The Frequency and Location of Hemorrhage and Infarction in Stroke Patients Having Hypertension by Computed Tomography (CT) Scan
Article Information
Md. Mosarraf Hossain1, Rashimul Haque Rimon2, Md. Anarul Islam3, Md. Shawkat Jamil4, Mohammad Arif Raihan5, Afroza Choudhury6, Mehjabin Rashid7
1Associate Professor (Neurology), Uttara Adhunik Medical College, Uttara, Dhaka, Bangladesh
2Professor (Neurology), Uttara Adhunik Medical College, Dhaka, Bangladesh
3Assistant Professor (Respiratory Medicine), Uttara Adhunik Medical College, Uttara, Dhaka, Bangladesh
4Assistant Registrar (Neurology), Uttara Adhunik Medical College, Uttara, Dhaka, Bangladesh
5Medical Officer, Dept. of Neurology, Uttara Adhunik Medical College Hospital (UAMCH), Uttara, Dhaka, Bangladesh
6Medical Officer, Dept. of Neurology, Uttara Adhunik Medical College Hospital (UAMCH), Uttara, Dhaka, Bangladesh
7Medical Officer, Dept. of Neurology, Uttara Adhunik Medical College Hospital (UAMCH), Uttara, Dhaka, Bangladesh
*Corresponding author: Md. Mosarraf Hossain, Associate Professor (Neurology), Uttara Adhunik Medical College, Uttara, Dhaka, Bangladesh
Received: 01 June 2022; Accepted: 04 June 2022; Published: 08 June 2022
Citation: Md. Mosarraf Hossain, Rashimul Haque Rimon, Md. Anarul Islam, Md. Shawkat Jamil, Mohammad Arif Raihan, Afroza Choudhury, Mehjabin Rashid. The Frequency and Location of Hemorrhage and Infarction in Stroke Patients Having Hypertension by Computed Tomography (CT) Scan. Fortune Journal of Health Sciences 5 (2022): 296-309
View / Download Pdf Share at FacebookAbstract
Introduction: Stroke is defined by the WHO as "The rapidly developing clinical symptoms and signs of focal (at times global) disturbance of cerebral function with symptoms lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin. Hypertension is a major risk factor for stroke and antihypertensive therapy provides general benefits to patients with a history of stroke or transient ischemic attacks.
Objective: To know the frequency and location of hemorrhage and infarction in stroke patients having hypertension by computed tomography (CT) scan.
Materials and Methods: This observational cross sectional study was done among stroke patients admitted in Neurology department of Uttara Adhunik Medical College Hospital (UAMCH) who have history of hypertension or taking antihypertensive drugs. Sampling was purposive and 100 samples were included in this study. All patients presenting to the emergency or neurology unit with clinical features of stroke was referred to the radiology department for CT scan of the brain. A detailed cardiovascular and neurological examination was done by the attending physician.
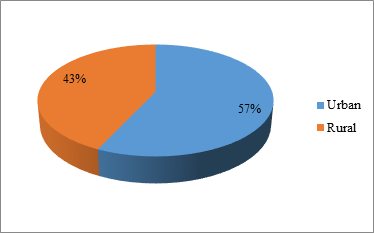
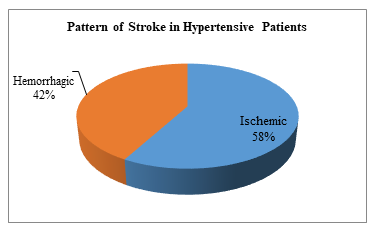
Results: In this study mean age was 60.24(±11.73) years, minimum age was 42 and highest age was 85 years. Maximum stroke were found between the ages 65 to 74 years. The mean age was 66.23(±11.8) years. My study shows 66% were male and 34% were female, and male female ratio was 1.94:1. This study shows female preponderance between 60-69 years age group but in subsequent decades there was male preponderance (p>0.05 that was not statistically significant. This present study shows that the study subjects were from both urban and rural areas with slight urban dominance (57%). The present study shows 58% were ischemic stroke and 42% were hemorrhagic stroke. In my study, haemorrhage was also more common in untreat
Keywords
Hemorrhage, Stroke Patients, Hypertension Tomography (CT) Scan
Article Details
1. Introduction
Stroke is defined by the WHO as "The rapidly developing clinical symptoms and signs of focal (at times global) disturbance of cerebral function with symptoms lasting more than 24 hours or leading to death with no apparent cause other than that of vascular origin [1, 2]. Hypertension is a major risk factor for stroke and antihypertensive therapy provides general benefits to patients with a history of stroke or transient ischemic attacks (TIA's) [3]. However, the level to which BP should be lowered to achieve maximal benefits among survivors of stroke and TIA's is not precisely known, although post hoc analysis of PROGRESS, [4] suggests a goal<13mm Hg systolic BP (SBP).
