The Clinical Presentation and Management of Postpartum Haemorrhage: A Single Center Experience
Article Information
Lubna Jahan1*, Kaoser Jahan2, Shabeen Afreen3, Sharmin Akter4, Yeasmin Akter5, Nafisa Jesmin6, Shanta Tribedi7, Sharmin Nahar8, Pushpita Sharmin9, A K M Shahidur Rahman10
1Junior Consultant, Department of Obstetrics and Gynecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh
2Associate Professor, Department of Obstetrics and Gynecology, Army Medical College, Cumilla, Bangladesh
3Assistant Professor, Department of Obstetrics and Gynecology, Kurmitola General Hospital, Dhaka, Bangladesh
4Assistant Professor, Department of Obstetrics and Gynecology, Institute of Child and Mother Health, Matuail, Dhaka, Bangladesh
5Consultant Gynecologist, Department of Gynecology and Obstetrics, Combined Military Hospital (CMH), Dhaka, Bangladesh
6Junior Consultant, Department of Obstetrics and Gynecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh
7Junior Consultant, Department of Obstetrics and Gynecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh
8Medical Officer, Department of Obstetrics and Gynecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh
9Medical Officer, Department of Obstetrics and Gynecology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
10Medical Officer, Department of Nephrology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
*Corresponding Author: Dr. Lubna Jahan, Junior Consultant, Department of Obstetrics and Gynaecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh.
Received: 26 May 2023; Accepted: 01 June 2023; Published: 06 June 2023
Citation: Jahan L, Jahan K, Afreen S, Akter S, Akter Y, Jesmin N, Tribedi S, Nahar S, Sharmin P, Rahman AKMS. The Clinical Presentation and Management of Postpartum Haemorrhage: A Single Center Experience. Obstetrics and Gynecology Research. 6 (2023): 182-187.
View / Download Pdf Share at FacebookAbstract
Postpartum haemorrhage (PPH) is a potentially life threatening complication of each child delivery. PPH is one of the leading causes of maternal mortality and morbidity in the developing countries. This hospital based observational study was conducted among 100 patients with postpartum haemorrhage (PPH) to assess the clinical presentation and management of PPH. The mean(±SD) age of the study patients was 25±5.40 years; most of the patients were multiparous, delivered at term that took place at home but had no previous medical disease, while a small proportion of the study patients had history of proper antenatal care (ANC). It was observed that PPH frequently developed following vaginal delivery had various risk factors and most of which were primary PPH. The uterine atony was the major causes (52%) of PPH, followed by genital tract trauma (18%), retained placenta (16%) and retained bits of placental tissue/membrane (8%). Regarding management; oxytocics was used in 71% patients, 100% study patients required blood transfusion, of them 44% cases were treated by conservative medical management, 51% cases were managed by minor surgical procedure and 5% cases needed major surgical procedure. Only 6% study cases developed various complications like- sepsis, transfusion reaction, renal failure and shock. Therefore, all pregnant women should have proper ante natal care (ANC) and better maternal outcome could be ensured by proper management at appropriate time.
