The Efficacy and Patient Satisfaction with a Mini-Scleral Lens after penetrating Keratoplasty
Article Information
Cristina Peris-Martínez*1,2, Magdalena Catalán-Gómez1, Esteban Porcar-Izquierdo3, Juan Carlos Montalt-Rodrigo3, María José Roig-Revert1
1Fundación de Oftalmología Médica (FOM) de la Comunitat, Valenciana, Valencia, Spain
2Faculty of Medicine and Odontology, University of Valencia, Spain
3Department of Optics, Optometry and Vision Sciences, Physics College, University of Valencia, Burjassot, Valencia, Spain
*Corresponding Author: Cristina Peris Martínez, Fundación de Oftalmología Médica (FOM) de la Comunitat, Valenciana, Valencia, Spain
Received: 17 March 2023; Accepted: 12 April 2023; Published: 27 April 2023
Citation: Cristina Peris-Martínez, Magdalena Catalán-Gómez, Esteban Porcar-Izquierdo, Juan Carlos Montalt-Rodrigo, María José Roig-Revert. The Efficacy and Patient Satisfaction with a Mini- Scleral Lens after penetrating Keratoplasty. Journal of Surgery and Research. 6 (2023): 167-173.
View / Download Pdf Share at FacebookAbstract
Background: To analyse the efficacy and patient satisfaction of fitting a mini-scleral lens (SL) after keratoplasty surgery in patients unsatisfied with their visual outcomes.
Material and Methods: A retrospective chart review of 22 consecutive patients was performed between 2018 and 2019. Demographic data, indications for keratoplasty, ocular parameters, and visual results were evaluated. In addition, subjective visual quality (SVQ) and comfort, complications, daily wear time, and the reason for discontinuing SL wear during the 6-month follow-up were analysed.
Results: Twenty-two eyes of 22 patients (6 females and 16 males; mean age 48.82 ± 17.19 years) were assessed. Keratoconus was the main indication for keratoplasty (9 eyes, 40.9%), followed by corneal opacities (5 eyes), and Fuchs endothelial dystrophy (4 eyes). High refractive anisometropia was found in 14 eyes (63.6%) and 6 eyes presented significant irregular astigmatism. LogMAR visual acuity improved significantly with SL when compared with the best spectacle-correction (mean, 0.12 ± 0.12 vs 0.52 ± 0.33, respectively; p < 0.01). Six patients discontinued SL wear (27.3%). Among the other 16 patients, the mean daily wear time was 11.47 ± 1.52 h; of these, 14 (87.5%) were successfully fitted and enjoyed favourable SVQ and comfort. No significant complications were found during the follow-up period.
Conclusions: Mini-scleral lenses may be a safe and effective alternative for treating complicated eyes after keratoplasty; they may provide optimal visual rehabilitation and/or restore binocular vision with significant efficacy and patient satisfaction.
Keywords
Penetrating keratoplasty, Keratoconus, Irregular astigmatism, Scleral contact lenses
Penetrating keratoplasty articles; Keratoconus articles; Irregular astigmatism articles; Scleral contact lenses articles
Gastroparesis articles Gastroparesis Research articles Gastroparesis review articles Gastroparesis PubMed articles Gastroparesis PubMed Central articles Gastroparesis 2023 articles Gastroparesis 2024 articles Gastroparesis Scopus articles Gastroparesis impact factor journals Gastroparesis Scopus journals Gastroparesis PubMed journals Gastroparesis medical journals Gastroparesis free journals Gastroparesis best journals Gastroparesis top journals Gastroparesis free medical journals Gastroparesis famous journals Gastroparesis Google Scholar indexed journals Indocyanine green articles Indocyanine green Research articles Indocyanine green review articles Indocyanine green PubMed articles Indocyanine green PubMed Central articles Indocyanine green 2023 articles Indocyanine green 2024 articles Indocyanine green Scopus articles Indocyanine green impact factor journals Indocyanine green Scopus journals Indocyanine green PubMed journals Indocyanine green medical journals Indocyanine green free journals Indocyanine green best journals Indocyanine green top journals Indocyanine green free medical journals Indocyanine green famous journals Indocyanine green Google Scholar indexed journals Gastrojejunal anastomosis articles Gastrojejunal anastomosis Research articles Gastrojejunal anastomosis review articles Gastrojejunal anastomosis PubMed articles Gastrojejunal anastomosis PubMed Central articles Gastrojejunal anastomosis 2023 articles Gastrojejunal anastomosis 2024 articles Gastrojejunal anastomosis Scopus articles Gastrojejunal anastomosis impact factor journals Gastrojejunal anastomosis Scopus journals Gastrojejunal anastomosis PubMed journals Gastrojejunal anastomosis medical journals Gastrojejunal anastomosis