The Design and Process of Ultrasound Guided Evaluation of Septic Arthritis in Emergency Departments
Article Information
Scott C Everett1*, Andrew L Alejo1, Haley Durdella2, Benjamin L Boswell2,3
1College of Medicine, Northeast Ohio Medical University (NEOMED), Rootstown OH, USA
2Department of Emergency Medicine, University Hospitals, Cleveland OH, USA
3Department of Sports Medicine, University Hospitals, Cleveland OH, USA
*Corresponding Author: Scott C Everett, College of Medicine, Northeast Ohio Medical University (NEOMED), Rootstown OH, USA.
Received: 13 March 2023; Accepted: 14 April 2023; Published: 19 April 2023
Citation:
Scott C Everett, Andrew L Alejo, Haley Durdella, Benjamin L Boswell. The Design and Process of Ultrasound Guided Evaluation of Septic Arthritis in Emergency Departments. Journal of Orthopedics and Sports Medicine. 5 (2023): 188-191.
View / Download Pdf Share at FacebookAbstract
The current standard of evaluating septic arthritis in the emergency department involves arthrocentesis analysis and culture. Culture results can then help guide pathogen specific treatment. Without prompt treatment of septic arthritis, the joint undergoes irreversible destruction leading to chronic pain and need for surgical replacement. Therefore, we propose an additional method and process of using ultrasound imaging in order to evaluate certain findings that could be used to help diagnose septic arthritis without having to undergo additional procedures. Using the ultrasound prior to doing arthrocentesis can help increase available information that allows the emergency department physician to use their best clinical judgment as to the proceeding treatment or need for additional testing. This improves the quality of care for our patients in a cost effective manner. By outlining the steps involved, including the specific ultrasound technique, further studies can be guided in order to find specific imaging findings using ultrasonography that correlates to septic arthritis.
Keywords
Ultrasound; Septic arthritis; Septic joint; Tenosynovitis; Infection
Sports medicine articles Sports medicine Research articles Sports medicine review articles Sports medicine PubMed articles Sports medicine PubMed Central articles Sports medicine 2023 articles Sports medicine 2024 articles Sports medicine Scopus articles Sports medicine impact factor journals Sports medicine Scopus journals Sports medicine PubMed journals Sports medicine medical journals Sports medicine free journals Sports medicine best journals Sports medicine top journals Sports medicine free medical journals Sports medicine famous journals Sports medicine Google Scholar indexed journals Septic arthritis articles Septic arthritis Research articles Septic arthritis review articles Septic arthritis PubMed articles Septic arthritis PubMed Central articles Septic arthritis 2023 articles Septic arthritis 2024 articles Septic arthritis Scopus articles Septic arthritis impact factor journals Septic arthritis Scopus journals Septic arthritis PubMed journals Septic arthritis medical journals Septic arthritis free journals Septic arthritis best journals Septic arthritis top journals Septic arthritis free medical journals Septic arthritis famous journals Septic arthritis Google Scholar indexed journals Joint articles Joint Research articles Joint review articles Joint PubMed articles Joint PubMed Central articles Joint 2023 articles Joint 2024 articles Joint Scopus articles Joint impact factor journals Joint Scopus journals Joint PubMed journals Joint medical journals Joint free journals Joint best journals Joint top journals Joint free medical journals Joint famous journals Joint Google Scholar indexed journals Orthopaedic articles Orthopaedic Research articles Orthopaedic review articles Orthopaedic PubMed articles Orthopaedic PubMed Central articles Orthopaedic 2023 articles Orthopaedic 2024 articles Orthopaedic Scopus articles Orthopaedic impact factor journals Orthopaedic Scopus journals Orthopaedic PubMed journals Orthopaedic medical journals Orthopaedic free journals Orthopaedic best journals Orthopaedic top journals Orthopaedic free medical journals Orthopaedic famous journals Orthopaedic Google Scholar indexed journals Joint destruction articles Joint destruction Research articles Joint destruction review articles Joint destruction PubMed articles Joint destruction PubMed Central articles Joint destruction 2023 articles Joint destruction 2024 articles Joint destruction Scopus articles Joint destruction impact factor journals Joint destruction Scopus journals Joint destruction PubMed journals Joint destruction medical journals Joint destruction free journals Joint destruction best journals Joint destruction top journals Joint destruction free medical journals Joint destruction famous journals Joint destruction Google Scholar indexed journals Rheumatoid arthritis articles Rheumatoid