The Road to Sepsis in Polytrauma Patients: Waypoints between Damage Control Surgery and Early Total Care to Avoid Sepsis
Article Information
Cédric Niggli1*, Philipp Vetter1, Jan Hambrecht1, Philipp Niggli2, Hans-Christoph-Pape1, Ladislav Mica1
1Department of Trauma Surgery, University Hospital Zurich, 8091 Zurich, Switzerland
2Department of Mathematics, ETH Zurich, 8092 Zurich, Switzerland
*Corresponding Author: Cédric Niggli, Department of Trauma Surgery, University Hospital Zurich, 8091 Zurich, Switzerland
Received: 26 October 2023; Accepted: 06 November 2023; Published: 13 December 2023
Citation: Cédric Niggli, Philipp Vetter, Jan Hambrecht, Philipp Niggli, Hans-Christoph-Pape, Ladislav Mica. The Road to Sepsis in Polytrauma Patients: Waypoints between Damage Control Surgery and Early Total Care to Avoid Sepsis. 6 (2023): 420-431.
View / Download Pdf Share at FacebookAbstract
Prompt and effective sepsis treatment is crucial for reducing multiorgan failure and improving patient outcomes following polytrauma. The management of severe trauma involves two strategies: damage control surgery (DCS) and early total care (ETC), each with distinct timing and objectives to prevent sepsis development. This study aimed to examine different clinical and laboratory parameters in the DCS and ETC groups regarding the development of sepsis. A retrospective cohort study was conducted at the University Hospital. Participants included trauma patients aged ≥16 years with an Injury Severity Score (ISS) ≥16, investigating sepsis within 21 days of admission. DCS and ETC groups were compared in relation to sepsis development. Statistical methods encompassed group comparisons with Welch’s t-test, binary logistic regression, and conditional augmented inverse probability weighting (CAIPW). 2881 patients were included in the final study. The analysis showed that ISS had a significant impact on sepsis risk in both groups. Other factors like GCS, temperature, and ATLS shock class influenced sepsis risk in the ETC group, while leucocytosis, low pH, and high Quick values impacted sepsis risk in the DCS group. The study's key results indicate that sepsis is more common in the DCS group due to the higher frequency of DCS procedures in patients with high ISS scores, making them more susceptible to infection. The study highlights the complexity of choosing between DCS and ETC strategies, with both having advantages and challenges concerning sepsis development in polytrauma patients.
Keywords
Sepsis, Polytrauma, Damage control surgery, Early total care
Sepsis articles; Polytrauma articles; Damage control surgery articles; Early total care articles
Sepsis articles Sepsis Research articles Sepsis review articles Sepsis PubMed articles Sepsis PubMed Central articles Sepsis 2023 articles Sepsis 2024 articles Sepsis Scopus articles Sepsis impact factor journals Sepsis Scopus journals Sepsis PubMed journals Sepsis medical journals Sepsis free journals Sepsis best journals Sepsis top journals Sepsis free medical journals Sepsis famous journals Sepsis Google Scholar indexed journals Polytrauma articles Polytrauma Research articles Polytrauma review articles Polytrauma PubMed articles Polytrauma PubMed Central articles Polytrauma 2023 articles Polytrauma 2024 articles Polytrauma Scopus articles Polytrauma impact factor journals Polytrauma Scopus journals Polytrauma PubMed journals Polytrauma medical journals Polytrauma free journals Polytrauma best journals Polytrauma top journals Polytrauma free medical journals Polytrauma famous journals Polytrauma Google Scholar indexed journals Damage control surgery articles Damage control surgery Research articles Damage control surgery review articles Damage control surgery PubMed articles Damage control surgery PubMed Central articles Damage control surgery 2023 articles Damage control surgery 2024 articles Damage control surgery Scopus articles Damage control surgery impact factor journals Damage control surgery Scopus journals Damage control surgery PubMed journals Damage control surgery medical journals Damage control surgery free journals Damage control surgery best journals Damage control surgery top journals Damage control surgery free medical journals Damage control surgery famous journals Damage control surgery Google Scholar indexed journals Early total care articles Early total care Research articles Early total care review articles Early total care PubMed articles Early total care PubMed Central articles Early total care 2023 articles Early total care 2024 articles Early total care Scopus articles Early total care impact factor journals Early total care Scopus journals Early total care PubMed journals Early total care medical journals Early total care free journals Early total care best journals Early total care top journals Early total care free medical journals Early total care famous journals Early total care Google Scholar indexed journals improved mortality rates articles improved mortality rates Research articles improved mortality rates review articles improved mortality rates PubMed articles improved mortality rates PubMed Central articles improved mortality rates 2023 articles improved mortality rates 2024 articles improved mortality rates Scopus articles improved mortality rates impact factor journals improved mortality rates Scopus journals improved mortality rates PubMed journals improved mortality rates medical journals improved mortality rates free journals improved mortality rates best journals improved mortality rates top journals improved mortality rates free medical journals improved mortality rates famous journals improved mortality rates Google Scholar indexed journals leucocytosis articles leucocytosis Research articles leucocytosis review articles leucocytosis PubMed articles leucocytosis PubMed Central articles leucocytosis 2023 articles leucocytosis 2024 articles leucocytosis Scopus articles leucocytosis impact factor journals leucocytosis Scopus journals leucocytosis PubMed journals leucocytosis medical journals leucocytosis free journals leucocytosis best journals leucocytosis top journals leucocytosis free medical journals leucocytosis famous journals leucocytosis Google Scholar indexed journals traumatic surgery articles traumatic surgery Research articles traumatic surgery review articles traumatic surgery PubMed articles traumatic surgery PubMed Central articles traumatic surgery 2023 articles traumatic surgery 2024 articles traumatic surgery Scopus articles traumatic surgery impact factor journals traumatic surgery Scopus journals traumatic surgery PubMed journals traumatic surgery medical journals traumatic surgery free journals traumatic surgery best journals traumatic surgery top journals traumatic surgery free medical journals traumatic surgery famous journals traumatic surgery Google Scholar indexed journals stopgap remedies articles stopgap remedies Research articles stopgap remedies review articles stopgap remedies PubMed articles stopgap remedies PubMed Central articles stopgap remedies 2023 articles stopgap remedies 2024 articles stopgap remedies Scopus articles stopgap remedies impact factor journals stopgap remedies