However, there had been concern the lowering BP might impair cerebral perfusion in patients with atherosclerotic ICA or MCA occlusive disease and thereby increase stroke risk [5]. At the beginning of 21stcentury and emerging of new era, cerebrovascular decease is a major cause of death and disability worldwide [6]. Among the stroke subtypes, cerebral ischemia and infarction constitute about 85-90% of the total stroke subtypes in western countries with only about 10-15% patients with cerebral haemorrhage [7]. But contrary to the western population, hemorrhagic stroke constitutes a larger percentage of stroke subtypes on this side of the globe as seen in countries like Japan and China probably because of poorly controlled hypertension [8].
In spite of general decline in the incidence of stroke in last thirty years, approximately 780000 individuals in the United States experience a clinically evident stroke each year, a substantially larger number of individuals possibly more than 9,000000 each year- seem to have clinically silent but MR imaging-detectable Tissue ischemia [9, 10]. Up to 50% of strokes may be attributable to elevated blood pressure and hypertension is the most important modifiable risk factor for stroke [11,12]. In Bangladesh the gravity of the situation can be assessed by the high incidence of admission of stroke patient in general hospitals despite lack of adequate data.
In a study in IPGM&R (now BSMMU) in 1986 it was found that of all the patients attending department of Medicine stroke patients comprised 16.96% among which 70% due to thrombo-embolism. 22% due to cerebral hemorrhage, 8% due to other causes. In 1983 it was found that stroke was the 2nd commonest cause of emergency admission in Dhaka Medicine College Hospital [13]. The risk of stroke has been shown to have direct relationship to elevation of both systolic and diastolic blood pressure in men and women of all ages; the strongest association being with elevation of systolic blood pressure. The risk of stroke is increased by about 25% with each 10mm of Hg rise in systolic blood pressure and with diastolic blood pressure of more than 110mm of Hg: risk is 15 times more than of individual with less than 80 mm of Hg [14].
The factors responsible for the inadequate level of blood pressure control include treatment resistant high blood pressure, recent start of drug therapy, patient's noncompliance with treatment, and suboptimal care [15]. Both ischemic and hemorrhagic stroke have strong gradients with blood pressure, the relative risk of ischemic and hemorrhagic stroke increases 2.23 and 3.18 times respectively. Fall in blood pressure observed over the 20th century may lead to bigger reduction in the incidence of hemorrhagic stroke compared with ischemic stroke [16]. For diagnosing and differentiating the type of stroke as early as possible, computed tomography (CT) scanning of the brain is the gold standard investigative procedure and in practice most stroke patients should ideally have a CT scan done [17]. CT scan is preferable to magnetic resonance imaging (MRI) in the acute stage because MRI does not easily detect intracranial hemorrhage within the first 48 hours after a bleeding episode [18]. An intracerebral hematoma on CT appears as a homogenous well defined area of hyper attenuation which may be surrounded by a zone of low attenuation attributable to edema, ischemia or clot retraction [19]. At some stage, as early as 2 weeks, the hematoma becomes a smaller area of low attenuation. It is found that the smaller the hematoma, the more likely it was to resolve completely [20]. Large hematoma volume, mid line shift or pineal gland displacement, intracerebral hemorrhage rupturing into the ventricular system and varying shapes of lesion in different sectional views of CT scan are the factors that predict mortality [21, 22]. Despite new post-stroke management strategies it remains a serious disease affecting not only the patient but his family as well [19, 20]. It is difficult to be sure clinically about the type of stroke (Hemorrhagic or ischemic) in majority of cases as there is no specific differentiating feature [17]. The only confirmatory test is computed tomography (CT) of brain. However, some features like sudden onset of coma or changing state of consciousness with severe headache vomiting and meningeal irritation suggest intracranial bleed similarly in cerebral infraction patient usually presents with sudden onset of stroke with lateralizing neurological deficit (hemiparesis, aphasia, homonymous hemianopia) with or without clinically delectable risk factors (hypertension. atrial fibrillation, rheumatic heart disease, recent myocardial infarction) [23]. Cerebrovascular Accident of stroke is a major cause of morbidity. For any treatment to be contemplated it is important to know whether we are dealing with a bleed or an infarer [24].
