trainees is a crucial skill for physicians to master, as it dictates the training course direction in a clinical service framework. Many studies discussed the meth-ods or processes of medical decision-making [6, 16, 17]. Still, research regarding where or what rotation is a more suitable training place or discipline is hard to find in the literature. One qualitative study revea-led medical students commenting EM rotation as an outstanding venue to develop decision-making skills [11]. In practice, medical decision-making is often complicated, dynamic, and under time pressure, especially in ED [16]. Studies pointed out that multiple contextual factors like possible acute life-threatening conditions, limited time, case experience, and scanty information available all made decision-making in ED even more complex and challenging [16, 17]. We believe that our PGY training program had the following contextual factors that contributed to decision-making as the most valuable lesson learned during EM rotation.
First, exposure to a large case volume was one crucial element; a study of the decision-making process revealed that individual physicians' case experience could have a medium effect on the confidence rating [16]. In our program, the PGY physicians took care of an average of twenty patients during a shift. Although our result indicated that some trainees felt the pressure from this patient volume, the large case volume exposed provided the opportunity to increase decision-making confidence gained from previous similar case experiences. Another contextual factor was on-the-spot feedback, the third high-frequency emotional issue theme perceived by PGY physicians. When trainees encountered difficulty in decision-making, the most direct and efficient solution was to consult senior staff or faculty from the team. PGY is part of a care team but works primarily independently in other disciplines rotation, guidance and support are avail-able; nevertheless, help is somewhere and minutes away in reality. Unlike in the EM clinical setting, the EM attending physician is available 24-hour, PGY physicians can consult and request guidance without time or distance barriers. For inexperienced PGY physicians to perform clinically at an individual's best level, adequate supervision is needed, and timely supervision is also essential in a fast-paced, high-tension work environment like ER.
We further sorted the ten most valuable lessons perceived into groups based on the similarity of theme nature. We identified two groups of clinical judgment and the domain of interpersonal commu-nication. Three themes of decision-making, critical thinking, and disposition were relevant to how doctors think and the realm of clinical judgment. Furthermore, the other three themes, including team and patient communication, effective communicati-on, and handover, were all relevant to the interperso-nal and communication skills domain of ACGME core competencies. We think these two domains were the strengths of our EM rotation, as trainees felt significant impacts on these two clinical judgment and communication skills during training. ER is a high-pressure environment. Nevertheless, we do not discuss frequently and openly how ER doctors face pressure at the workplace; studies on such a subject are rarely found in the literature. When pressure is manageable by physicians, it lets physicians stay alert, motivated, able to work and learn. When the pressure becomes excessive and unmanageable, it leads to stress that can elicit health issues and interfere with the clinical performance of physicia-ns—the results of this study highlight that pressure is an inevitable and vital issue during ED rotation.
Interestingly, our analysis may suggest that the existing pressure did not lead to the worst scenario of stress but instead might play toward a positive role for PGY physicians as an external stimulus of learning. We believe that the on-the-spot-feedback theme has a significant role in pressure relief; a previous study found that colleagues are an essential resource for stress relief [18]. Based on our data, we hypothesize that faculty supervision with on-the-spot-feedback may be an effective technique to reduce stress for inexperienced physicians in the ER. The compulsory post-rotation survey has been a requirement for PGY trainees in our department. We kept the routine in consideration of the internal consistency and selection bias; the implementation aimed to exclude a low response rate as a limitation in this study.
However, a recent study revealed a conflicting result that compulsory evaluation might raise concerns over reliability [19]. We felt that different medical schools attended by PGY physicians and compulsory surveys contributed to a fair representation of the database in our research.
4.1 Limitations
Some aspects of this research may limit the generalization of the results. First, our PGY physicians graduated from different medical schools; their previous EM exposure in clerkship may influence the perception of this rotation. Those who had impressive experience on some professional development elements from EM clerkship may constrain the expression of the crucial impact on particular themes.
Second, this study was done at a single site. Although nationwide PGY EM training is guided by goals and objectives specified by the PGY EM rotation task force of Taiwan Joint Commission, the official accreditation agency for healthcare education programs in Taiwan, the actual execution of the PGY program curriculum may be influenced by various local factors, such as the availability of teaching modalities, type, quality of instant guidance provided to the PGY trainees, and case diversity [20]. Third, it was involved in a single discipline. Generalizing our results to other PGY discipline or training sites should be done with caution. Another limitation of this research was the lack of an in-depth analysis of coded themes. Our study focused on what outstanding impact resulted from EM rotation. The results did not infer each theme’s absolute positive or negative influence on PGY physicians.
5. Conclusion
The study indicated that EM rotation was productive in professional development for undifferentiated physicians. Gaining experiences in clinical judgment and communication were the strengths of the EM PGY program, and PGY physicians perceived decision-making as the most valuable lesson learned from EM rotation. Trainees benefit the most on general competency training from the EM rotation may not be the same as program directors anticipated or the trainees expected. This analysis model might be a novel way of assessing the achievement of learning objectives from the trainee's perspective. However, we need a prospective standardized study protocol for a further affirmative conclusion.
