The Graphical Representation of The Cell Count in The Aspirate as A Groundbreaking Method for The Diagnosis of A Painful Hip Endoprosthesis
Article Information
Marius Hoyka MD1, Elke Weissbarth MTA1, Irina Berger MD2, Bernd Fink MD1,3
1Department for Joint Replacement, Revision Arthroplasty and Rheumatic Orthopaedics, Orthopaedic Clinic Markgröningen, Kurt-Lindemann-Weg 10, 71706 Markgröningen, Germany
2Institute of Pathology, Klinikum Kassel, Mönchebergstraße 41-43, 34125 Kassel, Germany
3Orthopaedic Department, University Hospital Hamburg-Eppendorf, Martinistrasse 52, 20251 Hamburg, Germany
*Corresponding Author: Bernd Fink MD, Department for Joint Replacement, Revision Arthroplasty and Rheumatic Orthopaedics, Orthopaedic Clinic Markgröningen, Kurt-Lindemann-Weg 10, 71706 Markgröningen, Germany, E-mail:bernd.fink@rkh-gesundheit.de
Received: 21 May 2025; Accepted: 06 June 2025; Published: 23 June 2025
Citation: Marius Hoyka, Elke Weissbarth, Irina Berger, Bernd Fink. The Graphical Representation of The Cell Count in The Aspirate as A Groundbreaking Method for The Diagnosis of A Painful Hip Endoprosthesis. Archives of Clinical and Medical Case Reports. 9 (2025): 125-129.
View / Download Pdf Share at FacebookAbstract
Following total hip arthroplasty, pain can occur for a variety of reasons even if the patient has experienced years free of any discomfort. The cause of this pain is often difficult to identify. In the following, a case is described in which the diagnosis of trunnionosis could be made using a new method of graphic visualisation of cell count analysis of an aspirate and the otherwise misinterpretation of a periprosthetic infection with its therapy-related consequences could be avoided.
Keywords
Trunnionosis; Hip Arthroplasty; Cell Count Analysis; Periprosthetic Joint Infection (PJI); LMNE Matrix
Article Details
1. Introduction
Hip arthroplasty is the treatment of choice for end-stage osteoarthritis that can no longer be adequately treated by conservative means [1,2]. Pain can recur after years of pain-free use. The causes of pain can be very varied and should be investigated using different diagnostic methods, whereby a periprosthetic infection should always be excluded [2]. This report describes a case in which a new diagnostic method for analyzing the aspirate of an arthroplasty was instrumental in establishing the diagnosis of pain with a total hip arthroplasty.
2. Case Presentation
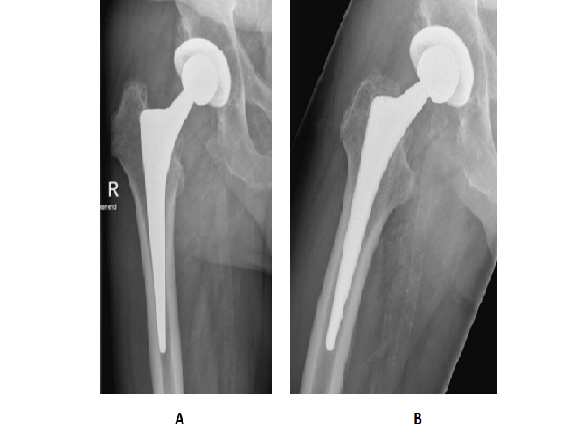
The now 77-year-old male patient underwent implantation of a cementless total hip arthroplasty for right-sided hip osteoarthritis in 2012. Subsequently, the patient was symptom-free. 13 years after the operation, the patient suddenly experienced pain in the right groin region. Trauma and clinical evidence of an infectious origin in the form of fever or chills were absent according to the patient's own information. An increase in pain symptoms was reproducible when walking and when changing from a sitting to a standing position. Secondary findings in the patient included a prostate cancer metastasised to the 12th thoracic vertebral body. The clinical examination revealed a freely mobile hip joint without accompanying rotational pain. Only hip flexion against resistance led to discrete inguinal pain symptoms. There was no Lasègue or Pseudolasègue signs. The subsequent radiological imaging of the right hip joint in two planes showed an unchanged position of the inserted implant without
Magnetic resonance imaging (MRI) of the lumbar spine was performed to rule out a vertebral origin. In addition to degenerative changes in the lumbar vertebral bodies, a spinal canal stenosis at level L3/4 and a metastasis due to a prostate carcinoma in 12th thoracic vertebral body were detected, but these could not be interpreted as the cause of the inguinal pain symptoms. A metal artefact reduced sequence (MARS) MRI of the right hip joint was performed to further evaluate the periarticular musculature and soft tissue. This revealed an attachment tendinopathy with slight fluid accumulation in the area of the greater trochanter (Figure 2).
