The Effect of the Number of Eating Out on Metabolic Syndrome and the Moderating Effect of Health Behavior in Korean
Article Information
SunA LEE1*
1Graduate School of Public Health, Inje University, Busan, South Korea, Nurse, Inje University Busan Paik Hospital
*Corresponding Author: SunA LEE. Busan Paik Hospital, Inje University, 75, Bokji-ro, Busanjin-gu, Busan 47392, Republic of Korea.
Received: 19 August 2023; Accepted: 26 August 2023; Published: 11 September 2023.
Citation:
SunA LEE. The Effect of the Number of Eating Out on Metabolic Syndrome and the Moderating Effect of Health Behavior in Korean. Journal of Environmental Science and Public Health. 7 (2023): 140-153.
View / Download Pdf Share at FacebookAbstract
Objectives: This study was conducted to prepare fundamental data and prevention measure of metabolic syndrome, and assess the effect of the number of Korean eating out on metabolic syndrome and the moderating effect of health behavior among Korean adults.
Methods: Study subjects were number of 5,206 people with biochemical indicators and basic variables, meal variables, and health behavior variables among the people who participated in the 8th National Health and Nutrition Survey (2019). The collected data were analysed by one-way ANOVA, regression analysis, and Hayes' Process Macro model 1 analysis using IBM SPSS(ver. 26.0) statistical package program.
Results: There were significant correlations between the number of eating out, metabolic syndrome, and health behavior. There was positive (+) effect of eating out on metabolic syndrome. There was significant moderating effect of stress recognition rate in the relationship between the number of eating out and metabolic syndrome.
Conclusion: As above results, the author consider that it should be reducing the number of eating out to reduce metabolic syndrome, and health behavior management is also necessary, especially stress management. This study will be fundamental data of future study on metabolic syndrome and health improvement among adults.
Keywords
Number of eating out, Metabolic syndrome, Health behavior
Number of eating out articles; Metabolic syndrome articles; Health behavior articles
Article Details
1. Introduction
Metabolic syndrome refers to a condition in which one of abdominal obesity, high blood sugar, high blood pressure, high triglycerideemia, and low HDL-cholesterolemia has three or more [1]. According to the death ranking for 10 years from 2008to 2018, released by the National Statistical Office in 2019, it is followed by malignant neoplasm (cancer), cerebrovascular disease, heart disease, and diabetes respectively [2]. In addition, it is reported that people with more than three metabolic syndrome risk factors are more than twice as likely to develop cardiovascular disease, diabetes, and increase the risk of various cancers such as breast cancer and colon cancer [3]. According to industrial accident statistics released by the Ministry of Employment and Labor in 2014, heart disease deaths ranked second in all deaths in Korea, and 318 out of 351 deaths from occupational diseases were cerebral cardiovascular disease [4,5]. Metabolic syndrome is used as an indicator for evaluating these cardiovascular diseases. Therefore, the management of metabolic syndrome is an urgent and important problem as it can reduce the mortality rate and the prevalence rate of occupational diseases in Korea as a whole.
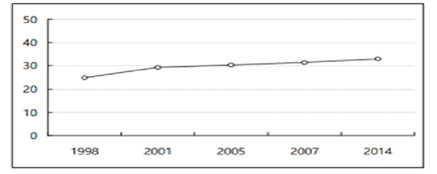
Every year, about 41 million people (71 percent of the world's mortality rate) dies from non-communicable disease (NCD) and the death toll of people aged 30-69 is increasing by 15million worldwide each year [6]. Metabolic syndrome is closely related to the early mortality rate from these non-infectious diseases (NCDs). The prevalence of metabolic syndrome is on the rise worldwide, and the prevalence of metabolic syndrome among Koreans is also continuously increasing from 24.9% in 1998 to 29.2% in 2001, 30.4% in 2005, 31.3% in 2007, and 33.0% in 2014 [7].
Metabolic syndrome is a disease caused by complex factors, and although no clear mechanism has been reported yet, dietary habits, including dietary factors, are analyzed to be an important factor [8]. Health behaviors related to metabolic syndrome include drinking, smoking, and stress recognition. According to the study [9], drinking has a significant effect on increasing HDL cholesterol. It has been studied that smoking increases insulin resistance and blood sugar and increases triglycerides [10]. Studies have reported that smoking and drinking increase the risk of cardiovascular disease caused by metabolic syndrome [11], In addition, it was said that the risk rate of metabolic syndrome of smokers is higher than that of non-smokers [12]. People with high stress awareness had a 2.39 times higher risk of metabolic syndrome prevalence than people with low stress recognition [13]. As such, health risk behaviors such as smoking, excessive drinking, lack of exercise, and excessive stress affect chronic disease prevalence and resulting death [14], and health behavior is also closely related to quality of life. Several studies have reported that metabolic syndrome is more affected by multiple lifestyles such as smoking, drinking, stress, and relaxation than genetic factors [15]. Therefore, it is important to establish strategies and management measures to improve risk health behaviors that increase metabolic syndrome.
The number of patients with metabolic syndrome is expected to increase steadily in the future due to changes in the social and economic environment, obesity, eating habits, and lifestyle changes. So, it is urgent to prevent and manage the metabolic syndrome. Most existing studies related to metabolic syndrome tend to grasp the connection between the relationship between metabolic syndrome and influencing factors such as demographic and sociological characteristics, health behavior, and diet. On the other hand, it is difficult to find previous studies on the effect of the increasing number of eating out on metabolic syndrome and the moderating effect of health behavior due to the westernization of eating habits and the development of eating out culture in modern society.
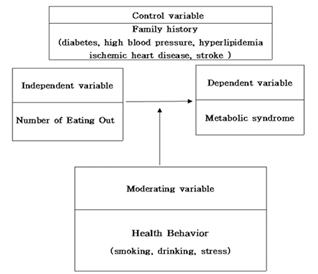
Therefore, this study was conducted to expand these existing studies to select the number of eating out as an independent variable and to verify the moderating effect of health behavior (smoking, drinking, and stress recognition rate) through family history. Our study findings will also help prepare effective metabolic syndrome management programs and to provide policy implications <Figure 1>.
