The Primary Outcome of a Prospective Study: Nucleoplasty with Endoscopic Microdiscectomy
Article Information
Habeeb M Alhaboubi1*, Abdulrahman K Abuhaimed2, Mahdi Bassi3
1Department of Orthopedic Surgery, Dammam Central Hospital, Dammam, Saudi Arabia
2Department of Orthopedic Surgery, Collage of Medicine, Imam Abdulrahman Bin Faisal University, Dammam, Saudi Arabia
3Department of Orthopedic Surgery, Dr.Soliman Fakeeh Hospital, Jeddah, Saudi Arabi
*Corresponding Author: Habeeb M Alhaboubi, Department of Orthopedic Surgery, Dammam Central Hospital, Dammam, Saudi Arabia
Received: 13 May 2020; Accepted: 26 May 2020; Published: 01 June 2020
Citation:
Habeeb M Alhaboubi, Abdulrahman K Abuhaimed, Mahdi Bassi. The Primary Outcome of a Prospective Study: Nucleoplasty with Endoscopic Microdiscectomy. Journal of Spine Research and Surgery 2 (2020): 044-057.
View / Download Pdf Share at FacebookAbstract
Purpose: Evaluation of combined endoscopic microdiscectomy with Radiofreqent ablation Nucleoplasty where it is predicted to show more satisfying short-term outcome.
Study Design: A consecutive cohort of 23 patients with lumbar discogenic back pain who underwent Nucleoplasty with endoscopic microdiscectomy. Outcome measurements evaluating pain intensity and functional disability were completed preoperatively, at 1 months, at 6 months, and at the 1-year follow-up visit.
Methods: All cases (N=23) following up with confirmed diagnosis of contained lumber discogenic back pain, who failed conservative treatment and fulfilled the criteria for surgical intervention, then underwent endoscopic microdiscectomy with nucleoplasty, and followed up by regular clinic visits for a period of one year maximum. Primary outcome variables that are going to be used in the research is Visual analogue scale (out of 10) and the Oswestry disability index (out of 100).
Results: Of the 23-patient cohort, the 1 year follow up rate was at 100%. The mean VAS for low back pain preoperatively, postoperatively, 1 month, 6 months, and 1 year were 9.17, 6.04, 4.57, 2.02 respectively. The functional assessment was evaluated using ODI and showed a mean of 52.75 preoperatively, and 34.96 at 1 month post operatively, 29.30 at 6 months post operatively, and 16.96 at year post operatively.
Conclusion: In this minimal invasive approach, Nucleoplasty with Endoscopic Microdiscectomy, it showed promising short-term outcomes with less post-operative pain, hospital stay, minimal blood loss and no reported post-operative complication which can be an alternative option to the standard open Microdiscectomy.
Keywords
Nucleoplasty, Minimal invasive, Lumbar disc herniation, Microdiscectomy
Nucleoplasty articles Nucleoplasty Research articles Nucleoplasty review articles Nucleoplasty PubMed articles Nucleoplasty PubMed Central articles Nucleoplasty 2023 articles Nucleoplasty 2024 articles Nucleoplasty Scopus articles Nucleoplasty impact factor journals Nucleoplasty Scopus journals Nucleoplasty PubMed journals Nucleoplasty medical journals Nucleoplasty free journals Nucleoplasty best journals Nucleoplasty top journals Nucleoplasty free medical journals Nucleoplasty famous journals Nucleoplasty Google Scholar indexed journals Minimal invasive articles Minimal invasive Research articles Minimal invasive review articles Minimal invasive PubMed articles Minimal invasive PubMed Central articles Minimal invasive 2023 articles Minimal invasive 2024 articles Minimal invasive Scopus articles Minimal invasive impact factor journals Minimal invasive Scopus journals Minimal invasive PubMed journals Minimal invasive medical journals Minimal invasive free journals Minimal invasive best journals Minimal invasive top journals Minimal invasive free medical journals Minimal invasive famous journals Minimal invasive Google Scholar indexed journals Lumbar disc herniation articles Lumbar disc herniation Research articles Lumbar disc herniation review articles Lumbar disc herniation PubMed articles Lumbar disc herniation PubMed Central articles Lumbar disc herniation 2023 articles Lumbar disc herniation 2024 articles Lumbar disc herniation Scopus articles Lumbar disc herniation impact factor journals Lumbar disc herniation Scopus journals Lumbar disc herniation PubMed journals Lumbar disc herniation medical journals Lumbar disc herniation free journals Lumbar disc herniation best journals Lumbar disc herniation top journals Lumbar disc herniation free medical journals Lumbar disc herniation famous journals Lumbar disc herniation Google Scholar indexed journals Microdiscectomy