Declarations
Ethics approval and consent to participate
The study design received approval from the Investigational Review Board of MacKay Memorial Hospital.
Consent for publication
The theme and retrospective nature of the study did not require a formal consent process.
Availability of data and materials
The data supporting this study’s findings are available from the corresponding author upon reasonable request.
Competing interests
All authors declare no competing interests.
Funding
None to report.
Authors' contributions
All authors participated in the analysis and interpretation of the data in the study. WT was a significant contributor to the study concept, study design, and manuscript writing. All authors read and approved the final manuscript.
Acknowledgments
Not applicable
References
- Lue B-H, Cheng Y-R, Wang C-W, et al. Analysis of the Viewpoint of First Postgraduate Year Residents towards General Medicine Training. J Med Education 13 (2009): 268-274.
- Jer-Chia Tsai, Keh-Min Liu, Kun-Tai Lee, et al. Evaluation of the effectiveness of postgraduate general medicine training by objective structured clinical examination---pilot study and reflection on the experiences of Kaohsiung Medical University Hospital. Kaohsiung J Medical Sci 24 (2008): 627-633.
- Ying-Ying Yang, Fa-Yauh Lee, Hui-Chi Hsu, et al. A core competence-based objective structured clinical examination (OSCE) in evaluation of clinical performance of postgraduate year-1 (PGY₁) residents. J Chin Medical Assoc Jcma 74 (2011): 19-204.
- Chang J-C, Chen W, Chen H-S, et al. Satisfaction Survey of Community Medicine Course for Postgraduate Year One Medical Students. Taipei City Med J 6 (2009): 8-94.
- Shou-Hung Hung, Wen-Yu Hu, Wen-Jing Liu, et al. An Interventional Study Assessing Community Medicine Learning among Residents Undertaking the Course "Post-Graduate Year One (PGY-I) General Medicine." J Med Education 9 (2005): 33-45.
- Macy J. The Role of Emergency Medicine in the Future of American Medical Care. Ann Emerg Med 25 (1995): 230-233.
- Avegno J L, Murphy-Lavoie H, Lofaso D P, et al. Medical students' perceptions of an emergency medicine clerkship: an analysis of self-assessment surveys. Int J Emerg Medicine 5 (2012): 25.
- Lampe C J, Coates WC, Gill A M. Emergency Medicine Subinternship: Does a Standard Clinical Experience Improve Performance Outcomes?: EM SUBINTERNSHIP. Acad Emerg Med 15 (2008): 82-85.
- Ginsburg S, Vleuten C P, van der Eva K W, Lingard L. Cracking the code: residents' interpretations of written assessment comments. Med Educ 51 (2017): 401-410.
- Hatala R, Sawatsky A P, Dudek N, et al. Using In-Training Evaluation Report (ITER) Qualitative Comments to Assess Medical Students and Residents: A Systematic Review. Acad Med 92 (2017): 868-879.
- Marianne Yeung, Jennifer Beecker, Meridith Marks, et al. A new emergency medicine clerkship program: students' perceptions of what works. Cjem 12 (2010): 212-219.
- Wald H S, Reis S P. Beyond the margins: reflective writing and development of reflective capacity in medical education. J Gen Intern Med 25 (2010): 746-749.
- Shapiro J, Ortiz D, Ree Y Y, et al. Medical students' creative projects on a third year pediatrics clerkship: a qualitative analysis of patient-centeredness and emotional connection. Bmc Med Educ 16 (2016): 93.
- Kind T, Everett V R, Ottolini M. Learning to connect: students' reflections on doctor-patient interactions. Patient Educ Couns 75 (2008): 149-154.
- David S. Interpreting qualitative data. 6th ed (2020).
- Hausmann D, Zulian C, Battegay E, et al. Tracing the decision-making process of physicians with a Decision Process Matrix. Bmc Med Inform Decis 16 (2016): 133.
- Franklin A, Liu Y, Li Z, et al. Opportunistic decision making and complexity in emergency care. J Biomed Inform 44 (2011): 469-476.
- Yue-Yung Hu, Megan L Fix, Nathanael D Hevelone, et al. Physicians' needs in coping with emotional stressors: the case for peer support. Archives Surg Chic Ill 147 (2011): 212-217.
- Sola Aoun Bahous, Pascale Salameh, Angelique Salloum, et al. Voluntary vs. compulsory student evaluation of clerkships: effect on validity and potential bias. Bmc Med Educ 18 (2018): 9.
- Gerbase M W, Germond M, Nendaz M R, et al. When the Evaluated Becomes Evaluator: What Can We Learn From Students' Experiences During Clerkships?. Acad Med 84 (2009): 877-885.