The Impact of Insecurity on the Care of Pregnant Women in the Democratic Republic of the Congo: A Cross-Sectional Study
Article Information
Michel DIKETE EKANGA1, Philippe SIMON1, Yves COPPIETERS3, Anne DELBAERE1, Clotilde LAMY1, WEI-HONG ZHANG4, KASUNZU HAKIZIMANA5, JOLIE KINJA5, ALINE KATEREKWA5, MARIE-IMMACULEE KASELA KAPUNGWE6, Michel Kyembwa2, Richard KABUYANGA KABUSEBA2
1Free University of Brussels, University clinics of Brussels, Erasmus Hospital, Obstetric Gynecology Department. Belgium
2North Kivu Provincial Hospital, Goma, DR Congo
3Free University of Brussels, School of Public Health, Center for Research in Epidemiology, Biostatistics and clinical Research, Belgium
4International Center for Reproductive Health, Department of Public Health and Primary Care, Faculty of Medicine and Health Sciences, Ghent University, Belgium,
5Rutshuru Provincial Regional Hospital, Kivu, DR Congo
6Pamela Kasavubu Hospital, Kinshasa, DR Congo
*Corresponding Author: Michel DIKETE EKANGA, Free University of Brussels, University clinics of Brussels, Erasmus Hospital, Obstetric Gynecology Department, Belgium.
Received: 01 June 2023; Accepted: 09 June 2023; Published: xx July 2023
Citation: Michel DIKETE EKANGA, Philippe SIMON, Yves COPPIETERS, Anne DELBAERE, Clotilde LAMY, WEI-HONG ZHANG, KASUNZU HAKIZIMANA, JOLIE KINJA, ALINE KATEREKWA, MARIE-IMMACULEE KASELA KAPUNGWE, Michel Kyembwa, Richard KABUYANGA KABUSEBA. The Impact of Insecurity on the Care of Pregnant Women in the Democratic Republic of the Congo: A Cross- Sectional Study. Obstetrics and Gynecology Research. 6 (2023): 188-196
View / Download Pdf Share at FacebookAbstract
Introduction:
The highest levels of maternal mortality and obstetric complications are found in conflict and post-conflict areas, where the number of maternal deaths per 100,000 live births is generally above 800. According to a recent analysis of demographic data and healthcare surveys, local exposure to incidents of armed conflict increases the risk of mortality during pregnancy and delivery by 10% for each additional incident recorded. The purpose of our study is to analyse the care and outcomes of deliveries at Rutshuru General Hospital, which is located in the east of the Democratic Republic of the Congo, in a region faced with insecurity.
Materials and methods:
The reference population was recruited at the Rutshuru General Hospital (North Kivu) between September 2021 and January 2022. It is an observational, prospective, descriptive and analytical study examining all deliveries that occurred during the study period. The normality test of continuous variables was applied using graphs (histograms, box plots). The median and interquartile range were calculated to describe asymmetrical distributions. The mean and standard deviation were calculated to describe normally distributed variables. Associations between delivery via caesarean section and the various explanatory variables were analysed using logistic regression.
Results:
1,243 patients delivered at the Rutshuru General Hospital during the period studied. The average age of our population was 25 years. The majority of the women were married (93.5%), had no level of education (74.3%) and no profession (93.7%). 45% of patients had a prior history of caesarean sections. The percentage of caesarean sections in this study was 52.1%. The incision was most commonly transverse (84.5%) and the type of anaesthesia used was most commonly locoregional (spinal anaesthesia) (99.4%). 11% of deliveries included intra-operative complications and 89% of new-borns did not require intensive neonatal care and were with their mothers. Maternal mortality was estimated at 0.5%, with an average length of stay of seven days.
Conclusions:
Insecurity resulting from armed conflicts had a negative impact on the education, employment and socio-economic status of the population and, as a result of this, poor care for pregnant woman. This story shows that new-borns delivered via caesarean section have a lower risk of perinatal complications that new-borns delivered via vaginal delivery in areas faced with insecurity as a result of armed conflicts. We observed, however, a higher number of maternal complications following delivery via caesarean section than via vaginal delivery.
