The Impact of Decentralizing HIV Services on Patients at St. Elizabeth Hospital Shisong, Cameroon
Article Information
Blaise Nkengfua1, Nkengafac Nyiawung Fobellah2*, Sylvester Ndeso Atanga1, Belleh Nyiawung Fobellah3
1Department of Nursing, School of Health and Human Services, St. Monica Higher Institute, Buea, Cameroon
2Department of Public Health, School of Health and Human Services, St. Monica Higher Institute, Buea, Cameroon
3International Relations Institue of Cameroon, University of Yaounde I, Yaounde, Cameroon
*Corresponding author: Nkengafac Nyiawung Fobellah, Department of Public Health, School of Health and Human Services, St. Monica Higher Institute, Buea, Cameroon
Received: 10 June 2021; Accepted: 23 June 2021; Published: 13 October 2021
Citation: Blaise Nkengfua, Nkengafac Nyiawung Fobellah, Sylvester Ndeso Atanga, Belleh Nyiawung Fobellah. The Impact of Decentralizing HIV Services on Patients at St. Elizabeth Hospital Shisong, Cameroon. Archives of Clinical and Biomedical Research 5 (2021): 803-813.
View / Download Pdf Share at FacebookAbstract
Background: Cameroon is one of the global health priority countries. Without decentralization of HIV services from physicians to nurses and midwives, the sustainable scale up of antiretroviral therapy (ART) in resource limited settings may not be possible; this is a key consideration in achieving epidemic control. Until 2005, policy allowed only physicians to prescribe antiretroviral therapy to HIV infected persons which delayed care delivery.
Objective: In October 2014 there was effective implementation of option B+ strategy. We intended to compare antiretroviral therapy (ART) uptake, Retention to ART, and male partner participation (MAP) in Prevention of Mother to Child Transmission of HIV (PMTCT) pre and post B+ implementation, following change in staffing policy.
Design: A retrospective chart review study in which routine program data was collected from PMTCT and HIV Management unit (HMU). Methods: We evaluated ART Uptake, retention to ART and Male partner participation (MAP) in PMTCT pre (December 2011 to November 2014) and post (December 2014 to November 2017).
Results: A total of 2958 (pre) and 2696 (post) women presented to antenatal care (ANC). Of the 284 women who tested HIV positive, A majority was treated post task shifting, pre 111 (60.22%) vs. post; 173 (92.7%). The average 6 and 12 months retention rates of clients to ART was 57 (89.49) and 48 (84.21%) at ANC post B+, similarly, at HMU we saw an insignificantly change in the number of clients retained at 6 and 12 months on ART pre B+, (Pre 85.735% vs. Post 80.93 p-value 0.045< 0.5). MAP pre/post was [105 (3.55%) vs. 272 (10.09%) P-value =0.266].
Conclusions: A considerable growth in ART uptake was seen at PMTCT/ANC only following task sharing. The retention rates for both pregnant, breastfeeding women and all ages was approximately the same 85% which is
Keywords
Antiretroviral therapy; HIV; HIV services; Task sharing(or task shifting); Adherence; Retention; Male as partner participation; Option B+; Vertical transmission of HIV
Antiretroviral therapy articles; HIV articles; HIV services articles; Task sharing(or task shifting) articles; Adherence articles; Retention articles; Male as partner participation articles; Option B+ articles; Vertical transmission of HIV articles.
Article Details
1. Introduction
The scale up of antiretroviral therapy in a sustainable manner to meet the need of people living with HIV is one key consideration in achieving epidemic control in every setting [1]. However, without adequate health systems global HIV/ AIDS targets cannot be achieved [1]. Cameroon is one of the global health priority countries that account for the greatest share of the world’s communicable disease burden and family planning needs and where health systems weaknesses create binding constraints on sustainable maternal and child survival [2]. Cameroon is also one of the 57 countries listed by World health Organization as having human resources for health crisis [3] World Health Organization estimates shows that she has 1.1 physicians and 7.8 nurses and midwives per 100,000 population [4] Recent report indicates that Cameroon’s HIV prevalence rate is estimated at 5.1 percent, the highest rate for the West and Central Africa sub-region [5].