arthritis Research articles Rheumatoid arthritis review articles Rheumatoid arthritis PubMed articles Rheumatoid arthritis PubMed Central articles Rheumatoid arthritis 2023 articles Rheumatoid arthritis 2024 articles Rheumatoid arthritis Scopus articles Rheumatoid arthritis impact factor journals Rheumatoid arthritis Scopus journals Rheumatoid arthritis PubMed journals Rheumatoid arthritis medical journals Rheumatoid arthritis free journals Rheumatoid arthritis best journals Rheumatoid arthritis top journals Rheumatoid arthritis free medical journals Rheumatoid arthritis famous journals Rheumatoid arthritis Google Scholar indexed journals Prosthetic joint articles Prosthetic joint Research articles Prosthetic joint review articles Prosthetic joint PubMed articles Prosthetic joint PubMed Central articles Prosthetic joint 2023 articles Prosthetic joint 2024 articles Prosthetic joint Scopus articles Prosthetic joint impact factor journals Prosthetic joint Scopus journals Prosthetic joint PubMed journals Prosthetic joint medical journals Prosthetic joint free journals Prosthetic joint best journals Prosthetic joint top journals Prosthetic joint free medical journals Prosthetic joint famous journals Prosthetic joint Google Scholar indexed journals Corticosteroid injections articles Corticosteroid injections Research articles Corticosteroid injections review articles Corticosteroid injections PubMed articles Corticosteroid injections PubMed Central articles Corticosteroid injections 2023 articles Corticosteroid injections 2024 articles Corticosteroid injections Scopus articles Corticosteroid injections impact factor journals Corticosteroid injections Scopus journals Corticosteroid injections PubMed journals Corticosteroid injections medical journals Corticosteroid injections free journals Corticosteroid injections best journals Corticosteroid injections top journals Corticosteroid injections free medical journals Corticosteroid injections famous journals Corticosteroid injections Google Scholar indexed journals Synovial arthrocentesis articles Synovial arthrocentesis Research articles Synovial arthrocentesis review articles Synovial arthrocentesis PubMed articles Synovial arthrocentesis PubMed Central articles Synovial arthrocentesis 2023 articles Synovial arthrocentesis 2024 articles Synovial arthrocentesis Scopus articles Synovial arthrocentesis impact factor journals Synovial arthrocentesis Scopus journals Synovial arthrocentesis PubMed journals Synovial arthrocentesis medical journals Synovial arthrocentesis free journals Synovial arthrocentesis best journals Synovial arthrocentesis top journals Synovial arthrocentesis free medical journals Synovial arthrocentesis famous journals Synovial arthrocentesis Google Scholar indexed journals Erythematous articles Erythematous Research articles Erythematous review articles Erythematous PubMed articles Erythematous PubMed Central articles Erythematous 2023 articles Erythematous 2024 articles Erythematous Scopus articles Erythematous impact factor journals Erythematous Scopus journals Erythematous PubMed journals Erythematous medical journals Erythematous free journals Erythematous best journals Erythematous top journals Erythematous free medical journals Erythematous famous journals Erythematous Google Scholar indexed journals Arthrocentesis articles Arthrocentesis Research articles Arthrocentesis review articles Arthrocentesis PubMed articles Arthrocentesis PubMed Central articles Arthrocentesis 2023 articles Arthrocentesis 2024 articles Arthrocentesis Scopus articles Arthrocentesis impact factor journals Arthrocentesis Scopus journals Arthrocentesis PubMed journals Arthrocentesis medical journals Arthrocentesis free journals Arthrocentesis best journals Arthrocentesis top journals Arthrocentesis free medical journals Arthrocentesis famous journals Arthrocentesis Google Scholar indexed journals Knee joint articles Knee joint Research articles Knee joint review articles Knee joint PubMed articles Knee joint PubMed Central articles Knee joint 2023 articles Knee joint 2024 articles Knee joint Scopus articles Knee joint impact factor journals Knee joint Scopus journals Knee joint PubMed journals Knee joint medical journals Knee joint free journals Knee joint best journals Knee joint top journals Knee joint free medical journals Knee joint famous journals Knee joint Google Scholar indexed journals Crystal arthropathy articles Crystal arthropathy Research articles Crystal arthropathy review articles Crystal arthropathy PubMed articles Crystal arthropathy PubMed Central articles Crystal arthropathy 2023 articles Crystal arthropathy 2024 articles Crystal arthropathy Scopus articles Crystal arthropathy impact factor journals Crystal arthropathy Scopus journals Crystal arthropathy PubMed journals Crystal arthropathy medical journals Crystal arthropathy free journals Crystal arthropathy