Keywords
Maternal Deaths; Pregnancy; Caesarean Section; Republic of the Congo
Maternal Deaths articles Maternal Deaths Research articles Maternal Deaths review articles Maternal Deaths PubMed articles Maternal Deaths PubMed Central articles Maternal Deaths 2023 articles Maternal Deaths 2024 articles Maternal Deaths Scopus articles Maternal Deaths impact factor journals Maternal Deaths Scopus journals Maternal Deaths PubMed journals Maternal Deaths medical journals Maternal Deaths free journals Maternal Deaths best journals Maternal Deaths top journals Maternal Deaths free medical journals Maternal Deaths famous journals Maternal Deaths Google Scholar indexed journals Pregnancy articles Pregnancy Research articles Pregnancy review articles Pregnancy PubMed articles Pregnancy PubMed Central articles Pregnancy 2023 articles Pregnancy 2024 articles Pregnancy Scopus articles Pregnancy impact factor journals Pregnancy Scopus journals Pregnancy PubMed journals Pregnancy medical journals Pregnancy free journals Pregnancy best journals Pregnancy top journals Pregnancy free medical journals Pregnancy famous journals Pregnancy Google Scholar indexed journals Caesarean Section articles Caesarean Section Research articles Caesarean Section review articles Caesarean Section PubMed articles Caesarean Section PubMed Central articles Caesarean Section 2023 articles Caesarean Section 2024 articles Caesarean Section Scopus articles Caesarean Section impact factor journals Caesarean Section Scopus journals Caesarean Section PubMed journals Caesarean Section medical journals Caesarean Section free journals Caesarean Section best journals Caesarean Section top journals Caesarean Section free medical journals Caesarean Section famous journals Caesarean Section Google Scholar indexed journals Republic of the Congo articles Republic of the Congo Research articles Republic of the Congo review articles Republic of the Congo PubMed articles Republic of the Congo PubMed Central articles Republic of the Congo 2023 articles Republic of the Congo 2024 articles Republic of the Congo Scopus articles Republic of the Congo impact factor journals Republic of the Congo Scopus journals Republic of the Congo PubMed journals Republic of the Congo medical journals Republic of the Congo free journals Republic of the Congo best journals Republic of the Congo top journals Republic of the Congo free medical journals Republic of the Congo famous journals Republic of the Congo Google Scholar indexed journals sexual violence articles sexual violence Research articles sexual violence review articles sexual violence PubMed articles sexual violence PubMed Central articles sexual violence 2023 articles sexual violence 2024 articles sexual violence Scopus articles sexual violence impact factor journals sexual violence Scopus journals sexual violence PubMed journals sexual violence medical journals sexual violence free journals sexual violence best journals sexual violence top journals sexual violence free medical journals sexual violence famous journals sexual violence Google Scholar indexed journals midwives articles midwives Research articles midwives review articles midwives PubMed articles midwives PubMed Central articles midwives 2023 articles midwives 2024 articles midwives Scopus articles midwives impact factor journals midwives Scopus journals midwives PubMed journals midwives medical journals midwives free journals midwives best journals midwives top journals midwives free medical journals midwives famous journals midwives Google Scholar indexed journals maternal age articles maternal age Research articles maternal age review articles maternal age PubMed articles maternal age PubMed Central articles maternal age 2023 articles maternal age 2024 articles maternal age Scopus articles maternal age impact factor journals maternal age Scopus journals maternal age PubMed journals maternal age medical journals maternal age free journals maternal age best journals maternal age top journals maternal age free medical journals maternal age famous journals maternal age Google Scholar indexed journals child weight articles child weight Research articles child weight review articles child weight PubMed articles child weight PubMed Central articles child weight 2023 articles child weight 2024 articles child weight Scopus articles child weight impact factor journals child weight Scopus journals child weight PubMed journals child weight medical journals child weight free journals child weight best journals child weight top journals child weight free medical journals child weight famous journals child weight Google Scholar indexed journals perinatal morbidity articles perinatal morbidity Research articles perinatal morbidity review articles perinatal morbidity PubMed articles perinatal morbidity PubMed Central articles perinatal morbidity 2023 articles perinatal morbidity 2024 articles perinatal morbidity Scopus articles perinatal morbidity impact factor journals perinatal morbidity Scopus journals perinatal morbidity PubMed journals perinatal morbidity medical journals perinatal morbidity free journals perinatal morbidity best journals perinatal morbidity top journals perinatal morbidity free medical journals perinatal morbidity famous journals perinatal morbidity Google Scholar indexed journals Public Health articles Public Health Research articles Public Health review articles Public Health PubMed articles Public Health PubMed Central articles Public Health 2023 articles Public Health 2024 articles Public Health Scopus articles Public Health impact factor journals Public Health Scopus journals Public Health PubMed journals Public Health medical journals Public Health free journals Public Health best journals Public Health top journals Public Health free medical journals Public Health famous journals Public Health Google Scholar indexed journals
Article Details
Introduction
The highest levels of maternal mortality and obstetric complications are found in conflict and post-conflict areas[1], where the number of maternal deaths per 100,000 live births is generally above 800. According to a recent analysis of demographic data and healthcare surveys, local exposure to incidents of armed conflict increases the risk of mortality during pregnancy and delivery by 10% for each additional incident recorded[2]. There is evidence at the national level that countries experiencing high levels of armed conflict tend to have higher maternal mortality rates (MMR). However, during an armed conflict the actual combat is generally confined to a limited area within the country, affecting a subset of the population[2]. In the regions of Africa currently experiencing conflict or post-conflict, populations are poorer and have higher rates of illiteracy, and fertility rates are high[2]. Difficulties in monitoring pregnancies and providing care during delivery may be an especially significant cause of the increase in maternal and perinatal mortality in these conflict areas. Insecurity arising from conflicts disrupts healthcare systems, including the availability of infrastructure, human resources, food, rapid communication and good governance[3,4]. Insecurity may also increase the time it takes to access basic obstetric care. Woman may delay their decision to request care or face undue transport delays when routes are not safe, which hinders travel to healthcare facilities. They may also experience delays in receiving quality care in healthcare facilities and pharmacies in insecure areas due to damaged infrastructure, as well as shortages in supplies and human resources. Due to the insecurity and the resulting lack of employment, women may not have sufficient financial resources to pay the costs for adequate healthcare[5]. The Democratic Republic of the Congo (DRC) has faced insecurity, human rights abuses and displacement of populations linked to armed conflicts since 1996, especially in the east of the country. Sexual violence is common[6,7] and used as weapon of war. Mukwege et al.[8], have examined sexual violence in armed conflicts by interviewing combatants in South Kivu about their experience of sexual violence, what they think the cause may be, and how it could be reduced. The combatants questioned stated that they wanted to protect women and men during armed conflicts, but the contexts in which they operated led them, against their wishes, to adopt violent behaviours towards civilians they were supposed to be protecting. Although there are ample studies in the literature describing the mechanisms by which conflicts affect access to healthcare, few studies examine the impact of conflicts on the use of maternal healthcare, and report mixed findings[9]. Maternal mortality rates can be negatively impacted by armed conflicts, which indicates a higher level of vulnerability among women and which is often connected to the absence or limited access to maternal healthcare during conflicts. Previous research in Uganda showed that armed conflicts have a negative impact on the use of maternal healthcare services by women for a number of individual or political reasons or issues relating to the healthcare system[10]. The purpose of our study is to analyse the care and outcomes of deliveries at Rutshuru General Hospital in order to make proposals to improve the quality of care in the east of the Democratic Republic of the Congo, in a region faced with insecurity.