Keywords
Clinical Presentation; Management; Maternal Mortality; Postpartum Haemorrhage (PPH)
Clinical Presentation articles Clinical Presentation Research articles Clinical Presentation review articles Clinical Presentation PubMed articles Clinical Presentation PubMed Central articles Clinical Presentation 2023 articles Clinical Presentation 2024 articles Clinical Presentation Scopus articles Clinical Presentation impact factor journals Clinical Presentation Scopus journals Clinical Presentation PubMed journals Clinical Presentation medical journals Clinical Presentation free journals Clinical Presentation best journals Clinical Presentation top journals Clinical Presentation free medical journals Clinical Presentation famous journals Clinical Presentation Google Scholar indexed journals Management articles Management Research articles Management review articles Management PubMed articles Management PubMed Central articles Management 2023 articles Management 2024 articles Management Scopus articles Management impact factor journals Management Scopus journals Management PubMed journals Management medical journals Management free journals Management best journals Management top journals Management free medical journals Management famous journals Management Google Scholar indexed journals Maternal Mortality articles Maternal Mortality Research articles Maternal Mortality review articles Maternal Mortality PubMed articles Maternal Mortality PubMed Central articles Maternal Mortality 2023 articles Maternal Mortality 2024 articles Maternal Mortality Scopus articles Maternal Mortality impact factor journals Maternal Mortality Scopus journals Maternal Mortality PubMed journals Maternal Mortality medical journals Maternal Mortality free journals Maternal Mortality best journals Maternal Mortality top journals Maternal Mortality free medical journals Maternal Mortality famous journals Maternal Mortality Google Scholar indexed journals Postpartum Haemorrhage articles Postpartum Haemorrhage Research articles Postpartum Haemorrhage review articles Postpartum Haemorrhage PubMed articles Postpartum Haemorrhage PubMed Central articles Postpartum Haemorrhage 2023 articles Postpartum Haemorrhage 2024 articles Postpartum Haemorrhage Scopus articles Postpartum Haemorrhage impact factor journals Postpartum Haemorrhage Scopus journals Postpartum Haemorrhage PubMed journals Postpartum Haemorrhage medical journals Postpartum Haemorrhage free journals Postpartum Haemorrhage best journals Postpartum Haemorrhage top journals Postpartum Haemorrhage free medical journals Postpartum Haemorrhage famous journals Postpartum Haemorrhage Google Scholar indexed journals vaginal articles vaginal Research articles vaginal review articles vaginal PubMed articles vaginal PubMed Central articles vaginal 2023 articles vaginal 2024 articles vaginal Scopus articles vaginal impact factor journals vaginal Scopus journals vaginal PubMed journals vaginal medical journals vaginal free journals vaginal best journals vaginal top journals vaginal free medical journals vaginal famous journals vaginal Google Scholar indexed journals caesarean delivery articles caesarean delivery Research articles caesarean delivery review articles caesarean delivery PubMed articles caesarean delivery PubMed Central articles caesarean delivery 2023 articles caesarean delivery 2024 articles caesarean delivery Scopus articles caesarean delivery impact factor journals caesarean delivery Scopus journals caesarean delivery PubMed journals caesarean delivery medical journals caesarean delivery free journals caesarean delivery best journals caesarean delivery top journals caesarean delivery free medical journals caesarean delivery famous journals caesarean delivery Google Scholar indexed journals placenta articles placenta Research articles placenta review articles placenta PubMed articles placenta PubMed Central articles placenta 2023 articles placenta 2024 articles placenta Scopus articles placenta impact factor journals placenta Scopus journals placenta PubMed journals placenta medical journals placenta free journals placenta best journals placenta top journals placenta free medical journals placenta famous journals placenta Google Scholar indexed journals cervical lacerations articles cervical lacerations Research articles cervical lacerations review articles cervical lacerations PubMed articles cervical lacerations PubMed Central articles cervical lacerations 2023 articles cervical lacerations 2024 articles cervical lacerations Scopus articles cervical lacerations impact factor journals cervical lacerations Scopus journals cervical lacerations PubMed journals cervical lacerations medical journals cervical lacerations free journals cervical lacerations best journals cervical lacerations top journals cervical lacerations free medical journals cervical lacerations famous journals cervical lacerations Google Scholar indexed journals uterine rupture articles uterine rupture Research articles uterine rupture review articles uterine rupture PubMed articles uterine rupture PubMed Central articles uterine