2. Materials and Methods
This observational cross sectional study was done among stroke patients admitted in Neurology department of Uttara Adhunik Medical College Hospital (UAMCH) who have history of hypertension or taking antihypertensive drugs. Study duration from January 2020 to December 2021. Sampling was purposive and 100 samples were included in this study. All patients presenting to the emergency or neurology unit with clinical features of stroke was referred to the radiology department for CT scan of the brain. A detailed cardiovascular and neurological examination was done by the attending physician. Important clinical history and risk factors was taken from each patient (ie hypertension, diabetes mellitus, coronary artery disease, smoking, alcohol intake, previous history of TIA/ stroke). USG of the carotid / vertebral artery was also done where advised. Any patients with suspected stroke were included in this study regardless of cause like tumoral bleed or secondary to vascular malformation. Infarct with secondary hemorrhagic was included under primary infarct. Repeat CT scan after 24 hour was done in any patient with clinical stroke and normal early CT scan findings.
3. Results
Table 1: Age group distribution of the study population (n=100)
|
Age group |
Frequency |
Percent |
|
40-49 years |
12 |
12 |
|
50-59 years |
19 |
19 |
|
60-69 years |
30 |
30 |
|
70-79 years |
23 |
23 |
|
80 or more |
16 |
16 |
|
Total |
100 |
100.0 |
|
Mean±SD |
62.32(±10.15) |
42-85 years |
Table -1 shows mean age was 62.32 (±10.15) years, minimum age was 42 and highest age was 85 years. Maximum were re 5th to 7th decade.
Table 2: Distribution of age according to sex (n=100)
|
Age group |
Sex |
Total |
P value |
|
|
Male |
Female |
|||
|
40-49 years |
10(15.15) |
02(5.88) |
12 |
0.41 |
|
50-59 years |
14(21.21) |
05(14.70) |
19 |
|
|
60-69 years |
14(21.21) |
16(47.05) |
30 |
|
|
70-79 years |
16(24.24) |
07(20.58) |
23 |
|
|
80 or more |
12(18.18) |
04(11.76) |
16 |
|
|
Total |
66 |
34 |
100 |
|
Table-2 shows female preponderance between 60-69 years ago group but in subsequent decades there was male preponderance (p>0.05) that was not statistically significant.
Table 3: Distribution of sex according to type of stroke (N=100)
|
Sex |
Infarction |
Hemorrhage |
Total |
|
Male |
40 |
26 |
66 |
|
Female |
18 |
16 |
34 |
Table-3 shows both ischemic 40(68.96%) &hemorrhagic 26(61.90%) strokes are more common in male patients.
Table 4: Distribution of location of infarction in CT scan (N=58)
|
Location |
Number of cases |
Frequency |
|
Capsulo-ganglionic region |
23 |
36.65% |
|
Cerebral cortex |
18 |
31.01% |
|
Thalamus |
7 |
12.06% |
|
Pons |
4 |
06.895 |
|
Cerebellum |
6 |
10.34% |
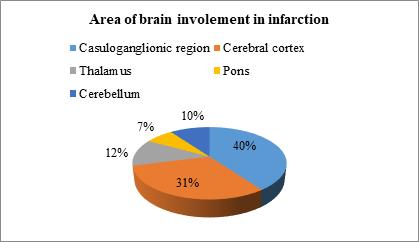
Table-4 shows infarction in CT scan involved, capsulo-ganglionic region (23 cases; 39.65%), cerebral cortex (18 cases; 31.03%), thalamus (07 cases; 12.06%), pons (04 cases; 6.89%), and cerebellum (06 cases; 10.34%) respectively.