best journals Crystal arthropathy top journals Crystal arthropathy free medical journals Crystal arthropathy famous journals Crystal arthropathy Google Scholar indexed journals Quadricep tendon articles Quadricep tendon Research articles Quadricep tendon review articles Quadricep tendon PubMed articles Quadricep tendon PubMed Central articles Quadricep tendon 2023 articles Quadricep tendon 2024 articles Quadricep tendon Scopus articles Quadricep tendon impact factor journals Quadricep tendon Scopus journals Quadricep tendon PubMed journals Quadricep tendon medical journals Quadricep tendon free journals Quadricep tendon best journals Quadricep tendon top journals Quadricep tendon free medical journals Quadricep tendon famous journals Quadricep tendon Google Scholar indexed journals Bursitis articles Bursitis Research articles Bursitis review articles Bursitis PubMed articles Bursitis PubMed Central articles Bursitis 2023 articles Bursitis 2024 articles Bursitis Scopus articles Bursitis impact factor journals Bursitis Scopus journals Bursitis PubMed journals Bursitis medical journals Bursitis free journals Bursitis best journals Bursitis top journals Bursitis free medical journals Bursitis famous journals Bursitis Google Scholar indexed journals
Article Details
Abbreviations:
CT: Computed Tomography; FAST: Focused Assessment with Sonography for Trauma; IRB: Institutional Review Board; MRI: Magnetic Resonance Imaging; POCUS: Point of Care Ultrasound; RUSH: Rapid Ultrasound in Shock; US: Ultrasound
1. Introduction
Septic arthritis is an inflammatory process that may involve one or multiple joints. The inflammation is secondary to an infection with a bacteria, fungi, mycobacteria, virus, or other pathogen [1]. It is usually monoarticular, involving a large joint such as the hip or knee, however polyarticular septic arthritis that involves more than one joint or the smaller joints is also prevalent. Acute bacterial septic arthritis is an orthopaedic emergency, and if not treated promptly, can lead to substantial joint destruction. Various risk factors include older age (>60 years old), trauma, recent bacteremia, diabetes, cirrhosis, renal disease, intravenous drug use, a history of corticosteroid injections, a prosthetic joint, or rheumatoid arthritis [2].
If there is any clinical suspicion for septic arthritis, such as erythema, pain, or edema of the joint, it is important to culture the synovial fluid to find specific microorganisms that guide initial antibiotic choice. The most common pathogen involved is Staphylococcus aureus, with Methicillin-resistant Staphylococcus aureus also leading to deleterious effects to the joint [3]. Commonly, vancomycin is used for gram-positive cocci, ceftriaxone for gram-negative cocci, and ceftazidime for gram-negative rods [4]. If the fluid culture returns as negative for organisms, yet the clinician is still suspecting septic arthritis, a broad-spectrum combination of vancomycin plus ceftazidime or an aminoglycoside is appropriate [4]. Treatment must not be delayed, as this can lead to further serious complications locally, and systemically.
The current standard of practice for septic arthritis when a patient arrives in the emergency room is joint aspiration with fluid analysis and culture and clinical judgement when to start antibiotics while the analysis and culture are pending [5] as shown in Figure 1. Ultrasound is an imaging technique that can be done quickly as soon as the patient arrives to the emergency room. Costs of operation for an ultrasound in comparison to Computed Tomography (CT) or Magnetic Resonance Imaging (MRI), is often a much less financial burden to the patient. Ultrasound has been implemented in Focused Assessment with Sonography for Trauma (FAST) exams when patients come in to quickly get information that guides clinical judgement in trauma emergencies. Additionally, the Rapid Ultrasound in Shock (RUSH) examination can also be quickly implemented for diagnosis of shock etiology in critically ill patients [6]. Therefore, the ease, accessibility, and convenience of using ultrasounds in the emergency room should be explored in evaluating septic arthritis.
The purpose of this paper is to outline the technique and steps needed to evaluate septic arthritis with ultrasound findings to further clinical judgement when a patient presents with a proposed case of septic arthritis. Having more information to give better underlying data when deciding the best course of action, is always advantageous for both the patient, and the physician, leading to higher quality of patient care. While not the current standard of care, using an ultrasound prior to doing synovial arthrocentesis, may yield additional results that can guide the treatment plan without having to do additional procedures while only taking a few minutes to perform for those trained in ultrasound guided techniques.