rupture 2023 articles uterine rupture 2024 articles uterine rupture Scopus articles uterine rupture impact factor journals uterine rupture Scopus journals uterine rupture PubMed journals uterine rupture medical journals uterine rupture free journals uterine rupture best journals uterine rupture top journals uterine rupture free medical journals uterine rupture famous journals uterine rupture Google Scholar indexed journals pre-eclampsia articles pre-eclampsia Research articles pre-eclampsia review articles pre-eclampsia PubMed articles pre-eclampsia PubMed Central articles pre-eclampsia 2023 articles pre-eclampsia 2024 articles pre-eclampsia Scopus articles pre-eclampsia impact factor journals pre-eclampsia Scopus journals pre-eclampsia PubMed journals pre-eclampsia medical journals pre-eclampsia free journals pre-eclampsia best journals pre-eclampsia top journals pre-eclampsia free medical journals pre-eclampsia famous journals pre-eclampsia Google Scholar indexed journals
Article Details
1. Introduction
Postpartum haemorrhage (PPH) remains one of the major causes of maternal deaths in both developing and developed countries worldwide; over 125000 women die of postpartum haemorrhage (PPH) each year[1]. Postpartum haemorrhage (PPH) is a potentially life threatening complication of both vaginal and caesarean delivery[2]. PPH is best diagnosed clinically as excessive bleeding that makes the patients symptomatic (pallor, weakness, palpitation, restlessness, confusion, syncope) and result in sign of hypovolemia (hypotension, tachycardia, oliguria, low oxygen saturation) [2]. A timely accurate diagnosis of PPH is important to initiate intervention and improve outcome [1-2]. Postpartum haemorrhage (PPH) can be divided into two types: primary PPH that occurs within 24 hours after delivery and secondary PPH that occurs 24 hours to 6 weeks after delivery [1-2]. According to World Health Organization (WHO), definition of primary PPH is the loss of 500 ml or more blood from the genital tract within 24 hours after birth of a baby[3]. Postpartum haemorrhage (PPH) is a leading cause of maternal death worldwide; the average maternal mortality rate from PPH is 25%[4]. In Bangladesh about 31% of maternal death occurs due to PPH[5]. The most common cause of immediate severe PPH (that is occurring within 24 hours of delivery) is uterine atony (failure of the uterus to properly contract after delivery); retained placenta, vaginal or cervical lacerations and uterine rupture or inversion also contribute to PPH[6]. Delayed PPH (occurring more than 24 hours after childbirth) often results from infection, sub-involution or retained placental fragments[6]. Factors that are thought to increase the risk of PPH are- over distension (multiple pregnancy, macrosomia/polyhydramious), prolonged labour, induced or augmented labour, grand multiparity (more than 4), instrumental delivery, pre-eclampsia, problems with placenta (retained placenta, placenta previa), previous PPH, maternal bleeding disorder etc[7]. Complication from PPH includes anaemia and hypovolumic shock; blood transfusion may be necessary and transfusion associated risks are not uncommon[8]. In severe cases haemorragic shock may lead to anterior pituitary ischemia with delay or failure of lactation (i.e. postpartum pituitary necrosis), acute renal failure, disseminated intravascular coagulation (DIC) or death may also occur[8]. The use of prophylactic oxytocics in active management of the third stage of labour reduces risk of PPH by 60% [9]. Together with the prevention, active management and treatment of anemia and skilled birth attendance at all deliveries can prevent PPH in thousands of women worldwide each year. This study was undertaken to assess the clinical presentation and management of postpartum haemorrhage (PPH) at a tertiary care hospital in Bangladesh. This study helps to draw attention necessary for the prevention and management of postpartum haemorrhage (PPH).
2. Materials and Methods
This prospective observational study was conducted at Department of Obstetrics and Gynaecology, Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh. The study protocol was approved by the institutional review board (IRB), DMCH, Dhaka, Bangladesh. A total of 100 patients with PPH were enrolled according to the selection criteria. Patients admitted in DMCH with gestational age more than 28 weeks and developed PPH (both primary and secondary) following delivery (by normal vaginal delivery or caesarean section) were included. Patients with gestational age less than 28 weeks were excluded from the study. Informed written consent was obtained from each study patient prior to enrollment. Relevant physical and clinical examinations of each patient were performed then presentation, causes, risk factors, management and outcome of PPH were assessed accordingly. All necessary information of each patient was collected from hospital records. Collected data were cross-checked and compiled. Statistical analysis was performed by using computer based soft-ware Statistical Package for Social Science (SPSS).