However, there the patient was clinically symptom-free. Evidence of femoral or periacetabular metastasis could also be ruled out. The preliminary infection diagnostic procedure revealed a slightly elevated CRP in the serum of 10.6 mg/L with a normal leucocyte count. An intra-articular aspiration of the right hip joint was performed in order to obtain synovial fluid. Macroscopically pus-like aspirate and an elevated alpha-defensin level of 1.3 initially confirmed the suspicion of an infectious genesis (Figure 3).
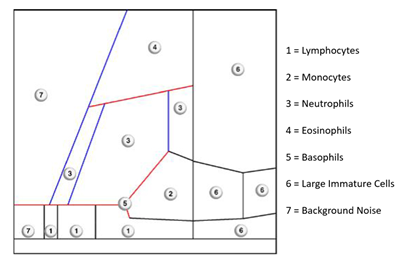
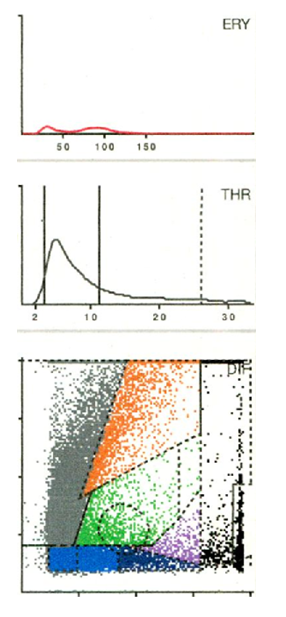
Further determination of the synovial cell count was carried out using the Yumizen H500 automated cell counter (Horiba Medical, Montpellier, France), a laboratory diagnostic device for analysing and differentiating leukocytes from blood and other body fluids. A total of 26 different laboratory parameters are recorded, including the 5 cell types - eosinophils, neutrophils, monocytes, lymphocytes and basophils - as well as atypical lymphocytes and large, immature cells. These cell types are mapped graphically in a so-called LMNE matrix as a function of their cell volume (X-axis) and their light scattering or absorption (Y-axis) [3,4]. The cellular volume differentiation is based on an impedance measurement, while the differentiation of the light absorption is carried out by flow cytometry. This enables the graphical classification and thus differentiation of four leukocyte populations: Lymphocytes, monocytes, neutrophils and eosinophils. Impurities occur in the so-called NOISE area of the LMNE matrix (Figure 4).
In addition to the proportion of polymorphonuclear leukocytes, the Yumizen H500 also provides additional erythrocyte and platelet distribution curves depending on the cell size (X-axis) and quantity (Y-axis) in order to detect a haematoma and distinguish it from an infection [4]. Based on this cellular analysis, a total of seven different cell distribution diagrams can be distinguished: Type I (abrasion type), Type IB (mixed type of abrasion and haematoma contamination), Type II (infection type), Type III (mixed type of infection and abrasion), Type IV (indifference type), Type V (haematoma type), Type VI (mixed type of haematoma and infection) [5-7].
The analysis of the aspirate in this case revealed a cell count of 36,970 cells/μL and a proportion of polymorphonuclear leukocytes of 10.7%. Cultivation of the aspirate for 14 days did not reveal the presence of any microbial organisms. According to the ICM definition for periprosthetic infections, this resulted in a score of 11 (elevated CRP = 3 points, elevated cell count in the aspirate = 3 points, elevated alpha-defensin value = 2 points, pus = 3 points) and thus the provisional diagnosis of a periprosthetic infection [7]. However, the LMNE matrix of the graphical representation of the aspirate showed the abrasion type (type I) (Figure 5).
The subsequent microscopic examination of the aspirate (driven by the result of the LMNE matrix) confirmed this suspicion (Figure 6), and an additional manual cell count determination using a Neubauer improved counter chamber (Carl Roth GmbH, Karlsruhe, Germany) resulted in a cell count of 310 cells/μL.
Based on the graphic analysis of the cell aspirate and subsequent microscopic confirmation of the evidence of abrasion, trunnionosis (with the metal head in place) was now suspected. A new blood sample was taken to determine the cobalt, chromium and nickel ion concentration with detection of not elevetad levels of the metal ions in the blood (cobalt 4.8 μg/L, chromium 1.0 μg/L, nickel 1.8 μg/L).