Materials and method
The reference population was recruited at the Rutshuru General Hospital (North Kivu) between September 2021 and January 2022. Rutshuru General Hospital is the general referral hospital for the Rutshuru health zone, which has a number of outlying health centres. The population is predominantly poor and living in an insecure situation due to armed conflict and sexual violence caused by several armed militia throughout the region. It is an observational, prospective, descriptive and analytical study examining all deliveries that occurred during the study period. General practitioners and midwives at the hospital are able to perform vaginal and caesarean deliveries; most are performed by general practitioners. The number of deliveries per year is estimated at 3,000. A data collection form was designed. Data collection was carried out by a team of investigators made up of doctors and midwives in the maternity unit. The sources of information were delivery records, partograms, surgical reports and NN (neonatal) records. Sociodemographic parameters (maternal age, marital status, level of education, ethnicity, occupation, primary residence, weight, height), medical and surgical history, obstetric environment (prenatal monitoring), and maternal and perinatal morbidity and mortality (complications and outcome) were analysed. Oral consent from patients was obtained once the purpose of the study was explained.
Methods:
The normality test of continuous variables was applied using graphs (histograms, box plots). The median and interquartile range were calculated to describe asymmetrical distributions. The mean and standard deviations were calculated to describe normally distributed variables.
Associations between delivery via caesarean section and the various explanatory variables were analysed using logistic regression. We reported the relative odds with the confidence interval of 95% and the p-value of the Wald test for each variable. The multivariable model was constructed using a descending stepwise selection method for the explanatory variables and an entry probability of 0.05, an exit probability of 0.10, and also based on Akaike information criteria (AIC) – leading to the same final model. The quality of the adjustment was verified using the Hosmer and Lemeshow test. The collinearity of the explanatory variables was verified according to a variance inflation factor (VIF) (< 5). The level of significance was set at 0.05.
Analyses were performed using Sata /SE 17.0 and R 4.0.0.
Results:
1,243 patients delivered at the Rutshuru General Hospital during the period studied. The average age of our population was 25 years. The majority of the women were married (93.5%), had no level of education (74.3%) and no profession (93.7%) (Table 1). 45% of patients had a prior history of caesarean sections (Table 2). The majority of the deliveries were at term (98.1%). 99% of pregnant women were monitored via prenatal consultations (PNCs), with 83.5% attending more than three PNCs during their pregnancy. Prior history of caesarean section was indicated in 51% of cases of dystocia and 45% of cases of scarred uterus. 99.7% of patients had a partogram during labour (Table 3).
The percentage of caesarean sections in this study was 52.1%. The incision was most commonly transverse (84.5%) and the type of anaesthesia used was most commonly locoregional (spinal anaesthesia) (99.4%). 11% of deliveries included intra-operative complications and 89% of new-borns did not require intensive neonatal care and were with their mothers.
99% of these caesarean sections were performed by the general practitioner (Table 3).
The rate of maternal mortality was 0.5%, with an average length of admission of seven days (Table 3). Fewer neonatal complications were observed in new-borns delivered by caesarean section compared to those delivered by vaginal delivery (p < 0.001); more complications were observed in patients who had delivered via caesarean section (p=0.002); caesarean sections were more common among women who were employed in the private sector (Table 4). Fewer caesarean sections were performed on women who had primary and secondary levels of education than women with no level of education (p=0.009), there were more intra- and post-operative complications among deliveries via caesarean section than vaginal delivery (p- 0.001) and there were fewer neonatal complications following delivery via caesarean section than following vaginal delivery (p<0.001) (Table 5). Post-operative complications were observed more frequently in women with a multi-scarred uterus (Table 6). Women who did not have any education had more children than those with a primary or secondary level of education or higher (p<0.001) (Table 7). There is a statistically significant correlation between parity and age (p<0.001) (Table 8). There is no statistically significant correlation between per operative complications and the distance between the place of residence and the hospital (p-0.09) (Table 9). There is no statistically significant correlation between the distance and per- or post-operative complications (p-0.57).