articles Microdiscectomy Research articles Microdiscectomy review articles Microdiscectomy PubMed articles Microdiscectomy PubMed Central articles Microdiscectomy 2023 articles Microdiscectomy 2024 articles Microdiscectomy Scopus articles Microdiscectomy impact factor journals Microdiscectomy Scopus journals Microdiscectomy PubMed journals Microdiscectomy medical journals Microdiscectomy free journals Microdiscectomy best journals Microdiscectomy top journals Microdiscectomy free medical journals Microdiscectomy famous journals Microdiscectomy Google Scholar indexed journals low back pain articles low back pain Research articles low back pain review articles low back pain PubMed articles low back pain PubMed Central articles low back pain 2023 articles low back pain 2024 articles low back pain Scopus articles low back pain impact factor journals low back pain Scopus journals low back pain PubMed journals low back pain medical journals low back pain free journals low back pain best journals low back pain top journals low back pain free medical journals low back pain famous journals low back pain Google Scholar indexed journals sciatica articles sciatica Research articles sciatica review articles sciatica PubMed articles sciatica PubMed Central articles sciatica 2023 articles sciatica 2024 articles sciatica Scopus articles sciatica impact factor journals sciatica Scopus journals sciatica PubMed journals sciatica medical journals sciatica free journals sciatica best journals sciatica top journals sciatica free medical journals sciatica famous journals sciatica Google Scholar indexed journals neurological deficit articles neurological deficit Research articles neurological deficit review articles neurological deficit PubMed articles neurological deficit PubMed Central articles neurological deficit 2023 articles neurological deficit 2024 articles neurological deficit Scopus articles neurological deficit impact factor journals neurological deficit Scopus journals neurological deficit PubMed journals neurological deficit medical journals neurological deficit free journals neurological deficit best journals neurological deficit top journals neurological deficit free medical journals neurological deficit famous journals neurological deficit Google Scholar indexed journals Radiofreqent ablation articles Radiofreqent ablation Research articles Radiofreqent ablation review articles Radiofreqent ablation PubMed articles Radiofreqent ablation PubMed Central articles Radiofreqent ablation 2023 articles Radiofreqent ablation 2024 articles Radiofreqent ablation Scopus articles Radiofreqent ablation impact factor journals Radiofreqent ablation Scopus journals Radiofreqent ablation PubMed journals Radiofreqent ablation medical journals Radiofreqent ablation free journals Radiofreqent ablation best journals Radiofreqent ablation top journals Radiofreqent ablation free medical journals Radiofreqent ablation famous journals Radiofreqent ablation Google Scholar indexed journals Oswestry disability index articles Oswestry disability index Research articles Oswestry disability index review articles Oswestry disability index PubMed articles Oswestry disability index PubMed Central articles Oswestry disability index 2023 articles Oswestry disability index 2024 articles Oswestry disability index Scopus articles Oswestry disability index impact factor journals Oswestry disability index Scopus journals Oswestry disability index PubMed journals Oswestry disability index medical journals Oswestry disability index free journals Oswestry disability index best journals Oswestry disability index top journals Oswestry disability index free medical journals Oswestry disability index famous journals Oswestry disability index Google Scholar indexed journals
Article Details
Introduction
Lumbar disc herniation can cause central canal stenosis or spinal nerve root compression. The local inflammatory response and the anatomical features of the herniated disc and spinal canal determine the resultant clinical syndrome which may include low back pain, and sciatica with or without neurological deficit [1]. In nations like the United States, its prevalence is between 8% and 57%. According to the estimate provided by the experts, nearly 29% of individuals encounter a low back pain that could disable the individual at a certain stage of his or her life [2] Mainstay of treatment for patients with radicular pain due to lumbar disc herniation involves open lumbar discectomy, and has provided excellent outcome in over six decades [3, 4].