free journals Gastrojejunal anastomosis best journals Gastrojejunal anastomosis top journals Gastrojejunal anastomosis free medical journals Gastrojejunal anastomosis famous journals Gastrojejunal anastomosis Google Scholar indexed journals Antrectomy articles Antrectomy Research articles Antrectomy review articles Antrectomy PubMed articles Antrectomy PubMed Central articles Antrectomy 2023 articles Antrectomy 2024 articles Antrectomy Scopus articles Antrectomy impact factor journals Antrectomy Scopus journals Antrectomy PubMed journals Antrectomy medical journals Antrectomy free journals Antrectomy best journals Antrectomy top journals Antrectomy free medical journals Antrectomy famous journals Antrectomy Google Scholar indexed journals gastroparesis articles gastroparesis Research articles gastroparesis review articles gastroparesis PubMed articles gastroparesis PubMed Central articles gastroparesis 2023 articles gastroparesis 2024 articles gastroparesis Scopus articles gastroparesis impact factor journals gastroparesis Scopus journals gastroparesis PubMed journals gastroparesis medical journals gastroparesis free journals gastroparesis best journals gastroparesis top journals gastroparesis free medical journals gastroparesis famous journals gastroparesis Google Scholar indexed journals pacemakers articles pacemakers Research articles pacemakers review articles pacemakers PubMed articles pacemakers PubMed Central articles pacemakers 2023 articles pacemakers 2024 articles pacemakers Scopus articles pacemakers impact factor journals pacemakers Scopus journals pacemakers PubMed journals pacemakers medical journals pacemakers free journals pacemakers best journals pacemakers top journals pacemakers free medical journals pacemakers famous journals pacemakers Google Scholar indexed journals blood dilation articles blood dilation Research articles blood dilation review articles blood dilation PubMed articles blood dilation PubMed Central articles blood dilation 2023 articles blood dilation 2024 articles blood dilation Scopus articles blood dilation impact factor journals blood dilation Scopus journals blood dilation PubMed journals blood dilation medical journals blood dilation free journals blood dilation best journals blood dilation top journals blood dilation free medical journals blood dilation famous journals blood dilation Google Scholar indexed journals antrectomy articles antrectomy Research articles antrectomy review articles antrectomy PubMed articles antrectomy PubMed Central articles antrectomy 2023 articles antrectomy 2024 articles antrectomy Scopus articles antrectomy impact factor journals antrectomy Scopus journals antrectomy PubMed journals antrectomy medical journals antrectomy free journals antrectomy best journals antrectomy top journals antrectomy free medical journals antrectomy famous journals antrectomy Google Scholar indexed journals Clostridium difficile articles Clostridium difficile Research articles Clostridium difficile review articles Clostridium difficile PubMed articles Clostridium difficile PubMed Central articles Clostridium difficile 2023 articles Clostridium difficile 2024 articles Clostridium difficile Scopus articles Clostridium difficile impact factor journals Clostridium difficile Scopus journals Clostridium difficile PubMed journals Clostridium difficile medical journals Clostridium difficile free journals Clostridium difficile best journals Clostridium difficile top journals Clostridium difficile free medical journals Clostridium difficile famous journals Clostridium difficile Google Scholar indexed journals
Article Details
1. Introduction
Keratoplasty surgery is a procedure in which the damaged cornea is replaced entirely (penetrating keratoplasty) or partially (lamellar keratoplasty) with a donated corneal graft [1,2]. The main indication for keratoplasty is keratoconus, followed by Fuchs endothelial dystrophy, pseudophakic bullous keratopathy, fungal keratitis, corneal scarring and others [2,3]. Despite good graft clarity that can be achieved after keratoplasty, some patients can still present unsatisfactory visual outcomes. For example, a previous study reported that after surgery, 18 out of 104 eyes (17%) proved unsatisfactory with the best spectacle-correction [2]. These patients mainly presented an increase in higher-order aberrations, significant degrees of astigmatism and/or high refractive anisometropia [2-5]. A previous study reported that higher-order aberrations in these cases can be 5.5 times more than normal eyes [5]. Consequently, in these cases, nonsurgical options to achieve visual rehabilitation