Table 5: Location of lacunar infarction in CT scan (N=16)
|
Location |
No. of cases with lacunar infarctions (n=16) |
|
Internal capsule |
6 (37.50%) |
|
Basal ganglia |
5 (31.25%) |
|
Cerebral cortex |
3 (18.75%) |
|
Thalamus |
2 (12.50%) |
Table-5 shows predominant area involved in lacunar infarction were internal capsule (37.5%) & basal ganglia (31.25 %).
Table 6: Location of primary intracranial haemorrhage (N=40)
|
Location |
Number of cases |
Frequency |
|
Capsulo-ganglionic region |
19 |
45.23% |
|
Thalamus |
10 |
23.80% |
|
Cerebral cortex |
06 |
14.28% |
|
Pons |
03 |
07.14% |
|
Cerebellum |
02 |
4.76% |
Table-6 shows area involved in hypertensive strokes are capsule-ganglionic region (19 cases; 45.23%), thalamus (10 cases; 23.80%), cerebral cortex (06 cases; 14.28%), pons (03 cases; 7.14%) & cerebellum (02 cases; 4.76%) respectively.
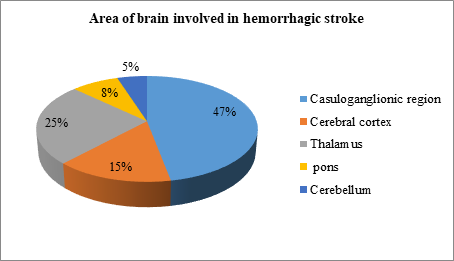
Figure VI: Distribution of brain area involved in hemorrhagic stroke.
Figure-VI shows hypertensive haemorrhage has a predilection for capsule-ganglionic region, thalamus, pons, cerebral cortex and cerebellum.
Table 7: Distribution of staging of blood pressure (BP) in study population (N=100)
|
Stage |
Frequency |
Percent |
|
Stage-I Hypertension (SBP 140-159/DBP 80-89) |
21 |
21 |
|
Stage-II Hypertension (SBP 160-179/DBP 90-99) |
42 |
42 |
|
Stage-III Hypertension (SBP 180-179/DBP2≥ 110 |
37 |
37 |
|
Total |
100 |
100 |
SBP-Systolic Blood Pressure, DBP = Diastolic Blood Pressure.
Table-7 shows 21% were stage-1, 42% were stage-II and 37% were stage-III.
Table 8: Distribution of level of hypertension among the pattern of stroke (N=100)
|
Hypertension |
Ischemia |
Hemorrhage |
P value |
|
Stage-I |
15(25.86%) |
06(14.28%) |
<0.04 |
|
Stage-II |
28(48.27%) |
14(33.33%) |
|
|
Stage-III |
15(25.86%) |
22(52.38%) |
|
|
Total |
58(100) |
42(100) |
100 |
Table-8 shows significant association of level of hypertension with Patten of stroke. Ischemic stroke were found predominantly in stage-1 (25.86%) and stage-11 (48.27%) where predominantly 22(52.38%) hemorrhagic stroke were found in stage-III (p<0.05) that was statistically significant.
Table 9: Distribution of stroke according to treatment status (N=100)
|
Level of treatment |
Ischemia |
Hemorrhage |
Total |
|
Regularly treated |
15 |
05 |
20 |
|
Irregularly treated |
25 |
11 |
36 |
|
Untreated |
18 |
22 |
44 |
Table-9 shows hemorrhage in more common in untreated (22cases, 59.09%) hypertensive patients.
Table 10: Distribution of short term complications among the types of stroke (N=100)
|
Type of Stroke |
Hyponatremia |
RTI |
Pressure Sore |
DVT |
Death |
|
Ischemia |
04(6.89%) |
06(10.34%) |
04(6.89%) |
01(1.72%) |
02(3.44%) |
|
Hemorrhage |
09(21.42%) |
10(23.80%) |
07(16.6%) |
03(7.14%) |
04(6.89%) |
|
Total |
13 |
16 |
11 |
04 |
06 |
RTI: Respiratory tract infection, DVT: Deep venous thrombosis
Table-10 shows that all the short term complications including Hyponatremia (21.42%), RTI (23.80%), Pressure sore (16.6%), DVT (7.14%) and death (9.52%) are common among hemorrhagic stroke patients.