1.1 Aim (hypothesis)
Evaluation of combined endoscopic microdiscectomy with Radiofreqent ablation Nucleoplasty where it is predicted to show more satisfying short-term outcome, this includes shorter hospital stay, minimal blood loss, less operation time, less post- operative pain, less soft tissue injury, no reported post-operational complications (infections, post laminectomy syndrome, dural tear, and nerve root injury), and this are to be considered as our outcome variables. With comparison to the gold standard open microscopic discectomy, it is predicted to show similar long term outcome in both, pain relieve and restoration of functional activity.
1.2 Background and significance (Literature review)
Nucleoplasty (percutaneous lumbar disc decompression) is a minimally invasive procedure that utilizes radiofrequency energy as a treatment for symptomatic lumbar disc herniation, against open microdiscectomy, which would be the mainstay treatment modality. The literature reports a favorable outcome in up to 77% of patients at 6 months [5]. Minimal invasive approach for surgical treatment of discogenic back pain has increased in popularity in the recent years and was regarded as a feasible alternative option to the standard open microdiscectomy. According to one study, Patients were randomized in two groups receiving Either MAMD (minimal access microdiscectomy) or SOMD (standard open microdiscectomy). Physical and mental health and pain relief were assessed (ODI, SF-36 questionnaire, VAS leg and back pain). Results Of the 60 initial patients (SOMD: 30 pts, MAMD: 30 pts), 38 were available for long-term follow-up. Mean follow-up time was 33 months. Long-term follow-up revealed significant postoperative pain relief in both groups. Good to excellent results concerning physical and mental health and pain relief were achieved in both groups. Significantly less peridural scar tissue formation was observed in the MAMD patients, but without clinical impact. In conclusion, MAMD is a feasible alternative to the standard open approach. Both groups show significant and long-lasting pain relief and good to excellent results regarding health-related quality of life [6]. In a prospective outcome predictor study, 87 patients who underwent percutaneous endoscopic lumbar discectomy and thermal annuloplasty (PELDTA) for discogenic low back pain (DLBP). Clinical outcomes were assessed using the visual analog scale (VAS), the Oswestry disability index (ODI), and the modified MacNab criteria. The univariate and multivariate analyses were performed to evaluate the outcome predictors. The VAS and ODI scores at postoperative 6 months and 2 years were significantly improved (p< 0.001). Based on the modified MacNab criteria, the global outcomes were excellent in 39 out of 79 patients (49.4%), good in 17 patients (21.5%), fair in 10 patients (12.7%), and poor in 13 patients (16.5%). Therefore, the percentage of symptomatic improvement was 83.5% and the success rate (excellent or good) was 70.9%. In the univariate and multivariate analyses, the presence of concurrent disc herniation with DLBP was the most significant predictor (OR=3.207, 95% CI 1.02–10.06, p=0.046). As a Conclusions, PELDTA may be effective for patients with chronic DLBP in selected cases. Central disc herniation causing DLBP was the most important predictor for clinical success [7].