3. Results and Observations
This study was intended to assess the clinical profile and management among 100 cases of PPH. The mean age of the study patients was 25±5.40 years (Table- 1). Most of the patients (36%) fall in the age group of 25 to 30 years, while lowest number of patients (2%) belongs to the 35 to 40 years age group. On the other hand, second lowest percentage (24%) belongs to the age group 15 to 20 years (Table- 1). Most of the patients were house wife (65%) and 35% patients were service holder (Table- 1). In this study; most of the patients (58%) were multiparous with an average of 2-4 child and only 14% have 1 child, while 28% had >4 child (Table- 1). It was observed that, most of the study patients delivered at term, 76% of them were in between 37-40 weeks, 14% beyond 40 weeks and 10% in between 34-36 weeks (Table- 1). In this study only a small proportion of the patients (19%) consulted qualified persons such as doctors, nurses and family welfare visitors (FWV) while most of the patients (81%) had negative answer regarding antenatal care (ANC) (Table- 1).
|
Variables |
Frequency (n) |
Percentage (%) |
|
Age (mean±SD) |
25±5.40 years |
|
|
Age group (in year) |
||
|
15-20 |
24 |
24 |
|
20-25 |
22 |
22 |
|
25-30 |
36 |
36 |
|
30-35 |
16 |
16 |
|
35-40 |
2 |
2 |
|
Occupational status |
||
|
House wife |
65 |
65 |
|
Service holder |
35 |
35 |
|
Parity |
||
|
1 |
14 |
14 |
|
02-Apr |
58 |
58 |
|
>4 |
28 |
28 |
|
Gestational age (in weeks) |
||
|
34-36 |
10 |
10 |
|
37-40 |
76 |
76 |
|
40+ |
14 |
14 |
|
Antenatal care (ANC) during their most recent pregnancy |
||
|
Consulted |
19 |
19 |
|
Not consulted |
81 |
81 |
Table 1: Basic data of the study population (N= 100)
Among the 100 PPH patients; 14% patients had different medical disease, of them 10% women had hypertension, 2% women had diabetes mellitus and 2% women had jaundice during pregnancy, but 86% study patients had no medical disease (Figure- 1).
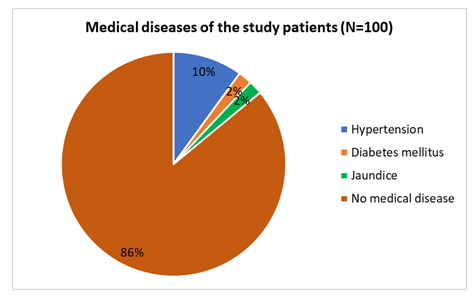
Figure 1: Distribution of different medical diseases among the study patients (N= 100)
Data analysis revealed that, most to the deliveries (80%) took place at home. Percentage of PPH (20%) was low among hospital deliveries due to routine use of active management at third stage of labour in hospitals (Figure- 2).
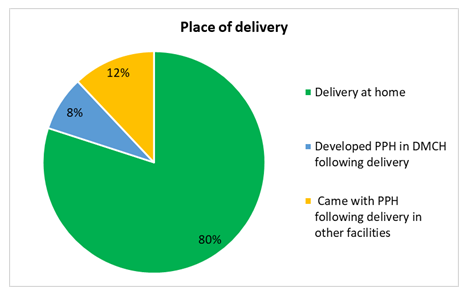
Figure 2: Distribution of the study cases by place of delivery (N= 100)
Out of 100 study patients; 84% patient had PPH following vaginal delivery, 8% patients developed PPH after lower uterine caesarean section (LUCS) delivery and 6% PPH was due to instrumental delivery. Only 1 patient underwent subtotal hysterectomy following ruptured uterus and 1 patient developed PPH during caesarean section due to placenta accrete and after failure of conservative management caesarean hysterectomy was performed as a life saving measure (Table- 2).
