The Effect of Valsalva maneuver on Migraine Headache
Article Information
Kamran Shirbache1, Ali Shirbacheh2, Mozhgan Sadat Hashemi1, Ghasem Pishgahi1, Mansour V Shirbacheh3, Omid Mirmosayyeb4,Vahid Shaygannejad5*, Mansoureh Togha6,7*
1Tehran University of Medical Sciences, Tehran, Iran
2Isfahan University of Medical Sciences, Isfahan, Iran
3St. Joseph Medical Clinic, 1708 S Yakima Ave, Tacoma, WA 98405, États-Unis
4Isfahan Neurosciences Research Center, Isfahan University of Medical Sciences, Isfahan, Iran
5Department of Neurology, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
6Professor of Neurology, Tehran University of Medical Sciences, Tehran, Iran
7President of Iranian Headache Association, Tehran, Iran
*Corresponding authors: Mansoureh Togha, Department of Neurology, Tehran University of Medical Sciences, Tehran, Iran
Vahid Shaygannejad, Department of Neurology, School of Medicine, Isfahan University of Medical Sciences, Isfahan, Iran
Received: 12 July 2022; Accepted: 19 July 2022; Published: xx July 2022
Citation: Kamran Shirbache, Ali Shirbacheh, Mozhgan Sadat Hashemi, Ghasem Pishgahi, Mansour V Shirbacheh, Omid Mirmosayyeb,Vahid Shaygannejad, Mansoureh Togha. The Effect of Valsalva Maneuver on Migraine Headache. Archives of Clinical and Biomedical Research 6 (2022): 632-638.
View / Download Pdf Share at FacebookAbstract
Background: This study investigated the effect of Valsalva maneuver (VM) on migraine headache (MH).
Method: This is a double-blind, randomized clinical trial that has been registered with the IRCT20210525051405N1 code. The VM was induced among the study group in the acute phase of MH using a simulator. In the control group, a pseudo-simulator was used in the acute phase of MH. The patients recorded the effects of this maneuver on the severity of their headaches on a checklist, and their data were analyzed through logistic regression under the generalized estimating equations (GEE) method.
Results: We evaluated 74 migraine patients,42 in the intervention group and 32 in the control group. The age and gender indexes were equalized in both groups. This study shows that there is no significant statistical difference in the Pain Score of the two groups before and after the VM (B=0.842, P value= 0.074). There were however significant statistical differences in Overall Headache Relief Rate (B= 2.550, P value=0.000) and the rate of relief improved with repeated use (B=2.172, P value=0.000) in the study group. VM did not affect use of analgesic medications in the study group (B=0.518, P value=0.160).
Conclusion: The Valsalva maneuver improved the headache of migraine patients overall, and it could be a remedial technique for migraine patients, but more extensive studies are needed.
Keywords
Valsalva maneuver; migraine; headache; treatment
Article Details
Introduction
Headache is a common medical condition. There are different types of headaches including migraine, tension-type, and cluster headaches [1]. Headache is experienced by nearly every one and can cause significant physical suffering and disruption of daily activities. Migraine Headache (MH) is the most common disabling form of headaches [2] There have been many different modalities used in treating MH with over the counter non-steroidal anti-inflammatory drugs (NSAIDs) being the most commonly used modality. In addition to being of limited efficacy, chronic NSAIDs use can cause significant side effects such as peptic ulcer, weight gain, drowsiness and osteoporosis [3]. There has been a continuing effort to develop non-pharmacological treatments. Many individuals suffering from headache have found partial relieve in lying down in a quiet/dark room, drinking lukewarm fluids or taking a shower [4]. Neuromodulation are new techniques in which neurostimulation devices are used to produce a rehabilitative biological response in MH [5-8].