2. Method
A consecutive cohort of 23 patients with lumbar discogenic back pain who underwent Nucloplasty with endoscopic microdiscectomy between December/13/ 2014 to July/6/2016 were included in this prospective study. Patients were operated by the one surgeon, who used the same surgical technique at the same institution for the study period. All cases (N=23) following up at the orthopedic department with confirmed diagnosis of contained lumber discogenic back pain, who failed conservative treatment and fulfilled the criteria for surgical intervention, then underwent endoscopic microdiscectomy with Nucleoplasty, and followed up by regular clinic visits for a period of one year maximum. Questionnaires with outcome measurements evaluating pain intensity and functional disability were completed preoperatively, at 1 months, at 6 months, and at the 1-year follow-up visit or during telephone interviews by the independent observer. At each follow-up, the pain intensity of the low back pain was measured using a visual analog scale (VAS, 0–10 points), and the functional status was assessed using the Oswestry disability index (ODI). All patients are instructed to fill VAS and ODI survey through every visit (Preoperational, 1 month post operation, 6 months post-operation, and 1 year post-operation), where they were instructed and assisted by healthcare professionals throughout the process. Data was collected through OAISIS electronic healthcare system where all of the information were documented and acquired by co-investigators and not the main surgeon himself. No exclusion based on BMI or preoperative history of trauma was done. All patients were contacted individually via telephone and e-mail for conformation and accurate input of data and outcome subjective satisfaction of the operation. Inclusive criteria include Intractable chronic low back pain without improvement after conservative treatment for 6 months, Central or posterolateral (paracentral) contained disc herniation (Grade I and II) on magnetic resonance imaging, No history of previous back surgery, Age range from 20 to 75 years old, Level of surgery range between L3 to S1. Exclusive criteria include Age below 20 and above 75, Lateral recess stenosis, sequestrated disc, Fractures, tumors, or infections, Extruded or sequestrated herniations on magnetic resonance imaging, Non lumber disc herniation, Concurrent back pain due to other pathologies, Congenital spinal anomalies, Cases with Oswestery more than 70 , or less than 40. Primary outcome variables that are going to be used in the research is Visual analogue scale (out of 10), the Oswestry disability index (out of 100), and outcome subjective satisfaction. Secondary outcome variables that are going to be used in the research are length of operation, length of hospital stay, blood loss, postoperative infections, dural tear, reoperation, and nerve root injury. Other variables are age, gender, level of surgery, patient occupation, smoking, comorbidities, alcohol intake, history of trauma, use of steroids, sitting intolerance, and body mass index.
2.1 Surgical technique
all patient underwent general anesthesia , and positioned
on Jackson's table prone position , after confirmation of the level with C-arm, standard prep and drape was done, using one C-Arm the fluoroscope was taken lateral and the arm were moved to oblique position until the scotch view appear (Figure 1), then a guide needle passed vertically toward the middle third of the disc ( Kambin Triangle, Figure 2 and 5 ) and a dilator passed though 8 mm incision with the portal, the positioned was checked in two planned AP and Lateral , then the endoscope thorough the portal passed until it reach the lateral border of the pedicle, using the Camera to protect the nerve root and the dura, a sharp knife penetrate the disc then using scissors and Pituitary the disc were taken until 1/3 of the disc were out (Figure 3 and 6), a radiofrequent ablation then take place (Figure 4), local xylocain 2% with depomedrole, the skin closed by 0.3 suture.
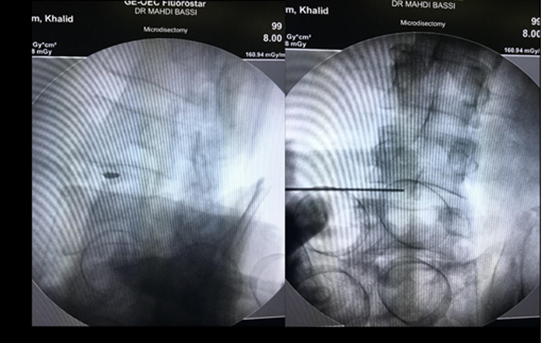
Figure 1: The needle guide. (A) AP; (B) Posterolateral.
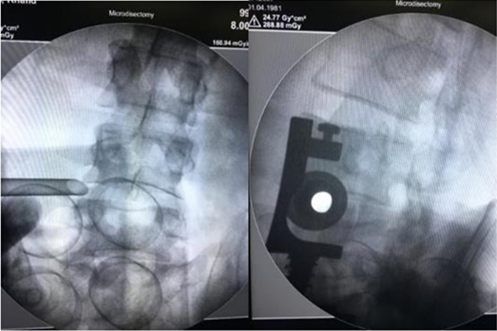
Figure 2: The working channel positioned at kambin tringle. (A) AP; (B) Posteolateral.