|
Variables |
n |
Median [IQR] / n (%) |
|
Age (years) |
1241 |
25 [20 – 30] |
|
Marital status |
1227 |
|
|
Single |
79 (6.4) |
|
|
Divorced |
1 (0.1) |
|
|
Married |
1147 (93.5) |
|
|
Level of education |
1220 |
|
|
None |
906 (74.3) |
|
|
Primary |
153 (12.5) |
|
|
Secondary |
156 (12.8) |
|
|
Higher |
5 (0.4) |
|
|
Occupation |
272 |
|
|
None |
255 (93.7) |
|
|
Private |
17 (6.3) |
|
|
Distance from Rutshuru (km) |
1141 |
6 [1.5 – 12] |
Table 1: Sociodemographic data
|
Gravidity |
1243 |
3 [2 – 6] |
|
Parity |
1241 |
2 [1 – 4] |
|
Live children |
1241 |
2 [0 – 4] |
|
Abortions |
1239 |
|
|
0 |
1026 (82.8) |
|
|
1 |
165 (13.3) |
|
|
2 to 6 |
48 (3.9) |
|
|
2 |
28 (2.3) |
|
|
3 |
12 (1.0) |
|
|
4 |
4 (0.3) |
|
|
5 |
3 (0.2) |
|
|
6 |
1 (0.1) |
|
|
Deaths |
1239 |
|
|
0 |
1007 (81.3) |
|
|
1 |
139 (11.2) |
|
|
2 to 4 |
93 (7.5) |
|
|
Malaria treated (curative) during the pregnancy? |
1216 |
|
|
No |
1138 (93.6) |
|
|
Yes |
78 (6.4) |
|
|
Haemoglobin (g/dL) |
35 |
10.4 ± 1.8 |
|
Medical consultation during pregnancy |
1153 |
|
|
No |
533 (46.2) |
|
|
Yes |
620 (53.8) |
|
|
Prior history of caesarean section |
1082 |
|
|
No |
594 (54.9) |
|
|
Yes |
588 (45.1) |
|
|
If yes, how many times |
470 |
|
|
1 |
232 (49.4) |
|
|
2 |
115 (24.5) |
|
|
3 |
74 (15.7) |
|
|
4 |
31 (6.6) |
|
|
5 |
18 (3.8) |
|
|
Did children delivered via previous caesarean sections live? |
628 |
|
|
No |
168 (26.7) |
|
|
Yes |
460 (73.3) |
|
|
If they died, how many died? |
20 |
|
|
1 |
14 (70.0) |
|
|
2 |
5 (25.0) |
|
|
3 |
1 (5.0) |
Table 2: Medical data
|
Length of pregnancy |
1231 |
|
|
< 9 months |
24 (1.9) |
|
|
9 months to 40 weeks |
1207 (98.1) |
|
|
PNC attended |
1223 |
|
|
No |
3 (0.3) |
|
|
Yes |
1220 (99.7) |
|
|
How many times |
1229 |
|
|
3 or more |
1026 (83.5) |
|
|
Fewer than 3 |
203 (16.5) |
|
|
Indication for the most recent caesarean section |
481 |
|
|
Scarred uterus |
217 (45.1) |
|
|
Scarred uterus + dystocia |
66 (13.7) |
|
|
Scarred uterus + dystocia + distress |
24 (5.0) |
|
|
Scarred uterus + presentation |
13 (2.7) |
|
|
Scarred uterus + distress |
89 (18.5) |
|
|
Dystocia |
247 (51.3) |
|
|
Dystocia + presentation |
3 (0.6) |
|
|
Dystocia + distress |
9 (1.9) |
|
|
Bleeding during 3rd trimester |
9 (1.9) |
|
|
Presentation |
55 (11.4) |
|
|
Acute foetal distress |
173 (36.0) |
|
|
Other |
8 (1.7) |
|
|
Monitored via partogram at the hospital |
1219 |
|
|
No |
3 (0.3) |
|
|
Yes |
1216 (99.7) |
|
|
Delivery method |
1213 |
|
|
Vaginal |
575 (47.4) |
|
|
Caesarean section |
638 (52.6) |
|
|
Vaginal with ventouse |
824 |
|
|
No |
819 (99.4) |
|
|
Yes |
5 (0.6) |
|
|
Including only vaginal deliveries: |
393 |
|
|
No |
391 (99.5) |
|
|
Yes |
2 (0.5) |
|
|
If caesarean, for what indication(s) |
584 |
|
|
Scarred uterus |
326 (55.8) |
|
|
Dystocia |
240 (41.1) |
|
|
Dystocia + presentation |
2 (0.3) |
|
|
Dystocia + distress |
10 (1.7) |
|
|
Bleeding during 3rd trimester |
28 (4.8) |
|
|
Bleeding + distress |
2 (0.3) |
|
|
Presentation |
71 (12.2) |
|
|
Presentation + distress |
7 (1.2) |
|
|
Acute foetal distress |
176 (30.1) |
|
|
Other |
42 (7.2) |
|
|
Type of incision |
629 |
|
|
LMI |
92 (14.6) |
|
|
Pfannenstiel incision |
1 (0.2) |
|
|
Inverted T |
2 (0.3) |
|
|
Transverse |
533 (84.7) |
|
|
Transverse, LMI |
1 (0.2) |
|
|
Including only caesarean deliveries: |
616 |
|
|
LMI |
91 (14.8) |
|
|
Pfannenstiel incision |
1 (0.2) |
|
|
Inverted T |
2 (0.3) |
|
|
Transverse |
512 (84.6) |
|
|
Transverse, LMI |
1 (0.2) |
|
|
Presence of adhesions |
610 |
|
|
No |
300 (49.2) |
|
|
Yes |
310 (50.8) |
|
|
Types of hysterotomy |
629 |
|
|
Low vertical |
594 (94.4) |
|
|
T and/or upper midline |
4 (0.6) |
|
|
Upper transverse |
31 (4.9) |
|
|
