The Effect of Third Trimester Corticosteroid Therapy on Fetal Doppler Velocimetry in Gestational Hypertension Complicated By Intrauterine Growth Restriction
Article Information
Hany Maged Abd El Aal1*, Doaa Mohamed Ahmed Mohamed Hassan2
1Department of Obstetrics and Gynecology, Faculty of Medicine, Al-Azhar University, Egypt
2Al Nasr Hospital for Health Insurance, Nasr City, Behind Rabaa El Adaweya Mosque, Cairo, Egypt
3Reproductive health and Family planning department, National Research Centre, Egypt
*Corresponding Author: Hany Maged Abd El Aal, Department of Obstetrics and Gynecology, Faculty of Medicine, Al-Azhar University, Egypt
Received: 04 June 2019; Accepted: 13 June 2019; Published: 17 June 2019
Citation:
Neha Abd El Moniem Mohamed Zakaria, Hany Maged Abd El Aal, Doaa Mohamed Ahmed Mohamed Hassan, Mahmoud Alalfy. The Effect of Third Trimester Corticosteroid Therapy on Fetal Doppler Velocimetry in Gestational Hypertension Complicated By Intrauterine Growth Restriction. Obstetrics and Gynecology Research 2 (2019): 014-034.
View / Download Pdf Share at FacebookAbstract
Background
Althouh there is a great advance in antenatal care, gestational hypertension still one of the major reasons of maternal and neonatal morbidity and mortality. For this reason, early screening of gestational hypertension and fetal growth retardation can permit cautious antenatal monitoring and proper timing of delivery to steer clear of serious complications.
Patient and Methods
This is a prospective study that included 100 singleton pregnant women with gestational hypertension and complicated with IUGR fetuses who were divided into 2 groups (A and B), each group consists of 50 patients: All patients in group A subjected to fetal Doppler flow indices measurement before corticosteroid administration, and repeated within five days after its administration. Its effect on fetal outcome detected after termination of pregnancy. While women in group B included 50 patients who did not receive corticosteroid therapy. Fetal Doppler flow indices was measured, and after termination of pregnancy effect on fetal outcome was detected as well.
Results
There was statistically significant difference between the study group after corticosteroid administration and the control group regarding the mean Doppler indices in the form of (MCA PI-RI, UMA PI-RI and CPR). MCA shows higher values in study group after corticosteroid administration than the control group (PI 1.52 ± 0.10 and 1.5 ± 0.18 and RI from 0.78 ± 0.12 to 0.76 ± 0.02. While UMA shows lower values in study group after corticosteroid administration than the control group (PI 1.31 ± 0.16 and 1.36 ± 0.08 and RI 0.72 ± 0.01 and 0.73 ± 0.02. CPR also shows higher values in study group after corticosteroid administration than the control group 1.05 ± 0.05 and 1.04 ± 0.05.
Conclusio
Keywords
Doppler Velocimetry, Corticosteroid Therapy, Obstetrics and Gynecology
Doppler Velocimetry articles Doppler Velocimetry Research articles Doppler Velocimetry review articles Doppler Velocimetry PubMed articles Doppler Velocimetry PubMed Central articles Doppler Velocimetry 2023 articles Doppler Velocimetry 2024 articles Doppler Velocimetry Scopus articles Doppler Velocimetry impact factor journals Doppler Velocimetry Scopus journals Doppler Velocimetry PubMed journals Doppler Velocimetry medical journals Doppler Velocimetry free journals Doppler Velocimetry best journals Doppler Velocimetry top journals Doppler Velocimetry free medical journals Doppler Velocimetry famous journals Doppler Velocimetry Google Scholar indexed journals Corticosteroid Therapy articles Corticosteroid Therapy Research articles Corticosteroid Therapy review articles Corticosteroid Therapy PubMed articles Corticosteroid Therapy PubMed Central articles Corticosteroid Therapy 2023 articles Corticosteroid Therapy 2024 articles Corticosteroid Therapy Scopus articles Corticosteroid Therapy impact factor journals Corticosteroid Therapy Scopus journals Corticosteroid Therapy PubMed journals Corticosteroid Therapy medical journals Corticosteroid Therapy free journals Corticosteroid Therapy best journals Corticosteroid Therapy top journals Corticosteroid Therapy free medical journals Corticosteroid Therapy famous journals Corticosteroid Therapy Google Scholar indexed journals Obstetrics and Gynecology articles Obstetrics and Gynecology Research articles Obstetrics and Gynecology review articles Obstetrics and Gynecology PubMed articles Obstetrics and Gynecology PubMed Central articles Obstetrics and Gynecology 2023 articles Obstetrics and Gynecology 2024 articles Obstetrics and Gynecology Scopus articles Obstetrics and Gynecology impact factor journals Obstetrics and Gynecology Scopus journals Obstetrics and Gynecology PubMed journals Obstetrics and Gynecology medical journals Obstetrics and Gynecology free journals Obstetrics and Gynecology best journals Obstetrics and Gynecology top journals Obstetrics and Gynecology free medical journals Obstetrics and Gynecology famous journals Obstetrics and Gynecology Google Scholar indexed journals Fetal articles Fetal Research articles Fetal review articles Fetal PubMed articles Fetal PubMed Central articles Fetal 2023 articles Fetal 2024 articles Fetal Scopus articles Fetal impact factor journals Fetal Scopus journals Fetal PubMed journals Fetal medical journals Fetal free journals Fetal best journals Fetal top journals Fetal free medical journals Fetal famous journals Fetal Google Scholar indexed journals antenatal care articles antenatal care Research articles antenatal care review articles antenatal care PubMed articles antenatal care PubMed Central articles antenatal care 2023 articles antenatal care 2024 articles antenatal care Scopus articles antenatal care impact factor journals antenatal care Scopus journals antenatal care PubMed journals antenatal care medical journals antenatal care free journals antenatal care best journals