In this study, we are evaluating the efficacy of VM as a safe method to relieve migraine headaches. Although not all migraine headaches experience these stages completely, four stages are described for migraines. Stage 1: prodrome or alert stage, stage 2: Aura or hypersensitivity phase, stage 3: Attack or onset of headache and stage 4: Post-drom which takes some time for the person to return to normal life [2]. Cerebral blood flow has been shown to differ in different phases of acute MH. Facco E has shown that in the prodromal phase, the cerebral blood flow is reduced while it is increased in the attack phase when compared to normal [11]. This has been reaffirmed by studies done by Cheng MH and Jakob [9,10]. VM is a basic maneuver where the participant first takes a deep breath and then forcefully exhales while the mouth and the nose are blocked for 15 seconds [12]. VM results in rapid sequence of changes in heart rate and blood pressure in five distinct phases [12]. During phase 0, (deep inspiration) negative intra-thoracic pressure increases venous return to the heart with resultant decreased systemic blood pressure, increased heart rate and increased peripheral vasoconstriction. In Phase I (starts of forced exhalation against a closed airway) intra-thoracic and intra-abdominal pressure peaks. This results in an increase in venous return and an increase in systolic and diastolic pressure without a change in heart rate. In Phase II (relieving the obstruction and continuing the exhalation normally) there is a drop in venous return as well as stroke volume and compensatory increased in heart rate. In Phase III (End of maneuver and start normal breathing) the intra-thoracic pressure returns to normal which in turn increases right sided venous return and a decrease in peripheral blood volume. In Phase IV (continuing normal breathing) the increased in venous return leads to an increase in stroke volume and cardiac output. As a result, VM alters the peripheral (cerebral) and central blood flow during its different phases [13]. The correlation of different phases of VM and cerebral (peripheral) as well as changes in cerebral blood flow during a MH [9,14], creates the possibility of using VM as a simple [15] and safe method in treatment of MH.
Methods and Materials
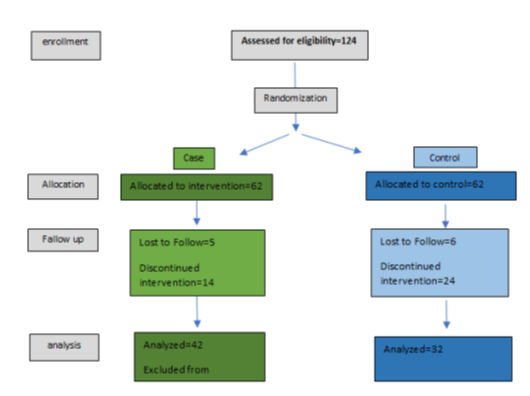
This study is a double-blind, randomized clinical trial that evaluated the effect of VM on the acute phase of MH. All subjects had received a diagnosis of MH by a board-certified neurologist based on ICHD3 criteria [2]. The subjects were randomized into an intervention and control group (blocked method at Sealdenvelop.com). Using G-POWER software, the size of each group was calculated to be 62. (Reliability coefficient = 95%, Study power factor = 80%, P1 = 30%, P2 = 13%, Z = 0.05, B = 0.2). Inclusion criteria are migraine patients who have been diagnosed with migraine for more than one year and with the onset age before age 50. Each patient underwent a full history and physical examination. Individuals with history of cerebral aneurysm, recent brain surgery, hemorrhagic stroke, recent myocardial infarction, heart failure, coronary artery disease, syncope, retinopathy and retinal surgery, intraocular lens implantation, uncontrolled diabetes, aortic valve stenosis, carotid artery stenosis, uncontrolled hypertension, systolic blood pressure less than 90 mm Hg and cough induced headache were excluded from the study [12]. Each patient was asked to exhale into a device for 15 seconds during acute phase of MH. The patients were asked to repeat this maneuver three times in a row with 5-minute intervals. A standardized checklist was to record headache characteristics during the three months of the study. All patients were educated on using the device and filling the checklists. They scored the severity of their headache from 1 to 10, then used the device and again rescored the headache after that and expressed whether they felt better after the maneuver or not. Patients were instructed to take pain killers after the third maneuver as needed. They were asked to record at least 4 episodes of headache during the study period. In the study group, the device used generated resistant pressure of 40 mmHg whereas in patients were given a similar device, but no pressure was generated against the exhalation when used, resulting in no VM. Weekly (in person or phone) checkup was conducted for each patient. Following the completion of the study, the related data, including the differences in headache scores before and after the maneuver (Pain Score difference), overall headache relief rate after the maneuver, improving effect of the device on multiple uses and the decrease in analgesic consumption were extracted from the checklists and entered the SPSS software version 22. The data were analyzed through Generalized Estimated Equations (GEE) in both groups and the effect of intervention on different episodes of headache was evaluated statistically (Figure 1).