According to Alongifor, Cameroon has a shortage of medical professionals, with fewer than two doctors for every 10,000 people with health treatments often provided by nurses [6]. These show some of the realities facing her health system and perhaps why the WHO recommendation on task shifting of HIV services becomes important consideration not only to beef up PMTCT service uptake but sexual and reproductive health in general [7]. The shortage of health workers most especially prescribing physicians represents a major barrier to preventing and treating the disease [7]. The WHO report on task shifting call for the implementation of task shifting to rapidly scale up HIV services and other strategies to consider like training of health care worker to deal with the work force crises [7]. The role that nurses have played in ART prescription has been quite evident elsewhere in Sub-Saharan Africa for example, in one study carried out in Uganda indicates that nursing cadre were the backbone of ART service delivery [8]. Providers of health care services realized that the number of physicians could hardly meet the growing need of HIV treatment in Uganda so, they turned to non-physicians cadre such as nurses, midwives and lay workers to meet the increasing demand of ART. The number of people on ART increased tremendously from 2700 to over a million Ugandans accessing ART and a majority of care providers are nurses [8]. Also, one study in Botswana shows that better utilization of nurses has the potential to increase access to ART, reduce congestion at centralized ART centers, reduce unnecessary travel by patients and allow for localized provision of support for adherence Miles et al [9].
Recent reports shows that treatment coverage is low, for example UNAIDS progress report on HIV epidemic in Cameroon indicates that number on treatment was 210 000(37%). Adults on ART 197 000 (38%) [10, 11], This means that even more than the current number needs to be identified and place on treatment for her to meet the 95-95-95 UNAIDS target set for 2025 and finally meet the UN declaration of 2016 to end AIDS epidemic by 2030. Until 2005, the policy allowed only physicians to prescribe ARVs for HIV infected persons [7]. There was chronic shortage of physicians in most developing countries where the prevalence was highest. This resulted in many People Living with HIV (PLHIV) initiating treatment late [5]. Retention and adherence to ART was relatively lower in most developing countries than in developed countries. This led WHO to recommend task shifting of HIV services from physicians to nurses and midwives as the main intervention to address this need [7].
Unfortunately, antiretroviral therapy requires a high adherence to minimize treatment failure and viral resistance [12]. Without adequate adherence, antiretroviral agents would not be capable of suppressing HIV replication because of insufficient concentrations of drugs in the blood and may lead to difficulties suppressing plasma viral load and also increase the development of resistance viruses [12]. With few physicians prescribing this made it difficult for many clients to be attended to thus need for task shifting from physicians to nurses and midwives [7]. Male partner participation is a key component in optimization of PMTCT services [13, 15].
According to [11] the benefits are enormous: Firstly, it provides opportunity to capture both the pregnant mothers and their partners to prevent mother to child transmission of HIV. Secondly, because there is an over growing discordant rate among couples, so involving both parents safeguard the child from HIV. Finally, it increases adherence to PMTCT and it outcomes [13]. The government of Cameroon in August 2012 adopted option B+ for national PMTCT policy. This approach advocates the systematic initiation of antiretroviral therapy (ART) for HIV positive pregnant or breastfeeding women regardless of the clinical and immunological stage [15]. The effective implementation of option B+ began in late 2014 in this health facility. Many researcher works have examined the impact of ART uptake and retention on patient outcomes, but, little comparison has been carried out following the implementation of option B+.
The main objective of this work was to determine whether or not task sharing of HIV services among physicians, nurses and midwives had any impact on people living with HIV when compared to when services were provided by physicians only and document information for better management of patients. The specific objectives were to compare the proportion of clients enrolled on triple lifelong ART, retention in care and male partner participation in PMTCT during the period when ART prescription and monitoring was done by physicians only and when the task was shared among physicians, nurses and midwives.