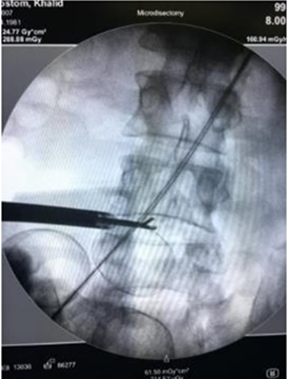
Figure 3: Using the non toothed pituitary.
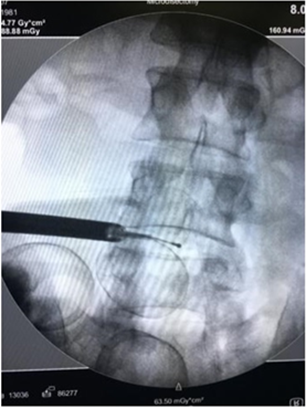
Figure 4: The tip of nucleoplasty probe in the middle of the disc.
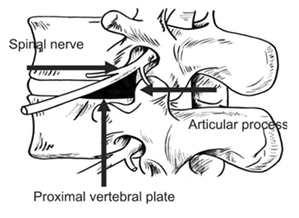
Figure 5: Schematic description of kambin triangle.
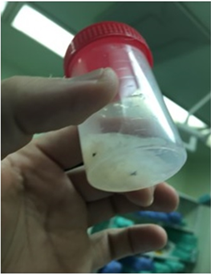
Figure 6: Sample of removed disc material.
2.2 Statistical analysis
Statistical results were conducted using SPSS to asses statistical significance in the primary outcomes of VAS and ODI preoperatively and postoperatively at 1 month, 6 month and 1 year and to establish any correlation between different variables which are used in this study. P < 0.05 was considered significant.
3. Result
3.1 Patient characteristics
Of the 23-patient cohort, the 1 year follow up rate was at 100%. The mean age was 41.6 ± 12.3 years (Range 22 – 74). The study had 15 men and 8 women. 22 patients had a single level and 1 had a two-level procedure, therefore 24 discs were treated with PELDRN (Percutaneous Endoscopic Microdiscectomy and Radiofrequant Nucleoplasty). The most common segment was L4-L5 (82.6%) and L5-S1 (8.7%). The procedure was primary for 91% of the patients and a revision for 8.7%. Site of radiculopathy was assigned left, right, or bilateral with distribution of 43.5%, 34.8%, and 21.7% respectively. 21.7% of patients were smokers, 78.3% were nonsmokers. 30.4% had history of trauma before the onset of their symptoms, while 69.6% didn’t. Eleven patients (47.8%) had potentially contributing comorbidities. Usage of steroids among the patients was at 8.7%. sitting intolerance was positive in 21.7%. The mean body mass index was 30 ± 9 (Range 17.5 – 63). Among the patients 65.2% had Herniation only while 34.8% had a concurrent degenerative disc disease, 69.6% had a single herniation, while 30.4% had a grouped herniation. The duration of symptoms in months was recorded with a mean of 47.57 ± 75. (Table 1 and 2).
3.2 Visual analogue scale scores and the Oswestry disability index assessment
The mean VAS for low back pain preoperatively, postoperatively, 1 month, 6 months, and 1 year were 9.17 ± 0.887, 6.04 ± 2.246, 4.57 ± 2.019, 2.02 ± 1.379 respectively. The functional assessment was evaluated using ODI and showed a mean of 52.75 ± 14.303 preoperatively, and 34.96 ± 20.171 1 month post operatively, 29.30 ± 17.504 6 months post operatively, and 16.96 ± 9.833 1 year post operatively. (Table 3).