|
Mode of delivery |
Number of patients (n) |
Percentage (%) |
|
Vaginal delivery |
84 |
84 |
|
Instrumental delivery |
6 |
6 |
|
LUCS |
8 |
8 |
|
Caesarean hysterectomy |
1 |
1 |
|
Subtotal hysterectomy following rupture of the uterus |
1 |
1 |
|
Total |
100 |
100 |
Table 2: Distribution of the study patients by mode of delivery (N= 100)
We observed that most of the patients (55%) had no detectable risk factors. On risk factors analysis; 10% study patients had pre-eclampsia or eclampsia, 2% had multiple pregnancies, 6% had ante partum haemorrhage (APH), 2% had hepatitis/Jaundice, 1% had multiple fibroid, 13% had prolonged/obstructed labour, 2% had instrumental delivery and 9% of the patient had prolonged third stage of labour (Table- 3).
|
Risk factors |
Frequency (n) |
Percentage (%) |
|
Pre-eclampsia/eclampsia |
10 |
10 |
|
Multiple pregnancy |
2 |
2 |
|
Ante partum haemorrhage (APH) |
6 |
6 |
|
Hepatitis/Jaundice |
2 |
2 |
|
Multiple fibroid |
1 |
1 |
|
Prolonged/Obstructed labour |
13 |
13 |
|
Instrumental delivery |
2 |
2 |
|
Prolonged 3rd stage of labour |
9 |
9 |
|
No risk factors |
55 |
55 |
|
Total |
100 |
100 |
Table 3: Different risk factors among the study patients (N= 100)
In this study, primary postpartum haemorrhage (PPH) was found in 92% cases and secondary postpartum haemorrhage (PPH) was only in 8% study cases (Figure- 3).
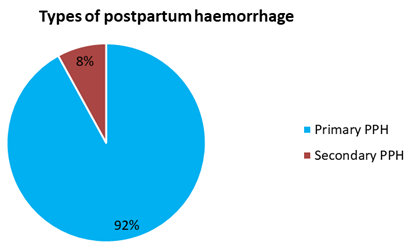
Figure 3: Distribution of study patients by type of postpartum haemorrhage (N= 100)
Among the study patients oxytocics was used in 71% patients; of them only oxytocin was used in 12.70% patients, oxytocin+ ergometrine was used in 40.80% patients, oxytocin+ misoprostol was used in 16.90% patients and oxytocin+ ergometrine+ misoprostol was used in 29.60% patients (Figure- 4).
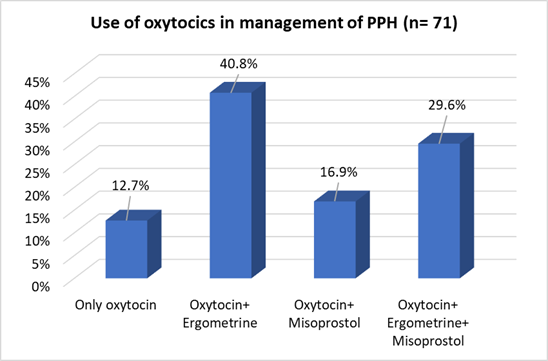
Figure 4: Use of oxytocics in management of PPH (N= 71)
We found that uterine atony was the major causes [52 (52%) cases] of PPH, followed by genital tract trauma in 18 (18%) cases, retained placenta in 16 (16%) cases and retained bits of placental tissue/membrane in 8 (8%) cases. Uterine rupture was found in 2 (2%) cases. One patient was found with placenta accrete and another one was found uterine inversion during caesarean section. While, 2 patients were diagnosed as coagulation failure as evidenced by marked raise of prothrombin time and serum fibrin degradation product (FDP) (Table-4).
|
Causes of PPH |
Frequency (n) |
Percentage (%) |
|
Uterine atony |
52 |
52 |
|
Genital tract trauma |
18 |
18 |
|
Retained placenta |
16 |
16 |
|
Retained bits of placental tissue/membrane |
8 |
8 |
|
Uterine rupture |
2 |
2 |
|
Placenta accrete |
1 |
1 |
|
Uterine inversion |
1 |
1 |
|
Coagulation disorder |
2 |
2 |
|
Total |
100 |
100 |
Table 4: Various causes of PPH among the study patients (N= 100).