2. Materials and Methods
2.1 Study design
We carried out a pre/post retrospective study using secondary data from two entry points, that is for HIV infected antenatal women. We also used data from HMU for all people living with HIV we used HIV management unit from ST. Elizabeth Hospital Shisong for two 3years periods. Pre (December 2011 to November 2014) and post (December 2014 to November 2017). The objective was to compare ART uptake, retention to ART and male partner involvement in PMTCT on treatment outcomes for infected women especially along the PMTCT cascade. We also looked at ART uptake and retention for all people living with HIV from HMU. Pre and post B+ implementation. For objective one, A total of 364 HIV infected pregnant and breastfeeding mothers, 1669 people of all ages record was reviewed see table 1and 3 for details. As concerns objective two, The 1, 3, 6& 12 month retention was evaluated. St. Elizabeth Hospital Shisong in the Kumbo East of the North West Region of Cameroon. It is located 100M north of Bamenda the nearest largest town and lies about 2000m above sea level and on the Bamenda Highlands Ring Road with a population of about 80,212 as of 2005 census [16]. She started the implementation of B+ in October 2014. we targeted pregnant and breastfeeding women and their HIV exposed infants on option B+.
2.2 Ethical consideration
Approval to conduct the study was obtained from the Associate Provost of Academic Affairs of St. Monica Higher institute in Buea.
2.3 Data analysis
Microsoft excel 2010; SPSS.20 program was used for data analysis also T- test was applied, and tables were used for data presentation. A P value <0.05 was considered statistically significant. We compared initiation to ART, their treatment outcomes, we looked at retention to ART, transferred out, number of death, missed appointment and Lost to Follow Up(LTFU), Concerning HIV Exposed Infant (HEI), we evaluated the number who received antiretroviral prophylaxis and cotrim preventive therapy, HIV transmission postpartum using Polymerase Chain Reaction(PCR) at 6-8 week and at 18 months. We compared outcomes pre and post B+.
3. Results
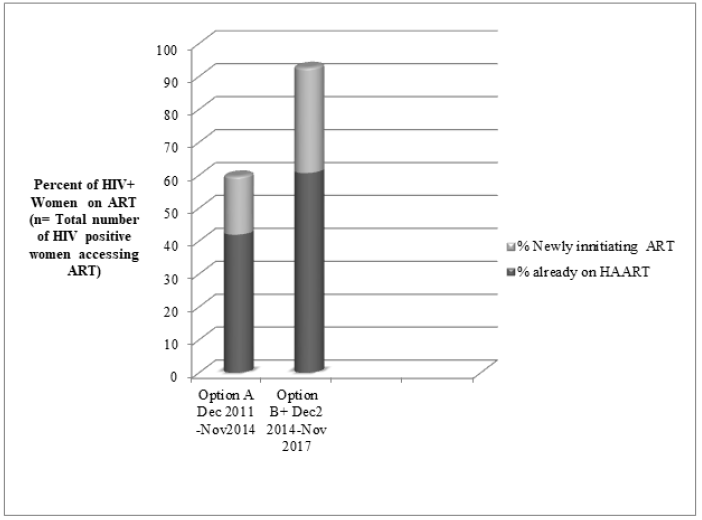
Task shiftinging had a huge impact on ART up for antenatal women at PMTCT entry point, The total number of antenatal women accessing ART who received triple ART treated rose significantly from 101 (60.22%) to 173 (92.7%) pre and post task sharing respectively. See Table 1 and Figure 1 for details. For antenatal women, their retention for the first three month was above 90 but dropped slightly below 90 for all 3 years to an average of 89.47 & 84.21 at 6 &12 months respectively. Please see Table 2 below for details. With regards to retention rates to ART all ages at HMU. The mean initiation to ART pre B+ was 258.33 vs post 298 consequently an average increase of 39.77 new patients were seen post task shifting. The average 6 &12month rate was pre task sharing was 85.735% vs post task sharing 80.93 P=.045. This is a significant drop. Please see Table 3 below for details. For MAP in PMTCT, out of the 5654 antenatal women only 377 (6.67%) percent of their men followed their women to ANC. Pre B+105 (3.55%) vs. Post B+ 272 (10%) please see Table 4. Concerning vertical transmission, 406 HIV expose infants were delivered in this hospital. Six weeks rate stood at pre 9.04% vs post 4.89%, however, the rate increased unexpectedly to 9.3% at 18 months for both pre/post.