2. Materials and Methods
2.1 Setting and Data collection
The purpose of this study is to examine the effect of the number of times Koreans eat out on metabolic syndrome, and to examine the moderating effect of health behavior after controlling their family history in this process. <Figure 2> is shown below when the model of the empirical study to be tested in this study is schematized.
Korea Health Statistics 2019: Korea National Health and Nutrition Examination Survey (KNHANES
It was implemented after obtaining approval for exemption from deliberation by the Life Research Ethics Review Committee of Inje University Busan Paik Hospital. Exemption from deliberation Content: This study is based on the 8th National Health Survey website (https:/knhanes.kdca.go.kr) [16] We confirm that it is an exemption from deliberation because we obtain approval for the use of raw data from both surveys and use information from which identification information of the study subjects has been removed through research .
(IRB File NO:2022-06-037). All data generated or analysed during this study are included in this published article [and its supplementary information files].
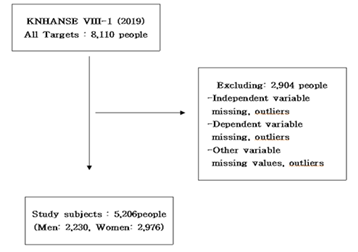
The National Health and Nutrition Survey is a legal survey on people's health behavior, chronic disease prevalence, food and nutrition, conducted under Article 16 of the National Health Promotion Act, and is a government-designated statistic based on Article 17 of the Statistics Act (Approval No. 117002). In the 8th, 1st (2019), the subjects of the survey were 10.859, and the participants were 8.110. This study finally conducted an analysis of 5,206 people (2,230 men and 2,976 women) excluding the outliers and missing values of the variables selected among the participating subjects <Figure 3>.
2.2 Measures
- metabolic syndrome
Metabolic syndrome was defined as a case that satisfies more than three of the following five items.
≥ 3 Risk factors
- Abdominal obesity only
Waist circumference ≥ 90cm (male), ≥ 85 cm (female)
- Triglycerides;≥150mg/dL
- High density cholesterol < 40 mg/dL (male), < 50 mg/dL (female)
- High blood pressure
Blood pressure ≥130/85mmHg or antihypertensive
- fasting blood glucose ≥ 110 mg/dL (including diabetes)
Measurement method: The number of metabolic syndrome factor branches (0-5 points) for each individual is calculated.
- Number of eating out
Among the questions of the National Health and Nutrition Survey, the number of dining out was used, and on average, it means how often you ate out other than home-cooked food (including delivery food, packaged food, meals, and food provided by religious organizations) over the past year.
Measurement method: Almost never (less than once a month) (0 point), 1 to 3 times a month (1 point), 1 to 2 times a week (3 point), 3 to 4 times a week (3 point), 5 to 6 times a week (4 point), 1 to 5 times a day (5 point), and 2 or more times a day (6 point).
3. Health behavior
In this study, health behavior refers to smoking, drinking, and stress recognition rates.
Measurement method:
① Smoking: Never smoked (0 point), Less than 5 packs(100 pieces) (1 point), More than 5 packs(100 pieces) (2 point)
② Drinking: In the past year, it was classified as Do not drink for a year (0 point), Less than once a month (1 point), About once a month (2 point), 2~4 times a month(3 point),
2~3 times a week (4 point), More than 4 times a week (5 point)
③ Stress perception rate: It was subdivided into Very much felt (0 point), a lot felt(1 point)(1 point), a little bit felt(2 point), Hardly felt (3 point)
In this study, each variable is defined and measured as shown in <Table 1>
Table 1: Operational definition of study variables
|
Variables |
Operational definition |
||
|
Dependent Variable |
Metabolic syndrome |
Waist circumference: |
|
|
≥ 90cm(men), ≥ 85cm(women) |
|||
|
Triglycerides;≥150mg/dL |
|||
|
HDL-C:< 40mg/dL(men), |
|||
|
< 50mg/dL(women) |
|||
|
Blood pressure:≥130/85mmHg or |
|||
|
hypertension Rx |
|||
|
Glucose :≥100mg/dL |
|||
|
(includes diabetes) |
|||
|
->Calculate the number of factors (0-5 points) for each individual |
|||
|
->More than any 3 of the following |
|||
|
5 factors |
|||
|
Independent variable |
Number of eating out |
Hardly (less than once a month)(0 point) |
|
|
1~3 times per month (1 point) |
|||
|
1~2 times a week (2 point) |
|||
|
3~4 times a week (3 point) |
|||
|
5~6 times a week (4 point) |
|||
|
Once a day (5 point) |
|||
|
More than twice a day (6 point) |
|||
|
Moderating variable |
Health behavior |
smoking |
Never smoked (0 point) |
|
Less than 5 packs(100 pieces) (1 point) |
|||
|
More than 5 packs(100 pieces) (2 point) |
|||
|
drinking |
Do not drink for a year (0 point) |
||
|
Less than once a month (1 point) |
|||
|
About once a month (2 point) |
|||
|
2~4 times a month(3 point) |
|||
|
2~3 times a week (4 point) |
|||
|
More than 4 times a week (5 point) |
|||
|
Stress |
Very much felt (0 point) |
||
|
Recog- |
a lot felt(1 point)(1 point) |
||
|
nition |
a little bit felt(2 point) |
||
|
rate |
Hardly felt (3 point) |
||
|
Control |
family |
high blood pressure |
One of parent diagnosed by a doctor -> Yes/No |
|
hyperlipidemia |
Yes/No |
||
|
ischemic heart disease |
Yes/No |
||
|
stroke |
Yes/No |
||
|
diabetes |
Yes/No |
||
2.3 Data analysis
The data of this study used SPSS 26.0 and SPSS Process Macro model 1. Frequency analysis and descriptive statistics analysis were conducted to analyze the general characteristics, percentage, frequency, and standard deviation of the subjects. An independent sample t-test and a one-way distribution analysis were conducted to analyze the variations by socio-demographic characteristics of the study subjects. Pearson's Correlation was performed to determine the degree of correlation between each variable coefficient. Multiple regression analysis was conducted to analyze the effect of the independent variable on the dependent variable. For the moderating effect test, the significance was verified with SPSS Process MacroModel 1 bootstrapping proposed by Preacher, Rucker, and Hayes (2013). Ethical consideration was taken from the Life Research Ethics Review Committee of Inje University Busan Paik Hospital, South Korea.