antenatal care top journals antenatal care free medical journals antenatal care famous journals antenatal care Google Scholar indexed journals gestational hypertension articles gestational hypertension Research articles gestational hypertension review articles gestational hypertension PubMed articles gestational hypertension PubMed Central articles gestational hypertension 2023 articles gestational hypertension 2024 articles gestational hypertension Scopus articles gestational hypertension impact factor journals gestational hypertension Scopus journals gestational hypertension PubMed journals gestational hypertension medical journals gestational hypertension free journals gestational hypertension best journals gestational hypertension top journals gestational hypertension free medical journals gestational hypertension famous journals gestational hypertension Google Scholar indexed journals fetal growth articles fetal growth Research articles fetal growth review articles fetal growth PubMed articles fetal growth PubMed Central articles fetal growth 2023 articles fetal growth 2024 articles fetal growth Scopus articles fetal growth impact factor journals fetal growth Scopus journals fetal growth PubMed journals fetal growth medical journals fetal growth free journals fetal growth best journals fetal growth top journals fetal growth free medical journals fetal growth famous journals fetal growth Google Scholar indexed journals Gestational Hypertension articles Gestational Hypertension Research articles Gestational Hypertension review articles Gestational Hypertension PubMed articles Gestational Hypertension PubMed Central articles Gestational Hypertension 2023 articles Gestational Hypertension 2024 articles Gestational Hypertension Scopus articles Gestational Hypertension impact factor journals Gestational Hypertension Scopus journals Gestational Hypertension PubMed journals Gestational Hypertension medical journals Gestational Hypertension free journals Gestational Hypertension best journals Gestational Hypertension top journals Gestational Hypertension free medical journals Gestational Hypertension famous journals Gestational Hypertension Google Scholar indexed journals intra uterine articles intra uterine Research articles intra uterine review articles intra uterine PubMed articles intra uterine PubMed Central articles intra uterine 2023 articles intra uterine 2024 articles intra uterine Scopus articles intra uterine impact factor journals intra uterine Scopus journals intra uterine PubMed journals intra uterine medical journals intra uterine free journals intra uterine best journals intra uterine top journals intra uterine free medical journals intra uterine famous journals intra uterine Google Scholar indexed journals gestational age articles gestational age Research articles gestational age review articles gestational age PubMed articles gestational age PubMed Central articles gestational age 2023 articles gestational age 2024 articles gestational age Scopus articles gestational age impact factor journals gestational age Scopus journals gestational age PubMed journals gestational age medical journals gestational age free journals gestational age best journals gestational age top journals gestational age free medical journals gestational age famous journals gestational age Google Scholar indexed journals
Article Details
Aim of the work
To evaluate and compare the changes of fetal Doppler indices (MCA, UA and CPR) in singleton pregnancies complicated by gestational hypertension and IUGR from 28 to 34 weeks of gestation after corticosteroid therapy and its impact on fetal and neonatal outcome.
Introduction
Althouh there is a great advance in antenatal care, gestational hypertension still one of the major reasons of maternal and neonatal morbidity and mortality. For this reason , early screening of gestational hypertension and fetal growth retardation can permit cautious antenatal monitoring and proper timing of delivery to steer clear of serious complications [1].
Gestational hypertension is defined as elevated blood pressure (systolic BP>=140 mmhg or diastolic BP>=90 mmhg) after 20 weeks of gestation [2].
Intrauterine growth restriction (IUGR) is known as failure inability of the fetus to gain its expected weight. The most common definition for IUGR is, the estimated fetal weight less than tenth percentile for gestational age which is a common sequel of hypertensive disorders with pregnancy [3].
Corticosteroid therapy is effective in decreasing the incidence of respiratory distress and other unfavorable sequeles of preterm labour as, intraventricular hemorrhage, necrotizing enterocolitis, and intra uterine fetal death [4].
The recommended dose for corticosteroid treatment is ; either 2 doses each of 12 mg betamethasone intramuscular 24-hours apart, or four doses each of 6 mg dexamethasone intramuscular 12-hours apart within 2 days for IUGR at 24 to 34 weeks of gestation with considering labour a week after its administration [5].
Doppler ultrasonography is an easy non invasive method ofdiagnosis which has an important role in IUGR in which it can expect the possible perinatal outcome through its ability to measure vascular blood flow velocity as umbilical artery (UA), middle cerebral artery (MCA), so it could help in planning the time of delivery [6].
Cerebroplacental ratio (CPR) is an earlier predictor of poor outcome than Doppler indices of MCA or UA alone that help in better expectation of fetal distress and low Apgar score [7].
Aim of the work
To asses and compare the changes of fetal Doppler indices (MCA, UA and CPR) in singleton pregnancies complicated by gestational hypertension and IUGR from 28 to 34 weeks of gestation after corticosteroid therapy and its impact on fetal outcome.
Patients and methods
1. Setting
This study was carried out in Obstetrics and Gynecology department (High risk unit) of Sayed Galal hospital of Al-Azhar university.