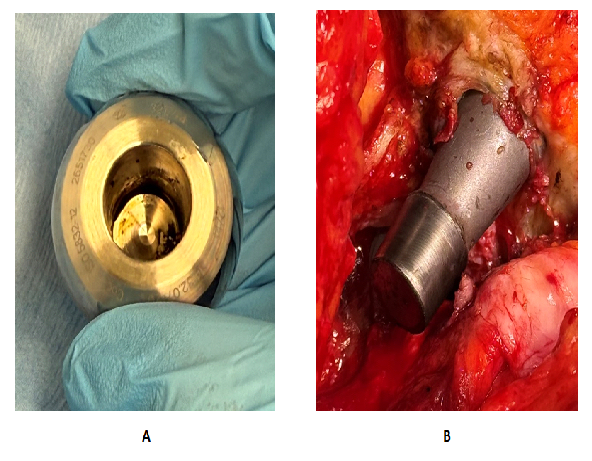
Due to the suspected diagnosis of trunnionosis as the cause of the groin complaints, aseptic head and inlay replacement was indicated. As soon as the joint capsule was opened, pus-like fluid appeared. After removal of the prosthesis head, there were clear traces of corrosion on the head and cone, which once again confirmed the diagnosis of trunnionosis (Figure 7).
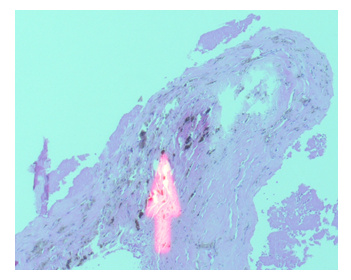
As part of the revision procedure, five tissue samples were taken that were in direct contact with the prosthesis. Microbiological incubation did not reveal any evidence of microorganisms. Further tissue samples were sent for histopathological examination. Here, metal debris and areas with aseptic necrosis were detected and the diagnosis of trunnionosis was confirmed (Figure 8). After the operation, the patient was free of symptoms again.
3. Discussion
This report describes a case in which trunnionosis was the cause of pronounced groin pain after 13 years of pain-free hip arthroplasty. The trunnionosis had not been recognisable by any imaging procedure. The graphic representation of the cell count of the joint aspirate was groundbreaking for the diagnosis and further diagnostic tests. The aspiration of the affected joint showed a synovial fluid that had a pus-like appearance macroscopically, while the automated cell count analysis revealed significantly elevated values (36,970 cells/μL) and the alpha-defensin was also elevated. Together with the discretely elevated CRP value of 10.6 mg/L and the pus-like aspirate, the evaluation according to the ICM definition would have resulted in a score of 11. Consequently, a culture-negative periprosthetic infection would have been diagnosed as the cause of pain [7]. This diagnosis would have led to revision of the prosthesis, which may have had to be performed via an extended trochanteric osteotomy, because the stem was firmly osteointegrated. Thus, the graphic representation of the cell count with the clear evidence of a type I (abrasion type) with a pronounced spot in the so-called NOISE field of the LMNE matrix (Figure 5) allowed the correct diagnosis to be made and the removal of the prosthesis to be avoided. To treat the trunnionosis causing the symptoms, it was sufficient to change the head and inlay for the patient to be subsequently symptom-free again.
Even if the microscopic examination of the aspirate also gave the suspicion of trunnionsis, this is not a routine examination due to the time required and the necessary specific knowledge. The graphical determination of the cell count analysis of the aspirate was decisive for indicating further specific examinations. Trunnionosis is a rare problem with hip prostheses due to abrasion and corrosion at the head-neck connection of the prosthesis stem. This phenomenon mainly occurs (as in the case described) with metal heads on titanium necks and can lead to pain and even failure of the prostheses [8-11].
The case described is similar to the findings with metal-on-metal pairings with adverse reaction to metal debris (ARMDs). Here, too, aspirates are described as looking like pus, the cell count of the aspirate can be significantly increased, the alpha-defensin test can be positive and the CRP value can be increased [12-14]. In previous publications, we were also able to show that the graphic representation of the cell count of the aspirate provides significant insights into the interpretation of such cases [4,5]. We found a very high sensitivity of 90.2 % and specificity of 91.2 % for the diagnosis of chronic periprosthetic infections [5]. In addition, we were able to demonstrate that there is a high degree of agreement between the graphical aspirate analysis with the type classification and the histological classification of the periprosthetic membrane of the same name according to Krenn and Morowitz [15-17] (Cramer value = 0.529) [5].