Intra-operative complications |
527 |
|
|
No |
467 (88.6) |
|
|
Yes |
60 (11.4) |
|
|
Which? |
65 |
|
|
Epiplo-uterine and/or utero parietale |
3 (4.6) |
|
|
Bleeding |
33 (50.8) |
|
|
Massed dead, IUFD or stillbirth |
5 (7.8) |
|
|
Pre-labour rupture |
4 (6.1) |
|
|
Uterine rupture |
6 (9.2) |
|
|
Placental senescence |
1 (1.5) |
|
|
Other |
13 (20.0) |
|
|
New-borns |
1170 |
|
|
With their mother (1) (2) |
1045 (89.3) |
|
|
Dead (1)(2) |
38 (3.3) |
|
|
Dead (1)(2), with their mother (1)(2) |
25 (2.1) |
|
|
Neonatal unit (1)(2) |
54 (4.6) |
|
|
Neonatal unit (1)(2), dead (1)(2) |
1 (0.1) |
|
|
Neonatal unit (1)(2), with their mother |
7 (0.6) |
|
|
Weight 1 (g) |
1240 |
3056 ± 600 |
|
Weight 2 (g) |
28 |
2220 ± 686 |
|
Sex 1 |
1225 |
|
|
Female |
574 (46.9) |
|
|
Male |
651 (53.1) |
|
|
Sex 2 |
28 |
|
|
Female |
10 (35.7) |
|
|
Male |
18 (64.3) |
|
|
Type of anaesthesia |
643 |
|
|
General |
4 (0.6) |
|
|
Spinal |
639 (99.4) |
|
|
Qualification of practitioner |
642 |
|
|
Generalist |
641 (99.8) |
|
|
Specialist |
1 (0.2) |
|
|
Iron supplement during pregnancy |
1217 |
|
|
No |
27 (2.2) |
|
|
Yes |
1190 (97.8) |
|
|
Per- or post-operative complications |
1111 |
|
|
No |
1080 (97.2) |
|
|
Yes |
31 (2.8) |
|
|
Which? |
44 |
|
|
Bleeding |
27 (61.4) |
|
|
Other |
17 (38.6) |
|
|
Maternal death |
1110 |
|
|
No |
1105 (99.5) |
|
|
Yes |
5 (0.5) |
|
|
Length of stay (days) |
1205 |
7 [4 – 10] |
Table 3: Obstetric data
|
n |
Caesarean section n (%) |
OR [95% CI] |
p-value |
|
|
Per-operative complications |
521 |
445 (96.5) |
0.27 |
|
|
No |
461 |
60 (100.0) |
1 |
|
|
Yes |
60 |
3.02 [0.50 -/+ ∞] |
||
|
Neonatal |
1149 |
583 (53.6) |
1 |
< 0.001 |
|
No |
1088 |
18 (29.5) |
0.36 [0.21 – 0.64] |
|
|
Yes |
61 |
|||
|
Per- or post-operative complications |
1087 |
576 (54.5) |
1 |
0.002 |
|
No |
1057 |
29 (98.7) |
24.22 [3.29 – 178.43] |
|
|
Yes |
30 |
|||
|
Distance from Rutshuru (km) |
1113 |
1.01 [0.99 – 1.03] |
0.29 |
|
|
Level of education |
1191 |
485 (54.9) |
1 |
0.009 |
|
None |
884 |
61 (41.2) |
0.58 [0.41 – 0.82] |
|
|
Primary |
148 |
83 (53.5) |
0.95 [0.67 – 1.34] |
|
|
Secondary |
155 |
0 (0.0) |
- |
|
|
Higher |
4 |
|||
|
Occupation |
267 |
123 (48.8) |
1 |
0.03 |
|
None |
252 |
12 (80.0) |
4.20 [1.16 – 15.22] |
|
|
Private |
15 |
|||
|
Number of PNCs |
1201 |
99 (50.0) |
1 |
0.38 |
|
Fewer than 3 |
198 |
536 (53.4) |
1.15 [0.85 – 1.56] |
|
|
3 or more |
1003 |
Table 4: Analyses of deliveries via caesarean section according to social factors: Single variable analyses
|
OR [95% CI] |
p-value |
|
|
Per- or post-operative complications |
0.001 |
|
|
No |
1 |
|
|
Yes |
26.53 [3.57 – 197.45] |
|
|
Neonatal |
< 0.001 |
|
|
No |
1 |
|
|
Yes |
0.31 [0.17 – 0.59] |
|
|
Level of education |
0.003 |
|
|
None |
1 |
|
|
Primary |
0.51 [0.34 – 0.76] |
|
|
Secondary |
1.12 [0.76 – 1.64] |
Table 5: Multivariable analysis (n = 1015, caesarean = 568):
|
Per- or post-operative complications OR [95% CI] |
p-value |
|
|
Number of uterine scars |
1.46 [1.00 – 2.12] |
0.048 |
Table 6: Analyses of the risk of intra- or post-operative complications according to the number of uterine scars, including indications of caesarean section due to scarred uterus = 299, ncompl = 20)
|
n |
Parity Median [IQR] |
p-value |
|
|
Level of education |
1218 |
3 [1 – 5] |
< 0.001* |
|
None |
904 |
2 [0 – 4] |
|
|
Primary |
153 |
1 [0 – 3] |
|
|
Secondary or higher |
161 |
*None vs Primary padjusted = 0.003; None vs Secondary or higher padjusted< 0.001; Primary vs Secondary or higher padjusted = 0.10
Table 7: Analyses of parity according to level of education
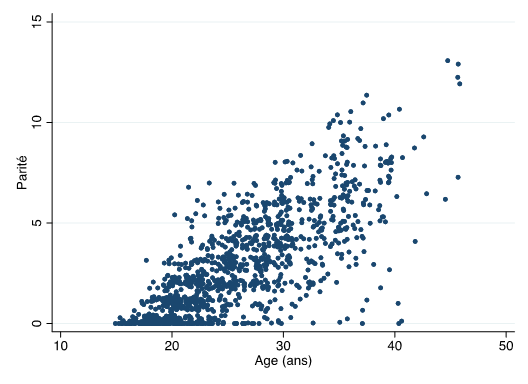
Figure 1: Analyses of correlation between parity and age
n = 1239, rs = 0.78, p < 0.001