3.3 Operation parameters and complications
Of the 23-patient cohort, length of operation showed an average of 1 hour and 13 mins ± 25 mins (Range 30 mins – 2 hours). Length of hospitalization showed an average of 2 days ± 1 day (Range 1 day – 5 days). Of this group of patients, there were no complications or sign and symptoms of post-operative infections, nerve root injury, deep venous thrombosis, dural tear (noticed during the procedure or any of its signs or symptoms during the follow up) (Table 2). A one way repeated measured analysis of variance (ANOVA) was conducted to evaluate the null hypothesis that there is no change in VAS when measured preoperatively, 1 month post-operatively, 6 months post-operatively, and 1 year post-operatively in the designated group (n=23). The result of the ANOVA indicated a significant time effect, Wilks’ Lambda = 0.035, F (3 , 20)=186.2, p < 0.01, ?² = 0.96. Thus there is significance evidence to reject the null hypothesis (Table 4). Three paired samples t-tests were used to make post hoc comparisons between conditions. A first paired samples t-test indicated that there was a significant difference in the VAS score preoperatively (M=9.17, SD=0.887) and 1 month post operatively (M=6.04, SD=2.246) conditions;t(22)=5.663, p<0.01. A second paired samples t-test indicated that there was a significant difference in the VAS score preoperatively (M=9.17, SD=0.887) and 6 months post-operatively (M=4.57, SD=2.019) conditions;t(22)=9.406, p<0.01. A third paired samples t-test indicated that there was a significant difference in the VAS score preoperatively (M=9.17, SD=0.887) and 1 year post-operatively (M=2.02, SD=1.379) conditions; t(22)=22.144, p<0.01 (Table 5). These results suggest that our procedure have a significant effect on the visual analogue scale pain score (Figure 8). Specifically, our results show that individuals undergoing the procedure display a significant decrease in the reported VAS score over time. The same analysis was conducted to evaluate the null hypothesis that there is no change in ODI when measured preoperatively, 1 month post-operatively, 6 months postoperatively, and 1 year post-operatively in the designated group (n=23). The result of the ANOVA indicated a significant time effect, Wilks’ Lambda =0.091 F (3 , 20)= 66.876, p < 0.01, ?² = 0.90. Thus there is significance evidence to reject the null hypothesis (Table 4). Follow up three paired samples t-tests were used to make post hoc comparisons between conditions. A first paired samples t-test indicated that there was a significant difference in the ODI score preoperatively (M=52.75, SD=14.303) and 1 month post operatively (M=34.96, SD=20.171) conditions; t(22)=3.398, p<0.01. A second paired samples t-test indicated that there was a significant difference in the ODI score preoperatively (M=52.75, SD=14.303) and 6 months post-operatively (M=29.30, SD=17.504) conditions; t(22)=5.135, p<0.01. A third paired samples t-test indicated that there was a significant difference in the ODI score preoperatively (M=52.75, SD=14.303) and 1 year post-operatively (M=16.96, SD=9.833) conditions; t(22)=11.457, p=0.015 (Table 6).
|
Data |
No. of patients |
Percentage % |
|
Gender |
||
|
Female |
8 |
34.8 |
|
Male |
15 |
65.2 |
|
Spine level operated |
||
|
L5-S1 |
2 |
8.7 |
|
L4-L5 |
19 |
82.6 |
|
L3-L4 |
1 |
4.3 |
|
L4-S1 |
1 |
4.3 |
|
Primary vs revision |
||
|
Primary |
21 |
91.3 |
|
Revision |
2 |
8.7 |
|
Site of radiculopathy |
||
|
Left |
10 |
43.5 |
|
Right |
8 |
34.8 |
|
Bilateral |
5 |
21.7 |
|
Smoking |
||
|
No |
18 |
78.3 |
|
Yes |
5 |
21.7 |
|
History of trauma |
||
|
Negative |
16 |
69.6 |
|
Positive |
7 |
30.4 |
|
Use of steroid |
||
|
No |
21 |
91.3 |
|
Yes |
2 |
8.7 |
|
Sitting intolerance |
||
|
Present |
5 |
21.7 |
|
Absent |
18 |
78.3 |
|
Concurrent disc herniation and degeneration vs Herniation only |
||
|
Herniation only |
15 |
65.2 |
|
Herniation plus DDD |
8 |
34.8 |
|
Grouped herniation vs non grouped herniation |
||
|
Single |
16 |
69.6 |
|
Grouped |
7 |
30.4 |
Table 1: Descriptive statistics of frequencies among patients.