Scopus journals stopgap remedies PubMed journals stopgap remedies medical journals stopgap remedies free journals stopgap remedies best journals stopgap remedies top journals stopgap remedies free medical journals stopgap remedies famous journals stopgap remedies Google Scholar indexed journals surgical team articles surgical team Research articles surgical team review articles surgical team PubMed articles surgical team PubMed Central articles surgical team 2023 articles surgical team 2024 articles surgical team Scopus articles surgical team impact factor journals surgical team Scopus journals surgical team PubMed journals surgical team medical journals surgical team free journals surgical team best journals surgical team top journals surgical team free medical journals surgical team famous journals surgical team Google Scholar indexed journals IBM WATSON Trauma Pathway Explorer© articles IBM WATSON Trauma Pathway Explorer© Research articles IBM WATSON Trauma Pathway Explorer© review articles IBM WATSON Trauma Pathway Explorer© PubMed articles IBM WATSON Trauma Pathway Explorer© PubMed Central articles IBM WATSON Trauma Pathway Explorer© 2023 articles IBM WATSON Trauma Pathway Explorer© 2024 articles IBM WATSON Trauma Pathway Explorer© Scopus articles IBM WATSON Trauma Pathway Explorer© impact factor journals IBM WATSON Trauma Pathway Explorer© Scopus journals IBM WATSON Trauma Pathway Explorer© PubMed journals IBM WATSON Trauma Pathway Explorer© medical journals IBM WATSON Trauma Pathway Explorer© free journals IBM WATSON Trauma Pathway Explorer© best journals IBM WATSON Trauma Pathway Explorer© top journals IBM WATSON Trauma Pathway Explorer© free medical journals IBM WATSON Trauma Pathway Explorer© famous journals IBM WATSON Trauma Pathway Explorer© Google Scholar indexed journals
Article Details
Introduction
Among polytrauma patients, septic complications account for the leading cause of death after the first week [1]. The presence of Compensatory Anti-Inflammatory Response Syndrome (CARS), characterized by immunological exhaustion, increases the vulnerability of polytrauma patients to subsequent infectious complications, including sepsis [2,3]. Prompt, accurate, and effective sepsis treatment has been shown to decrease the incidence of multi-organ failure (MOF), leading to improved mortality rates and overall clinical outcomes [4].
The management of severe trauma and injuries uses two strategies: damage control surgery (DCS) and early total care (ETC). While both attempt to avoid consequences like sepsis, their timing and objectives are different.
DCS is frequently used on patients who have suffered severe trauma and complex injuries. The primary goal of DCS is to immediately minimize life-threatening contamination and hemorrhage while minimizing the patient's surgical trauma and physiological stress. DCS seeks to shorten the first procedure's time and avoid overly traumatic surgery, which might hasten the onset of sepsis. ETC is an alternate strategy and involves performing a definitive surgical repair as quickly as feasible after a serious injury, without the need for temporary fixation or other stopgap remedies. It aims to minimize the need for subsequent procedures and accelerates recuperation. ETC reduces the chance of contamination and ensuing sepsis growth. It's crucial to remember that the decision between DCS and ETC is based on several variables, including the patient's overall health, the severity of their injuries, and the availability of resources and knowledge. A qualified surgical team should choose the precise strategy depending on the requirements of each unique patient.
To predict the outcome of severely injured patients, this study group, in collaboration with IBM, developed the IBM WATSON Trauma Pathway Explorer©, a visual analytics tool [5,6]. This validated, interactive tool predicts different events based on clinical and laboratory parameters, such as sepsis within 21 days of patient admission, depending on different treatment strategies such as DCS and ETC. The question therefore arose as to how frequently sepsis occurs with certain selected parameters in the ETC and DCS group.
The objective of this study was to examine different clinical and laboratory parameters in the DCS and ETC groups regarding the development of sepsis.
Methods
Study design
The research for this article was conducted on the basis of the STROBE Statement, a guideline for observational studies in epidemiology [7]. The data was obtained through a retrospective cohort study conducted at the University Hospital Zurich, covering the period from January 1996 to December 2012.
Participants
Inclusion criteria for the patients were age ≥16 years and an Injury Severity Score (ISS) ≥16, with an ISS score equal to or greater than 16 defining a polytrauma [8]. Patients admitted directly to the trauma bay were considered. Excluded from the study were patients with a missing surgical treatment strategy (DCS or ETC).
Outcome
The outcome examined was sepsis within 21 days of the patient's admission to the trauma hospital. The development of sepsis was studied separately for the DCS and ETC groups.
To classify as sepsis, a SIRS score of ≥2 was required, along with an additional infectious focus [9]. An infection diagnosis was established either through strong clinical sepsis criteria (such as organ dysfunction, hypotension, and hypoperfusion) or through microbiological detection [9]. Sepsis had to occur at any time during the 21-day observation period.
SIRS was determined based on the presence of two or more of the following criteria: body temperature >38°C or <36°C, heart rate >90 bpm, respiratory rate >20 breaths/min, and white blood cell count >12’000/µl or <4’000/µl [9]. The evaluation of SIRS was performed for the initial 21 days after admission or throughout the patient's hospital stay.
This study utilized the older sepsis definition based on the ACCP/SCCM Consensus Conference Committee [9]. In more recent years, an alternative definition for sepsis, known as the Sepsis-3 Criteria, has emerged [10]. However, for the data collection in this hospital cohort, all sepsis criteria were evaluated following the well-established older and more widely used definition. Additionally, some recent research has suggested that the older sepsis definition outperforms the newer one [11].
Parameters
DCS and ETC groups were examined regarding the development of sepsis. Patients who did not receive an intervention were assigned to the DCS group.
The DCS concepts include:
- Rapid control of bleeding: The primary goal of DCS is to achieve rapid hemostasis by controlling active bleeding through various techniques, such as tourniquets, packing, and ligation. This is crucial in preventing further hemorrhage and improving the patient's hemodynamic stability [12].
- Minimization of surgical insult: During the initial operation, surgeons focus on addressing the most critical injuries while avoiding extensive manipulation of tissues and organs to reduce surgical trauma. This helps limit the patient's exposure to anesthesia and reduces the risk of complications associated with prolonged surgery [13].