|
PMTCT Option Used |
Pre Task Shifting |
Post Task shifting |
Total |
|
Option A& B |
Option B+ |
||
|
Number of Women with Known HIV+ status attending ANC |
87 |
116 |
203 |
|
% of Women with Known HIV+ status attending ANC |
42.86% |
57.14% |
100% |
|
Number of Women Already on HAART attending |
78 |
116 |
194 |
|
% of women already on HAART attending ANC |
47.03% |
52.97% |
100% |
|
Number of women tested HIV+ at ANC |
99 |
62 |
161 |
|
Newly Initiated on ART |
33 |
57 |
90 |
|
Total number of women accessing ART |
186 |
178 |
364 |
|
Percent already on HAART |
41.93 |
60.67 |
|
|
PERCENT Newly initiated on ART |
17.74 |
32.02 |
|
|
Total treated |
(111) 60.22% |
(173) 92.7% |
Table 1: Percentages of Women Treated with ART Pre and post Task Shifting.
|
Year |
Pre Task Shifting |
Post Task Shifting |
Total |
||||
|
2012 |
2013 |
2014 |
2015 |
2016 |
2017 |
||
|
Total Number Initiated On ART |
43 |
23 |
30 |
26 |
16 |
15 |
57 |
|
One Month After |
00 |
00 |
00 |
26 |
16 |
15 |
57 |
|
Number Seen Taking Treatment |
00 |
00 |
00 |
26 |
16 |
15 |
57 |
|
Number Transferred Out |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number Of Death |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number Missed appointment |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
1 Month Rates |
00 |
00 |
00 |
100 |
100 |
100 |
100 |
|
Two Month After |
00 |
00 |
00 |
25 |
15 |
15 |
55 |
|
Number Seen Taking Treatment |
00 |
00 |
00 |
25 |
15 |
15 |
55 |
|
Number Transferred Out |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number Of Death |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number Missed appointment |
00 |
00 |
00 |
1 |
1 |
0 |
2 |
|
2 Month Rates |
00 |
00 |
00 |
96.15 |
93.75 |
100.00 |
96.49 |
|
Three Months After |
00 |
00 |
00 |
24 |
14 |
14 |
52 |
|
Number Seen Taking Treatment |
00 |
00 |
00 |
24 |
14 |
14 |
52 |
|
Number Transferred Out |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number Of Death |
00 |
00 |
00 |
1 |
0 |
0 |
1 |
|
Number Miss Appointment |
00 |
00 |
00 |
1 |
0 |
6 |
|
|
3 Month Rates |
00 |
00 |
00 |
92.31 |
87.50 |
93.33 |
91.23 |
|
Total Number Initiated On ART |
61 |
70 |
65 |
26 |
16 |
15 |
57 |
|
Six Month After |
00 |
00 |
00 |
23 |
13 |
15 |
51 |
|
Number Seen Taking Treatment |
00 |
00 |
00 |
23 |
13 |
15 |
51 |
|
Number Transferred Out |
00 |
00 |
00 |
0 |
1 |
0 |
1 |
|
Number Of Death |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number LTFU |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Six Month Rates |
00 |
00 |
00 |
88.46 |
81.25 |
100.00 |
89.47 |
|
12 Months After |
00 |
00 |
00 |
21 |
14 |
13 |
48 |
|
Number Seen Taking Treatment |
00 |
00 |
00 |
21 |
14 |
13 |
48 |
|
Number Transferred out |
00 |
00 |
00 |
3 |
1 |
2 |
6 |
|
Number of deaths |
00 |
00 |
00 |
0 |
0 |
0 |
0 |
|
Number LTFU |
00 |
00 |
00 |
1 |
0 |
0 |
1 |
|
12 month Retention Rate |
00 |
00 |
00 |
80.77 |
87.50 |
86.67 |
84.21 |
Table 2: Average Retention Rates women on ART per year PMTCT entry point.