2. Study design and population
This prospective study included 100 singleton pregnant women with gestational hypertension and complicated with
IUGR fetuses.
The 100 patients were divided into 2 groups (A and B), each group consists of 50 patients:
*Group A:
Will include 50 patients who received corticosteroid therapy in third trimester (from 28 to 34 weeks) to stimulate fetal lung maturity. Fetal Doppler flow indices will be measured before and after therapy.
After termination of pregnancy, effect on fetal outcome to be detected (Apgar score and need for NICU admission).
*Group B (control group):
Will include 50 patients who did not receive corticosteroid therapy. Fetal Doppler flow indices will be measured, and after termination of pregnancy effect on fetal outcome to be detected as well. The results to be compared to group A.
3. Inclusion criteria
*Patients with gestational hypertension (systolic BP>=140 mmhg or diastolic BP>=90 mmhg after 20 weeks of gestation).
*Fetuses confirmed to be IUGR.
*Gestational age from 28 to 34 weeks (based on last menstrual period).
*Singleton pregnancies.
*No fetal anomalies; to be excluded by ultrasonography.
4. Exclusion criteria
*Structural, congenital anomalies, or chromosomal disorders.
*Patients could not complete the study due to Intra-Uterine Fetal Death (IUFD).
*Patients need emergency termination of pregnancy.
*Patients start corticosteroid therapy course before enrolling in the study.
5. Ethical consideration
This study followed the ethical committee rules of Obstetric and Gynecology, Al-Azhar university and ethical committee approval was taken before patient enrollment into the study .
Study procedure was explained to all patients, voluntary participation and confidentially was guaranteed.
6. Procedure
*All patients in group A absolutely underwent fetal Doppler flow indices measurement before corticosteroid administration, and to be repeated within five days after its administration. Its effect on fetal outcome to be detected after termination of pregnancy.
All patients in group A received four doses of corticosteroids (Dexamethasone 6mg each dose) given intramuscularly 12-hours apart within two days.
*Patients in group B underwent fetal Doppler flow indices measurements but without corticosteroid administration, fetal outcome to be detected as well.
Technique of Doppler examination: The ultrasound used in the study was Medison operating at a frequency of 2 to 6 MHz (curvilinear probe) with pulsed and colour Doppler capability.
UMA: Colour Doppler mode is first used to identify a free floating loop of the umbilical cord. With the use of lowest possible wall filter and angle of insonation (<10?) measurements are obtained.
MCA: A transaxial view of the fetal head is obtained; section chosen is a plane that is slightly more caudal to the plane used for BPD measurements, which include the cerebral peduncles. Proximal part of the MCA is chosen to place the Doppler sample volume. The angle of insonation is kept close to zero for this vessel. After obtaining a good waveform Peak systolic velocities are measured. Fetal outcome in form of Apgar score and need for NICU admission following termination of pregnancy. All results obtained from both groups to be compared.
7. Data collection Characteristic data include:
Maternal age, parity, gestational age at time of diagnosis, maternal blood pressure (BP), preeclampsia, maternal diabetes.
Fetal Doppler indices to be obtained from UA, MCA, CPR (MCA-RI/UA-RI).
8. Outcome
Fetal Doppler indices (MCA, UA, CPR).
Fetal outcome.
*Fetal outcome in the form of Apgar score and the need for NICU admission following termination of pregnancy.
*All results obtained from both groups were compared.
Results :
Table 1: Comparison between control group & patient group as regards age, gestational age and weight (at scan)
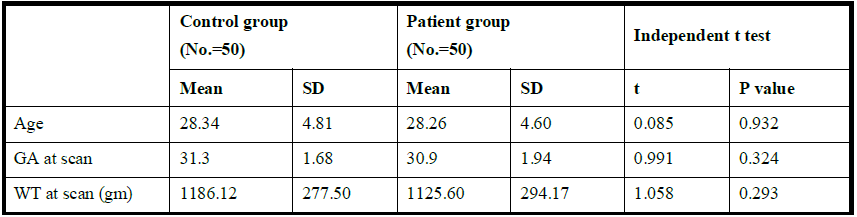
This table shows that there was no statistically significant difference in age, gestational age and weight (at scan) regarding studied group
Table 2: Comparison between patient group & control group as regards blood pressure
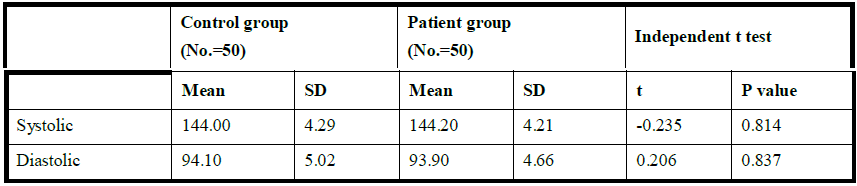
This table shows that there was no statistically significant difference in blood pressure regarding studied group
Table 3: Comparison between control group & patient group as regards MCA (PI and RI), UMA (PI and RI) and CRP (RI) before corticosteroid administration.