- Temporary stabilization: DCS involves temporary repairs to stabilize injuries, such as bowel resections with stapled closures, temporary vascular shunts, or the use of external fixators for fractures. These temporary measures buy time for the patient to recover from the initial shock and physiological derangement before definitive repairs are undertaken [14].
- Avoidance of sepsis and contamination: Surgeons try to minimize the risk of sepsis and contamination by controlling contamination sources, irrigating the affected areas, and using techniques like "damage control dressing" to manage open wounds [15].
- Definitive repair in staged procedures: Once the patient's condition has stabilized, definitive repairs of injuries are performed in staged procedures. These subsequent operations allow for more meticulous repair, reducing the risk of complications associated with rushed or complex initial surgeries [16].
- The main issues of ETC include:
- Immediate stabilization: The primary goal of ETC is to provide immediate stability to the fractured bone(s). This is achieved through early surgical intervention, allowing for early mobilization of the patient and minimizing the risk of further complications associated with prolonged immobilization [17].
- Single definitive surgery: ETC involves performing a single surgery to definitively fix the fracture rather than using a staged approach. The surgery aims to achieve anatomical alignment and stable fixation of the fracture site, allowing for early weight-bearing and rehabilitation [18].
- Early timing: ETC is typically performed within the first 24 to 72 hours after the injury, depending on the patient's overall condition, physiological stability, and the presence of other life-threatening injuries. It requires prompt assessment, coordination, and communication between the trauma team and orthopedic surgeons [19].
- Basic parameters consisting of patient data, clinical data, and lab values were included in the analysis to examine the relationship between these parameters and the development of sepsis in the DCS and ETC groups.
Patient data included age and sex. Clinical trauma-related parameters assessed were trauma mechanism (blunt vs. penetrating), ISS, temperature at admission, GCS at the accident site, and ATLS shock class. Lab data implied leucocytes, CRP, pH, lactate, hemoglobin, and Quick at admission of the patient. The parameters mentioned were analyzed for the DCS group as well as for the ETC group.
Data measurement
Age, sex, trauma mechanism, ISS, and temperature at admission (°C) were taken from the admission report in the emergency room. GCS at the accident site was retrieved from the rescue service protocol. Point-of-care testing (POCT) in the emergency room was conducted for pH, lactate (mmol/L), hemoglobin (g/dL), and Quick (%). Leucocytes (WBC/µl) and CRP (mg/L) were measured in the Department of Clinical Chemistry at the University Hospital Zurich.
Statistics
The baseline characteristics of the patient’s sample (overall, DCS, ETC) were described through medians with interquartile ranges (IQR) for interval data, ratio data and ordinal data, and percentages for binary variables. The differences between these groups were assessed using the Wilcoxon rank sum test for numerical data and Pearson’s Chi-squared test for categorical variables. A p-value <0.05 was considered significant.
Violin plots with Welch's t-test assessed the central tendency of the different parameters in the sepsis and non-sepsis cohorts for the DCS and ETC groups, respectively [20,21].
The differences in the probabilities of the two treatments (DCS vs. ETC) for the outcome sepsis were determined by the “Conditional Augmented Inversed Probability Weighting” (CAIPW) method. This method estimates the “Average Treatment Effect” (ATE) of DCS vs. ETC regarding sepsis by calculating the conditional means in regression modeling. CAIPW estimators amalgamate elements from both regression-adjustment and inverse-probability-weighted methods, which makes this method very robust [22-24]. The calculations were adjusted for ISS, as ISS has a non-negligible impact on the development of sepsis [25]. Two subgroups per parameter were chosen, whereas the cutoff was chosen randomly by the authors.
Binary logistic regression was performed to explore the impact of patient characteristics and lab parameters on the development of sepsis in the DCS and ETC groups. Odds ratios were used along with 95% confidence intervals [26].
No imputation method was chosen for missing values. Statistics were performed with R-4.2.2 [27-33].
Ethics
The study adhered to the guidelines for good clinical practice and Helsinki guidelines. The analysis of trauma patient records was approved by the University Hospital Zurich's ethics commission and the Zurich government upon the development of the database (Nr. StV: 1-2008). They again re-approved it for the development of the WATSON Trauma Pathway Explorer© (BASEC: 2021-00391).
Results
Patient selection
The polytrauma data bank consisted of 3653 patients between 1996 and 2012. Data preparation resulted in 3074 patients (84.2%) with an ISS ≥16 and 3059 patients (83.7%) with age ≥16 years. 178 patients (4.9%) were excluded due to missing surgical treatment strategy (DCS or ETC), resulting in a final study population of 2881 patients (78.9%). The number of participants at each stage is shown in figure 1.
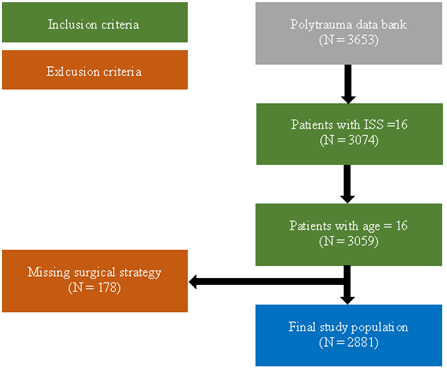
Figure 1: Flowchart of patient selection
Descriptive data
In total, 2881 patients were included. In both study groups (DCS and ETC), roughly ¾ of the participants were men and the median age of the participants was 43 years overall. DCS patients significantly experienced more penetrating traumas than ETC patients (9% vs. 6%, p = 0.006). Most trauma mechanisms were blunt. In the DCS group, patients were more severely injured with higher ISS scores (29 vs. 26, p <0.001). There were no significant differences in the length of ICU or length of hospitalization. DCS patients developed sepsis significantly more often than the ETC group (18% vs. 14%, p = 0.002). Likewise, patients in the DCS group were significantly more likely to die within 72 hours than those who underwent ETC (26% vs. 14%, p <0.001). ATLS shock class I was more represented in the ETC group, while shock classes II-IV were more common in the DCS group. Patients undergoing DCS were significantly colder than ETC patients (35.5 vs. 36.0°C, p <0.001). Among the laboratory parameters at admission, the following values differed significantly in the DCS and ETC group: pH (7.33 vs. 7.35, p <0.001), lactate (2.30 vs. 2.19mmol/L, p = 0.018), hemoglobin (11.20 vs. 12.40g/dL, p <0.001), hematocrit (33 vs. 37%, p <0.001) and Quick (79 vs. 89%, p <0.001). DCS and ETC did not differ in terms of GCS at site and leucocytes at admission. The numbers of total values for each parameter were also included (Table 1).