|
Pre Task Shifting |
Post Task shifting |
|||||||
|
Total (TT) |
2012 |
2013 |
2014 |
Grand TT |
2015 |
2016 |
2017 |
Grand TT |
|
Number Initiated On ART |
217 |
228 |
330 |
775 |
308 |
300 |
286 |
894 |
|
One Month After |
204 |
205 |
277 |
686 |
275 |
296 |
260 |
831 |
|
Number Seen Taking Treatment |
204 |
205 |
277 |
686 |
275 |
296 |
260 |
831 |
|
Number Transferred Out |
0 |
0 |
0 |
0 |
0 |
1 |
0 |
1 |
|
Number of Deaths |
1 |
1 |
2 |
4 |
1 |
2 |
0 |
3 |
|
Number Missed Appointment |
12 |
22 |
49 |
83 |
32 |
1 |
26 |
59 |
|
Retention Rate |
94.01 |
89.91 |
83.94 |
88.52 |
89.29 |
98.67 |
90.91 |
92.95 |
|
Three Months After |
204 |
203 |
276 |
683 |
273 |
290 |
215 |
778 |
|
Number Seen Taking Treatment |
204 |
203 |
276 |
683 |
273 |
290 |
215 |
778 |
|
Number Transferred Out |
0 |
0 |
0 |
0 |
0 |
1 |
0 |
1 |
|
Number of Death |
0 |
0 |
4 |
4 |
2 |
4 |
1 |
7 |
|
Number Missed Appointment |
8 |
26 |
49 |
83 |
33 |
4 |
68 |
105 |
|
Retention Rate |
94.01 |
89.04 |
83.64 |
88.13 |
88.64 |
96.67 |
75.17 |
87.02 |
|
Six Month After |
197 |
196 |
266 |
659 |
264 |
250 |
193 |
707 |
|
Number Seen Taking Treatment |
197 |
196 |
266 |
659 |
264 |
250 |
193 |
707 |
|
Number Transferred Out |
0 |
0 |
1 |
1 |
2 |
2 |
0 |
4 |
|
Number of Death |
1 |
0 |
6 |
7 |
4 |
8 |
1 |
13 |
|
Number LTFU |
5 |
32 |
76 |
113 |
38 |
35 |
57 |
130 |
|
Retention Rate |
90.78 |
85.96 |
80.61 |
85.03 |
85.71 |
83.33 |
67.48 |
79.08 |
|
12 Months After |
193 |
194 |
274 |
661 |
263 |
242 |
223 |
717 |
|
Number Seen on Taking Treatment |
193 |
194 |
274 |
661 |
263 |
242 |
223 |
717 |
|
Number Transferred Out |
2 |
0 |
0 |
2 |
2 |
0 |
0 |
6 |
|
Number of Death |
2 |
1 |
7 |
10 |
3 |
11 |
1 |
35 |
|
Number LTFU |
9 |
28 |
49 |
86 |
64 |
44 |
52 |
136 |
|
Retention Rate |
88.94 |
85.09 |
83.03 |
85.29 |
85.39 |
80.67 |
77.98 |
80.3 |
Table 3: Retention Rates of Client on ART per Month All ages (HMU).
|
Variable |
Pre B+ |
Post B+ |
Total |
t |
p-value |
||
|
Freq |
% |
Freq |
% |
||||
|
Number of women seen at ANC |
2958 |
52.32 |
2696 |
47.68 |
5654 |
21.28 |
.029 |
|
Number Women counseled & Tested for HIV |
2958 |
52.32 |
2696 |
47.68 |
5654 |
21.58 |
.029 |
|
Number of Men who follow their women for ANC |
105 |
27.85 |
272 |
72.15 |
377 |
2.26 |
.26 |
|
Number of Men tested for HIV |
105 |
27.85 |
272 |
72.15 |
377 |
2.26 |
.26 |
|
Number of MAP tested HIV positive |
3 |
30.00 |
7 |
70.00 |
10 |
2.45 |
.28 |
|
Percent of men who follow their women for ANC |
3.55 |
3.55 |
10.09 |
10.09 |
6.67 |
2.06 |
.28 |
|
Number of deliveries |
3525 |
50.15 |
3504 |
49.85 |
7029 |
334.70 |
.002 |
|
Number of HEI delivered |
237 |
58.37 |
169 |
41.63 |
406 |
5.968 |
.106 |
|
Number HEI given NVP prophylactic at birth |
233 |
57.96 |
169 |
42.04 |
402 |
6.166 |
.102 |
|
Number of HEI given CTX prophylaxis at 6-8weeks |
242 |
59.02 |
168 |
40.98 |
410 |
21.158 |
.030 |
|
Number of HEI who did PCR test at 6-8weeks |
166 |
38.43 |
266 |
61.57 |
432 |
6.16 |
.10 |
|
Number of HEI with PCR positive 6-8 weeks |
15 |
87.96 |
13 |
12.04 |
28 |
1.16 |
.45 |
|
Percent of HEI positive 6-8 weeks |
9.04 |
9.04 |
4.89 |
9.04 |
6.48 |
1.948 |
.30 |
|
Number of HEI with positive PCR linked to care |
6 |
35.29 |
11 |
64.71 |
17 |
10.12 |
.06 |
|
Number HEI did 2nd PCR |
6 |
52.32 |
43 |
87.76 |
49 |
1.31 |
.41 |
|
Number of HEI with 2nd PCR positive |
2 |
52.32 |
11 |
84.62 |
13 |
3.36 |
.18 |
|
Number of HEI who did rapid test at 18mnth |
0 |
27.85 |
3 |
100.0 |
3 |
.93 |
.52 |
|
Number HEI rapid test positive at 18 month |
0 |
30.00 |
4 |
100.0 |
4 |
.95 |
.51 |
|
Percent of HEI positive at 18 month |
---- |