3. Results
3.1 Sociodemographic Characteristics of Study Subjects
<Table 2> shows the results of frequency analysis to identify the socio-demographic characteristics of the study subjects. In terms of gender, more than half of the participants were women (57.2%) as compared to men (42.8%). 19.1% of the participants were in their 70s or older followed by 968 (18.6%) in their 50s. Most of the participants were married (83.8%). The highest academic background of the respondents was high schools (26.5%), followed by four-year universities (25.2%). In the family history of participants, 36.2% has hypertension, hyperlipidemia (6.3%), ischemic heart disease (5.6%), strokes (11%) and diabetes (18.4%).
Table 2: Sociodemographic Characteristics of Study Subjects
|
Variable |
Categories |
Frequency (n) |
Percentage (%) |
|
|
Gender |
Men |
2230 |
42.8 |
|
|
Women |
2976 |
57.2 |
||
|
Age |
under 30s |
590 |
11.3 |
|
|
30s |
749 |
14.4 |
||
|
40s |
951 |
18.3 |
||
|
50s |
968 |
18.6 |
||
|
60s |
955 |
18.3 |
||
|
over 70s |
993 |
19.1 |
||
|
Number of families |
1 |
688 |
13.2 |
|
|
2 |
1723 |
33.1 |
||
|
3 |
1279 |
24.6 |
||
|
over 4 |
1516 |
29.1 |
||
|
Marital status |
Married |
4361 |
83.8 |
|
|
Unmarried |
845 |
16.2 |
||
|
Education level |
Elementary school |
666 |
12.8 |
|
|
Middle school |
498 |
9.6 |
||
|
High school |
1381 |
26.5 |
||
|
2/3year university |
710 |
13.6 |
||
|
4year university |
1313 |
25.2 |
||
|
Guitar |
638 |
12.3 |
||
|
Family History |
High Blood |
NO |
3321 |
63.8 |
|
pressure |
YES |
1885 |
36.2 |
|
|
Hyperlipidemia |
NO |
4877 |
93.7 |
|
|
YES |
329 |
6.3 |
||
|
Ischemic heart |
NO |
4914 |
94.4 |
|
|
disease |
YES |
292 |
5.6 |
|
|
Stroke |
NO |
4634 |
89 |
|
|
YES |
572 |
11 |
||
|
Diabetes |
NO |
4247 |
81.6 |
|
|
YES |
959 |
18.4 |
||
|
Total |
5206 |
100 |
||
- Variations of Metabolic Syndrome by Sociodemographic Characteristics
A result of the independent sample t-test analysis for metabolic syndrome showed statistically significant differences in gender, marital status, and family history (high blood pressure, hyperlipidemia, ischemic heart disease, stroke, diabetes). Gender was higher for men than for women, marital status was higher for unmarried people than for married people, and in the family history, hypertension, hyperlipidemia, ischemic heart disease, stroke, and diabetes "NO" were higher than"YES". As a result of conducting a one-way distribution analysis (ANOVA), metabolic syndrome showed statistically significant differences in age, the number of families, and degree of education.
As a result of Duncan'spost-analysis, metabolic syndrome was the highest among those in their 30s ofage, followed by those in their 70s and older, 60s, and 50s, and those in their40s and 30s. The number of families was high in the order of four or more, three, two, and one, and the degree of education was the highest, followed by middle school, elementary school, high school, two-thirds-year university, and four-year university <Table 3>.
Table 3: Metabolic syndrome variations according to sociodemographic characteristics
|
Metabolic syndrome |
|||||
|
Variable |
M±SD |
t/F |
p |
||
|
Gender |
Men |
2.84±2.310 |
4.629 |
<.001 |
|
|
Women |
2.61±2.277 |
||||
|
Age |
under 30s |
4.32±2.556e |
455.469 |
<.001 |
|
|
30s |
1.56±1.942a |
||||
|
40s |
1.64±1.782a |
||||
|
50s |
1.99±1.768b |
||||
|
60s |
2.39±1.692c |
||||
|
over 70s |
2.70±1.705d |
||||
|
Number of |
1 |
2.06±1.709a |
116.731 |
<.001 |
|
|
families |
2 |
2.27±1.874b |
|||
|
3 |
2.61±2.319c |
||||
|
over 4 |
3.27±2.550d |
||||
|
Marital status |
Married |
2.08±1.820 |
-38.527 |
<.001 |
|
|
Unmarried |
4.00±2.604 |
||||
|
Education Level |
Elementary school |
2.83±1.752d |
717.591 |
<.001 |
|
|
Middle school |
3.23±2.112e |
||||
|
High school |
2.20±1.967c |
||||
|
2/3year university |
1.37±1.568b |
||||
|
4year university |
1.21±1.531a |
||||
|
Guitar |
4.54±2.196f |
||||
|
Family History |
High Blood pressure |
NO |
3.05±2.393 |
23.433 |
<.001 |
|
YES |
1.91±1.804 |
||||
|
Hyper- lipidemia |
NO |
2.76±2.301 |
7.478 |
<.01 |
|
|
lipidemia |
YES |
1.99±2.072 |
|||
|
Ischemic |
NO |
2.76±2.311 |
11.378 |
<.001 |
|
|
YES |
1.73±1.625 |
||||
|
Stroke |
NO |
2.78±2.338 |
11.129 |
<.001 |
|
|
YES |
2.03±1.598 |
||||
|
Diabetes |
NO |
2.85±2.342 |
15.481 |
<.001 |
|
|
YES |
1.94±1.821 |
||||
|
Post-hoc analysis : a<b<c<d<e<f |
|||||
- Correlation between study variables
Pearson's correlation analysis was conducted to confirm the correlation between the number of eating out, metabolic syndrome, and health behavior, which are the main variables of this study, and the analysis results are as shown in <Table 4>.