|
Treatment strategy |
|||||
|
Variable |
N |
Overall, N = 2,881 1 |
DCS, N = 1,908 1 |
ETC, N = 973 1 |
p-value 2 |
|
Age (years) |
2,881 |
43 (28, 61) |
44 (28, 61) |
43 (28, 60) |
0.2 |
|
Male |
2,881 |
2,124 (74%) |
1,405 (74%) |
719 (74%) |
0.9 |
|
Blunt trauma |
2,881 |
2,643 (92%) |
1,731 (91%) |
912 (94%) |
0.006 |
|
ISS |
2,881 |
27 (22, 38) |
29 (24, 41) |
26 (20, 34) |
<0.001 |
|
Length of ICU (days) |
2,865 |
5 (2, 12) |
5 (2, 12) |
5 (2, 12) |
0.2 |
|
Lentgh of hospitalisation (days) |
2,876 |
13 (4, 24) |
14 (3, 26) |
13 (6, 21) |
0.3 |
|
Sepsis |
2,881 |
477 (17%) |
345 (18%) |
132 (14%) |
0.002 |
|
Death within 72 hours |
2,881 |
641 (22%) |
501 (26%) |
140 (14%) |
<0.001 |
|
ATLS shock class |
2,857 |
<0.001 |
|||
|
1 |
1,727 (60%) |
1,059 (56%) |
668 (69%) |
||
|
2 |
720 (25%) |
502 (27%) |
218 (22%) |
||
|
3 |
215 (7.5%) |
169 (9.0%) |
46 (4.7%) |
||
|
4 |
195 (6.8%) |
157 (8.3%) |
38 (3.9%) |
||
|
GCS at site |
2,643 |
12.0 (4.0, 15.0) |
12.0 (4.0, 15.0) |
11.0 (5.0, 15.0) |
>0.9 |
|
Temperature at admission (°C) |
2,092 |
35.70 (34.60, |
35.50 (34.40, |
36.00 (35.08, |
<0.001 |
|
36.50) |
36.40) |
36.70) |
|||
|
Leucocytes at admission (WBC/µL) |
2,638 |
12.2 (9.0, 16.3) |
12.2 (8.9, 16.5) |
12.3 (9.2, 16.0) |
0.4 |
|
CRP at admission (mg/L) |
2,207 |
3 (1, 5) |
3 (1, 5) |
3 (1, 6) |
<0.001 |
|
pH at admission |
2,108 |
7.33 (7.26, 7.39) |
7.33 (7.25, 7.38) |
7.35 (7.29, 7.39) |
<0.001 |
|
Lactate at admission (mmol/L) |
2,468 |
2.30 (1.40, 3.60) |
2.30 (1.40, 3.80) |
2.19 (1.40, 3.29) |
0.018 |
|
Hemoglobin at admission (g/dL) |
2,450 |
11.70 (9.40, 13.40) |
11.20 (8.80, 13.00) |
12.40 (10.63, |
<0.001 |
|
13.80) |
|||||
|
Hematocrit at admission (%) |
2,557 |
35 (28, 40) |
33 (26, 38) |
37 (32, 41) |
<0.001 |
|
Quick at admission (%) |
2,253 |
83 (62, 96) |
79 (59, 94) |
89 (74, 100) |
<0.001 |
|
1 Median (IQR) or Frequency (%) |
|||||
|
2 Wilcoxon rank sum test; Pearson’s Chi-squared test |
|||||
Table 1: Descriptive statistics of the patient sample for Damage Control Surgery (DCS) and Early Total Care (ETC), including the number of total values.
Main results
Central tendency of different parameters for sepsis in the DCS vs. ETC groups
The violin plots in Figure 2 illustrate how different clinical parameters are distributed by sepsis in the DCS and ETC groups. Given are the 25th percentile, median, and 75th percentile, as well as the median values. The p-values are stated as well. The violin plots for age demonstrate that patients developing sepsis are younger in the DCS and ETC groups, whereas the difference is only significant in the DCS group. Septic patients have higher ISS scores in both groups, with p <0.001 in the ETC group. Patients developing sepsis have significantly higher leucocyte counts at admission in the DCS group, but not in the ETC group. The pH is lower for sepsis in both groups, however not significant. Lower hemoglobin and hematocrit values play a more meaningful role for sepsis in the DCS group (p = 0.07 and 0.04) than in the ETC group (p = 0.68 and 0.09) (Figure 2).