Ethical considerations
Anyone wishing to participate in the project signed the consent form or expressed their consent orally. Due to the harmlessness of the intervention and the exclusion of patients who were at risk of vulnerability, there was no danger to the patients in the study. Also, their information remained confidential. Every patient was announced that using the device might be effective in relieving the headache and they were allowed to take painkillers after using the device 3 times if needed. Therefore, there is no moral problem with the plan. The Ethics ID= IR.TUMS.NI.REC.1399.043.
Results
In this study, we included 124 patients from two neurologic clinics in Tehran and Isfahan from the 15th of November 2020 to the 15th of September 2021 for 10 months. Eventually, 74 patients properly cooperated with us until the end of the project and filled the checklist correctly. During the follow-up, 19 patients from the intervention group left the study, 5 patients did not answer their phones without any reason and 14 patients decided to give the devices back because their terrible headaches disabled them from using the device. In the control group, 30 patients left the project. Six of them interrupted their communication without giving us any reason and 24 patients gave up since they did not trust the devices and their severe headaches obligated them to take medicine quickly. As long as all of the patients were allowed to end their cooperation in any steps of the project based on the ethical consideration, this drop in sample size was inevitable. One patient's data was incomplete in the intervention group and was excluded during analysis. In the following, the patients' demographic information is mentioned in the table 1.
|
|
Intervention Group |
Control Group |
P-value |
|
|
Age(Mean, SD) |
39.40(9.983) |
40.39(9.215) |
0.715 |
|
|
Sex |
Male |
8 (19.0 %) |
5 (15.6 %) |
0.766 |
|
Female |
34 (81.0%) |
27 (84.4 %) |
||
|
Total |
42 |
32 |
||
Table 1: Demographic Characteristics
There were 42 patients in the intervention group and 32 patients in the control group, with one missing patient who did not register his group on the checklist. Gender ratio and Age average were equalized among both groups. (P value=0.766 for gender and P value=0.715 for Age). As far as patients recorded 4 episodes of migraine headache, three maneuver done in each attack, the efficacy of the Valsalva maneuver has been evaluated 12 times per case by scoring the headache before and after the maneuver. Additionally, the patients expressed their experience for each episode (of the 4 times) about the overall headache relief rate, improving effect on reuses and whether their need for analgesic has decreased or not; however, some patients experienced less than 4 attacks during the study and we had to settle for less. Based on the table 2 information, the change in headache score before and after the maneuver among the intervention and control group was not statistically significant. With B score=0.842 which is higher in the intervention group, the P-value is 0.074. (95% Confidence interval= -.080-1.765). The other important factor checked in this study was Overall Headache Relief Rate demonstrating the feeling of headache relief after Valsalva maneuver in the patients; for each headache episode, the patients scored this item in this way: 1 means no relief, 2 means feeling relief less than 50% and 3 means feeling relief more than 50%. Thereby, 4 relief rate scores were recorded for each patient. The probability distribution is multinomial and the information is set in a cumulative logit. As demonstrated in the table 2, in the interventional group, the overall headache relief rate was significantly improved with B= 2.550 via intervention group the P-value assigned <0.001. (95% Confidence interval= 1.791-3.308). Another item worth noticing is the improving effect of the device on reusing it multiple times during each headache episode, which means patients found the maneuver more helpful when they repeated it several times. For this factor, 1 stands for no improving effect and 2 means better effect sensation after multiple uses. Patients in the intervention group recorded a higher score with B=2.17 and P value<0.001 than the control group. (95% Confidence intervals= 1.131-3.213). The last parameter was the analgesic consumption which patients recorded whether they took any painkiller during the episode despite the maneuver. Score 1 means No medication and score 2 stands for painkiller use with B=0.518 and P value= 0.160. This item was not statically different among the two groups. (95% Confidence intervals= -0.205-1.242). We did not have any side effect related to the Valsalva maneuver during the study.