4. Discussion
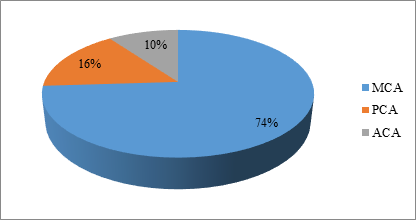
The incidence of stroke is increasing day by day in developed countries as well as well as in many developing countries including Bangladesh. Among all the risk factors hypertension is one of the most important and treatable factor. There are many reasons such as patient's compliance to take medicine and poor follow up in clinical practice that may lead to failure in reducing stroke mortality. As hypertension is one of the most important and treatable risk factor, so it is advisable to initiate community screening survey on well-defined population for early detection and treatment of it. The association between hypertension and stroke is well known. Hypertension is the greatest treatable risk is directly related to the level of blood pressure throughout its range, the incidence of stroke rises as the pressure rises. This observational cross sectional study was done among stroke patients admitted in neurology department of UAMCH who have history of hypertension or taking antihypertensive drugs. Sampling was purposive and 100 samples were included in this study. In this study mean age was 60.24(±11.73) years, minimum age was 42 and highest age was 85 years. Maximum were 5th to 7th decade. This result is compare with Hakim M et al. [25] study maximum stroke were found between the ages 65 to 74 years. The mean age was 66.23(±11.8) years. In our country a similar study was done by Chowdhury et al [26] on stroke patients and found the same age incidence of stroke between 5th to 7th decade that is nearly similar to my study. But this finding contradicted with the study conducted by WHO task Force in the western population where the peak age of incidence of stroke was 85 years. This discrepancy with the present study may be due to the reduced life expectancy in our country which is much less than that of the study group population of WHO [27]. A study by Bashar et al. found that the highest age of incidence of stroke was between 6th to 7th decades which coincided with the study of Chowdhury to and Arif et al.[28] This contradicted with the study by Aho et al. where the peak incidence was at or above the age of 85 years". This discrepancy with the present time is that a small portion of the population of our country survives up to that age. My study shows 66% were male and 34% were female, and male female ratio was 1.94:1. The result is comparable with Hakim M et al." shown male female ratio was 1.44:1 (male 59: female 41) this observation is closely approximated to the result of my study and also coincide with that of Chowdhury et al [26]. The present study defers with a previous study of Alamgir et al. [29] which showed male: female ratio was 4:1 Another study of western population in London in 1990 showed that male suffer more than female (Male female ratio was 1.5:1) [30] this also coincide with my study. The study done in Bangladesh in 1975 [29], showed a gross difference in male female and awareness of the society towards female and the availability of the hospital management to the female patients. This study shows female preponderance between 60-69 years age group but in subsequent decades there was male preponderance (p>0.05 that was not statistically significant. This present study shows that the study subjects were from both urban and rural areas with slight urban dominance (57%). This indicated that incidence of stroke is common both in urban and rural population which was contradicted by the study of Basher et al which showed mainly urban preponderamce [31]. The reason might be that the study was done in the hospitals of Dhaka where mostly theurban population could avail the hospital facilities due to economic condition. The present study was conducted in UAMCH which covers a wide range area of mainly rural areas of Gazipur, Mymensingh, Tangail and around Dhaka. The present study shows 58% were ischemic stroke and 42% were hemorrhagic stroke. These results are in agreement with various studies done in Pakistan [32-35]. Compared with Hakim M et al. [26] observed, CT finding of the studied patient showed that 61% had ischemic stroke while 39% had hemorrhagic stroke. This finding was almost similar with this study and also similar with study of Alam et al. done in Dhaka Medical College Hospital (DMCH) [36]. But this study contradicted with the study of Hayee et al. [37] which was also done in Dhaka where the incidence of ischemic stroke was higher (83.89%) Higher rate of hemorrhagic stroke has been reported in number of hospitals in countries such as Singapore, Malaysia (33%), Thailand (30%), Korea (31%), Taiwan (31%) [38, 39]. One of the cause of high incidence of