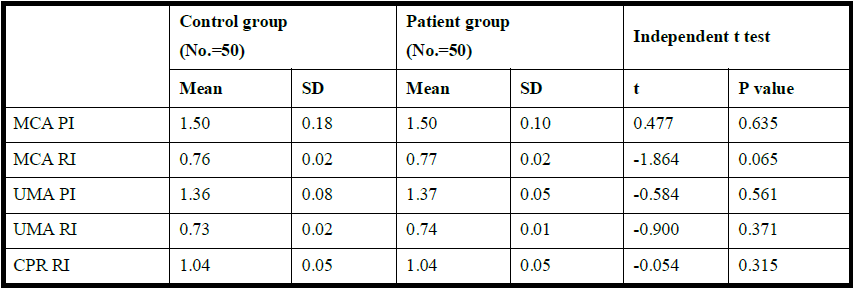
This table shows that there was no statistically significant in MCA, UMA and CRP between the control group and the patient group before corticosteroid administration.
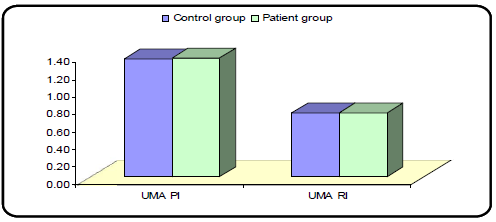
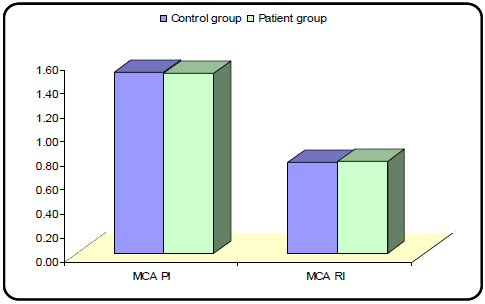
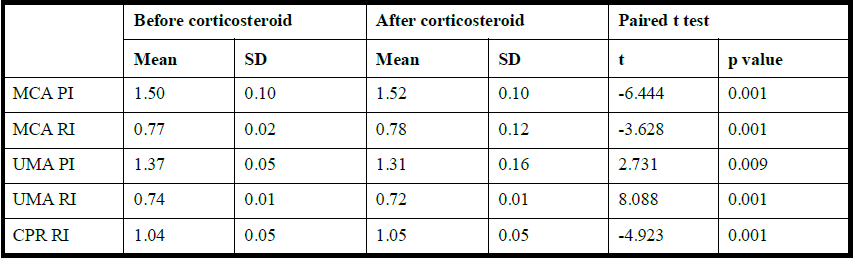
Table 4: Comparison between before and after corticosteroid as regards MCA (PI and RI), UMA (PI and RI) and CRP (RI)
This table shows that there was statistically significant increase in MCA and CPR and statistically significant decrease in UMA in patient group after corticosteroid in comparison to before corticosteroid
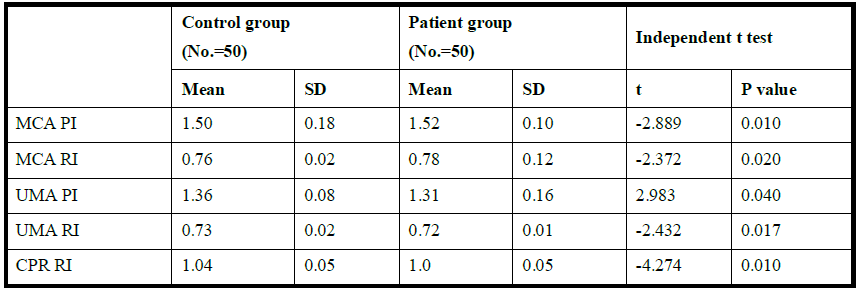
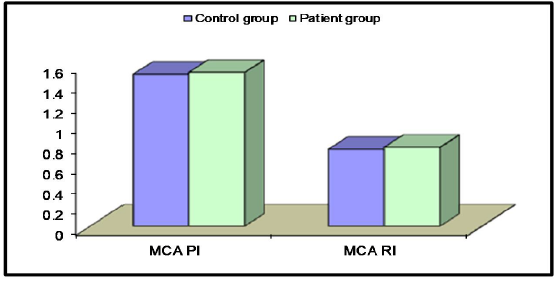
Table 5: Comparison between control group & patient group as regards MCA (PI and RI), UMA (PI and RI) and CRP (RI) after corticosteroid
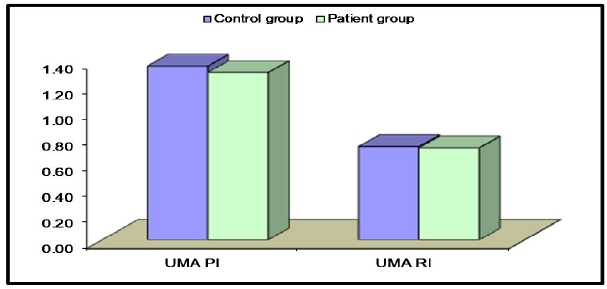
Table 2: Comparison between control group & patient group before corticosteroid administration as regards UMA (AEDFV and REDFV)
This table shows that there was no statistically significant difference in UMA (AEDFV and REDFV) between the control group and the patient group before corticosteroid administration
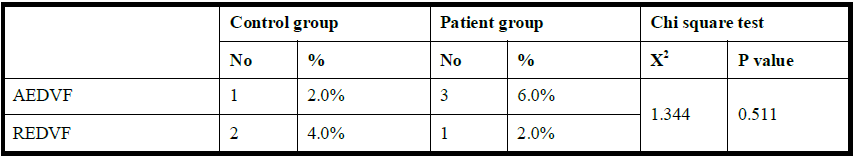
Table 7: Comparison between patient group before & after corticosteroid as regards UMA (AEDFV and REDFV)
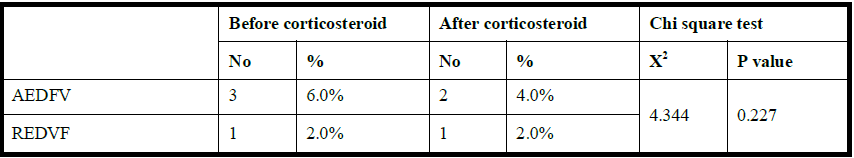
This table shows that there was no statistically significant difference in UMA (AEDFV and REDFV) in patient before and after corticosteroid administration
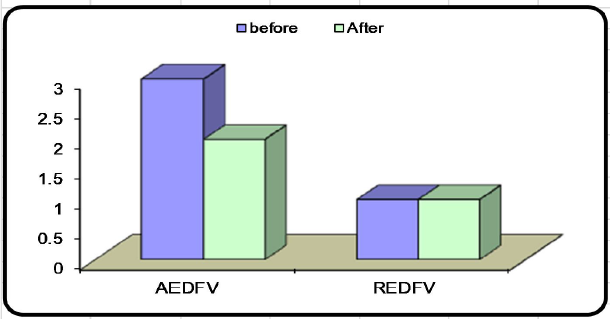
Table 8: Comparison between patient group & control group as regards gestational age and weight (at birth)
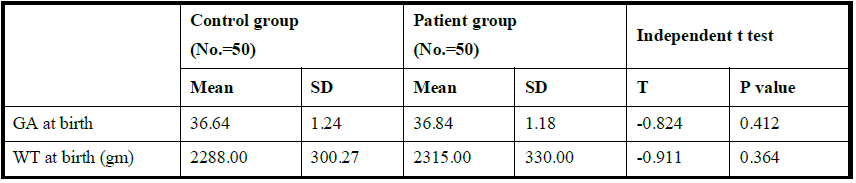
This table shows that there was no statistically significant difference in gestational age and weight (at birth) regarding studied group
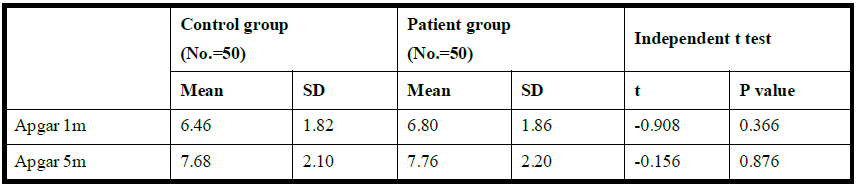
Table 9: Comparison between control group & patient group as regards Apgar score
This table shows that there was no statistically significant difference in Apgar score regarding studied group
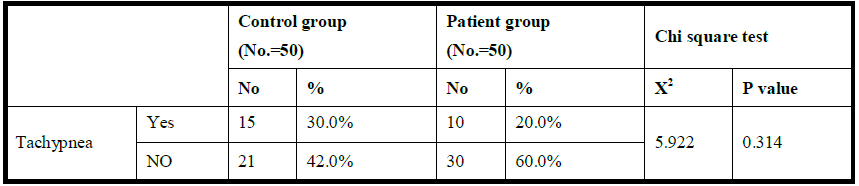
Table 10: Comparison between control group & patient group as regards tachypnea