and binocularity are mainly directed toward fitting rigid gas-permeable lenses [6-23]. These lenses are able to mask higher-order aberrations with the tear film between the posterior surface of the lens and the anterior surface of the cornea [24]. Other previous studies also reported fitting other types of lenses, such as soft and hybrid lenses, although to a lesser extent [25,26]. Previous studies have described different types of rigid gas-permeable lenses (corneal, semi-scleral, and mini or large scleral lenses) fitted on eyes after keratoplasty [6-23]. Firstly, large diameter corneal lenses (10 to 12 mm) were fitted to achieve a better centration [6-10]. These lenses had different back surface designs and/or lens eccentricity, depending on the different corneal profiles [8]. Therefore, the fitting procedure of these special designs (e.g. toric, bitoric, reverse geometry and others) can be difficult and require more time. Moreover, the results in some cases with high astigmatism can be unsuccessful [17]. In recent years, scleral lenses (SL) have gained popularity because the fitting procedure is easier than that of corneal lenses; moreover, as their diameter is large, SL vault the whole cornea [17]. There are different diameter SL available for post-keratoplasty eyes (large and mini-SL). Some previous studies report fitting SL with diameters of 18.50 or 19 mm (large SL); [15,16] however, eye care providers are mainly fitting mini-SL with diameters ranging from 15.80 to 16.50 mm [17-19,23]. For example, a study showed that the mean SL diameter was 16.6 mm (range 15.6 to 18.4 mm) [18]. Recently, a study based its strategy for treating cases of irregular corneas, including post-keratoplasty eyes, with lenses of 16.50 mm in diameter [23]. On the other hand, previous studies reported that visual acuity is significantly improved after fitting SL on post-keratoplasty eyes [15-19], however, little is known in the literature about the efficacy and patient satisfaction (subjective visual quality and comfort) wearing these lenses. In addition, criteria of success were not reported [15,23]. The present study describes the efficacy and patient satisfaction, as well as visual rehabilitation results, success rate, complications and clinical experience when fitting a mini-scleral lens (15.80 to 16.50 mm in diameter) in complicated eyes that have undergone keratoplasty surgery with suboptimal visual outcomes.
Material and Methods
Patients
A retrospective review of clinical data from the records of 22 patients who were fitted with a mini-SL (MSK; Conóptica SL, Hecht Contactlinsen) after keratoplasty was performed. Patients presented unsatisfactory visual outcomes with the best spectacle-correction or other types of contact lenses (except SL). They were selected from a database at Fundación de Oftalmología Médica (FOM) de la Comunitat Valenciana, between January 2018 and December 2019. A single optometrist at the FOM fitted the lenses in all cases. None of the patients presented ocular-surface diseases, allergies or systemic diseases. Moreover, they did not use medication that would have interfered in contact lens wear, nor had they undergone ocular surgery (except keratoplasty). All patients had consented to the use of their clinical data for research purposes. This study complied with the ethical standards required by the FOM and the University of Valencia, which concurs with the tenets of the Declaration of Helsinki.
Data collection
The data retrieved from medical records included demographic aspects (age and gender), initial diagnosis, previous ocular and contact lens wear history, time elapsed after keratoplasty surgery until fitting contact lenses, and the eye examination values before fitting the lens. The eye examination outcomes assessed were visual acuity with the best spectacle correction, corneal topographic analysis using the Pentacam Eye Scanner (Oculus Inc., Wetzlar, Germany) and visual acuity obtained with the contact lens. Moreover, the SL parameters (such as diameter, back optic zone radius and power), number of visits and lenses required until the SL was optimal for dispense were recorded. Finally, subjective visual quality on a typical five-level Likert scale (1, very poor; 2, poor; 3, neither poor nor favourable; 4, favourable; and 5, very favourable), subjective comfort on a typical five-level Likert scale (1, highly uncomfortable; 2, uncomfortable; 3, neither uncomfortable nor comfortable; 4, comfortable; and 5, very comfortable), daily wear time, complications, and the reason for discontinuing SL wear during the 6-month follow-up were studied.