As a result, the number of times to eat out (r=.096, p<.01) was positively correlated with metabolic syndrome, and stress recognition rate (r=-.361, p<.01) and smoking (r=-.253, p<.01) and drinking (r=-.091, p<.01) had a negative correlation <Table 4>.
Table 4: Correlation between study variales
|
Metabolic syndrome |
Number of eating out |
Health behaviors |
||||
|
Smoking |
Drinking |
Stress recognition rate |
||||
|
Metabolic syndrome |
1 |
|||||
|
Number of eating out |
.096** |
1 |
||||
|
Health |
Smoking |
-.253** |
.062** |
1 |
||
|
behavior |
Drinking |
-.091** |
.077** |
.284** |
1 |
|
|
Stress |
-.361** |
.006** |
.179** |
.029** |
1 |
|
|
recognition rate |
||||||
**p<01
- Effects of the Number of Eating Out on Metabolic Syndrome
Multiple linear regression analysis was performed to verify the effect of the number of eating out on metabolic syndrome, and demographic characteristics were controlled. As a result, the regression model was statistically significant (F=286.370, p<).001), the explanatory power of the regression model was about 42.5% (adjR2=.425).
On the other hand, the Durbin-Watson statistic was 1.857, which was close to 2, and was evaluated as having no problem with the assumption of the independence of the residuals.
As a result of verifying the significance of the regression coefficient, the number of times to eat out had a significant positive (+) effect on metabolic syndrome (β=.036, p<.001). In other words, it was evaluated that the higher the number of eating out, the higher the metabolic syndrome <Table 5>.
Table 5: The Effect of the Number of Eating Out on Metabolic Syndrome
|
Variable (reference value) |
B |
S.E. |
β |
t |
p |
|
Constant variable |
4.655 |
1.26 |
37.054 |
<.001 |
|
|
Gender(Women=0) |
|||||
|
Men |
0.11 |
0.04 |
0.024 |
2.739 |
<.001 |
|
Age(over 70s=0) |
|||||
|
under 30s |
0.618 |
0.119 |
0.122 |
5.201 |
<.001 |
|
30s |
-0.475 |
0.094 |
-0.068 |
-5.033 |
<.001 |
|
40s |
-0.461 |
0.089 |
-0.071 |
-5.159 |
<.001 |
|
50s |
-0.23 |
0.082 |
-0.036 |
-2.82 |
0.005 |
|
60s |
-0.066 |
0.074 |
-0.01 |
-0.891 |
0.373 |
|
Number of families (over 4=0) |
|||||
|
1 |
-0.845 |
0.076 |
-0.112 |
-11.098 |
<.001 |
|
2 |
-0.487 |
0.057 |
-0.094 |
-8.561 |
<.001 |
|
3 |
-0.21 |
0.051 |
-0.04 |
-4.102 |
<.001 |
|
Marital status(Unmarried=0) |
|||||
|
Married |
-0.687 |
0.087 |
-0.141 |
-7.914 |
<.001 |
|
Education(Guitar=0) |
|||||
|
Elementary school |
-0.814 |
0.079 |
-0.107 |
-10.339 |
<.001 |
|
Middle school |
-0.833 |
0.074 |
-0.108 |
-11.222 |
<.001 |
|
High school |
-1.668 |
0.059 |
-0.305 |
-28.375 |
<.001 |
|
2/3year university |
-2.509 |
0.074 |
-0.337 |
-33.715 |
<.001 |
|
4year university |
-2.756 |
0.062 |
-0.476 |
-44.45 |
<.001 |
|
Family History |
|||||
|
High Blood pressure(NO=0) |
|||||
|
YES |
-0.257 |
0.047 |
-0.051 |
-5.461 |
<.001 |
|
Hyperlipidemia(NO=0) |
|||||
|
YES |
0.028 |
0.089 |
0.003 |
0.317 |
0.751 |
|
Ischemic heart disease(NO=0) |
|||||
|
YES |
-0.048 |
0.097 |
-0.004 |
-0.489 |
0.625 |
|
Stroke(NO=0) |
|||||
|
YES |
0.015 |
0.073 |
0.002 |
0.201 |
0.841 |
|
Diabetes(NO=0) |
|||||
|
YES |
0.099 |
0.058 |
0.015 |
1.715 |
0.086 |
|
Number of eating out |
0.041 |
0.011 |
0.036 |
3.734 |
<.001 |
|
F=286.370(p<.001), R2=.426, adjR2=.425, D-W=1.857 |
|||||
- The moderating effect of smoking on the effect of eating out on metabolic syndrome
Looking at the moderating effect of smoking, it was found that the interaction effect between the number of eating out and smoking did not have a statistically significant effect on metabolic syndrome(B=-.0154, p>.05). In other words, it was evaluated that smoking had no effect on the relationship in which metabolic syndrome increased as the number of eating out increased <Table 6>.