4. Conclusion
The graphical presentation of cell count analysis from synovial aspirates of joints with endoprostheses is a novel and useful method for diagnosing true periprosthetic infections (PJI) and distinguishing PJI from elevated cell count measurements due to abrasion. The diagnostic accuracy of the cell count analysis is enhanced by using a device that visually displays an elevated leukocyte count and detects wear particles, which could otherwise lead to misinterpretation of the data. By combining cell counting with the graphical display in the LMNE matrix increasing the diagnostic value of the cell count analysis in joint aspirates. The case described here shows that the graphical representation of the cell count analysis of the joint aspirate represents a new and important diagnostic tool for the verification of chronic periprosthetic infections.
Acknowledgments: None
Ethical Guidelines: This was a retrospective review, and the patient provided release of information for research consent.
Conflicts of Interests: None
References
- Giakas AM, Hohmann AL, Boyajieff E, et al. Fragility and statistical differences between surgical approaches in total hip arthroplasty. Orthopedics 17 (2025): 1-8, Epub ahead of print
- Fink B, Lass R. Diagnostischer Algorithmus der schmerzhaften Hüfttotalendoprothese. Diagnostic Algorithm for Failure Analysis of Painful Total Hip Arthroplasties. Z Orthop Unfall 154 (2016): 527-544.
- HORIBA ABX Diagnostics.ABX Pentra XL80 Benutzerhandbuch RAB131HDE, S (2010): 1-348.
- Fink B, Hoyka M, Blersch BP, et al. Graphic type differentiation of cell count data for diagnosis of early and late periprosthetic joint infection: A new method. Technol Health Care (2023): 1-12.
- Fink B, Hoyka M, Weissbarth E, et al. The Graphical Representation of Cell Count Representation: A New Procedure for the Diagnosis of Periprosthetic Joint Infections. Antibiotics (Basel) 10 (2021): 346.
- Fink B, Hoyka M, Weissbarth E, et al. A new graphic type differentiation of cell account determination for distinguishing acute periprosthetic joint infection from hemarthrosis. Antibiotics (Basel) 11 (2022): 1284.
- Parvizi J, Tan TL, Goswami K, et al. The 2018 Definition of Periprosthetic Hip and Knee Infection: An Evidence-Based and Validated Criteria. J Arthroplasty 33 (2018): 1309-1314.
- Mistry JB, Chughtai M, Elmallah RK, et al. Trunnionosis in total hip arthroplasty: a review. J Orthop Traumatol 17 (2016): 1-6.
- Sultan AA, Cantrell WA, Khlopas A, et al. Evidence-Based Management of Trunnionosis in Metal-on-Polyethylene Total Hip Arthroplasty: A Systematic Review. J Arthroplasty 33 (2018): 3343-3353.
- Cooper HJ, Della Valle CJ, et al. Corrosion at the head-neck taper as a cause for adverse local tissue reactions after total hip arthroplasty. J Bone Joint Surg Am 94-A (2012): 1655-1661.
- Cooper HJ, Urban RM, Wixson RL, et al. Adverse local tissue reaction arising from corrosion at the femoral neck-body junction in a dual-taper stem with a cobalt-chromium modular neck. J Bone Joint Surg Am 95-A (2013): 865-872.
- Yi Ba PH, Corss MB, Moric M, et al. Do serologic and synovial tests help diagnose infection in revision hip arthroplasty with metal-on-metal bearings or corrosion? Clin Orthop Relat Res 473 (2015): 498-505.
- Mikhael MM, Hanssen AD, Sierra RJ. Failure of metal-on-metal total hip arthroplasty mimicking hip infection. A report of two cases. J Bone Joint Surg Am 91-A (2009): 443-446.
- Wyles CC, Larson DR, Houdek MT, et al. Utility of synovial fluid aspirations in failed metal-on-metal total hip arthroplasty. J Arthroplasty 28 (2013): 818-823.
- Krenn V, Otto M, Morawietz L, et al. Histopathologic diagnostics in endoprosthetics: periprosthetic neosynovialitis, hypersensitivity reaction, and arthrofibrosis. Orthopäde 38 (2009): 520-530.
- Krenn V, Morawietz L, Perino G, et al. Revised histopathological consensus classification of joint implant related pathology. Pathol Res Pract 210 (2014): 779-786.
- Müller M, Morawietz L, Hasart O, et al. Histopathological diagnosis of periprosthetic joint infection following total hip arthroplasty: use of a standardized classification system of the periprosthetic interface membrane. Orthopade 38 (2009): 1087-1096.