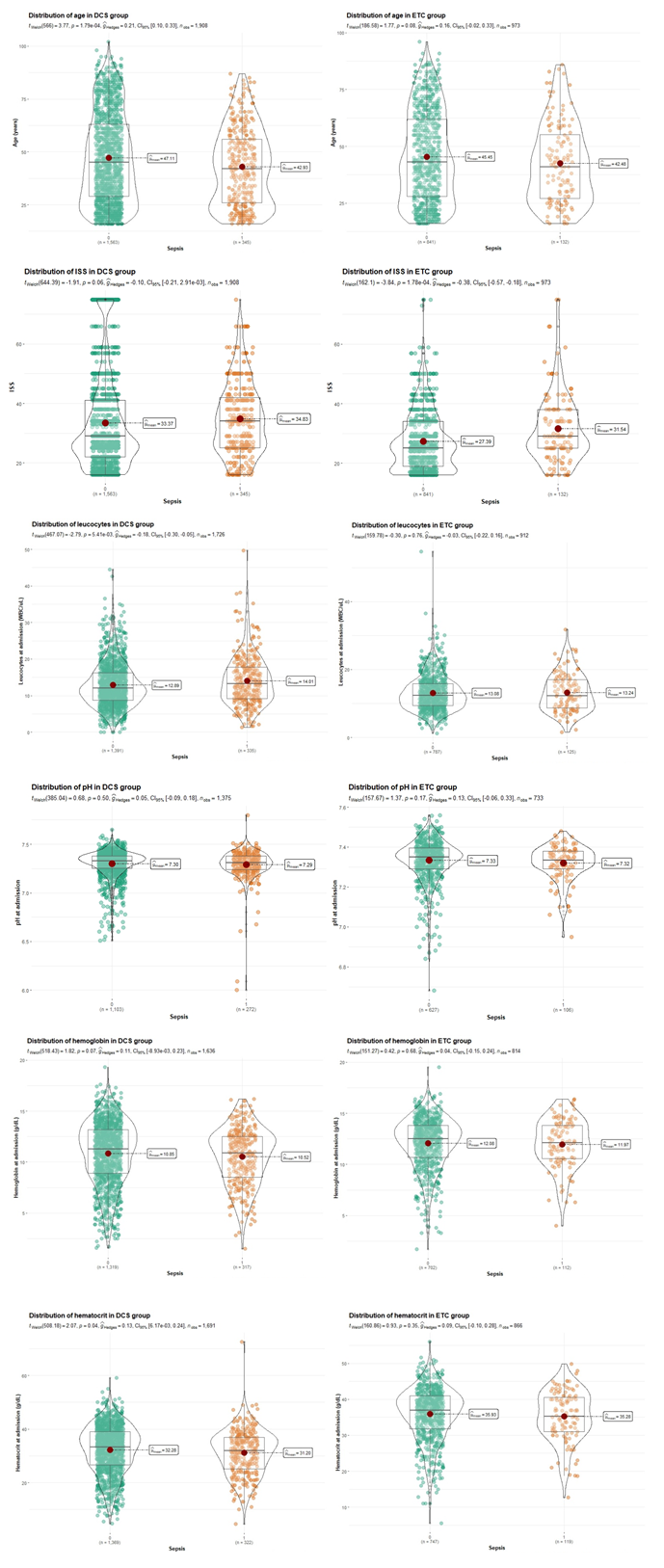
Figure 2: Violin plots displaying the central tendency of different parameters for sepsis and non-sepsis, separately for DCS and ETC
Differences in treatment effects for sepsis in the DCS vs. ETC groups
For almost all subgroups of parameters (except for the subgroup Quick <50 %), sepsis is more frequent in the DCS group than in the ETC group (Figure 3).
In the subgroup with age <50 years, DCS has an approx. 4% higher probability of sepsis compared to ETC, while in the subgroup with age >50 years, this probability increases to approx. 7% (Figure 3a).
The risk of developing sepsis in DCS-treated polytrauma patients increases in the subgroup with an ISS >30 compared to ETC procedures (Figure 3b).
Higher temperatures >36.0°C reduce the probability of DCS-treated patients developing sepsis, but it is still slightly higher than in the ETC group (Figure 3c).
With leucocytes >15’000/µl at admission, the probability of sepsis increases in DCS patients compared to ETC patients (Figure 3d).
In the subgroup with CRP <100mg/L at admission, there are no differences in the likelihood of sepsis between DCS and ETC procedures. However, as the CRP at admission increases to >100mg/L, DCS has about a 7% higher probability of sepsis than ETC (Figure 3e).
In the subgroup with a pH <7.4, DCS patients are about 2% more likely to develop sepsis than ETC patients, but about 12% more likely to develop sepsis in the subgroup with a pH >7.4 (Figure 3f).
Both patients in the lactate groups above and below 6mmol/L have a similarly higher risk of sepsis in the DCS group compared to the ETC group (Figure 3g).
Although the risk of sepsis in DCS patients is higher than in ETC patients in both hemoglobin and hematocrit subgroups, the risk decreases slightly when hemoglobin and hematocrit values increase (Figure 3h and Figure 3i).
In severe coagulopathy (Quick <50%), patients treated with DCS have an approx. 3% lower risk of developing sepsis than the ETC group, whereas DCS has an approx. 5% higher risk of sepsis in the subgroup with Quick >50% (Figure 3j).
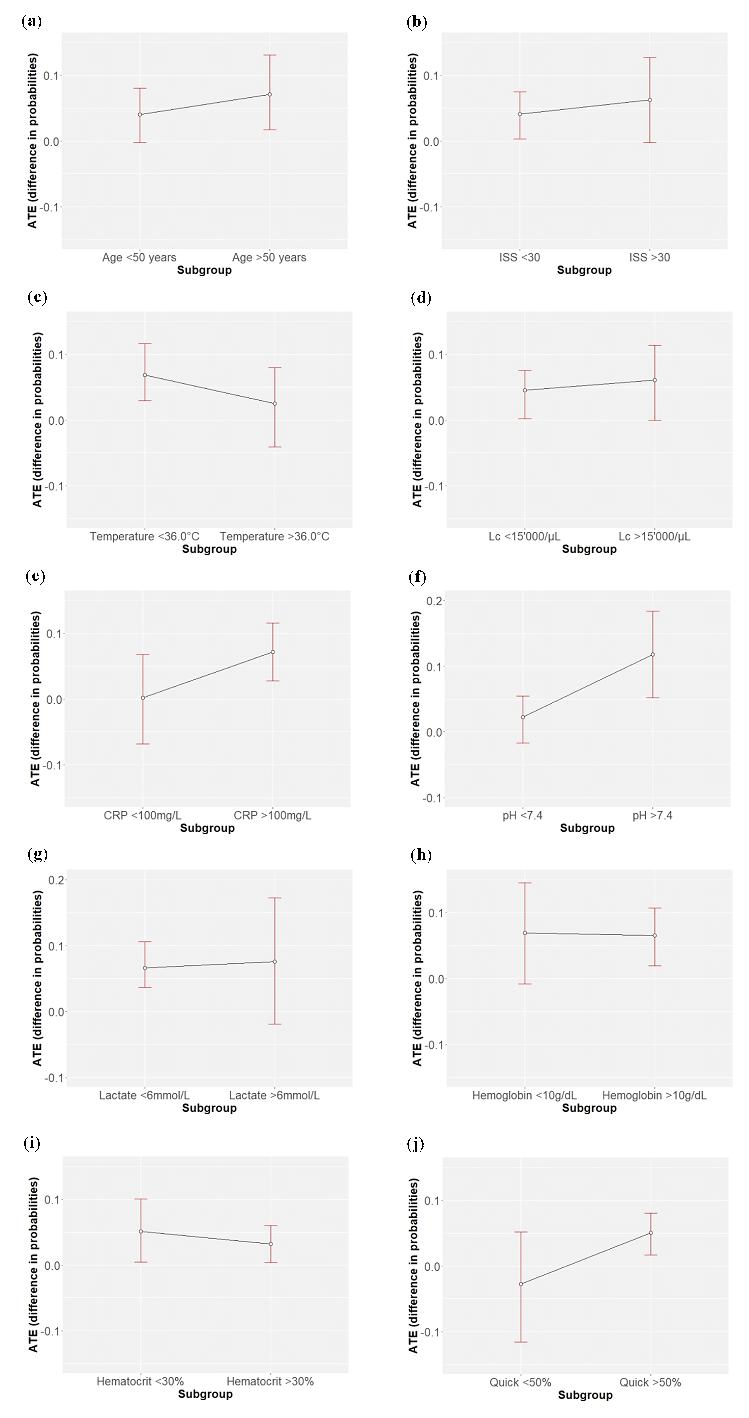
Figure 3: Differences in the treatment probabilities of DCS compared to ETC for the outcome sepsis in different subgroups of parameters, with means and corresponding confidence intervals: (a) age (years); (b) ISS; (c) temperature at admission (°C); (d) leucocytes at admission (WBC/µl); (e) CRP at admission (mg/L), (f) pH at admission; (g) Lactate at admission (mmol/L); (h) hemoglobin at admission (g/dL); (i) hematocrit at admission (%); (j) Quick at admission (%)
Correlation of different parameters with sepsis in the DCS vs. ETC group
The results of the binary logistic regression analysis examining the relationship between different parameters and sepsis in the DCS and ETC groups are presented in table 2.
Age, sex, and trauma mechanism in the DCS vs. ETC group have only little impact on the development of sepsis. The findings indicate that ISS has a significant impact on sepsis in both DCS and ETC-treated polytraumas. A lower GCS at site, higher temperature at admission, and higher ATLS shock class significantly increase the risk for sepsis in the ETC group. In contrast, leucocytosis is strongly associated with sepsis in the DCS group. Significant higher sepsis rates are also observed in DCS procedures with low pH and lactate values. Furthermore, high Quick values have a significant impact on sepsis only when DCS is performed (Table 2).