The Spearman correlation coefficient indicates that there is a very strong positive correlation (0.78) that is statistically significant (p < 0.001).
|
Intra-operative complications OR [95% CI] |
p-value |
|
|
Distance from Rutshuru (km) |
1.04 [0.99 – 1.10] |
0.09 |
Table 9: Analyses of the risk of intra-operative complications according to distance (n = 483, ncompl = 55)
|
Per- or post-operative complications OR [95% CI] |
p-value |
|
|
Distance from Rutshuru (km) |
1.02 [0.96 – 1.08] |
0.57 |
Table 10: Analyses of the risk of intra- or post-operative complications according to distance (n = 1015, ncompl = 30)
Discussion
We discuss first caesarean section frequency, its indications, the type of anaesthesia used, and maternal and perinatal complications, in contexts suffering from insecurity in a low-income country.
Caesarean section frequency
The frequency of caesarean sections in our study is 52% higher than in the rest of the DRC (8.8%). This is contrary to the recommendations of the WHO which stipulate that there is no justification for any region of the world to have a rate of caesarean section above 10% to 15%[11,12]. This declaration was founded on the limited data available at the time on rates of caesarean sections (CS) observed in Northern European countries, which had the lowest rates of maternal and perinatal mortality. Over time, this figure came to be considered the ‘optimal’ rate of CS by the international community. These rates have risen in developed and developing countries alike, sometimes reaching very high rates such as in Brazil and in the United States[12]. The WHO has since refined its message: the optimal rate of caesarean sections takes into account that women who need a caesarean section can receive one under the right conditions, and those who do not need one, will not get one and can be assisted in their delivery by qualified staff. The proportion of CS observed in our study is higher than that seen among the general population in the Democratic Republic of the Congo (DRC)[13]. Another study on the analysis of CS practices in SSA (sub-Saharan Africa) outlined CS rates ranging from 2% to 51%, with higher rates of maternal and perinatal complications compared to vaginal delivery[14]. This study showed that rates vary according to the population studied and access to healthcare[14]. In addition to the specific context of insecurity connected with armed conflict in the region, the rate of 52% is due to the transfer of patients from outlying maternity units to the Rutshuru General Referral Hospital which has more infrastructure and qualified staff, as well as higher-risk pregnancies being transferred for better treatment. Furthermore, the majority of patients who delivered via caesarean section in this hospital had a prior history of caesarean sections. A study conducted in South Kivu identified the rate of caesarean section at 6.9%[15]. The rate of CS described in this study appears to be lower than the average rate identified for South Kivu (10.8%), but higher than the national average (4.1%)[16]. The rate identified in this study is lower than the rate reported in our study for a number of reasons: the intensification of armed conflict and insecurity in the Rutshuru region, patients transferred to the Rutshuru General Hospital because they could not be properly cared for in outlying maternity units, the presence of more qualified staff and international experts associated with donations and upskilling of local staff. Patients with a prior history of CS, who cannot be treated at outlying maternity units due to a shortage of qualified staff, are transferred to the Rutshuru General Hospital.