This table shows that there was no statistically significant difference in tachypnea regarding studied group
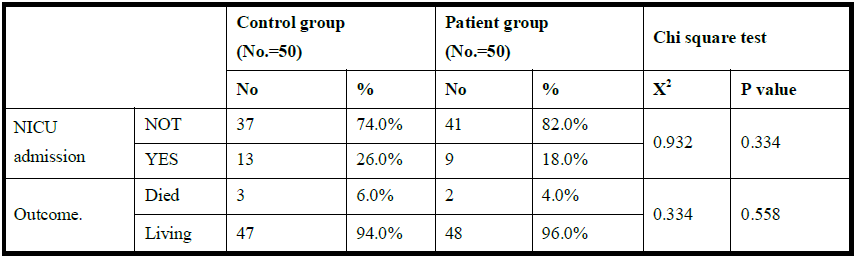
Table 11: Comparison between control group & patient group as regards NICU admission and outcome
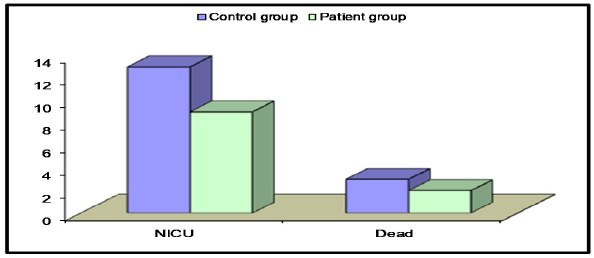
This table shows that there was no statistically significant difference in NICU admission and outcome regarding studied group
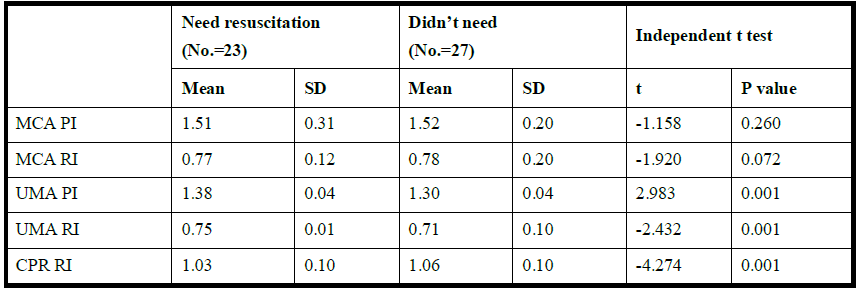
Table 12: Comparison between patient group after corticosteroid administration as regards MCA (PI and RI), UMA (PI and RI) and CRP (RI) in babies need resuscitation (tachypnic and NICU admitted) and babies did not need
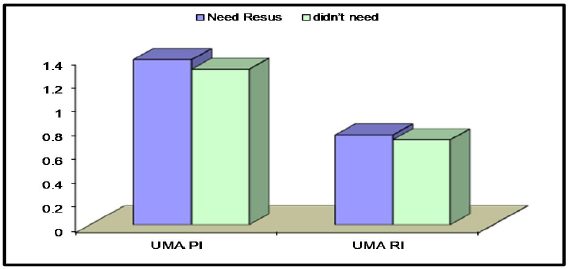
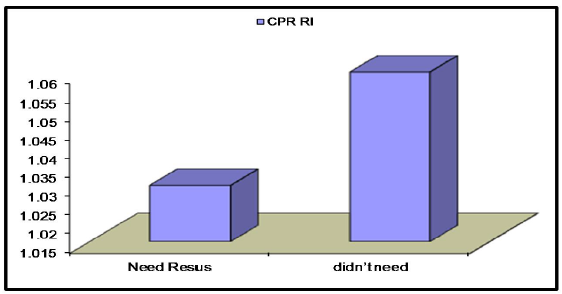
This table shows that there was statistically significant higher CPR and statistically significantly lower UMA (PI and RI) between babies need resuscitation (tachypnic and NICU admitted) and babies didn’t need after corticosteroid administration but there was no statistically significant difference in MCA(PI & RI) in babies didn’t need resuscitation in comparison to babies need.
Discussion
Fetal Doppler (MCA PI/RI and UMA PI/RI) is a valuable diagnostic method in the evaluation of fetuses with growth retardation [8,9].
Increased umbilical artery PI , RI and reduced MCA PI, RI) can be combined in CPR, which is the simple ratio between the MCA PI/RI and the UMA PI/RI. It has been shown that a suboptimal or low CPR is accompanied by short term markers of neonatal outcome such as cord blood acidemia, need for emergency operative delivery and neonatal ICU admission, stillbirth and neonatal morbidity [8, 10].
The current prospective observational study was designed to evaluate and compare fetal Doppler indices in the form of MCA PI/RI , UMA PI/RI and CPR RI before and after corticosteroid administration in a group of pregnant women with gestational hypertension complicated with IUGR at gestational age between 28 to 34 weeks aiming to determine if corticosteroids has any effect on fetal Apgar score or admission to NICU post delivery and was compared to a control group of pregnant women with gestational hypertension complicated with IUGR at gestational