|
Sepsis in DCS group |
Sepsis in ETC group |
|||||
|
Variable |
OR 1 |
95% CI 1 |
p-value |
OR 1 |
95% CI 1 |
p-value |
|
Age |
1 |
0.99, 1.00 |
0.3 |
1 |
0.99, 1.02 |
0.6 |
|
Male |
1.25 |
0.80, 1.97 |
0.3 |
1.01 |
0.49, 2.18 |
>0.9 |
|
Blunt trauma |
1.62 |
0.83, 3.43 |
0.2 |
1.42 |
0.25, 26.8 |
0.7 |
|
ISS |
1.02 |
1.01, 1.03 |
0.007 |
1.04 |
1.01, 1.07 |
0.012 |
|
ATLS shock class |
1.12 |
0.90, 1.39 |
0.3 |
1.58 |
1.04, 2.36 |
0.028 |
|
GCS at site |
1.02 |
0.98, 1.06 |
0.4 |
0.89 |
0.83, 0.95 |
<0.001 |
|
Temperature at admission |
0.93 |
0.82, 1.07 |
0.3 |
1.34 |
1.07, 1.73 |
0.017 |
|
Leucocytes at admission |
1.05 |
1.02, 1.08 |
0.002 |
1.01 |
0.96, 1.07 |
0.7 |
|
CRP at admission |
1 |
1.00, 1.01 |
0.2 |
1 |
1.00, 1.01 |
0.2 |
|
pH at admission |
0.1 |
0.01, 0.69 |
0.02 |
0.07 |
0.00, 3.85 |
0.2 |
|
Lactate at admission |
0.89 |
0.80, 0.98 |
0.019 |
0.93 |
0.78, 1.08 |
0.3 |
|
Hemoglobin at admission |
1.31 |
0.94, 1.87 |
0.12 |
1.76 |
0.99, 3.32 |
0.069 |
|
Hematocrit at admission |
0.89 |
0.79, 1.00 |
0.059 |
0.83 |
0.67, 1.01 |
0.078 |
|
Quick at admission |
1.01 |
1.00, 1.02 |
0.028 |
1 |
0.98, 1.02 |
0.8 |
|
1 OR = Odds Ratio, CI = Confidence Interval |
||||||
Table 2: Binary logistic regression analysis between sepsis and different parameters, separated for DCS and ETC (odds ratios are presented along with 95% confidence intervals) Table 2. Binary logistic regression analysis between sepsis and different parameters, separated for DCS and ETC (odds ratios are presented along with 95% confidence intervals).
Discussion
Key results
In principle, sepsis occurs more frequently in the DCS group than in the ETC group. This is mainly due to the fact that DCS procedures are more often performed with high ISS scores, which makes these patients more susceptible to infection and subsequent sepsis. The following statements about the different clinical parameters regarding the development of sepsis can be made:
- Age: DCS patients developing sepsis are significantly younger than those without sepsis. In patients >50 years, the risk for sepsis is increased for DCS procedures compared to ETC surgery.
- ISS: Septic patients have significantly higher ISS scores in DCS and ETC groups. ISS scores >30 trigger sepsis in DCS patients more than in ETC patients.
- Temperature: Higher temperatures are associated with sepsis in the ETC group. Cold patients (<36.0°C) undergoing DCS are affected by sepsis more than cold patients treated with ETC.
- Leucocytes and CRP: High leucocyte counts at admission play a significant role for sepsis in DCS-treated polytrauma patients. DCS patients are more likely to develop sepsis when they have high levels of inflammation markers (leucocytes, CRP) compared to ETC patients.
- pH and lactate: Acidosis in DCS patients significantly influences sepsis. Lactate does not seem to play a meaningful role here. Non-acidotic patients (pH >7.4) undergoing DCS have a much higher probability of sepsis than patients treated with ETC.