Table 6: Moderating Effect of Smoking
|
B |
SE |
t |
p |
95% Confidence interval |
||
|
LLCI |
ULCI |
|||||
|
(Constant variable) |
4.5586 |
0.128 |
35.6088 |
<0.01 |
4.3076 |
4.8095 |
|
Gender(Women=0) |
||||||
|
Men |
0.347 |
0.0473 |
7.332 |
<0.01 |
0.2542 |
0.4398 |
|
Age(over 70s=0) |
||||||
|
under 30s |
0.5309 |
0.1184 |
4.4827 |
<0.01 |
0.2988 |
0.7631 |
|
30s |
-0.4746 |
0.094 |
-5.0513 |
<0.01 |
-0.6588 |
-0.2904 |
|
40s |
-0.4453 |
0.0889 |
-5.0119 |
<0.01 |
-0.6195 |
-0.2712 |
|
50s |
-0.2363 |
0.0812 |
-2.9115 |
<0.1 |
-0.3954 |
-0.0772 |
|
60s |
-0.0579 |
0.0732 |
-0.7906 |
-0.2014 |
0.0856 |
|
|
Number of families(over 4=0) |
||||||
|
1 |
-0.7631 |
0.0762 |
-10.0105 |
<0.01 |
-0.9125 |
-0.6137 |
|
2 |
-0.4505 |
0.0567 |
-7.9417 |
<0.01 |
-0.5618 |
-0.3393 |
|
3 |
-0.1969 |
0.0511 |
-3.8565 |
<0.01 |
-0.297 |
-0.0968 |
|
Marital status(Unmarried=0) |
||||||
|
Married |
-0.6517 |
0.0865 |
-7.5368 |
<0.01 |
-0.8212 |
-0.4822 |
|
Education(Guitar=0) |
||||||
|
Elementary school |
-0.7742 |
0.0784 |
-9.8724 |
<0.01 |
-0.9279 |
-0.6205 |
|
Middle school |
-0.7784 |
0.074 |
-10.5131 |
<0.01 |
-0.9235 |
-0.6332 |
|
High school |
-0.1579 |
0.0593 |
-26.4882 |
<0.01 |
-1.6882 |
-1.4555 |
|
2/3year university |
-2.3981 |
0.0749 |
-32.0168 |
<0.01 |
-2.5449 |
-2.2512 |
|
4year university |
-2.6601 |
0.0625 |
-42.569 |
<0.01 |
-2.7826 |
-2.5379 |
|
Family History |
||||||
|
High Blood pressure(NO=0) |
||||||
|
YES |
-0.2482 |
0.0468 |
-5.3048 |
<0.01 |
-0.3399 |
-0.1565 |
|
Hyperlipidemia(NO=0) |
||||||
|
YES |
0.0105 |
0.088 |
0.1198 |
-0.162 |
0.1831 |
|
|
Ischemic heart disease(NO=0) |
||||||
|
YES |
-0.0304 |
0.0969 |
-0.3143 |
-0.2203 |
0.1594 |
|
|
Stroke(NO=0) |
||||||
|
YES |
0.0181 |
0.0728 |
0.2493 |
-0.1245 |
0.1608 |
|
|
Diabetes(NO=0) |
||||||
|
YES |
0.1191 |
0.0576 |
2.0666 |
<0.5 |
0.0061 |
0.2321 |
|
Number of eating out |
0.0552 |
0.0131 |
4.2325 |
<0.01 |
0.0297 |
0.0808 |
|
Smoking |
-0.1983 |
0.046 |
-4.3104 |
<0.01 |
-0.2884 |
-0.1081 |
|
Number of eatung out |
-0.0154 |
0.0103 |
-1.4968 |
-0.0356 |
0.0048 |
|
|
* smoking |
||||||
- The moderating effect of drinking on the effect of eating out on metabolic syndrome
According to the moderating effect of drinking, the interaction effect between the number of eating out and drinking was evaluated to have a negative (-) effect on metabolic syndrome (B=-.0358, p<).001) In other words, it was evaluated that drinking decreased its effect in the relationship where metabolic syndrome increases as the number of eating out increases <Table 7>.
Table 7: Moderating Effect of Drinking
|
|
B |
SE |
t |
p |
95% Confidence interval |
|
|
LLCI |
ULCI |
|||||
|
(Constant variable) |
4.4761 |
0.1299 |
34.4684 |
<.001 |
4.2215 |
4.7307 |
|
Gender(Women=0) |
||||||
|
Men |
0.0973 |
0.0411 |
2.3645 |
<0.5 |
0.0166 |
0.1779 |
|
Age(over 70s=0) |
||||||
|
under 30s |
0.5874 |
0.1187 |
4.9486 |
<.001 |
0.3547 |
0.82 |
|
30s |
-0.4973 |
0.0951 |
-5.2273 |
<.001 |
-0.6838 |
-0.3108 |
|
40s |
-0.4832 |
0.09 |
-5.3709 |
<.001 |
-0.6596 |
-0.3068 |
|
50s |
-0.2539 |
0.082 |
-3.0974 |
<.01 |
-0.4146 |
-0.0932 |
|
60s |
-0.0877 |
0.0739 |
-1.1873 |
<.001 |
-0.2326 |
0.0571 |
|
Number of families(over 4=0) |
||||||
|
1 |
-0.8308 |
0.0762 |
-10.9026 |
<.001 |
-0.9801 |
-0.6814 |
|
2 |
-0.4887 |
0.057 |
-8.5705 |
<.001 |
-0.6005 |
-0.377 |
|
3 |
-0.2125 |
0.0513 |
-4.1396 |
<.001 |
-0.3131 |
-0.1119 |
|
Marital status(Unmarried=0) |
||||||
|
Married |
-0.6879 |
0.0868 |
-7.9255 |
<.001 |
-0.858 |
-0.5177 |
|
Education(Guitar=0) |
||||||
|
Elementary school |
-0.7895 |
0.079 |
-9.9921 |
<.001 |
-0.9444 |
-0.6765 |
|
Middle school |
-0.8224 |
0.0744 |
-11.0501 |
<.001 |
-0.9683 |
-0.6765 |
|
High school |
-1.6566 |
0.0589 |
-33.4692 |
<.001 |
-1.772 |
-1.5412 |
|
2/3year university |
-2.4908 |
0.0744 |
-44.2364 |
<.001 |
-2.6367 |
-2.3449 |
|
4year university |
-2.7416 |
0.062 |
-5.3775 |
<.001 |
-2.8631 |
-2.6201 |
|
Family History |
||||||
|
High Blood pressure(NO=0) |
||||||
|
YES |
-0.2526 |
0.047 |
0.3725 |
<.001 |
-0.3447 |
-0.1605 |
|
Hyperlipidemia(NO=0) |
||||||
|
YES |
0.0329 |
0.0884 |
-0.4592 |
-0.1403 |
0.2062 |
|
|
Ischemic heart disease(NO=0) |
||||||
|
YES |
-0.0447 |
0.0972 |
0.2005 |
-0.2353 |
0.146 |
|
|
Stroke(NO=0) |
||||||
|
YES |
0.0147 |
0.0731 |
1.7713 |
-0.1286 |
0.1579 |
|
|
Diabetes(NO=0) |
||||||
|
YES |
0.1025 |
0.0579 |
6.1845 |
-0.0109 |
0.2159 |
|
|
Number of eating out |
0.0896 |
0.0145 |
5.1281 |
<.001 |
0.0612 |
0.118 |
|
Drinking |
0.1475 |
0.0288 |
-5.1616 |
<.001 |
0.0911 |
0.2039 |
|
Number of eating out |
-0.0358 |
0.0069 |
-2.3645 |
<.001 |
-0.0494 |
-0.0222 |
|
* Drinking |
||||||
- The moderating effect of Stress recognition rate on the effect of eating out on metabolic syndrome
Looking at the moderating effect of the stress recognition rate, it can be seen that the interaction effect between the number of eating out and the stress recognition rate has a negative (-) effect on metabolic syndrome (B=-.0149, p<.001). In other words, it was evaluated that the stress recognition rate further reduces the effect in the relationship where metabolic syndrome increases as the number of eating out increases <Table 8>.