Criteria of success
With regard to successful fitting criteria (including efficacy and patient satisfaction), complete success was considered when the patient had the following results [27,28]:
1) Visual acuity with SL improved two or more decimal lines when compared to the best spectacle-corrected visual acuity;
2) Contact lens daily wear time greater than, or equal to, 10h;
3) And subjective visual quality and comfort (patient satisfaction) values over 3 (i.e. favourable or very favourable for visual quality, and comfortable or very comfortable for subjective comfort; values 4 or 5 in a range of 1 to 5).
Partial success in fitting was considered when a parameter did not improve when compared to the previous conditions for complete success, and it was deemed unacceptable if two parameters were worse. The wear time criteria as a measure of success was based on the study by Ortenberg et al [15].
Lens Used
The lens in the present study is made of a high-DK gas-permeable material (Hexafocon B) Boston® X02 (Polymer Technology Corp., Wilmington, MA, USA). Its oxygen transmissibility ISO FATT Method: Dk is 141 x 10-11cm3 O2(cm)/[(sec.)(cm2)(mm Hg)]@35°C. The parameters of this lens are the following:
Diameter 12.30 to 16.50 mm (in 0.10-mm steps; standard diameters, 16.50 / 15.80 / 15.20 mm).
Base curves range from 5.00 to 10 mm (in 0.05-mm steps),
Power ranges from +30.00 to -30.00 D (in 0.25-D steps).
As described by the manufacturer, the lens is available in two exclusive profiles, normal MSK (for a prolate cornea) and reverse MSK (for an oblate cornea), so they can be fitted optimally to any corneal profile.
Fitting procedure
All contact lenses were fitted by the trial-lens method. The lens was selected using a specific software developed by the manufacturer (the apex scleral fit). This program shows the profile of the trial lens for four areas in the fitting procedure (the central, para-central and limbal corneal zones, as well as the peripheral or scleral zone). This process makes it easy to modify the sagittal heights in these four areas and it simulates the appropriate fitting. Parameters of corneal topography, eccentricity, visible iris diameter and corneal profile (prolate or oblate) are necessary for this estimation. Once the trial lens had been decided upon (by taking into account its suitability with the corneal and scleral surfaces), it was inserted in the eye for at least 30 minutes. Then, suitable fitting of the lens on the ocular surface was verified with a slit lamp. In addition, the lens was checked for good position and optimum movement. Finally, an over-refraction was performed which, together with the four parameters of the lens, was necessary in order to manufacture the lenses. At the next visit, the manufactured SL was inserted and allowed to settle on the eye for 2 hours, so that it could be verified that there were no adverse ocular effects or compression on the conjunctival vessels under the contact lens. If the lens did not show an appropriate fit, its parameters or over-refraction were changed. Finally, the patients were instructed in lens care and handling and they were advised to increase lens wear by 1 hour a day, until the following visit 1 week later. After 8 hours of lens wear, the appropriate fit was again evaluated following the same previous procedures (verification of visual acuity, lens position and movement, no corneal staining, and no compression on corneal areas or on the conjunctival vessel under the contact lens; Figure 1). Follow-up appointments were made for 1, 3, and 6 months later.
|
Parameters |
Patients (%) |
|
|
Sex |
Male |
16 (72.7) |
|
Female |
6 (27.3) |
|
|
Age |
< 20 years |
1 (4.5) |
|
21-40 years |
5 (22.7) |
|
|
41-60 years |
9 (40.9) |
|
|
> 60 years |
7 (31.8) |
|
|
Refractive error |
Hyperopia > 10.00 D |
2 (9.1) |
|
(Spherical Equivalent) |
Hyperopia (0.00 to +10.00 D) |
6 (27.3) |
|
Low myopia (-0.25 to -6.00 D) |
6 (27.3) |
|
|
Medium myopia (-6.25 to -10.00 D) |
2 (9.1) |
|
|
Impracticable assessment |
6 (27.3) |
|
|
Corneal astigmatism |
0.00-2.00 D |
1 (4.5) |
|
2.25-4.00 D |
8 (36.4) |
|
|
4.25-6.00 D |
5 (22.7) |
|
|
> 6.00 D |
2 (9.1) |
|
|
Impracticable assessment |
6 (27.3) |
Table 1: Demographic and clinical data after keratoplasty surgery (N = 22).