|
Parameter |
B |
Confidence interval |
P-value |
||
|
Pain Score difference (in 12 episodes) |
0.842 |
-0.08 |
1.765 |
0.074 |
|
|
Overall Headache Relief Rate |
No relief =1 |
2.55 |
1.791 |
3.308 |
0 |
|
Relief <50% =2 |
|||||
|
Relief >50% =3 |
|||||
|
Improving effect on reuse |
No =1 |
2.172 |
1.131 |
3.213 |
0 |
|
Yes =2 |
|||||
|
Reduce analgesic consumption (in 4 attacks) |
No =1 |
0.518 |
-0.205 |
1.242 |
0.16 |
|
Yes =2 |
|||||
Table 2: GEE analysis of main parameters among the intervention group and the control group
Discussion
We evaluated the effect of Valsalva maneuver on acute phase of migraine, and it seems helpful for patients to try it as an available remedy promptly. Although the improvement in pain score was not significant statistically, it was marginal and we suppose that in larger sample size the results would be statically meaningful. Noticeably, the two other parameters, Overall Headache Relief Rate and improving effect on reuse, show that VM can rehabilitate the patients' headache positively, which could be a valuable achievement. Nonetheless, the analgesic consumption did not change despite VM. We noticed all the patients take their painkillers as usual after the VM if they need. Since this was a research idea, it was not ethical to deprive patients of analgesics. Additionally, most patients did not trust the device completely and conducted their routine plans for more assurance. As far as investigated in several studies, the Valsalva maneuver (VM) could influence many physiologic mechanisms in the human body [16]. In this domain, various publications are confirmative in each part; Cardiovascular hemodynamic response [17], Respiratory indices (18), Ear-Nose-Throat and Autonomic nervous system [19-21]. The threshold pressure almost suggested is 40 mmHg for 15 seconds [17]; since the lower pressure could not cause the expected effects [16]. In addition, for more long-lasting effects, performing the VM multiple times is recommended in some studies, especially on cardiac autonomic function [22]. The unknown etiology of migraine leads to several theories explaining the concept of its mechanism; however, the dominating hypothesis is based on few propositions like Vascular Hypothesis [23], Activation of pain modulatory regions [24,25]. Neuronal Hyper excitability and its genetics [26] and neurotransmitters expression, mainly CGRP (27). What encourages us to conduct this project is investigating whether the physiologic effects of VM could improve migraine headache or not. Regarding the novelty of the subject, we must concentrate on the fundamental articles even if they are old [28]. The main purpose is to find a logical correlation between the VM and its effect on migraine via pathophysiological mechanisms. Thus, the primitive studies justifying the nature of VM and migraine would be considerably helpful. In an article, Symon examined the mechanism of auto-regulatory response in cerebral blood flow. By cranial instrumentalization connected to the right atrium through a femoral vein, they evaluated brain hemodynamic components and vascular response with different percentages of CO2. They examined the validity of two metabolic and myogenic theories in the mechanism of the effect of auto-regulatory response on cerebral blood flow. Myogenic theory emphasizes on the effect of local reflex on the vessel wall in the auto-regulatory response and considers its effect to be separate from the systemic reflex. The researchers stated that with a decrease in perfusion, acidic metabolites accumulate and dilatation of the vessel wall occurs subsequently, but since the initial response of cerebral arteries to autoregulation is very fast in less than 15 seconds, metabolic theory does not seem to justify this phenomenon. The paper notes that CO2 as a vasodilator cannot reverse the effect of the auto-regulatory response on increased intravascular pressure, and although CO2 competes with other vasodilators of the autonomic system, there is no evidence that it competes with vasoconstrictors [29]. As far as cerebral autoregulation is affected noticeably during VM [31], all these mechanisms would be manipulated by this maneuver. Additionally, CO2 increases in phases 2 and 3 of VM, the mechanism of action of this factor in VM on cerebral blood flow, vascular ton and eventually the severity of migraine headache is questionable [29]. As mentioned in many references, the different phases of VM accompany fluctuations in blood pressure [13-16]. Our results on overall headache relief rate in cases support that VM may downregulate the vascular cascade, which finally induces migraine attack. The other idea mentioned in a study conducted by Frank and his colleagues is the rate of changes in cerebrovascular resistance [32], leading to a blood