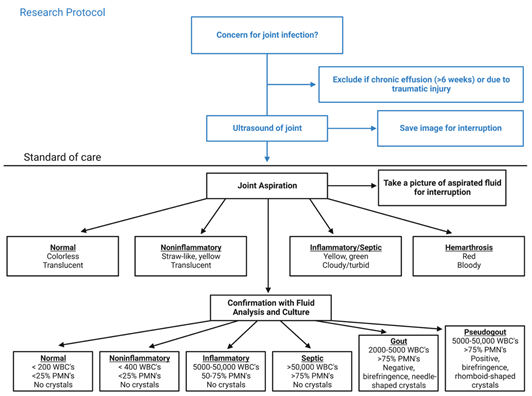
Figure 1: Research Protocol with Current Standard of Care.
2. Methods
The electronic arrival board in the emergency department will be used to prescreen a patient’s chief complaint: erythematous, edematous, warm and/or painful joint. The potential participant’s treating attending physician will give approval for recruitment prior to approach. A study team member who is approved to obtain consent will go through the consent form with the patient and make sure the patient understands the risks and benefits and all questions they may have are answered. Patients are offered to enroll in study if inclusion criteria was met. The provider contacted one of the US physicians to inform them of potential participants if they were not on service. All studies must be approved by the participants’ Institutional Review Board (IRB) prior to enrolling patients. All patients that were recruited gave informed consent.
Inclusion criteria included age range from 18 to 89 years old and an erythematous, edematous, warm, painful joint. Exclusion criteria included chronic joint effusion (>6 weeks) and traumatic joint injury. Patients who meet study inclusion criteria and who consent to the study will be assessed with the standard of care as well as with an ultrasound image. Participant’s medical records will be accessed to collect data about subjects prior to intervention. Clinical findings that will be recorded will include a full set of patient’s vital signs (heart rate, blood pressure, temperature, respiratory rate and pulse oximetry), as well as appearance of joint from physical exam (erythematous, edematous, warm to palpation, tender to palpation, and range of motion assessment).
The current standard of care to assess a septic joint is an arthrocentesis and laboratory fluid analysis of the aspirated fluid to determine the final diagnosis. Prior to performing the standard of care, an ultrasound image of the involved joint will be saved for interruption. The ultrasound image will be assessed for an effusion (>2mm between capsule and bone). The fluid inside the effusion will be assessed. The ultrasound image will be captured using a Mindray M9 Ultrasound System.
A linear probe was used to assess the knee joint. An anterior longitudinal suprapatellar approach was used as seen in Figure 2. The patient lies supine with the knee flexed at 15 degrees, while the transducer was placed longitudinally in the midline with the distal end of the probe over the superior pole of the patella, while fanning the probe to get the optimal angle to assess the knee joint. Overlying skin or subcutaneous tissue was also assessed on ultrasound for cobblestoning. A researcher that is blinded to the final diagnosis and fluid analysis will evaluate the ultrasound image for interruption. The image interruption will then be compared to the standard of care (fluid analysis and final diagnosis) in order to draw conclusions regarding findings on ultrasound images in the setting of a septic joint. These patients will be contacted and communicated with only while in the Emergency Department and no follow up was needed.
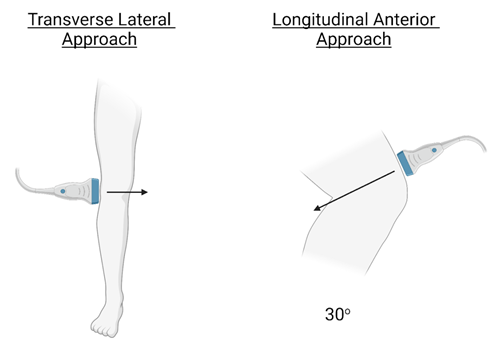
Figure 2: Approaches to Scanning the Knee Joint.
3. Discussion
A review article on sonography of knee effusions stated that for fluid evaluation in the knee, US and MRI were highly correlated [7]. One study cited in this article stated the most sensitive sonographic approach is the transverse scan of the lateral parapatellar recess with knee extension [8,9]. Detection of fluid levels at 4mL in live patients was evaluated. Another study in the article showed that a longitudinal scan of the suprapatellar recess with 30 degrees of knee flexion is superior to scans of the lateral and medial parapatellar recesses at various angles of flexion (0°, 15°, 30°, 45°, 60°, and 90°) [10]. The anterior longitudinal suprapatellar approach, as outlined above in addition to the lateral transverse approach, both appear to be valid ways to obtain images that can be used to evaluate septic arthritis. Additionally, while scanning for effusions in the synovial recesses, other differentials to consider are cysts, bursitis, and other lesions such as crystal arthropathy.