Regarding clinical presentations; most of the patients (90%) were presented with primary PPH and 8% cases were secondary PPH. One (1%) patient presented PPH with shock and 1% patient presented PPH with renal failure (Table- 5).
|
Clinical presentations |
Frequency (n) |
Percentage (%) |
|
Primary PPH |
90 |
90 |
|
Secondary PPH |
8 |
8 |
|
PPH with Shock |
1 |
1 |
|
PPH with renal failure |
1 |
1 |
|
Total |
100 |
100 |
Table 5: Clinical presentations of the study patients (N= 100)
Among 100 study patients, blood transfusion was required in 90 (90%) cases. Out of 90 patients; 10 (20%) patients required 1 unit blood transfusion, 40 (44.44%) patients required 2 units blood transfusion, 30 (33.33%) patients required 3 units blood transfusion and 10 (20%) patients required massive blood transfusion (>4 units) (Table- 6).
|
Number of unit needed |
Frequency (n) |
Percentage (%) |
|
1 unit |
10 |
11.11 |
|
2 units |
40 |
44.44 |
|
3 units |
30 |
33.33 |
|
>4 units or massive transfusion |
10 |
11.11 |
Table 6: Number of patients required blood transfusion (n= 90)
In this study among the 100 PPH cases; 44 (44%) cases were treated by conservative medical management, 51 (51%) cases were managed by minor surgical procedure and only 5 (5%) cases needed major surgical intervention (Table- 7).
|
Management/procedure |
Frequency (n) |
Percentage (%) |
|
Conservative/medical treatment |
44 |
44 |
|
Minor surgical management |
51 |
51 |
|
Intrauterine inflation of balloon Catheter |
9 |
9 |
|
Exploration of uterus |
8 |
8 |
|
Manual removal of placenta |
16 |
16 |
|
Repair of the perineal tear |
10 |
10 |
|
Repair of the cervical tear |
8 |
8 |
|
Major surgical management |
5 |
5 |
|
B-lynch brace suture |
1 |
1 |
|
Bilateral uterine arteries ligation |
1 |
1 |
|
Repair of ruptured uterus |
1 |
1 |
|
Subtotal hysterectomy following ruptured uterus |
1 |
1 |
|
Caesarean hysterectomy |
1 |
1 |
Table 7: Mode of treatment of PPH among the study patients (N= 100)
Analyzing the outcomes of the study patients following PPH management revealed that most of the patients (94%) were discharged without any complication. Only 6% of cases developed various complications; of them 1 patient developed sepsis, 2 patients had transfusion reaction, 1 patient developed renal failure and 2 patients had died- 1 due to cardiac arrest following hazards of general anesthesia (G/A) and another 1 was died due to irreversible shock following PPH (Table- 8).
|
Complications |
Frequency (n) |
Percentage (%) |
|
Sepsis |
1 |
1 |
|
Transfusion reaction |
2 |
2 |
|
Anesthetics complication (cardiac arrest) |
1 |
1 |
|
Renal failure |
1 |
1 |
|
Irreversible shock |
1 |
1 |
Table 8: Number of patient developed complications following PPH management
4. Discussion
Postpartum haemorrhage (PPH) is associated with increased risk of maternal mortality. This study was conducted to assess the clinical presentation and management of PPH among hospitalized patients. This prospective observational study was conducted at Obstetrics and Gynaecology Department of Dhaka Medical College Hospital (DMCH), Dhaka, Bangladesh which is one of the largest tertiary care hospitals in the country where a large number of patients particularly from lower socio-economic condition seek admission for management. The duration of the study was one year. A total of 100 patients were randomly selected who admitted in the obstetric ward, DMCH with postpartum haemorrhage (PPH). This study observed the current situation of PPH at a tertiary care hospital in Bangladesh. The results of this study might help to build up the public awareness as well as proper management of PPH and reduce maternal mortality in Bangladesh. It also helps our decision makers and healthcare providers to take necessary steps.