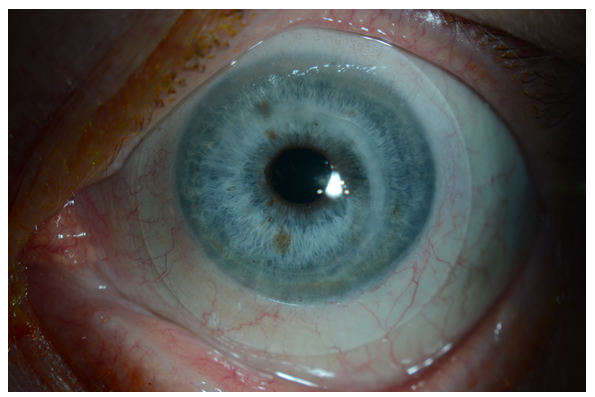
Figure 1: A mini-scleral contact lens fitted after keratoplasty surgery in this study.
|
Corneal Anomalies |
Patients (%) |
|
Keratoconus |
9 (40.9) |
|
Corneal opacities |
5 (22.7) |
|
Fuchs endothelial dystrophy |
4 (18.2) |
|
Herpes simplex virus |
1 (4.5) |
|
Pseudomonas keratitis |
1 (4.5) |
|
Reticular corneal dystrophy |
1 (4.5) |
|
Corneal perforation |
1 (4.5) |
Table 2: Indications for keratoplasty surgery (N = 22)
The mean logMAR visual acuity before keratoplasty was 0.77 ± 22. After keratoplasty, logMAR visual acuity improved with the best spectacle-correction (0.52 ± 0.33; p = 0.33). An average of 5 months (range 3 to 8) elapsed before fitting the SL. Once fitted, patients improved up to 0.12 ± 0.12 (p = 0.01, when compared to the best spectacle-correction. These outcomes were maintained during the 6-month follow-up (Figure 2).
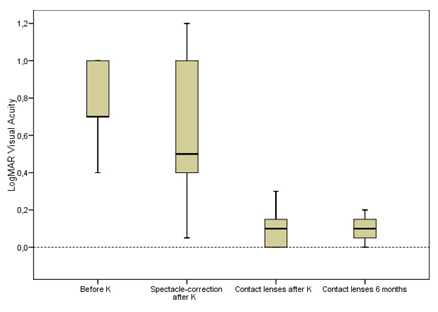
Figure 2: LogMAR visual acuity before and after keratoplasty surgery, as well as with a mini-scleral contact lens, and after 6 months of lens wear. K = keratoplasty surgery.
Data analysis
Statistical analysis was performed using SPSS 26.0 software (SPSS Inc., Chicago, IL, USA). A nonparametric statistical test (the Wilcoxon test) was used to compare differences in visual acuity before and after keratoplasty with the best spectacle-correction, as well as with the contact lens. All visual acuities were converted to logMAR (logarithm of the minimum angle of resolution) for statistical analysis. The level of statistical significance was taken as P < 0.05.