Table 8: Moderating Effect of Stress recognition rate
|
B |
SE |
t |
p |
95% Confidence interval |
||
|
LLCI |
ULCI |
|||||
|
(Constant variable) |
4.6544 |
0.1333 |
34.9289 |
4.3932 |
4.9156 |
|
|
Gender(Women=0) |
||||||
|
Men |
0.0854 |
0.0399 |
2.1389 |
<0.5 |
0.0071 |
0.1637 |
|
Age(over 70s=0) |
||||||
|
under 30s |
0.6301 |
0.1178 |
5.3499 |
<0.01 |
0.3992 |
0.861 |
|
30s |
-0.3806 |
0.094 |
-4.0499 |
-0.5649 |
-0.1964 |
|
|
40s |
-0.399 |
0.0887 |
-4.5005 |
<0.01 |
-0.5728 |
-0.2252 |
|
50s |
-0.1985 |
0.081 |
-2.4507 |
<0.5 |
-0.3573 |
-0.0397 |
|
60s |
-0.0686 |
0.0731 |
-0.9387 |
-0.2118 |
0.0746 |
|
|
Number of families(over 4=0) |
||||||
|
1 |
-0.7952 |
0.0756 |
-10.5176 |
<0.01 |
-0.9434 |
-0.647 |
|
2 |
-0.4526 |
0.0565 |
-8.0155 |
<0.01 |
-0.5633 |
-0.3419 |
|
3 |
-0.1909 |
0.0509 |
-3.7521 |
<0.01 |
-0.2906 |
-0.0911 |
|
Marital status(Unmarried=0) |
|
|
||||
|
Married |
-0.651 |
0.0861 |
-7.5601 |
<0.01 |
-0.8198 |
-0.4822 |
|
Education(Guitar=0) |
||||||
|
Elementary school |
-0.6114 |
0.0797 |
-7.67 |
<0.01 |
-0.7377 |
-0.4551 |
|
Middle school |
-0.6048 |
0.0758 |
-7.9754 |
<0.01 |
-0.7535 |
-0.4561 |
|
High school |
-1.4366 |
0.0612 |
-23.4665 |
<0.01 |
-1.5566 |
-1.3166 |
|
2/3year university |
-2.2737 |
0.0762 |
-29.8367 |
<0.01 |
-2.4231 |
-2.1243 |
|
4year university |
-2.5221 |
0.0644 |
-39.191 |
<0.01 |
-2.6482 |
-2.3959 |
|
Family History |
||||||
|
High Blood pressure(NO=0) |
||||||
|
YES |
-0.2245 |
0.0467 |
-4.81 |
<0.01 |
-0.3161 |
-0.133 |
|
Hyperlipidemia(NO=0) |
||||||
|
YES |
0.0652 |
0.0877 |
0.7435 |
-0.1068 |
0.2372 |
|
|
Ischemic heart disease(NO=0) |
||||||
|
YES |
-0.0216 |
0.0965 |
-0.2238 |
-0.2108 |
0.1676 |
|
|
Stroke(NO=0) |
||||||
|
YES |
0.0326 |
0.725 |
0.4498 |
-0.1095 |
0.1748 |
|
|
Diabetes(NO=0) |
||||||
|
YES |
0.1208 |
0.0574 |
2.1033 |
0.0082 |
0.2333 |
|
|
Number of eating out |
0.0618 |
0.0167 |
3.6936 |
<0.01 |
0.029 |
0.0946 |
|
Stree recognition rate |
-0.2846 |
0.0507 |
-5.6116 |
<0.01 |
-0.384 |
-0.1852 |
|
Number of eating out * |
-0.0149 |
0.012 |
-1.2346 |
<0.01 |
-0.0385 |
-0.0087 |
|
Stress recognition rate |
||||||
4. Discussion
According to a Study [17] on the Age of the Sociodemographic Characteristics of Metabolic Syndrome, the prevalence of hypertension, diabetes, and hypercholesterolemia, which are greatly related to metabolic syndrome, increases as age increases, which is not exactly consistent with this study. The introduction of Western lifestyles increases the preference and frequency of eating instant food among young people and increases the risk of irregular and negative eating due to an increase in irregular life for those under 30s and students, which found be similar with our findings. In previous studies on the prevalence of family history and metabolic syndrome, metabolic syndrome was reported to be higher in the elderly, middle and old age than in cases with no family history of diabetes, myocardial infarction, angina, stroke, high blood pressure, and lipid dyslipidemia [18]. However, in this study, metabolic syndrome was found to be the most common among those in their 30s due to differences in subjects, so it is thought that "no" is higher than "Yes" family history of high blood pressure, hyperlipidemia, ischemic heart disease, stroke, and diabetes. In addition, a study [19] reported that it was irrelevant to the family history as a result of verifying the difference in the number of metabolic syndrome in adult men. Therefore, it is necessary to reveal the specific differences and causes of metabolic syndrome according to the family history through subsequent studies.