- Hemoglobin and hematocrit: Septic patients in the ETC group have significantly lower hematocrit values. Low hemoglobin and hematocrit values are more relevant in the DCS group compared to the ETC group regarding the development of sepsis.
- Quick: Quick scores >50% are associated with sepsis in DCS patients. Coagulopathy of trauma shock (Quick <50%) is associated with sepsis in ETC-treated polytrauma patients more than in patients undergoing DCS.
Limitations
This study features several limitations. First, the study did not consider the temporal progression of laboratory parameters, nor did it make any effort to incorporate additional factors like Interleukin-6 or Procalcitonin. Second, the comorbidities of the patients could not be considered because they were not documented. Third, it remains impossible to ascertain the count of patients who were ventilated and intubated upon hospital admission. This aspect, however, could be important as it might influence respiratory infections that could potentially trigger sepsis. Fourth, the database was initiated on August 01, 1996, with continuous collection of patient data. It is reasonable to assume that there could have been fluctuations over the years in terms of admitting polytrauma patients, and not all patients may have been consistently included in the registry. Fifth, variations in measurement methods for diverse laboratory values throughout the entire duration of the study could have led to minor discrepancies in blood levels. Sixth, there is a notable quantity of missing values upon admission (particularly for temperature, CRP, pH, and Quick), which might be acceptable considering the extensive patient sample. Moreover, no conclusions can be drawn about the long-term survival rate of the cohort. Finally, minor adjustments to treatment protocols over the past decade might have impacted the emergence of sepsis subsequent to DCS or ETC procedures.
Interpretation
As in this study, an analysis of the German trauma registry revealed that individuals belonging to the DCO group had a higher occurrence of sepsis than patients undergoing ETC (27). A study by Pape et al. compared ETC for femur fractures in stable patients with DCO procedures. The findings indicated that ETC was associated with shorter ventilation times and lower occurrence of sepsis when compared to the DCO group (28). In a more recent study, Bläsius et al. discovered a higher sepsis rate in seriously injured patients who had been treated with DCS (29). We did not observe significant differences in the length of ICU stay between the DCO and ETC groups. This can be partly attributed to the fact that while the sepsis rate is higher in DCO, the mortality rate is also higher.
Regarding sepsis development, DCS may indirectly influence the risk by limiting the extent of surgical manipulation during the initial procedure. While this approach reduces the immediate surgical insult, it can create a window of vulnerability during which potential sources of infection, such as open wounds or internal contamination, remain untreated. Delayed definitive surgery exposes patients to a risk of infections gaining a foothold, which, if left unchecked, could progress to sepsis.
The aggressive nature of ETC, involving extensive surgical procedures and interventions, can also potentially overwhelm the patient's immune system. This could lead to an exaggerated inflammatory response, increasing the risk of a systemic inflammatory state that might contribute to the development of sepsis.
There is consensus in the literature to switch to DCS in the presence of hypothermia, acidosis, and coagulopathy, to improve the outcome of multiple injured patients (30). However, little is known about the effects of individual parameters on the development of sepsis in the two groups DCS vs. ETC:
Age
Elderly patients undergoing DCS may be more susceptible to developing sepsis compared to patients undergoing ETC. They have a less robust immune response due to multiple comorbidities, and potential contaminants that remain untreated in elderly patients undergoing DCS procedures could trigger infection.
ISS
This study states that patients subjected to DCS are more prone to developing sepsis when their ISS scores are elevated, in comparison to patients who have undergone ETC. The higher incidences of sepsis in the DCS-treated patients with high ISS scores are most likely caused by longer ventilation periods, as well as the higher incidences of severe head, chest, and abdominal trauma, which have all been recognized as relevant risk factors for unfavorable outcomes following trauma (31).
Temperature
In this study, we observe that patients who have undergone DCS exhibit a heightened susceptibility to sepsis when exposed to colder temperatures, as opposed to patients who have undergone ETC. This underscores the significant impact of lower temperatures on promoting sepsis among individuals who have undergone DCS, emphasizing a distinct contrast in the sepsis response between the two patient groups.
Leucocytes and CRP
Highly elevated leucocyte counts at admission may be an indicator of trauma burden (analogous to high ISS scores) and are therefore associated with an increased likelihood of sepsis.
Furthermore, high inflammation markers can suggest a heightened inflammation state already at admission and contribute to the development of sepsis, mainly in the DCS group. Contamination is more likely to remain untreated in the DCS group than in patients undergoing ETC.
pH and lactate
The study suggests that in the context of polytrauma patients who do not exhibit acidosis (a condition often associated with poor tissue perfusion and oxygenation), undergoing DCS procedures might somehow contribute to triggering sepsis when compared to ETC-treated patients. This might suggest that even in patients who appear relatively stable in terms of acid-base balance, there could be factors related to the DCS procedure itself that increase the risk of sepsis development.
Hemoglobin and hematocrit
Low levels of hemoglobin and hematocrit might have greater clinical implications on sepsis in patients who have undergone DCS compared to those who have been treated with ETC. In the context of trauma and surgical procedures, low hemoglobin and hematocrit levels indicate anemia, which is a risk factor for sepsis (32,33). The potential for blood loss and subsequent anemia may be more present in DCS because ISS scores are higher.
Quick
Undeniably, sepsis triggers coagulation activation and impairment of anticoagulant and fibrinolytic pathways leading to disseminated intravascular coagulation (DIC). However, it remains unanswered whether coagulopathy at admission (Quick <50 %) specifically causes more sepsis in ETC-treated polytrauma patients compared to DCS-treated patients, as in this study. Certainly, there are several other factors contributing to this aspect, including the type and extent of trauma and overall clinical management.
Generalisability
Contrary to what we anticipated, this study did not reveal the superiority of DCO in comparison to ETC regarding the occurrence of sepsis in polytrauma patients.
Both DCS and ETC strategies have their merits and challenges when it comes to sepsis development in polytrauma patients. DCS limits initial surgical insult but delays definitive treatment, potentially allowing infections to take hold. ETC provides comprehensive care promptly but might expose patients to the risk of an exaggerated immune response. The choice between these approaches depends on the patient's overall condition, the severity of injuries, and the medical team's expertise, and it underscores the complex balance between preventing complications and managing immediate threats in critically injured individuals. Finding the golden path remains very difficult.