hemorrhagic stroke in this hospital based present study may be due the acute admission is more related to hemorrhagic stroke. It is traditionally believed that intra-cerebral hemorrhage is more closely associated with hypertension than infarction but the Farmingham study showed that the incidence of athero-thrombotic lesions also closely correlated with the blood pressure levels. It has been observed that sudden, prolonged and profound hypertension in a hypertensive can lead to small vessel infarct [40]. In untreated cases of hypertension, hemorrhage was more common than infarction. In treated cases infarction was more common than haemorrhage [41]. In my study, haemorrhage was also more common in untreated hypertensives (59.09%), whereas ischemia in treated cases (71.42%). This study reveals that ischemic stroke were found predominantly in stage-1 (15 cases; 25.86%) & in stage-II (28 cases;48.27%) hypertensives where hemorrhage stroke were found predominantly in stage-III(22 cases; 52.38%)(p<0.05) that was statistically significant which supports the opinion of several researchers findings who found more association of stroke with high grade hypertension [42]. Of the 58 patients with infarction, the middle cerebral artery was involved in approx 74 % the posterior cerebral artery in approx 16%, the anterior circulation in 10 %. Thus most of the stroke was involved the middle cerebral arterial territory (approx 74 %). The posterior fossa was involved in 10 cases (16%) out of which 6 had cerebellar infarct and 4 had pontine infarct. In a study by Kazui et al. [43] 75% cases MCA infarction, 13% ACA and 8% PCA which is comparable to this study. Internal capsule & the basal ganglia are the prime sites of involvement in hypertensive infarctive patients which is also supported by the study of Shams & Khan et al. [44] Lacunar infarctions are deep subcortical infarctions that generally involve perforating arteries supplying regions such as deep gray matter and brainstem. Lacunar infarctions are generally less than 1 cm and are not larger than 1.5 cm in diameter [45]. Lacunar infarctions are predominantly in the basal ganglia, the white matter of the internal capsule, the brainstem, and the deep white matter of the hemispheres. Perforating arteries responsible for lacunar infarctions have been demonstrated to have microatheromata, lipohyalinosis, and fibrinoid necrosis [45]. Many of these pathologic changes have been attributed to hypertension, and a high percentage of patients with lacunar infarctions have hypertensions [46]. CT scan of brain revealed hemorrhage in the region of capsule-ganglionic region (19 cases; 45.23%), thalamus (10 cases; 23.80%), cerebral cortex (06 cases: 14.28%), pons (03 cases; 7.14%) cerebellum (02 cases; 4.76%) and sub arachnoid hemorrhage (02 cases: 4.76%) respectively. This result correlates with Weisberg LA (1990) hypertension causes bleeding in characteristics location such as basal ganglia (putamen), thalamus, pons and cerebellum 10abstract & with A. S. Fauci-2015 [47]. In this study it was revealed that short term complications are more common with hemorrhage than infarction which also correlates with several studies [1, 48, 49].
5. Limitation of the Study
The study has some limitation which is as follows:
- The study was conducted upon a small size of population which is too small to conclude over this commonest and burning issue.
- The study was conducted in a very limited area to represent.
The study time was very limited to represent as overall result.
6. Conclusion
Hypertension is a major risk factor of stroke. Infarction is more common form of stroke than hemorrhage. CT scan is important to differentiate between cerebral infarction and intracerebral hemorrhage because nowadays, proper management of the acute stroke syndrome is based on the correct diagnosis of the pathological type. Despite intensive research efforts, few effective treatments are available once stroke has occurred. An increase in compliance with the pharmacological and non-pharmacological therapeutic regimen might be a key to reduction of stroke incidence and prevalence among hypertensive patients. Treatment of hypertension significantly reduces the risk of stroke and its adequate control is a cornerstone in stroke prevention. Therefore, stroke prevention should be a primary focus for all health care providers.
Recommendations
This may not reflect the exact situation of the disease in the community. Proximity to the reality cannot be under estimated. So-large scale, multicentre study should be under taken.
References
- Dunbabin DW and Sandercock P. Preventing stroke by the modification of riskfactors. Stroke 21 (1990): 36-39.