Results
Table 1 shows the demographic and clinical data of the twenty-two post-keratoplasty eyes. The mean ± SD age of the sixteen Caucasian males and six Caucasian females was 48.82 ± 17.19 years (range 19 to 74 years). All patients underwent keratoplasty in only eye, keratoconus being the main indication, followed by corneal opacities or corneal scars and Fuchs endothelial dystrophy (Table 2). After keratoplasty, high refractive anisometropia was found in fourteen patients (63.6%), and they all had prolate corneas, except three cases (oblate cornea). Moreover, six eyes presented significant irregular astigmatism and/or abnormal corneal profiles; hence, it was difficult to determine refractive status. The mean logMAR visual acuity before keratoplasty was 0.77 ± 22. After keratoplasty, logMAR visual acuity improved with the best spectacle-correction (0.52 ± 0.33; p = 0.33). An average of 5 months (range 3 to 8) elapsed before fitting the SL. Once fitted, patients improved up to 0.12 ± 0.12 (p = 0.01, when compared to the best spectacle-correction. These outcomes were maintained during the 6-month follow-up (Figure 2). Fourteen eyes were fitted with SL measuring 16.50 mm in diameter and eight eyes with SL measuring 15.80 mm in diameter. The mean back optic zone radius was 7.89 ± 0.68. A prolate MSK design was manufactured for 19 lenses and a reverse MSK design for 3. An average of 1.33 ± 0.50 lenses (range 1 to 2) were required until deemed optimal for dispensing, and 2.68 ± 0.75 visits (range 2 to 4) were needed to complete the fitting process. During the follow-up period (6 months), six patients discontinued SL wear (27.3%). The reasons for discontinuation were that 2 patients had corneal graft rejection, 2 experienced intolerance or discomfort, 1 was dissatisfied with his/her vision, and 1 found it difficult to insert and remove the SL. Among the other 16 patients, the mean daily wear time was 11.47 ± 1.52 h. Fourteen patients stated that SL were comfortable or very comfortable, and 2 reported them to be neither uncomfortable nor comfortable. In addition, all of them improved two or more decimal lines when compared to the best spectacle-corrected vision and reported that their visual quality was favourable or very favourable. These results demonstrate that 14 of 16 patients (87.5%) achieved a completely successful fitting. No significant adverse ocular events occurred during this period.
Discussion
The patients in the present study were mainly males (16/6) and the mean age was 48 years. These demographic values concur with those of previous studies fitting SL in post-keratoplasty eyes, where the proportion of males was significantly higher than females (approximately 2/3 males and 1/3 females) [15-18]. In addition, the mean age in these studies ranged between 43 to 59 years, and they reported that keratoconus was the main indication for keratoplasty, as do the results in this study. After keratoplasty, in some cases, fitting contact lenses represents a unique challenge. It should be noted that the reattachment of the corneal graft in the bed of the new cornea may cause a complex irregular corneal shape. Commonly, there is no continuous transition from the centre to the periphery of the cornea, and it presents irregular areas where there is a different flattening between the meridians (Figure 3). Moreover, keratoplasty can be steeper or flatter than the host cornea, and in many cases a mixture of both in different areas of the cornea. Therefore, a great variability of corneal profiles can be found in these patients. Consequently, when visual outcomes are suboptimal with the best spectacle-correction, contact lenses (mainly rigid gas-permeable as reported previously) are a suitable option for visual rehabilitation and/or restoring binocular vision (if refractive anisometropia occurs). The fitting procedure of SL was based on the sagittal depth. The lens should vault the cornea with sufficient central, paracentral and limbal clearance (approximately 200, 100, 50 µ after lens settling, respectively). A sagittal depth that is too great may cause central bubbles under the lens, as well as less visual acuity. The landing curve should rest on the sclera aligned parallel to the conjunctiva. An excessive compression on conjunctival blood vessels or impingement should be avoided [18,29]. In the process of selecting the trial lens, the software used to simulate the fit was significantly helpful, so much so that 16 of 22 cases (72.7%) only needed one lens for dispensing, and in the other 6 cases, only two were needed. Changes were made to increase the corneal clearance (2 cases), and variations in the limbal and/or landing curve for the other four cases. Moreover, the majority of cases only needed two or three visits to complete the fitting process. Therefore, the