3.55 |
9.30 |
9.30 |
--- |
.98 |
.51 |
|
Number of HEI rapid test positive linked to care |
0 |
50.15 |
4 |
100.0 |
4 |
.95 |
.51 |
Table 4: Prevention along the PMTCT Cascade pre and Task Shifting (post B+).
The findings suggest that there was a significant increase in the number of client put on ART post task shifting at PMTCT but not in HMU. The average retention rates to ART at PMTCT entry points were similar to that at HMU following B+. At HMU there was a significant decrease in client retention post B+. We observed a higher Male partner participation post task shifting.
4. Discussion
Firstly, we observed a considerable improvement in antenatal women treated with ART pre 101 (60.22%) vs. post 173 (92.7%). This growth is most likely due to the fact that policy change gave the nurses and midwives the opportunity to initiate and monitor women on ART. Early infant diagnosis using Polymerase chain reaction (PCR) result obtained 6-8 weeks indicates that vertical transmission was below five percent post B+. (Pre B+ 9.04% vs. Post B+ 4.89%). But, unfortunately, these rates increased to 9.3% at 18 months both pre and post B+ see table 4 in the. This rate is lower than national estimate reported by Nguefack et al [17]. Although this value is lower than that obtained in Lilongwe Malawi country where B+ started [18]. This drop in MTCT at 6 week is most likely related to the effectiveness of the antiretroviral medicine taken by mothers during pregnancy. The rise MTCT seen at 18 month might be related to poor adherence of HEI to antiretroviral prophylaxis.
A further analysis of the figures showed that there was a significant decrease in average retention rate 6 and 12 months post task shifting (Pre 85.75 Vs post 80.93). These rates were similar to that obtained in Malawi [19]. The fall in retention might be related to low knowledge on effectiveness of ART, influence of faith pastors and or stigma. This show that retention in care is sub optimal (<90) in both entry points and this may lead to inadequate suppression of the virus. This means that more effort is needed to have mothers retained on ART as we scale up ART in PMTCT. Despite the decreased 6-8 week seen we noticed an overall lower male partner participation rate pre B+ (pre B+ 3.33 vs. post 10.09 P=0 .288). In fact, the level of Male involvement in PMTCT was observed to be lower than that of studies carried out by Elias et al [20] but point to one common idea that men are yet to take an active role in antenatal care. The low MAP is most likely related to gender issues. Men traditional see antennal services as services reserve for women and do not see reasons why they should be involved.
5. Conclusions
This study established that the 6 and 12 months retention of client to ART at PMTCT/ANC are comparable to HMU post task shifting. However, we noticed a significant decrease in retention rates in HMU post B+ which confirm the fact that even more effort is required to reduce lost to follow up post B+ as the proportion of clients on triple ART regimen grow. We also observed that, Mother to child transmission rate at 6 weeks dropped post B+ but unfortunately, we observed a rise above elimination level postpartum indicating vertical transmission of HIV is concentrated postpartum.
Finally, male partner participation was more than tripled post B+ although their overall participation is still low. All this gaps in the utilization of HIV/AIDS services might be related to low knowledge of the effectiveness of available interventions, stigma, cultural beliefs, chronic poverty that prevent people from seeking care on time.