|
Data |
Minimum |
Maximum |
Mean |
Std. Deviation |
|
Age |
22 |
74 |
41.61 |
± 12.320 |
|
Body mass index |
17.5 |
63 |
30.013 |
± 9.0810 |
|
Chronicity |
1 |
300 |
47.57 |
± 75.212 |
|
Length of operation |
0.50 (30 mins) |
2 |
1.23 (1hr13mins) |
± .42062 |
|
Length of hospitalization |
1 |
5 |
1.78 |
± .951 |
Table 2: Descriptive Statistics of variables.
|
Data |
Preoperation |
1 months post-operation |
6 months post-operation |
1 year post-operation |
|
VAS score (Mean ± SD) |
9.17 ± 0.887 |
6.04 ± 2.246 |
4.57 ± 2.019 |
2.02 ± 1.379 |
|
ODI score (Mean ± SD) |
52.75 ± 14.303 |
34.96 ± 20.171 |
29.30 ± 17.504 |
16.96 ± 9.833 |
Table 3: Descriptive Statistics of VAS and ODI.
|
Value |
F |
Hypothesis df |
Error df |
Sig. |
Partial Eta Squared |
|||
|
VAS |
Wilks' lambda |
0.035 |
186.229 |
3 |
20 |
0 |
0.965 |
|
|
ODI |
Wilks' lambda |
0.091 |
66.876b |
3 |
20 |
0 |
0.909 |
|
Table 4: Multivariate test of VAS and ODI.
|
(I) |
(J) |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval for Difference |
||
|
VAS |
VAS |
Lower Bound |
Upper Bound |
T score |
|||
|
1 |
2 |
3.13 |
0.553 |
0 |
1.528 |
4.733 |
5.663 |
|
3 |
4,609 |
0.49 |
0 |
3.188 |
6.029 |
9.406 |
|
|
4 |
7.087 |
0.32 |
0 |
6.159 |
8.015 |
22.144 |
|
1 = VAS preoperation, 2 = VAS 1 month postoperation, 3 = VAS 6 months postoperation, 4 = VAS 1 year postoperation
Table 5: Pairwise Comparisons for VAS.
|
(I) ODI |
(J) ODI |
Mean Difference (I-J) |
Std. Error |
Sig. |
95% Confidence Interval for Difference |
T score |
|
|
Lower Bound |
Upper Bound |
||||||
|
1 |
2 |
17.783* |
5.233 |
0.015 |
2.615 |
32.95 |
3.398 |
|
3 |
23.435* |
4.563 |
0 |
10.207 |
36.662 |
5.135 |
|
|
4 |
35.783* |
3.123 |
0 |
26.73 |
44.836 |
11.457 |
|
1 = ODIpreoperation, 2 = ODI 1 month postoperation, 3 = ODI 6 months postoperation, 4 = ODI 1 year postoperation
Table 6: Pairwise Comparisons of ODI.
4. Discussion
These results suggested that our procedure have a significant effect on the Oswestry disability index. Specifically, our results show that individuals undergoing the procedure display a significant decrease in the reported ODI score over time (Figure 7). Further analysis of the other variables showed no significant relationship with age, gender, history of trauma, comorbidities, usage of steroids, herniation only vs herniation and degenerative disc disease, single herniation vs grouped herniation (Table 7). On the other hand, results show significantly better results when the operation is done as a primary procedure, rather than a revision (Table7). Results also displayed significantly better results with non-smokers and non-obese patients with regards to the disability index (Figure 9 and 10).
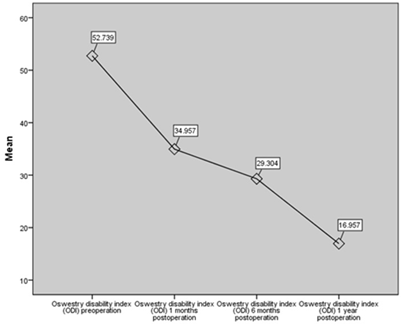
Figure 7: Chat of Oswestry Disability index (ODI) preoperative, 1 month, 6 months and 1 year post operative.