flow increase in the Middle Cerebral Artery(MCA). Although not so recent, this study propounds new points on how VM acts binary. The methodology used was transcranial doppler ultrasound that measured blood pressure at different levels during VM. These pressure alterations may overlap with pressure changes during migraine phases and decline the unknown mechanism causing pain relief. The idea that sympathetic response and cerebrovascular vasodilation, triggered by the VM, calls to mind headaches' associated improvement in migraine. It does worth reviewing another essential study that evaluated 3 patients with migraine in the acute phase of headache [33]. It considered the intracarotid stenosis as a pathology for aura in migraine and differently, extracranial dilation for the headache phase. The findings are based on angiographic observation and direct measurement of cerebral blood flow during migraine. We suppose, therefore, retrying this maneuver and analyzing the response regarding the migraine with aura and migraine without aura would be substantially relevant. In recent years, a considerable number of neurologists intend to introduce Cerebrospinal Fluid (CSF) pressure as an important background of migraine theme [34], taking into consideration the significant results they have achieved. The VM for a long time used to be assisted in detection of different diseases. An article published in 2013 states that VM could differentiate the primary cough-induced headache from the secondary. Owing to obstruction of CSF dynamic in patients with a posterior fossa occupied lesion, this maneuver could act as a trigger that starts the blockage [35]. The other study that examined the effect of increased intracranial pressure on cerebral blood flow proposed VM as a promoter that increases CSF pressure. These two studies are in harmony with the notion that VM trouble CSF circulation by a probable obstructive interaction. Seymour et al. also suggest the VM as a raiser of CSF pressure; however, their cases have previously had a brain tumor [30], as in Russel’s study, all the patients with positive response to the Valsalva test suffered from a posterior fossa lesion [35]. This hypothesis is highly valued in our project regarding CSF pressure converter since the former evaluations guess in migraine, we may confront an imbalance in cerebral fluid. After VM we see a reduction in the pressure and flow of CSF which may lead to headache relief [36]. The other remarkable idea is the effect of hypoxia on primary headaches such as migraine. The features found in high altitude headache and acute mountain sickness deeply matched migraine criteria [37]. In 2016, in an epidemiologic review, the prevalence of migraine was evaluated in the population living at altitude (4300 meters) [38]. That is to say, there is a link between hypoxia and migraine, especially migraine with aura [39]. According to physiologic theories, when PaO2 falls below 60 mmHg, a neurochemical cascade occurs through which NO secretion, calcitonin gene-phenotype, CGRP and Adenosine expression [38]; that attend depolarization in the cortex of brain, neurogenic inflammation and destruction of blood brain barrier [40,41]. The VM in some notions could simulate a transient hypoxic condition, but without these chronic subsequences. G perry et al. discussed in a study how different phases of VM alter oxygenation in cerebral artery. The main finding is coherent relation between the intensity of VM and the reduction in prefrontal artery oxygenation. The more intense VM resulted in greater reduction in flow velocity and TOI (Total Oxygenation Index) specifically during phases 2 and 3, returning to normal in the next phases. As a possible mechanism, these frequent passing changes in PaO2 may disturb the NO secretion cycle and manipulate the area of cerebral blood flow pattern. These alterations decrease the cerebral arteriovenous oxygen content difference. The cerebral vascular resistance (CVR) increases at first but decreases then, which might decrease headache severity [42]. Based on our findings, the VM could be beneficial for migraine patients during their headache episodes. It seems that more studies are needed to work on this field in order to study the efficiency of VM on mild, moderate or severe migraine, the chronic and acute phase of headache separately and even on tension type headache. Also, VM with other pressure of less or more than 40 mmHg should be investigated for gaining better results. Additionally, examination of patients performing the VM during MH more profoundly could lead to defining an instruction to use this maneuver with different pressures and various intervals to gain the highest positive feedback from it. All of these matters could be an interesting topic for future research.