References
- Pfeifer R, Tarkin IS, Rocos B, et al. Patterns of mortality and causes of death in polytrauma patients-Has anything changed? 40 (2009): 907-911.
- Giannoudis P. Current concepts of the inflammatory response after major trauma: An update injury 34 (2003): 397-404.
- Wafaisade A, Lefering R, Bouillon B, et al. Epidemiology and risk factors of sepsis after multiple trauma: An analysis of 29,829 patients from the Trauma Registry of the German Society for Trauma Surgery. Crit Care Med 39 (2011): 621-628.
- Kumar A, Roberts D, Wood KE, et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34 (2006): 1589-1596.
- Mica L, Niggli C, Bak P, et al. Development of a Visual Analytics Tool for Polytrauma Patients: Proof of Concept for a New Assessment Tool Using a Multiple Layer Sankey Diagram in a Single-Center Database. World J Surg 44 (2020): 764-772.
- Niggli C, Pape HC, Niggli P, et al. Validation of a visual-based analytics tool for outcome prediction in polytrauma patients (WATSON Trauma Pathway Explorer) and comparison with the predictive values of TRISS. J Clin Med 10 (2021): 698.
- Elm E von, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement?: guidelines for reporting observational studies. The Lancet 370 (2007): 1453-1457.
- Baker SP, O’Neill B, Haddon W, et al. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. Journal of Trauma 14 (1974): 187-196.
- Bone RC, Alan FCM, Robert BFA, et al. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Chest 101 (1992):1644-1655.
- Singer M, Deutschman CS, Seymour C, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). Journal of the American Medical Association. American Medical Association 315 (2016): 801-810.
- Gando S, Shiraishi A, Abe T, et al. The SIRS criteria have better performance for predicting infection than qSOFA scores in the emergency department. Sci Rep 10 (2020): 1-9.
- Brohi K, Singh J, Heron M, et al. Acute Traumatic Coagulopathy. J Trauma 54 (2003): 1127-1130.
- Rotondo MF, Schwab CW, McGonigal MD, et al. “Damage control”: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma 35 (1993): 375-382.
- Pape HC, Giannoudis P, Krettek C. The timing of fracture treatment in polytrauma patients: relevance of damage control orthopedic surgery. The American Journal of Surgery 183 (2001): 622-629.
- Brundage SI, McGhan R, Jurkovich GJ, et al. Timing of femur fracture fixation: effect on outcome in patients with thoracic and head injuries. J Trauma 52 (2002): 299-307.
- Roberts DJ, Bobrovitz N, Zygun DA, et al. Indications for use of thoracic, abdominal, pelvic, and vascular damage control interventions in trauma patients: A content analysis and expert appropriateness rating study. Journal of Trauma and Acute Care Surgery 79 (2015): 568-579.
- Pape HC, Giannoudis PV, Krettek C, et al. Timing of fixation of major fractures in blunt polytrauma role of conventional indicators in clinical decision making. J Orthop Trauma 19 (2005): 551-562.
- Nahm NJ, Vallier HA. Timing of definitive treatment of femoral shaft fractures in patients with multiple injuries: A systematic review of randomized and nonrandomized trials. Journal of trauma and acute care surgery 73 (2012): 1046-1063.
- Byrne JP, Nathens AB, Gomez D, et al. Timing of femoral shaft fracture fixation following major trauma: A retrospective cohort study of United States trauma centers. Plos Med 14 (2017): 251.
- Ruxton GD. The unequal variance t-test is an underused alternative to Student’s t-test and the Mann-Whitney U test. Behavioral Ecology 17 (2006): 688-690.
- Rasch D, Kubinger KD, Moder K. The two-sample t test: pre-testing its assumptions does not pay off. Statistical Papers 52 (2011): 219-231.
- Yan X, Abdia Y, Datta S, et al. Estimation of average treatment effects among multiple treatment groups by using an ensemble approach. Stat Med 38 (2019): 2828-2846.
- Naimi AI, Whitcomb BW. Defining and identifying average treatment effects. Am J Epidemiol 192 (2023): 685-687.
- Kurz CF. Augmented Inverse Probability Weighting and the Double Robustness Property. Medical Decision Making 42 (2022): 156-167.
- Mica L, Furrer E, Keel MTO. Predictive ability of the ISS , NISS , and APACHE II score for SIRS and sepsis in polytrauma patients. European Journal of Trauma and Emergency Surgery 38 (2021): 665-671.
- Nick TG, Campbell KM. Logistic Regression. In: Topics in Biostatistics 12 (2007): 273-301.
- von Lübken F, Prause S, Lang P, et al. Early total care or damage control orthopaedics for major fractures? Results of propensity score matching for early definitive versus early temporary fixation based on data from the trauma registry of the German Trauma Society (TraumaRegister DGU®). European Journal of Trauma and Emergency Surgery 49 (2023): 1933-1946.
- Pape HC, Rixen D, Morley J, et al. Impact of the method of initial stabilization for femoral shaft fractures in patients with multiple injuries at risk for complications (borderline patients). Ann Surg 246 (2007): 491-499.
- Bläsius FM, Laubach M, Andruszkow H, et al. Strategies for the treatment of femoral fractures in severely injured patients: trends in over two decades from the TraumaRegister DGU®. European Journal of Trauma and Emergency Surgery 48 (2022): 1769-1778.
- Roberts CS, Pape HC, Jones AL, et al. Damage Control Orthopaedics. J Bone Joint Surg 87 (2005): 23-35.
- Pape HC, Van Griensven M, Rice J, et al. Major secondary surgery in blunt trauma patients and perioperative cytokine liberation: determination of the clinical relevance of biochemical markers. J Trauma 50 (2001): 989-1000.
- Luo M, Chen Y, Cheng Y, et al. Association between hematocrit and the 30-day mortality of patients with sepsis: A retrospective analysis based on the large-scale clinical database MIMIC-IV. Plos One 17 (2022): e0265758.
- Czempik PF, Wiórek A. Iron deficiency in sepsis patients managed with divided doses of iron dextran: a prospective cohort study. Sci Rep 13 (2023): 96-105.