Recommendations
- 1 PMTCT/ANC entry point should be used to identify women eligible for ART and hence accelerate the number of people on ART so as to meet the UNAIDS target of 95.95.95 by 2025 and ultimately eliminate HIV/AIDS by 2030.
- 2 More research is required to further characterize the barriers and facilitators to retention to ART in order to be able to provides cultural competent, socially acceptable HIV/AIDS services to those who need it.
Limitation of the Study
This study had several limitations; firstly, the implementation of task shifting came at a time when there was a change in the initiation criteria of HIV infected persons on ART which is an HIV positive result. So, this might have had an influence on the numbers of antenatal women treated post B+. In addi-tion, the socio political crisis that has been going on for more than three years in the English speaking region might have contributed to the decrease in reten-tion of clients on ART post B+. We did not have current research on the impact of this crisis on patients to compare with. Moreover, the improvem-ent in male partner participation in PMTCT might have been because of other reasons like improvement in the national PMTCT program [20]. Furthermore, as stated above the result was taken from one health facility which may not reflect the exact situation in other facilities in the North West Region or Cameroon.
Conflict of Interest
We hereby declare that no conflict of interest exists.
Funding Statement
We hereby declare that this work was self-funded. No financial assistance was received.
Acknowledgments
We thank the St. Elizabeth Hospital management cooperation in the realization of this work. We also grateful for physicians, nurses, midwives, and all people living with or affected by HIV in this hospital.
References
- UNAIDS 90-90-90 Ambitious Treatment Target to help end AIDS epidemic (2014).
- USAIDS, USAID’s Vision for Health Systems Strengthening (2015).
- List of 57 countries with a human resources for health crisis (2021).
- Cameroon (2021).
- CNLS/GTC. The Impact of HIV and AIDS in Cameroon through 2020 (2010).
- Alongifor N C. Maternal Mortality in Cameroon: An Urgent Need for Action (2016).
- WHO Global recommendation on Task Shifting (2008).
- Zakumumpa H. Reimagining the role of Nurses workforce in Uganda after more than a decade of ART scale-up. BMC (2020).
- Miles K, Clutterbuck DJ, Seitio O, Sebegod M, Riley A. Antiretroviral roll-out in resource constrained setting; Capitalizing on nurses resources in Botswana. Bulletin of the World Health Organization 85 (2007).
- UNAIDS Country statistics (2019).
- UNAIDS Global AIDS Update (2017).
- Eyassu MA, Mothiba TM, Mbambo-kekana NP. Adherence to antiretroviral therapy among HIV and AIDS patients at the Kwa-Thema clinic in Gauteng Province, South Africa. African Journal of Primary Health Care & Family Medicine 8 (2016): 1.
- Haile F, Brhan Y. Male partner involve-ments in PMTCT: a cross sectional study Mekelle Northern Ethiopia. BMC Pregnancy and Childbirth 14 (2014).
- Improving Male Involvement to Support Eliminate of Mother to Child Transmission in Uganda: a Case Study UNICEF (2016).
- Cameroon MOH. National Guideline on the Prevention and Management of HIV in Cameroon (2015).
- Description of the population of Kumbo (2021).
- Nguefack H L N, Gwet H, Desmonde S, Oukem-Boyer OO M, Nkenfou C, Téjiokem M, et al. Estimating mother-to-child HIV transmission rates in Cameroon in 2011: a computer simulation approach. BMC Infectious Diseases 16 (2016).
- Kim MH, Ahmed S, Hosseinipour MC, Yu X, Nguyen C, Chimbwandira F, et al. The impact of option B+ on PMTCT Cascade Lilongwe, Malawi. J Acquir Immune Defic Syndr 70 (2015): 99-103.
- Kim MH, Ahmed S, Mina CH, Thomas P, Chiao EY. Update of PMTCT from Malawi, the country where option B+ started. Acquir Immune Defic Syndr 68 (2018).
- Elias M, Mmbaga EJ, Mohamed AA, Kishimba RS. Male partner involvement in the prevention of mother to child transmission of HIV infection in Mwanza Region, Tanzania. Pan Afr Med Journal 6 (2017): 1