- Hatano S. Experience from a multicenter stroke register: A preliminary report.Bulletin WHO 54 (1976): 541-553.
- Yamauchi H. Higashi T, Kagawa S, Kishibe Y. Takahashi M, Impaired perfusionmodifies the relationship between blood pressure and stroke risk in major cerebralartery disease J Neurol Neurosurg Psychiatry 8 (2013): 1-7.
- Arima H. Chalmers J, Woodward M. et al. Lower target blood pressures are safe and effective for the prevention of recurrent stroke the PROGRESS trial J Ilypertens 24 (2006): 1204-8.
- Klijn CI, Kappelle LJ. Haemodynamic stroke, clinical features, prognosis, and management. Lancet Neurol 9 (2010): 1008-17.
- Shyu WC, Lin SZ. Lee CC, Lin DD. Granulocyte colony stimulating factor for acuteischemic stroke: a randomized controlled trail CMAJ 174 (2006): 927:33. JanardhanV. Qureshi AL, Mechanism of ischemic brain injury, Curr Cardiol Resp 6 (2004): 117-123.
- Bamford J. Sandercock P. Dennis M et al. A prospective study of acutecerebrovascular disease in the community. The Oxfordshire community strokeproject (1981-86).
- Huang CY. Chan FL, Yu YL et al. Cerebrovascular disease in Hong Kong Chinese. Stroke 21 (1990): 230.
- Janardhan V. Qureshi AL, Mechanism of ischemic brain injury, Curr Cardiol Resp 6 (2004): 117-123.
- Khul CR Textor J, Cieseke J, Acute and subacute ischemic stroke at high-field-strength (3.0-T) diffusion weighted MR imaging intra individual comparative study.Radiology 234 (2005): 509-516.
- Goreer PB. Sacco RL, Smith DB Prevention of stroke a review of guidelines andmultidisciplinary consensus statement hom the national stroke association. JAMA 281 (1999): 281-1112-20.
- Golssteen LB, Adams R. Beeker K. Primary prevention of ischemic stroke: astatement for health care professionals from the stroke council of the American heartassociation Cerebrovas dis 103 (2001):103:163,182.
- Lai SM, Alter M. Friday g. Sobel E. A multifactional Analysis of risk factors forrecurrence of ischaemic stroke. Stroke 25 (1994): 958-962.
- Fang XH. Longstreth WTJ, Koronomal SC. Longitdinal study of blood pressure and stroke in over 37000 people in china. Cerebrovas dis b 11 (2001): 225-229.
- Arnett DK. Davis BR, Ford CE Pharmacogenetics association of the angiotensinconverting enzymes Insertion / Deletion polymorphism on blood pressure andcardiovascular risk in relation to antihypertensive treatment (Gen HAT) studyCirculation 11 (2005): 3374-83.
- Yun -MI. Sung J Blood pressure, hemorrhagic and ischemic stroke. The Koreannational occupational cohort study. BMJ 328 (2004): 324-25.
- Martin BM. Cerebrovascular Disease: Epidemiology. History, Examination and differential diagnosis. Medicine International 10 (196): 35-41.
- Khan NZ, Iqbal Z. Cerebrovascular disease, increasing incidence of primary intracerebral haemorrhage - a preliminary report of 100 cases. Pak J Neurol 5 (1999): 45-9.
- Savoyards M. CT. Scanning. In: Barnett HJM. Mohr JP, Stein BM, Yatsu FM, edsStroke (Pathophysiology, Diagnosis and Management) 1" edn. New York Churchill Livingstone (1986): 189-219.
- Kreel L Key R, Woo J, Wong HY, Nicholls MG. The radiological (CT) and clinical sequelae of primary intracerebeakhaemomhage Br J Radio 64 (1991): 1096-1100.
- Franke CT, Van Swieten JC, Algra A, Van Gijin J. Prognostic factors in patients with intracerebral haemorrhage. J NeurolNeurosurg Psychiatry 55 (1992): 653-7.
- Donnan GA investigation of patient with stroke and transient ischaemic attacks. Lancet 339 (1992): 473-6.