Indications for a caesarean section
The main indications for a caesarean section in our study are scarred uterus (55%) and dystocia (41%). One study reported the main indications for a caesarean section as being: prior history of a caesarean section or scarred uterus, dystocia, foetal distress, breech presentation, antenatal bleeding and hypertensive disorders[14]. The ‘once a caesarean, always a caesarean’ policy is widely applied in sub-Saharan Africa, mainly for fear of uterine rupture during labour. This policy helps reduce both the uterine rupture rate and emergency surgery responsible for the increase in maternal and perinatal mortality and morbidity. These repeat caesarean sections do not, however, sufficiently result in the expected medical benefits[14]. In fact, vaginal delivery after a caesarean section has a low risk both for the mother and for the child, except in around 1% of cases of scarred uterus such as those resulting from a vertical hysterotomy or when the indication is connected to an ongoing complication during pregnancy[14]. Although the International Federation of Gynecology and Obstetrics (IFGO) has published guidelines promoting vaginal delivery after a caesarean section for almost all women with prior history of caesarean section, fewer women are having vaginal deliveries in referral hospitals in sub-Saharan Africa[17]. A study conducted in Kivu analysed the practice of CS in the areas of armed conflict using the Robson classification. This study showed that Group 5 (all multiparous with at least one uterine scare, a single pregnancy, cephalic presentation, gestational age equal to or greater than 37 weeks) were contributing to the increase in rates of CS in these conflict areas, which confirms our results on the main indicators for CS[15]. After analysing these indications in our study, dystocia (difficult and protracted labour) was the main indication for the first caesarean. Dystocia is mainly caused by insufficient uterine contractions, sometimes by cephalopelvic disproportion, no progression in foetal descent due to a tumour, and abnormal presentation of the foetus. However, it is sometimes difficult to make this diagnosis before labour begins.Certain authors wondered whether dystocia was currently being over-diagnosed in order to justify more frequent use of CS[14].
The other indications such as foetal distress, bleeding in the third trimester and abnormal presentation of the foetus represented 4% of CS in our study.
Maternal risks
While caesarean sectionsare currently safer in developed countries, they still entail risks of many major abdominal procedures in sub-Saharan Africa. Maternal mortality is estimated to be approximately 2 to 11 times higher after a CS than after a vaginal delivery[18]. Infections, bleeding, anaesthetic complications, obstetric fistulae and pulmonary embolism are the main complications. Maternal morbidity associated with caesarean section is 5 to 10 times higher than with vaginal deliveries. These complications vary significantly between regions and according to the populations studied [14]. Our study reports around 11% intra- and post-operative complications; locoregional anaesthesia (spinal anaesthesia) was used in around 99% and CS was more commonly carried out by a general practitioner. The lack of obstetrician-gynaecologists explains in part the high frequency of CS in this study. There were few specialist physicians in this region faced with armed conflict due to the fear of being taken hostage by armed groups or being killed. More complications were observed in women who had delivered via CS compared to vaginal deliveries. This is consistent with a number of other studies, including Weiser et al.[18]. More complications were observed in women who had a multi-scarred uterus, and maternal mortality was estimated at 0.5%. This maternal mortality rate and the long-term post-operative complications are difficult to evaluate as the average length of stay was 7 days. Due to the insecurity, it was difficult to monitor these women after they left the hospital. 99% of the pregnant women had a partogram during labour, which explains the diagnosis of dystocia estimated at around 45% as an indication for CS in our study.
Our study did not show a statistically significant correlation between the distance and per- or post-operative complications.
Perinatal risks
In our study, new-borns delivered via CS presented with fewer neonatal complications than via vaginal delivery. This is due to the fact that the majority of pregnancies were at term, the type of anaesthesia used was most commonly locoregional and the main indication for CS was scarred uterus. The results of our study with respect to neonatal complications differ from the results reported in other studies[19-21]. Elective CSs account for approximately 9% of neonatal intensive care admissions. This rate increases in the event of an emergency caesarean section. Use of partograms to assess the labour is very low[19]. The main cause of admission to the neonatal unit was iatrogenic prematurity complicated by lung disease. The main lung disease was hyaline membrane disease or infant respiratory distress syndrome resulting from pulmonary immaturity[19]. Due to the lack of adequate intensive care units, caesarean sections in Africa increase perinatal risks. Elective and repeat caesarean sections have merit when the lungs are mature, in order to prevent respiratory distress syndrome. However, infants born via CS are more likely to present this syndrome[21].
Limitations of our study
- The study examined only the Rutshuru General Referral Hospital and did not examine other outlying facilities.
- The duration of our study should have been longer and included more centres in order to confirm our results.
Conclusion
In areas ravaged by armed conflict, specific healthcare needs are often neglected or ignored entirely. And yet, under bombardment, women are particularly vulnerable. Women need uninterrupted access to a functioning healthcare system, in particular due to the risk of death, disease and disability associated with pregnancy and childbirth. An armed conflict can disrupt a healthcare system that has already been made fragile and create unbearable situations for pregnant women and breastfeeding mothers. They require full and immediate access to pre- and post-natal care and medical assistance during pregnancy and childbirth.