Multiple linear regression analysis was conducted to verify the effect of the number of eating out on metabolic syndrome, and demographic characteristics and family history were controlled. As a result, the number of eating out had a significant positive (+) effect on metabolic syndrome. It was evaluated that metabolic syndrome increases as the number of eating out increases. As a previous study on the effect of the number of eating out on metabolic syndrome, the higher the number of eating out, the greater the obesity associated with metabolic syndrome [20]. Also there is a study [21] that the prevalence of metabolic syndrome is high in men who often eat out, so the results of this study were supported. However, according to the analysis [22] of factors related to metabolic syndrome and diet, the lower the number of eating out, the higher the risk of metabolic syndrome, which was not consistent with the results of this study. These results are believed to be due to differences in research timing, and it can be inferred that as dietary life becomes more westernized more than a decade after previous studies, high-density calorie intake increases due to increased consumption of instant food, and metabolic syndrome also increases. The study of the number of eating out and metabolic syndrome during the COVID-19 pandemic also suggests that it will be meaningful in presenting basic data for managing and preventing metabolic syndrome.
To analyze the moderating effect of health behavior on the effect of the number of eating out on metabolic syndrome, the demographic characteristics and family history were controlled, and the analysis was conducted using the SPSS Process Macro No. 1model proposed by Hayes (2013).
First, looking at the moderating effect of smoking, it can be seen that the interaction effect between the number of eating out and smoking does not have a statistically significant effect on metabolic syndrome. In other words, smoking was evaluated to have no effect on the relationship in which metabolic syndrome increases as the number of eating out increases. Although it is difficult to compare because there is no previous study on the moderating effect of smoking on metabolic syndrome, according to a study [23], on the effect of smoking on metabolic syndrome, the risk of developing metabolic syndrome Increased as the amount of smoking increased. Another study [24] also said that the risk of metabolic syndrome increased in the current smoking group, but there was no significant difference in the results of the studies, the 3rd National Health and Nutrition Survey [25]. In addition, as a result of a study [19], it was reported that smoking had no significant difference as a result of verifying the difference in the number of risk factors for metabolic syndrome. In a study of adults, smoking is a statistically significant variable in the metabolic syndrome group and the non-metabolic syndrome group, but there is also a result that it is not effective as a risk factor after correcting other variables [26]. As such, many studies have reported that smoking is a risk factor for metabolic syndrome, but the results are different, and the moderating effect of smoking in this study does not have a statistically significant effect on metabolic syndrome, so the relationship between smoking and metabolic syndrome is expected to require continuous investigation in the future.
Second, looking at the moderating effect of drinking, the interaction effect between the number of times of eating out and drinking had a negative (-) effect on metabolic syndrome. In other words, it was evaluated that drinking decreased its effect in the relationship where metabolic syndrome increases as the number of eating out increases. Previous studies on the moderating effect of drinking on metabolic syndrome cannot be found, so it is difficult to compare, but if you look at the study on the effect of drinking on metabolic syndrome, Drinking increases blood pressure, and the prevalence of metabolic syndrome is higher than that of non-drinkers [27,28,29]. Furthermore, alcohol consumption and metabolic syndrome are not related in both women and men [30]. It is reported [19] that was no significant difference in the number of risk factors for metabolic syndrome by drinking, but there is a study that analyzed that continuous drinking exceeding an appropriate amount affects the increase in the prevalence of metabolic syndrome [31]. Among the effects of drinking, a study reported that it is strongly related to cardiovascular disease as it is related to increased waist circumference and low-density lipoprotein cholesterol, which are risk indicators for metabolic syndrome.10 On the other hand, there are studies showing the preventive effect of cardiovascular disease by increasing insulin sensitivity and increasing high-density lipoprotein cholesterol when consumed in small amounts alcohol [32]. Previous studies that analyzed the relationship between drinking and the occurrence of metabolic syndrome presented different results due to the complex correlation between drinking and metabolic syndrome, and there was no common definition of moderate drinking, excessive drinking, and small amounts of drinking, so the results differed depending on the researcher or institution
Finally, looking at the moderating effect of the stress recognition rate, the interaction effect between the number of meals out and the stress recognition rate had a negative (-) effect on metabolic syndrome. It is found that the stress recognition rate further reduces the effect in the relationship where metabolic syndrome increases as the number of eating out increases. There is no study on the moderating effect of stress recognition rate on metabolic syndrome, so it is difficult to compare and examine the results of this study. Studies on the effects of stress on metabolic syndrome show that stress increases the risk of abdominal obesity, the central mechanism of metabolic syndrome, and exacerbates health behaviors such as excessive calorie intake, smoking, drinking, and lack of physical activity[33]. In addition, psychological factors such as stress, depression, anxiety, and anger are known to increase the risk of type 2 diabetes and cardiovascular disease [34], and male stress increases the incidence of metabolic syndrome [35], which supports this study.
Limitations
First, in the case of data collection, it is difficult to reflect the absolute amount of health-related behavior by using a questionnaire of health behaviors of smoking, drinking, and stress recognition rates, and it is insufficient to secure reliability in response.
Second, the qualitative aspect of individual health behavior items hasn’t been considered.
5. Conclusion
To the above results, this study is the first study on the effect of the number of eating out on metabolic syndrome and the moderating effect of health behavior in Korea.
To prevent metabolic syndrome, the number of times of eating out is reduced, stress management is also necessary during the management of health behavior, and this study is will be useful for using as a basic data for the development of metabolic syndrome prevention and health promotion programs in adults.
The policy implications of this study are as follows.
First, a control tower dedicated to metabolic syndrome is established to change the paradigm of the prevention perspective of metabolic syndrome, requiring specific, systematic, and continuous health management.
Second, various studies related to metabolic syndrome should be conducted nationwide, and customized prevention programs should be developed according to the results so that they can be actively used.
Third, it is necessary to improve the quality of life of patients with chronic diseases, increase access to medical care, and raise the risk and correct perception of metabolic syndrome.
Declarations
Ethics approval and consent to participate:
Ethics approval was waived by an IRB. The name of the IRB is Inje University Busan Paik Hospital Medical Life Research Ethics Review Committee. IRB File NO:2022-06-037
The data used in this study were anonymized before its use.
It confirmed that all methods were carried out in accordance with relevant guidelines and regulations in the declaration
The Content: This study is based on the 8th National Health Survey website (https:/knhanes.kdca.go.KR) We confirm that it is an exemption from deliberation because we obtain approval for the use of raw data from both surveys and use information from which identification information of the study subjects has been removed through research using national health and nutrition survey data
Consent for publication
Not applicable.