age between 28 to 34 weeks but without corticosteroid administration, the fetal Doppler indices and fetal outcome in this control group is going to be compared to that of the study group to find out if corticosteroids can improve this parameters in this kind of patients.
In the current study, There was no statistically significant difference between the study and control groups regarding mean age of the patients (study group: 28.26 ± 4.6 and control group: 28.34 ± 4.81 years) , mean blood pressure ( study group: systolic 144.2 ± 4.21, diastolic 93.9 ± 4.66 and control group systolic 144 ± 4.29, diastolic 94.1 ± 5.02 mmHg) ,mean gestational age at the time of scan (study group: 30.94 ± 1.94 and control group 31.3 ± 1.68 weeks) and mean weight at the time of scan (study group 1125.6 ± 294.17 and control group 1186.12 ± 277.5 gm (the mean gestational age at time of scan and the mean weight at time of scan.
Also , there was no statistically significant difference between the study group before corticosteroid administration and control group regarding the mean Doppler indices measured in the form of (MCA PI-RI, UMA PI-RI and CPR).
MCA PI : study group 1.5 ± 0.18 and control group 1.5 ± 0.10.
MCA RI: study group 0.77 ± 0.02 and control group 0.76 ± 0.02.
UMA PI: study group 1.37 ± 0.05 and control group 1.36 ± 0.08.
UMA RI: study group 0.73 ± 0.2 and control group 0.74 ± 0.1.
CPR: study group 1.04 ± 0.05 and control group 1.04 ± 0.05.
There was statistically significant difference in the study group before and after corticosteroid administration regarding the mean Doppler indices in the form of (MCA PI-RI, UMA PI-RI and CPR).
MCA PI shows increase from 1.5 ± 0.10 to 1.52 ± 0.10 and RI from 0.77 ± 0.02 to 0.78 ± 0.12.
While UMA PI shows decrease from 1.37 ± 0.05 to 1.31 ± 0.16 and RI from 0.74 ± 0.1 to 0.72 ± 0.1 . CPR also shows increase from 1.04 ± 0.05 to 1.05 ± 0.05.
There was statistically significant difference between the study group after corticosteroid administration and the control group regarding the mean Doppler indices in the form of (MCA PI-RI, UMA PI-RI and CPR).
MCA shows higher values in study group after corticosteroid administration than the control group (PI 1.52
- 10 and 1.5 ± 0.18 and RI from 0.78 ± 0.12 to 0.76 ± 0.02.