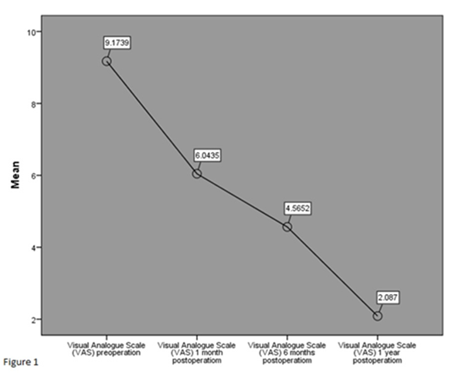
Figure 8: Chart of visual analogur scale (VAS) preoperative, 1 month, 6 months and 1 year post operative.
|
Parameters |
p value with VAS |
p value with ODI |
|
Age |
0.74 |
0.59 |
|
Gender |
0.91 |
0.95 |
|
Primary vs revision |
0.003* |
0.019* |
|
Smoking |
0.062 |
0.024* |
|
History of trauma |
0.298 |
0.216 |
|
Comorbidities |
0.357 |
0.698 |
|
Usage of steroid |
0.7 |
0.7 |
|
Sitting intolerance |
0.359 |
0.301 |
|
BMI |
0.321 |
0.021* |
|
Herniation only vs herniation and DDD |
0.429 |
0.544 |
|
Single herniation vs grouped |
0.676 |
0.852 |
*statistically significant value.
Table 7: Analysis for geometric and demographic parameters.
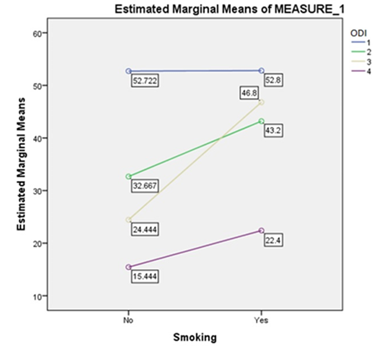
Figure 9: The effect of smoking on ODI score.
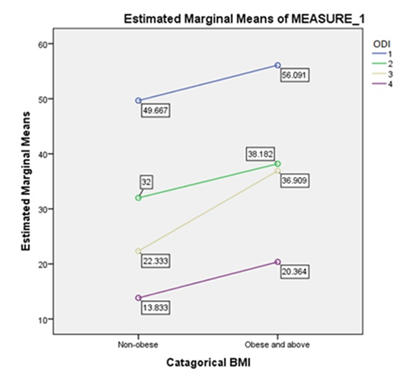
Figure 10: The effect of body mass index (BMI) on ODI score.
5. Conclusion
In this minimal invasive approach, Nucleoplasty with Endoscopic Microdiscectomy, it showed promising short-term outcomes with less post-operative pain, hospital stay, minimal blood loss and no reported post-operative complication which can be an alternative option to the standard open Microdiscectomy.
Limitation
Limitation of this study include small sample size and non-randomized selection of the samples.
References
- Long DM. Decision making in lumbar disc disease. Clinical neurosurgery 39 (1992): 36-51
- Manchikanti L. Epidemiology of low back pain. Pain physician 3 (2000): 167-192
- Williams RW. Microlumbar discectomy: a conservative surgical approach to the virgin herniated lumbar disc. Spine 3 (1978): 175-182
- Yorimitsu E, Chiba K, Toyama Y, et al. Long-term outcomes of standard discectomy for lumbar disc herniation: a follow-up study of more than 10 years. Spine 26 (2001): 652-657
- Ogbonnaya S, Kaliaperumal C, Qassim A, et al. Outcome of nucleoplasty in patients with radicular pain due to lumbar intervertebral disc herniation. Journal of Natural Science, Biology, and Medicine 4 (2013): 187-190.
- Gempt J, Jonek M, Ringel F, et al. Long-term follow-up of standard microdiscectomy versus minimal access surgery for lumbar disc herniations. Acta Neurochir (Wien) 155 (2013): 2333-2338.
- Ahn Y, Lee S-H. Outcome predictors of percutaneous endoscopic lumbar discectomy and thermal annuloplasty for discogenic low back pain. Acta Neurochirurgica 152 (2010): 1695-1702.