Availability of Data and Materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Competing interests
The authors declare that they have no competing interests.
Funding
Not applicable.
Authors' contributions
S.L. contributed to conceptualization, methodology, analysis, writing of original draft preparation, and editing.
Acknowledgements
The author would like to thank all of those who participated in the present study.
References
- National Health Insurance (2019).
- Statistics Korea. Statistics on the Cause of Death in Koreans in (2019).
- Ministry of Health and Welfare. Korea Centers for Disease Control and Prevention Community Health Survey (2009).
- Ministry of Employment and Labor (2014).
- Statistics Korea. Statistics on the Cause of Death in Koreans in (2014).
- WHO Fact sheets_Noncommunicable diseases (2021).
- Ministry of Health and Welfare (2015).
- Baik IK. Studies on Dietary Patterns in the Prevention of Metabolic Syndrome, Dept. of Foods and Nutrition, (master's thesis) College of Natural Sciences, Kookmin University, Seoul, Korea 16 (2011): 45-48.
- Oh SO. Effects of Alcohol on Obesity and Metabolic Syndrome, The Korean journal of obesity 18 (2011): 1-7.
- Jung C, Hark JS, Lee WY, et al. Effects of smoking, alcohol, exercise, level of education, and family history on the metabolic syndrome in Korean adults, Korean Journal of Medicine 63 (2005): 649-659.
- Taylor RB. Family Medicine: principles and practice. 6th ed. New York:Springer-Verlag (2006).
- Oh J D, LEE SY, Kim YJ, et al. Health Behavior and Metabolic Syndrome, Korean Journal of Family Medicine 30 (2009): 120-128.
- Chandola T, Brunner E, and Marmot M. Chronic stress at work and the metabolic syndrome: prospective study 332 (2006): 521-525.
- Kang KW, Sung JH, and Kim CY. High Risk Groups in Health Behavior Defined by Clustering of Smoking, Alcohol, and Exercise Habits, National Health and Nutrition Examination Survey 43 (2010): 73-83
- Kyung KJ. Lifestyle Disease, Journal of the Korean Medical Association 47 (2004): 188-194.
- Korea Centers for Disease Control and Prevention. The 9th (2019) Korea National Health and Nutrition Examination Survey (KNHANES VII). Guidelines for Using Raw Data. Korea Disease Control Prevention Agency, Republic of Korea (2019).
- Kim JY, Lee SW, and Baek H. Effects of Life Style on Metabolic Syndrome Stage according to the Sasang Constitution, Journal of Sasang constitutional medicine 29 (2017): 232-241.
- Park SE. Predictive Factors on Metabolic syndrome of Korean Adult in Age Groups, (master's thesis) Graduate School of Informatiion in Clinical Nursing Hanyang University (2016).
- LEE SJ. The analysis of relationship between lifestyle factors metabolic syndrome in male adult, (master's thesis) Graduate School of education Sungshin women University (2010).
- Kwak CG. Eat out obesity on the impact, Korean Food Science Research (2015).
- Na DW, Jeong E, Noh EK et al. Dietary Factors and Metabolic Syndrome in Middle-Aged, Rural Medical and Community Health Association 35(2010): 383-394.
- Kim M J. Analysis of Dietary Factors and metabolic syndrome for korean Adult -From the Korean National Heaith and Nutrition Examination Survey(2007, 2008), 2011, (master's thesis) Graduate School of Dankook University.
- Jo MK. A study on health behaviors diet and related factors for metabolic syndrome in korea adults, (master's thesis) Graduate School of Public Health, Korea,University (2010).
- Won YJ. Effects of stress and smoking on metabolic syndrome in adults aged 19 to 39 using 2016-2019 Korean National Health and Nutrition Survey, (master's thesis) Department of Epidemiology Graduate School of Public Health Yonsei University (2002).
- Min WH. Study of Food Frequency, Eating Habits and Nutritional Status in Taeumin Metabolic Syndrome Patients, (master's thesis) Graduate School of Kyung Hee University East and West Medicine (2007).
- Kim KR. Retrospective cohort study for risk factors of metabolic syndrome in a periodic health examination, The Graduate School of Hanyang University (2012).
- Han YJ. Trend Analysis on Prevalence Rate and Risk Factor of Metabolic Syndrome, (master's thesis) Major in Public Health Science The Graduate School of Nursing and Health profession Chung-Ang University (2003).
- Moon J H. The Risk Factors of Metabolic Syndrome and its Relation with γ-GTP in Steel-mill Workers, Annals of Occupational and Environmental Medicine 19 (2007): 17-25.
- Song MS. The metabolic syndrome and related factors of heath behavior in koreans, (master's thesis) Graduate School of Chonbuk National University (2011).
- Santos AC, Ebrahim S, and Barros H. Alcohol Intake, Smoking, Sleeping Hours, Physical Activity and the Metabolic Syndrome. Journal of the Preventive Medicine 44 (2007): 328-334.
- Kim SH, Choi HS, Ji SH, et al. Differences in the Prevalence and Lifestyle of Metabolic Syndrome in Korean Adult, Korean Journal of Family Practice 5 (2015): 500-509.
- Facchini F, Chen YD and Reaven GM. Light-tomoderate alcohol intake is associated with enhanced insulin sensitivity. Diabetes Care 17 (1994): 115-117.
- Cohen B E, Panguluri P, Na B, et al. Psychological risk factors and the metabolic syndrome in patients with coronary heart disease: findings from the Heart and Soul Study P sychiatry Research 175 (2010): 133-135
- Van Reedt Dortland A K, Giltay EJ, Van Veen T, et al. Metabolic syndrome abnormalities are associated with severity of anxiety and depression and with tricyclic antidepressant use. Acta P sychiatrica Scandinavica 122 (2010): 30-39.
- Shin DM. Relationship between Stress and Metabolic Syndrome among Korean adults, (master's thesis) Graduate School of of Public Health, the catholic university of korea (2016).