Insecurity resulting from armed conflicts had a negative impact on the education, employment and socio-economic status of the population and, as a result of this, poor care for pregnant woman.
This story shows that new-borns delivered via caesarean section have a lower risk of perinatal complications thannew-borns delivered via vaginal delivery in areas faced with insecurity as a result of armed conflicts. However, we observe a higher number of maternal complications following delivery via caesarean section than via vaginal delivery.
Contributions
This is a prospective study describing childbirth care in a region faced with insecurity resulting from armed conflict in the east of the Democratic Republic of the Congo.
References
- World Health Organization. Trends in Maternal Mortality 2000 to 2017: Estimates by WHO, UNICEF, UNFPA, World Bank Group and the United Nations Population Division. Report no. 9789241516488. WHO; 2019.
- Kotsadam A, Ostby G. Armed conflict and maternal mortality: a micro-level analysis of sub-Saharan Africa, 1989–2013. Soc Sci Med 239 (2019): 112526.
- Hynes M, Sakani O, Spiegel P, et al. A study of refugee maternal mortality in 10 countries, 2008–2010. Int Perspect Sex Reprod Health 38 (2012): 205-213.
- Kruk ME, Kujawski S, Moyer CA, et al. Next generation maternal health: external shocks and health-system innovations. Lancet 388 (2016): 2296-2365.
- Parmar PK, Jin RO, Walsh M, et al. Mortality in Rohingyarefugee camps in Bangladesh: historical, social, and political context. Sex Reprod Health Matters 27 (2019): 1610275.
- Freedman J. Explaining sexual violence and gender inequalities in the DRC. Peace Review 23 (2011): 170-175.
- VanWieringen K. To counter the rationality of sexual violence: existing and potentialpoliciesagainst the genocidal use of rape as a weapon of war in the Democratic Republic of Congo. J Int Humanit Action 5 (2020): 8-11.
- Ali Bitenga Alexandre , KitokaMokeMutondo , Juvenal BazilasheBalegamire , et al. Motivations for sexual violence in armed conflicts: voices from combatants in eastern Democratic Republic of Congo.Med ConflSurviv 37 (2021): 15-33.
- Chukwuma A, Ekhator-Mobayode UE. Armedconflict and maternal health care utilization: Evidence from the Boko Haram Insurgency in Nigeria. SocSci Med 226 (2019): 104-112.
- Namasivayam A, Arcos González P, Castro Delgado R, et al. TheEffect of ArmedConflict on the Utilization of Maternal Health Services in Uganda: A Population-basedStudy.PLoSCurr 3 (2017): 9-14.
- Betran AP, Merialdi M, Lauer JA, et al. Rates of caesarean section: analysis of global, regional and national estimates. PaediatrPerinatEpidemiol 21 (2007): 98-113.
- Ye J, Betrán AP, Guerrero Vela M, et al. Searching for the optimal rate of medicallynecessarycesareandelivery. Birth 41 (2014): 237-244.
- MINISTERE DU PLAN ET MACRO INTERNATIONAL 2008. ENQUETE DEMOGRAPHIQUE ET DE SANTE, REPUBLIQUE DEMOCRATIQUE DU CONGO 2007. CALVERTON, MARYLAND, USA. MINISTERE DU PLAN ET MACRO INTERNATIONAL (2007).
- MICHEL DIKETE1*, YVES COPPIETERS2, PHILIPPE TRIGAUX3, YVON ENGLERT1, PHILIPPE SIMON1 AND W ZHANG2 : AN ANALYSIS OF THE PRACTICES OF CAESAREAN SECTION IN SUB-SAHARAN AFRICA: ASUMMARY OF THE LITERATURE, ARCHIVES OF COMMUNITY MEDICINE AND PUBLIC HEALTH, AUGUST (2019).
- Guy Mulinganya, Espoir Bwenge MalembakaID, Melissa Lukula Akonkwa, et al.Applying the Robson classification to routine facility data to understand the Caesarean section practice in conflict settings of South Kivu, eastern DR Congo.PLOSONE 15 (2020): e0237450.
- INS. Enquête par grappes à indicateurs multiples, 2017–2018, rapport de re´sultats de l’enquête. Kinshasa, RépubliqueDémocratique du Congo. Kinshasa (2020).
- International Federation of Gynecology and Obstetrics Congress opens in Rome.
- Weiser TG, Uribe-Leitz T, Fu R, et al. Variability in mortalityaftercaesareandelivery, appendectomy, and groin hernia repair in low-income and middle-income countries: Implications for expanding surgical services. Lancet 385 (2015): S34.
- Nakimuli A, Nakubulwa S, Kakaire O, et al. Incidence and determinants of neonatal morbidity after elective caesarean section at the national referral hospital in Kampala, Uganda. BMC Res Notes 8 (2015): 624.
- Landry E, Pett C, Fiorentino R, et al. Assessing the quality of record keeping for caesarean deliveries: results from a multicenter retrospective record review in five low-income countries. BMC Pregnancy Childbirth 14 (2014): 139.
- Ugwu NU, de Kok B. Socio-cultural factors, gender roles and religious ideologies contributing to Caesarean-section refusal in Nigeria. Reprod Health 12 (2015): 70.