While UMA shows lower values in study group after corticosteroid administration than the control group (PI 1.31 ± 0.16 and 1.36 ± 0.08 and RI 0.72 ± 0.01 and 0.73 ± 0.02.
CPR also shows higher values in study group after corticosteroid administration than the control group 1.05
- 05 and 1.04 ± 0.05.
Although corticosteroid shows statistically significant improvement in all Doppler indices but there was no statistically difference regarding the outcome compared to the control group in the form of:
Mean gestational age at birth (study group 36.86 ± 1.18 and control group 36.64 ± 1.24 weeks). Mean weight at birth (study group 2315 ± 300 and the control group 2288 ± 300.27 gm).
Mean Apgar score after 1 min (study group 6.8 ± 1.86 and control group 6.46 ± 1.82) and after 5 min (study group 7.76 ± 2.2 and the control group 7.68 ± 2.1).
Number of fetuses born suffering from tachypnea (study group 10 fetuses which represent 20 % of the study group and control group 15 fetuses which represent 30 % of the control).
Number of fetuses admitted to the NICU (study group 9 fetuses which represent 18 % of the study population and control group 13 fetuses which represent 26 % of the control).
Number of dead fetuses (study group 2 fetuses which represent 4 % of the study group and control group 3 fetuses which represent 6 % of the control).
Number of alive fetuses (study group 48 fetuses which represent 96 % of the study group and control group 47 fetuses which represent 94 % of the control).
In the present study , the study group shows one patient with REDFV which represent 2 % of the study population and its outcome was ominous result in IUFD and three patients with AEDFV which represent 6 % of the study population and their outcome were one fetus its UMA Doppler change from absent to positive diastolic flow wave and the other two shows no improvement and one of them died in NICU, also the control group shows two patients with REDFV which represent 4 % of the control and their outcome were ominous which result in fetal death immediately post delivery and one patient with AEDFV which represent 2 % of the control and its outcome was ominous as well which result in fetal death post delivery in NICU… These results shows that AEDFV and REDFV are critical Doppler signs and in this study the fetal outcome was associated with high adverse fetal outcome and fetal compromise.. There was no statistically significant difference in the outcome between either the control group and study group or the study group before and after corticosteroid administration.
There was statistically significant difference between the babies who were not tachypnic and not admitted to the NICU in comparison to those who were suffering from tachypnea and admitted to NICU regarding UMA and CPR.
Fetuses born not suffering from tachypnea or not admitted to NICU shows statistically significant decrease in UMA PI 1.30 ± 0.04 and 1.38 ± 0.04 and RI 0.71 ± 0.10 and 0.75 ± 0.01 and statistically significant increase in CPR 1.06 ± 0.10 and 1.03 ± 0.10 than those were tachypnic and admitted to NICU..
While MCA shows no statistically significant difference between both groups PI 1.52 ± 0.20 and 1.51 ± 0.31 and RI 0.78 ± 0.20 and 0.77 ± 0.12.
So, finally in the present study , we found that corticosteroid administration in patients suffer from pregnancy induced hypertension and IUGR produces significant improvement in all Doppler indices in the form of increased MCA PI & RI and CPR values and decreased UMA PI & RI values. However, this significant improvement wasn’t associated with significant decrease in fetuses born suffering from tachypnea or admitted to NICU in comparison with the control group. Also, found that fetuses born not suffering from tachypnea or not admitted to the NICU shows significant increase in CPR value and significant decrease in UMA PI& RI values. Also, AEDFV and
REDFV signs of UMA Doppler are critical signs, usually associated with high adverse fetal outcome or fetal compromise.
This study agrees with a study made by Jain & Bindal, 2018 regarding the increase in MCA PI & RI and decrease in UMA PI & RI post corticosteroid administration in IUGRcomplicated pregnancies and also agrees with it regarding improvement of UMA PI in fetuses who born didn’t need resuscitation than those who need [11].
Also the present study agrees with a previous research made by ElSonsy et al., 2017, regarding improvement of all Doppler indices of (MCA PI & RI and UMA PI & RI) after dexamethasone injection in pregnancies with great possibility of preterm labor [12].
Moreover, the current study agrees with Shojaei & Mohammadi et al, 2015. regarding significant decrease in UMA PI& RI and significant increase in MCA RI and MCA-UMA-RI in IUGR fetuses with and without preeclampsia after giving betamethasone injection [2].
On contrary , the present study disagrees with a previous study made by Thuring et al., 2011 regarding UMA-RI, MCA-PI& RI that revealed no significant changes but in our study shows significant difference after corticosteroid administration and also disagree with it regarding significant changes in UMA waveform from REDFV to AEDFV, and from AEDFV to positive diastolic flow but in our study it shows no significant changes [13].
Also, the present study agrees with Kuber et al., 2016 regarding the ominous results of AEDFV and REDFV and the adverse perinatal outcome associated with high values of UMA and low values of MCA and CPR without corticosteroid administration (as control group of the current study ) [14].
A previous study made by Jain & Bindal 2018 which, they revealed that there was a statistically significant difference between all Doppler indices in UMA, MCA and DV before and 24 hours after maternal betamethasone administration. No significant effect on maternal UA was observed. Neonates of women who showed an improvement in UMA PI had significantly lesser requirement of assisted resuscitative measures, better Apgar at 1, 5, and 10 min and required lesser admissions to NICU compared to neonates of women who did not show any decrease in UMA PI [11].