Conclusion
We investigated the effect of VM on migraine. Although the determined mechanism is not clear, it appeared to have a rehabilitative effect on migraine headache overall which could be a practical remedy for patients during the headache. The drop in sample size was a limitation of our study which could be compensated by a larger quantity of patients in future studies to evaluate the efficiency of this maneuver on different severities and types of headaches separately and also on different VM pressure.
Conflicts of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
References
- Stovner L, Hagen K, Jensen R, et al. The global burden of headache: A documentation of headache prevalence and disability worldwide. Cephalalgia 27 (2007): 193-210.
- Headache Classification Subcommittee of the International Headache Society. The International Classification of Headache Disorders, 3rd edtn (beta version). Cephalalgia 33 (2013): 629-808.
- Lipton RB, Bigal ME. Chronic daily headache: is analgesic overuse a cause or a consequence? Neurology 61 (2003): 154-155
- Prophylaxis of migraine: general principles and patient acceptance. Domenico D’Amico1 and Stewart J Tepper 12 (2011): 21-32.
- Silberstein SD, Dodick DW, Saper J, Het al. Safety and efficacy of peripheral nerve stimulation of the occipital nerves for the management of chronic migraine: results from a randomized, multicenter, double-blinded, controlled study. Cephalalgia 32 (2012): 1165-1179.
- Martelletti P, Jensen RH, Antal A, et al. Neuromodulation of chronic headaches: position statement from the European Headache Federation. J Headache Pain 14 (2013): 86.
- Saper JR, Dodick DW, Silberstein SD, et al. Occipital nerve stimulation for the treatment of intractable chronic migraine headache: ONSTIM feasibility study. Cephalalgia 31 (2011): 271-285.
- Lipton RB, Goadsby PJ, Cady RK, et al. PRISM study: occipital nerve stimulation for treatment-refractory migraine. Cephalalgia 29 (2009): 30.
- Jakob M Hansen, Christoph J Schankin. Cerebral hemodynamics in the different phases of migraine and cluster headache J Cereb Blood Flow Metab 39 (2019): 595-609.
- Cheng MH, Wen SL, Zhou HJ, et al. Evaluation of headache and regional cerebral flood flow in patients with migraine. Clin Nucl Med 38 (2013): 874-877.
- Facco E, Munari M, Baratto F, et al. Regional cerebral blood flow (rCBF) in migraine during the interictal period: different rCBF patterns in patients with and without aura. Cephalalgia 16 (1996): 161-168.
- L Pstras, K Thomaseth, J Waniewski et al. The Valsalva manoeuvre: physiology and clinical examples. Acta Physiol 217 (2016): 103-119.
- Attubato MJ, Katz ES, Feit F, et al. Venous changes occurring during the Valsalva maneuver: evaluation by intravascular ultrasound. Am J Cardiol 74 (1994): 408-410.
- Dodick DW. A Phase-by-Phase Review of Migraine Pathophysiology. Headache 58 (2018): 4-16.
- American Academy of Neurology. Assessment: clinical autonomic testing report of the Therapeutics and Technology. Assessment Subcommittee of the American Academy of Neurology. Neurology 46 (1996): 873-880.
- Felker GM, Cuculich PS, Gheorghiade M. The Valsalva maneuver: a bedside "biomarker" for heart failure. Am. J. Med 119 (2006): 117- 122.
- O’Connor P, Sforzo GA, Frye P. Effect of breathing instruction on blood pressure responses during isometric exercise. Phys Ther 69 (1989): 757-761.
- Low PA. Testing the autonomic nervous system. Semin Neurol. 23 (2003): 407-421.
- Ewing DJ, Martyn CN, Young RJ, et al. The value of cardiovascular autonomic function tests: 10 years' experience in diabetes. Diabetes Care 8 (1985): 491-498.