The mean age of the study patients was 25±4.50 years where around 24% were within 20 years old. Majority of the patients (36%) were in between 25-30 years. Only 2% were aged above 35 years. These results were consistent with related previous studies[10-11]. In this study, only 14% of the patients were primigravida and majority (58%) of the patients had 2-4 child and 28% were grandmultipara. One previous study showed 58% were multiparous which was similar with this study[10]. Regarding the antenatal care; only 19 (19%) had history of regular and proper antenatal care (ANC), rest 81 (81%) study patients had no history of took any antenatal care at all. A previous study showed 26% had history of antenatal care and 74% had no antenatal care which was similar to this current study[10].
In this study we found that, most of the deliveries took place at home (80%). Previous studies showed 50% home deliveries and 30% hospital deliveries developed PPH[10, 12-13]. Which were not similar to our study, it was reported that PPH following home delivery is higher[12-14]. The low percentage of PPH among hospital deliveries could be due to active management of third stage of labour.
This present study showed that PPH developed following 84% of vaginal delivery, 8% of caesarean (LUCS) deliveries and 6% of instrumental delivery. Another related study found; 64.63% cases of PPH occurred after vaginal delivery, 23.17% cases of PPH occurred after instrumental delivery and 12.20% cases of PPH occurred after caesarean section[15]. These findings were almost similar to our study, therefore it could be documented that percentage of PPH following vaginal delivery was more than caesarean delivery.
This study showed that, association of some maternal risk factors related with postpartum haemorrhage (PPH). We found; 13% of the study patients had prolonged labour, 10% had pre-eclampsia and eclampsia, prolonged 3rd stage of labour in 9% of study cases, 6% had ante partum haemorrhage (APH) and 2% had multiple pregnancies. In this series; another study showed 15% had pre-eclampsia and eclampsia, 2.5% had multiple pregnancies, 7.5% had ante partum haemorrhage (APH), prolonged 3rd stage of labour was in 8% of cases which were nearly similar with this current study[16].
In this study majority of the study patients were admitted in hospital with primary PPH (92%), only 8% was admitted with secondary PPH. This result was comparable with a couple of previous studies[14-15].
Data analysis revealed that, the most common causes of PPH were- uterine atony (52%) followed by genital tract trauma (18%), retained placenta (16%) and retained bits of placenta tissue/membrane (8%). These observations were supported by previous studies[12-14]. In this study 90 patients required blood transfusion. Among them 80 patients needed 1-3 units blood transfusion and 10 patients required massive (>4 units) units blood transfusion. This finding was supported by similar previous studies [13-14]. Present study showed that among 100 PPH cases; 44 (44%) cases were managed by conservative medical treatment, 51 (51%) cases were managed by minor surgical procedure and only 5 (5%) cases needed major surgical intervention. These results were in a line of similar previous studies[10, 17-18].
In this present study most of the patients (94%) were discharged without any complications. Only 6 (6%) of the study cases were developed various complications like- shock (1%), sepsis (1%), transfusion reaction (2%), renal failure (1%) and cardiac arrest following GA (1%). Two (2%) patients had died out of 100 study patients, among them one patient had died following cardiac arrest due to hazards of general anesthesia (G/A) and another one had died due to irreversible shock following massive haemorrhage. These findings were consistent with a related previous study[11].
4. Conclusion
This study demonstrated that, 92% patients present with primary PPH and 55 % of the patients had no detectable risk factors. Regarding management; medical treatment and surgical management were found almost equal; 44% patients were managed by conservative medical treatment and 56% patients required surgical intervention. Therefore it has been revealed that without any risk factors patient may develop PPH, both surgical and conservative medical management have equal important role. Better maternal outcome could be ensured by proper management of PPH at proper time. All patients with risk factors, their delivery should be conducted in a well-equipped hospital.