- Kay R. Wong S KA. Yuk YL. Low Molecular Weight Heparin in the treatment of Acute ischemic stroke. N Engl J Med 333 (1995): 1588-93.
- Khan J, and urRehman A, Comparison of Clinical Diagnosis with Computed Tomography in Ascertaining Type of Stroke, J Ayub Med coll Abbottabad 17 (2005): 1-4.
- Hakim M, Hayee MA, Saha CK, Ali Z. Hasan SA Sociodemographic study of posterior circulation stroke survival, JCNCTA 20 (2009): 23-26.
- Chowdhury SGM Ahmed Q. Alam MN, Arif SM. Roy PK. Stroke in patients having inadequate or irregular antihypertensive therapy. Bangladesh Med Res Coun Bull 16 (1990): 53-60.
- Aho K. Harmsen P, Hatano S, Cerebrovascular Disease in the community Results of a WHO collaborative study. Bull WHO 58 (1980): 113-30.
- Arif SM A dissertation on study on risk factor foe in Bangladesh (1993).
- Alamgir SM Mannan MA, Cerebrovascular disease: A report of 53 cases, Bangladesh Med Res Coun Bull 1 (1995): 45-50.
- Thomson SBN, Morgan Epideminology of stroke. In Thompson SBNEDS. Occupational therapy for stroke rehabilitation, London Chapman and Hall 1 (1990): 1-14.
- Bashar A. A dessertation on "Study of risk factor of stroke" (1995): 78-80.
- Alam I. Haider 1. Wahab F Khan W. Taqweem MA, Nowsherwan. Risk factors stratification in 100 patients of acute stroke, J Postgrad Med Inst 18 (2004): 583-91.
- Demchuk AM, Coutts SB. Alberta stroke program early CT score in acute stroke triage. Neuroimaging Clin North Am 15 (2005): 409-19.
- Ali L. Jamil H, Shah MA. Risk factors in stroke. J Coll Physicians Surg Pak 7 (1997): 7-10.
- Koch S. Pabon D. Rabinstein AA. Chirinos J. Romano JG, Forteza A. Stroke etiologsamong Haitians living in Miami.
- Alam B. Stroke Evaluation of Risk Factors. Bangladesh Journal of Neuroscience 15 (1999): 14-18.
- Hayee A. Haque A. AnwarullahAKM.Haqre A. Akhtar N. Analyss of Risk factors of Stroke in 472 Cases. Bangladesh Journal of Neuroscience 14 (1999): 41-54.
- Poungvann N. stroke in developing world. Lancet 352 (1998): 19-20.
- Wong KS International prospective hospital-based study of acute stroke incidence Lancet 352 (1998).
- Kannel WB, Wolf PA, Vesta J et al. Epidemiological assessment of the role of BP in stroke. The Farmingham study JAMA 219 (1970): 301-10.
- Chhetri PK, Raut S. Computed tomography scan in the evaluation of patients with stroke. Journal of College of Medical Sciences-Nepal 8 (2012): 24-31.
- http://emedicine medscape.com/article/323120-overviews aw2aab6efcb 2014) 15:2014.
- Kazui S. Sawada T. Naritomi H et al. Angiographic evaluation of brain infarction. Stroke 24 (1993): 549-553.
- Shams UR, Khan MA. Clinical versus CT scan diagnosis in stroke. A comparativestudy of 50 cases. J Ayub Med Coll, Abbottabad 14 (2000): 2-5.
- CM Fisher. Capsular infarcts. ActaNeuropathol 36 (1979): 65-73.
- Michael Marks. Cerebral Ischemia and Infarction. In Scott W Atlas MRI of the brain and spine Third edition Lippincott Williams and Wilkins 18 (2002): 919.79.
- Fauci AS, Kasper DL, Hauser SL et al. Neurologic Disorders. Harrison's Principles of Internal Medicine. McGraw-Hill Education 446 (2015): 2583.
- Chiu D. Peterson L. Elkind MS, Rosand J, Gerber LM. Comparison of outcomes after intracerebralhemorrhage and ischemic stroke.
- Ingeman A. Andersen G. Hundborg HH, et al. In hospital medical complications, length of stay, and mortality among stroke unit patients. Stroke 42 (2011): 3214.