fitting procedure appears to be feasible for the mini-SL used in the present study. Although patients achieved an improved of visual acuity after keratoplasty (0.52 ± 0.33), they were still unsatisfied with their best spectacle-correction. However, after fitting the mini-SL, they achieved an average of 0.12 ± 0.12 logMAR visual acuity, which concurs with previous studies in fitting SL in post-keratoplasty eyes (range 0.09 to 0.21).15-19 It should be noted that those previous studies that fitted greater diameters (18.50 or 19 mm) presented slightly worse logMAR visual acuity values [15,16]. A greater amount of fluid-reservoir behind the lens could be the cause in these cases.29 Therefore, fitting mini-SL with diameters between 15.80 and 16.50mm (as in the present study) may provide better visual rehabilitation [17-19]. After 6 months the follow-up, the rate of discontinuation of mini-SL wear was 27.3% (6 of 22 cases). Two previous studies on post-keratoplasty eyes reported similar values (35.4% and 27%);18,15 however, in other studies these rates were lower than 20% [16,19]. The concept of successful fitting (including efficacy and patient satisfaction) is rarely reported in the literature. Ortenberg et al. referred to success in wearing time as being able to wear a SL for at least 10 h a day.15 Another study developed a questionnaire to determine subjective aspects of the patients having a mini-SL fitted.23 On a scale of 0 to 10 points, patients were asked about aspects of “Comfort”, “Visual quality”, “Handling rating”, and “Wearing time”. The authors referred to these aspects as subjective scores for efficacy in successfully fitted patients. However, no success criteria were reported. Recently, studies fitting corneo-scleral lenses in keratoconus patients used the same successful fitting criteria as those used in the present study [27,28]. According to the successful fitting criteria used, of the 16 patients who completed this study, 14 patients achieved complete success (daily wear time ≥ 10h, comfortable or very comfortable lens wear, favourable or very favourable subjective visual quality, and decimal visual acuity improved two or more lines compared to the best spectacle-correction after keratoplasty), and two patients were considered as partially successful (subjective comfort was neither uncomfortable nor comfortable). The mean daily wear time of the 16 patients was 11.47 h. Other previous studies fitting SL in post-keratoplasty eyes also reported similar values (range 9.62 to 11.8 h a day) [15-17]. Finally, no significant complications were found during the follow-up period. Two cases presented mild adverse events, such as slight conjunctival hyperaemia. These cases were resolved with a lubricant and weak hypotonic ophthalmic solution (0.1 % of sodium hyaluronate) without preservatives, moreover removal and cleaning of the lens after 6 h of wear. Future studies with a greater sample size are needed to confirm the outcomes of this study.
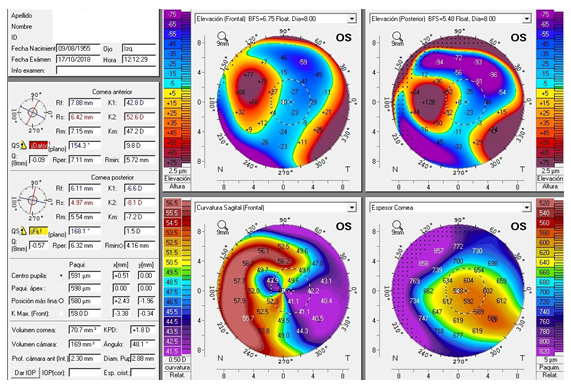
Figure 3: Pentacam corneal topography in a post-keratoplasty left eye. Anterior elevation map (top left). Posterior elevation map (top right). Keratometric map (bottom left). Pachymetry map (bottom right).
Conclusions
Mini-scleral lenses may be a valid alternative option for eye care providers when treating complicated eyes after keratoplasty surgery with a significant degree of astigmatism and/or refractive anisometropia, like the cases presented in this manuscript. Hence, they may provide visual rehabilitation and/or restoring binocular vision with significant efficacy and patient satisfaction.
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
References
- Reinhart WJ, Musch DC, Jacobs DS, et al. Deep anterior lamellar keratoplasty as an alternative to penetranting keratoplasty; a report by the American Academy of Ophtalmology. Ophthalmology 118 (2011): 209-218.
- Asena L, Altinors DD, Yilmaz G, et al. Visual rehabilitation after penetrating keratoplasty. Exp Clin Transplant 14 (2016): 130-134.
- Wietharn BE, Driebe WT. Fitting contact lenses for visual rehabilitation after penetrating keratoplasty: Eye Contact Lens Sci Clin Pract 30 (2004): 31-33.
- Bruce AS, Catania LJ. Clinical applications of wavefront refraction. Optom Vis Sci 91 (2014): 1278-1286.
- Pantanelli S, MacRae S, Jeong TM, et al. Characterizing the wave aberration in eyes with keratoconus or penetrating keratoplasty using a high-dynamic range wavefront sensor. Ophthalmology 114 (2007): 2013-2021.
- Eggink FA, Nuijts RM. A new technique for rigid gas permeable contact lens fitting following penetrating keratoplasty. Acta Ophthalmol Scand 79 (2001): 245-250.
- Lin JC, Cohen EJ, Rapuano CJ, et al. RK4 (Reverse-Geometry) contact lens fitting after penetrating keratoplasty. Eye Contact Lens 29 (2003): 44-47.