Limitation of the study
It was a single center study with a relatively small sample size that doesn’t reflect the actual situation in the total population of the country.
Recommendation
All pregnant women should include in ante natal care (ANC) coverage to screen out the risk and ensure safe delivery. Each and every delivery should be conducted by trained persons as because proper conducted delivery can significantly reduce PPH. Further large scale population based studies should be done.
Conflicts of interest
All authors declared that they have no conflict of interest regarding this publication.
REFERENCES
- Drife J. Management of primary postpartum haemorrhage. British journal of obstetrics and gynaecology 104 (1997): 275-277.
- Prata N, Gerdts C. Measurement of postpartum blood loss. Bmj 1 (2010): 340.
- Brant HA. Precise estimation of postpartum haemorrhage: difficulties and importance. British Medical Journal 1 (1967): 398.
- Callaghan WM, Kuklina EV, Berg CJ. Trends in postpartum hemorrhage: United States, 1994–2006. American journal of obstetrics and gynecology 202 (2010): 353-e1.
- Khatun F, Rasheed S, Moran AC, et al. Causes of neonatal and maternal deaths in Dhaka slums: implications for service delivery. BMC Public Health 12 (2012): 1-9.
- Ripley DL. Uterine emergencies: atony, inversion, and rupture. Obstetrics and gynecology clinics of North America 26 (1999): 419-434.
- Stones RW, Paterson CM, Saunders NJ. Risk factors for major obstetric haemorrhage. European Journal of Obstetrics & Gynecology and Reproductive Biology 48 (1993): 15-18.
- Sert M, Tetiker T, Kirim S, et al. Clinical report of 28 patients with Sheehan’s syndrome. Endocrine journal. 2003; 50(3): 297-301.
- Mc Donald SJ, Prendiville WJ, Blair E. Randomised controlled trial of oxytocin alone versus oxytocin and ergometrine in active management of third stage of labour. British Medical Journal 307 (1993): 1167-1171.
- Akhter S, Begum MR, Kabir Z, et al. Use of a condom to control massive postpartum hemorrhage. MedGenMed: Medscape general medicine 11; 5(2003): 38-40.
- Reyal F, Deffarges J, Luton D, et al. Severe post-partum hemorrhage: descriptive study at the Robert-Debre Hospital maternity ward. Journal de Gynecologie, Obstetrique et Biologie de la Reproduction 31 (2002): 358-364.
- Tsu VD. Postpartum haemorrhage in Zimbabwe: a risk factor analysis. BJOG: An International Journal of Obstetrics & Gynaecology 100 (1993): 327-333.
- Combs CA, Murphy EL, Laros Jr RK. Factors associated with postpartum hemorrhage with vaginal birth. Obstetrics & Gynecology 77 (1991): 69-76.
- Shaheen B, Hassan L. Postpartum haemorrhage: a preventable cause of maternal mortality. Journal of the College of Physicians and Surgeons--pakistan: JCPSP 17 (2007): 607-610.
- Brinsden P R, Clark A D. Postpartum haemorrhage after induced and spontaneous labour. Br Med J 2 (1978): 855-856.
- Goodburn EA, Gazi R, Chowdhury M. Beliefs and practices regarding delivery and postpartum maternal morbidity in rural Bangladesh. Studies in family planning (1995): 22-32.
- AbdRabbo SA. Stepwise uterine devascularization: a novel technique for management of uncontrollable postpartum hemorrhage with preservation of the uterus. American journal of obstetrics and gynecology 171(1994): 694-700.
- Cengiz H, Yasar L, Ekin M, et al. Management of intractable postpartum haemorrhage in a tertiary center: A 5-year experience. Nigerian medical journal: journal of the Nigeria Medical Association 53 (2012): 85.