Transverse imaging on the lateral aspect of the knee as seen in Figure 2, allows for proper assessment of the lateral patellar retinaculum, lateral femoral condyle, medial femoral condyle, and patella. The anterior approach utilizing the sagittal approach allows for assessment of the quadricep tendon, quadriceps fat pad, prefemoral fat pad, the distal end of the femur, and the joint recess. Suggested protocol for effusions is to start with a longitudinal scan of the lateral parapatellar recess with the knee in extension. If signs of effusion are present, no further imaging is necessary. If results of the lateral scan are negative or equivocal and there is still a high suspicion for effusion, it is recommended to evaluate the suprapatellar recess of the knee anterior with the knee flexed at 30 degrees [10].
A recent report by Kim et al. [11] used ultrasonography of the interphalangeal joint of the thumb to evaluate possible septic arthritis which displayed intra-articular effusion. They also described imaging of diffuse low-level echoes, which is characteristic of a septic origin. Similarly, Perez et al. [12] used point of care ultrasound (POCUS) to evaluate septic arthritis in the glenohumeral joint, as well as subdeltoid septic bursitis. They identified glenohumeral joint effusion, a distending hypoechoic subdeltoid bursa, and communication between these two fluid collections, suggestive of an infraspinatus rotator cuff tear. These previous studies both employed ultrasound in assistance to diagnose septic arthritis of various joints. Although they ended up both doing arthrocentesis to confirm the diagnosis of septic arthritis after the ultrasound, starting to deploy ultrasounds for evaluations of joints further supports new techniques to help diagnose septic arthritis.
In this study we explained how to use ultrasound to evaluate a joint for septic arthritis, specifically, the technique used to capture these images was described. This technique can assist further additional studies to help recognize ultrasound specific findings that correlate to septic arthritis. Being able to evaluate images without having to undergo one or more additional procedures with accurate diagnosis is beneficial to both the patient and the emergency department physician. Currently, there has not been any studies that evaluated ultrasound findings in septic arthritis in humans, which is a valuable additional study using the techniques described in this paper.
Conflicts of Interest
The authors have no conflicts of interest to declare.
References
- Earwood JS, Walker TR, Sue GJC. Septic Arthritis: Diagnosis and Treatment. Am Fam Physician 104 (2021): 589-597.
- Elsissy JG, Liu JN, Wilton PJ, et al. Bacterial Septic Arthritis of the Adult Native Knee Joint: A Review. JBJS Rev 8 (2020): e0059.
- Balato G, de Matteo V, Ascione T, et al. Management of septic arthritis of the hip joint in adults. A systematic review of the literature. BMC Musculoskelet Disord 22 (2021): 1006.
- Horowitz DL, Katzap E, Horowitz S, et al. Approach to septic arthritis. Am Fam Physician 84 (2011): 653-660.
- Long B, Koyfman A, Gottlieb M. Evaluation and Management of Septic Arthritis and its Mimics in the Emergency Department. West J Emerg Med 20 (2019): 331-341.
- Ghane MR, Gharib M, Ebrahimi A, et al. Accuracy of early rapid ultrasound in shock (RUSH) examination performed by emergency physician for diagnosis of shock etiology in critically ill patients. J Emerg Trauma Shock 8 (2015): 5-10.
- Li TY. Sonography of Knee Effusion. Journal of Diagnostic Medical Sonography 36 (2020): 545-558.
- Clark G. Popliteal (Baker’s) cysts of the knee. J Prolother 396 (2010): 396.
- Ward EE, Jacobson JA, Fessell DP, et al. Sonographic detection of Baker's cysts: comparison with MR imaging. American Journal of Roentgenology 176 (2001): 373-380.
- Mandl P, Brossaed M, Aegerter P, et al. Ultrasound evaluation of fluid in knee recesses at varying degrees of flexion. Arthritis care and research 64 (2012): 773-779.
- Kim S, Baradia H, Sambasivan A. The Use of Ultrasonography in Expediting Septic Joint Identification and Treatment: A Case Report. American Journal of Physical Medicine and Rehabilitation 99 (2020).
- Perez J, Sorensen S, Rosselli M. Utilisation of musculoskeletal ultrasonography for the evaluation of septic arthritis in a patient presenting to the emergency department with fever during the era of COVID-19. BMJ Case Reports 14 (2021): e242370.