ElSonsy et al., 2017 made a research that showed that Doppler studies were performed on the UMA, MCA and maternal UA just before dexamethasone administration and repeated 24 h after completion of the dexamethasone course. It shows that there were statistically significant improvement between all Doppler indices in UMA and fetal MCA 24 hours after maternal dexamethasone administration in comparison to Doppler indices before corticosteroid administration [12].
Kuber et al., 2016. A prospective study included 50 women with biometrically suspected singleton IUGR pregnancy to evaluate Uteroplacental and Fetoplacental circulation (UA, UMA, MCA) in using color Doppler Sonography. They revealed that 14 cases showed AEDFV and 4 patients showed REDFV.: 22 patients showed elevated UMA PI. Adverse perinatal outcome was observed in all patients with AEDFV and REDFV . Out of the 22 with elevated UMA PI, 15 showed adverse outcome. 36 cases showed low MCA PI and 6 showed a pseudo normalization. A cerebroplacental ratio of < 1.08 was observed in 16 patients, it was calculated in only those pregnancies that showed forward diastolic flow in umbilical artery (n= 22). 15 of them showed adverse perinatal outcome] 14].
Conclusion
Corticosteroid administration to hypertensive women is associated with improvement of all Doppler indices in the form of elevation of MCA PI & RI and CPR value and decrease of UMA PI & RI values.
Although corticosteroid administration was associated with all these Doppler indices enhancement but there was no associated improvement in the number of fetuses born suffering from tachypnea or admitted to NICU when compared to the other group of women who did not receive corticosteroids .
Fetuses who was delivered not affected by tachypnea or not admitted to the NICU shows improvement in UMA PI & RI and CPR in comparison to those who were tachypnic and admitted to the NICU.
AEDFV and REDFV signs of UMA are critical signs, usually associated with adverse fetal outcome or fetal compromise.
Further evaluation of corticosteroid effect on fetal Doppler indices and fetal outcome in patients with pregnancy induced hypertension and IUGR are required in form of repeated Doppler indices measurements including ductus venosus Doppler (DV) and maternal UA until time of delivery.
Disclosure statement
No potential conflict of interest was reported by the authors.
Author Contributions
The team of authors participated in this study in its aspects with:
- Substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work.
- Drafting the work or revising it critically for important intellectual content.
- Final approval of the version to be published.
- Agreement to be accountable for all aspects of the work in that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
References
- Nagar T, Sharma D, Choudhary M, Khoiwal S, Nagar RP and Pandita A. The role of uterine and umbilical artery Doppler in high-risk pregnancy: A prospective observational study from india. Clinical Medicine Insights: Reproductive Health 9 (2015): CMRH-S24048.
- Shojaei K, Mohammadi N. Comparing the Effects of Antenatal Betamethasone on Doppler Velocimetry Between Intrauterine Growth Restriction With and Without Preeclampsia. Global Journal of Health Science 7 (2015): 344.
- Callen PW. Ultrasonography in obstetrics and gynecology (5th ed.). Philadelphia, Saunders Elsevier.
- Crowther CA, and Harding JE. Repeat doses of prenatal corticosteroids for women at risk for preterm birth for preventing neonatal respiratory distress. Cochrane Database Syst Rev 3 (2007): CD003935.
- NICE Guidelines. hypertension in pregnancy: the management of hypertensive disorders during pregnancy. 2010.
- Siddiqui TS, Asim A. Shafqut A, Siddiqui TS and Tariq A. Comparison of perinatal outcome in growth restricted fetuses retaining normal umbilical artery Doppler flow to those with diminshed end-diastolic flow. J Ayub Med Coll Abbottabad 26 (2014): 221-224.
- DeVore GR. The importance of the cerebroplacental ratio in the evaluation of fetal well-being in SGA and AGA fetuses. Am J Obstet Gynecol 213 (2015): 5–15.
- Khalil A, Morales-Rosello J, Townsend R, et al. Are fetal cerebroplacental ratio and impaired placental perfusion recorde in the third trimester predictors of stillbirth and perinatal loss? Ultrasound Obstet Gynecol 47 (2016): 74-80.
- Figueras F, Gratacos E. Stage-based approach to the management of fetal growth restriction. Prenat Diagn 34 (2014): 655-659.
- Prior T, Mullins E, Bennett P, et al. Prediction of intrapartum fetal compromise using the cerebroumbilical ratio: a pro-spective observational study. Am J Obstet Gynecol 208 (2013): 124.e1-124.e6.
- Jain R & Bindal J. Effect of Antenatal Betamethasone on Fetal and Uteroplacental Blood Flow Velocity Waveforms in Preterm Pregnancies with Intra Uterine Growth Restriction. JMSCR, June 6 (2018): 265-272.
- ElSonsy E, Shaaban O M, Abbas A M, Gaber H H. Effects of antenatal dexamethasone administration on fetal and uteroplacental Doppler waveforms in women at risk for spontaneous preterm birth. Middle East Fertility Society J 22 (2017): 13–17.
- Thuring A, Malcus P, Marsal K. Effect of maternal betamethasone on fetal and uteroplacental blood flow velocity waveforms. J Ultrasound Obstet Gynecol 37 (2011): 668- 672.
- Kuber R, Rahnhawa S, Khaladkar S, Patil AM. Doppler study of middle cerebral artery and umbilical artery in biometrically suspected intra uterine growth restricted pregnancies. Int J Res Med Sci 4 (2016): 403-414.