- Gruenauer-Kloevekorn C, Kloevekorn-Fischer U, Duncker GI. Contact lenses and special back surface design after penetrating keratoplasty to improve contact lens fit and visual outcome. Br J Ophthalmol 89 (2005): 1601-1608.
- Geerards AJ, Vreugdenhil W, Khazen A. Incidence of rigid gas-permeable contact lens wear after keratoplasty for keratoconus: Eye Contact Lens 32 (2006): 207-210.
- Phan VA, Kim YH, Yang C, et al. Bitoric rigid gas permeable contact lenses in the optical management of penetrating keratoplasty. Contact Lens Anterior Eye 37 (2014): 16-19.
- Segal O, Barkana Y, Hourovitz D, et al. Scleral contact lenses may help where other modalities fail. Cornea 22 (2003): 308-310.
- Visser ES, Visser R, Van Lier HJ, et al. Modern scleral lenses part I: clinical features. Eye Contact Lens 33 (2007): 13-20.
- Visser ES, Visser R, Van Lier HJ, et al. Modern scleral lenses part II: patient satisfaction. Eye Contact Lens 33 (2007): 21-25.
- Romero-Jiménez M, Flores-Rodríguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye 36 (2013): 146-150.
- Ortenberg I, Behrman S, Geraisy W, et al. Wearing time as a measure of success of scleral lenses for patients with irregular astigmatism. Eye Contact Lens 39 (2013): 381-384.
- Severinsky B, Behrman S, Frucht-Pery J, et al. Scleral contact lenses for visual rehabilitation after penetrating keratoplasty: long term outcomes. Cont Lens Anterior Eye 37 (2014): 196-202.
- Alipour F, Behrouz MJ, Samet B. Mini-scleral lenses in the visual rehabilitation of patients after penetrating keratoplasty and deep lamellar anterior keratoplasty. Cont Lens Anterior Eye 38 (2015): 54-58.
- Barnett M, Lien V, Li JY, et al. Use of scleral lenses and miniscleral lenses after penetrating keratoplasty: Eye Contact Lens 42 (2016): 185-189.
- Rocha GA, Miziara PO, Castro AC, et al. Visual rehabilitation using mini-scleral contact lenses after penetrating keratoplasty. Arq Bras Oftalmol 80 (2017): 17-20.
- Abou Samra WA, Badawi AE, Kishk H, et al. Fitting tips and visual rehabilitation of irregular cornea with a new design of corneoscleral contact lens: objective and subjective evaluation. J Ophthalmol 12 (2018): 1-8.
- De Luis Eguileor B, Etxebarria Ecenarro J, Santamaria Carro A, et al. Irregular corneas: improve visual function with scleral contact lenses. Eye Contact Lens 44 (2018): 159-163.
- Ozek D, Kemer OE, Altiaylik P. Visual performance of scleral lenses and their impact on quality of life in patients with irregular corneas. Arq Bras Oftalmol 81 (2018): 475-480.
- Suarez C, Madariaga V, Lepage B, et al. First Experience With the ICD 16.5 mini-scleral lens for optic and therapeutic purposes. Eye Contact Lens 44 (2018): 44-49.
- Gemoules G. Therapeutic effects of contact lenses after refractive surgery. Eye Contact Lens 31 (2005): 12-22.
- Katsoulos C, Nick V, Lefteris K, et al. Fitting the post-keratoplasty cornea with hydrogel lenses. Cont Lens Anterior Eye 32 (2009): 22-26.
- Altay Y, Balta O, Burcu A, et al. Hybrid contact lenses for visual management of patients after keratoplasty. Niger J Clin Pract 21 (2017): 451-455.
- Montalt JC, Porcar E, España-Gregori E, et al. Visual quality with corneoscleral contact lenses for keratoconus management. Cont Lens Anterior Eye 41 (2018): 351-356.
- Montalt JC, Porcar E, España-Gregori E, et al. Visual quality with corneo-scleral contact lenses after intracorneal ring segment (ICRS) implantation for keratoconus management. Cont Lens Anterior Eye 42 (2019): 111-116.
- Van der Worp E. A Guide to Scleral Lens Fitting, Version 2.0 [monograph of the Internet]. Forest Grove, OR: Pacific University; 2015 [cited 30 Jan 2020]. Available from: http://commons.pacificu.edu/mono/10/