- Singer W, OpferGgehrking TL, McPhee BR, et al. Influence of posture on the Valsalva manoeuvre. Clin. Sci 100 (2001): 433-440
- Junqueira LF. Teaching cardiac autonomic function dynamics employing the Valsalva (Valsalva-Weber) maneuver. Adv Physiol Educ 32 (2008): 100-106.
- Goadsby PJ. The vascular theory of migraine- A great story wrecked by the facts. Brain 132 (2009): 6-7.
- Moulton EA, Becerra L, Johnson A, et al. Altered hypothalamic functional connectivity with autonomic circuits and the locus coeruleus in migraine. PLoS One 9 (2014): e95508.
- Pietrobon D, Moskowitz MA. Pathophysiology of migraine. Annu Rev Physiol 75 (2013): 365-391.
- Magis D, Lisicki M, Coppola G. Highlights in migraine electrophysiology: Are controversies just reflecting disease heterogeneity? Curr Opin Neurol 29 (2016): 320-330.
- Iyengar S, Ossipov MH, Johnson KW. The role of calcitonin gene-related peptide in peripheral and central pain mechanisms including migraine. Pain 158 (2017): 543-559.
- Porth CJ, Bamrah VS, Tristani FE, et al. The Valsalva maneuver: mechanisms and clinical implications. Heart Lung 13 (1984): 507-518.
- Symon L, Held K, Dorsch NW. On the myogenic nature of the autoregulatory mechanism in the cerebral circulation. Eur Neurol 6 (1972): 11-18.
- Kety SS, Shenkin HA, Schmidt CF. The effects of increased intracranial pressure on cerebral circulatory functions in man. J Clin Invest 27 (1948): 493-499.
- Tiecks FP, Douville C, Byrd S, et al. Evaluation of impaired cerebral autoregulation by the Valsalva maneuver. Stroke 27 (1996): 1177-1182.
- Tiecks FP, Lam AM, Matta BF, et al. Effects of the valsalva maneuver on cerebral circulation in healthy adults. A transcranial Doppler Study. Stroke 26 (1995): 1386-1392.
- Hachinski VC, Olesen J, Norris JW, et al. Cerebral hemodynamics in migraine. Can J Neurol Sci 4 (1977): 245-249.
- Togha M, Shirbache K, Rahmanzadeh R, et al. Prevalence of new-onset migraine in patients with idiopathic intracranial hypertension in comparison to the general population. Iran J Neurol 17 (2018): 161-166.
- Lane RJ, Davies PT. Modified Valsalva test differentiates primary from secondary cough headache. J Headache Pain 14 (2013): 31-42.
- Bhadelia RA, Madan N, Zhao Y, et al. Physiology-based MR imaging assessment of CSF flow at the foramen magnum with a valsalva maneuver. AJNR Am J Neuroradiol 34 (2013): 1857-1862.
- Schneider M, Bernasch D, Weymann J, et al. Characteristics of high-altitude headache. High Alt Med Biol, Abstract 5th World Congress on Mountain Medicine Barcelona (2003).
- Britze J, Arngrim N, Schytz HW, et al. Hypoxic mechanisms in primary headaches. Cephalalgia 37 (2017): 372-384.
- Arregui A, Cabrera J, Leon-Velarde F, et al. High prevalence of migraine in a high-altitude population. Neurology 41 (1991): 1668-1669.
- Dempsey JA, Morgan BJ. Humans in hypoxia: A conspiracy of maladaptation?! Physiology (Bethesda) 30 (2015): 304-316.
- Reet CS, Stoner JF and Tang X. Baroreflex and chemoreflex controls of sympathetic activity following intermittent hypoxia. Auton Neurosci Basic Clin 174 (2013): 8-14.
- Perry BG, Cotter JD, Mejuto G, et al. Cerebral hemodynamics during graded Valsalva maneuvers. Front Physiol 5: 349.
- Andreas Straube, J Ellrich, O Eren, et al. Treatment of chronic migraine with transcutaneous stimulation of the auricular branch of the vagal nerve (auricular t-VNS): a randomized, monocentric clinical trial. J Headache Pain16 (2015): 543.