The Application of Proximal Splenic Vein Ligation to Prevent Portal Vein Thrombosis in Laparoscopic Splenectomy Plus Pericardial Devascularization Surgery
Article Information
Kai Jiang*, Weiding Wu, Yuanbiao Zhang, Hongguo Yang, Zhiming Hu
Department of hepatobiliary and pancreatic surgery and Minimally invasive surgery, Zhejiang provincial people’s hospital, Hangzhou, Zhejiang, China
*Corresponding Author: Kai Jiang, Department of hepatobiliary and pancreatic surgery and Minimally invasive surgery, Zhejiang provincial people’s hospital, Shangtang Road 158#, Hangzhou, Zhejiang, China
Citation: Kai Jiang, Weiding Wu, Yuanbiao Zhang, Hongguo Yang, Zhiming Hu. The Application of Proximal Splenic Vein Ligation to Prevent Portal Vein Thrombosis in Laparoscopic Splenectomy Plus Pericardial Devascularization Surgery. Journal of Surgery and Research 2 (2019): 132-138.
View / Download Pdf Share at FacebookAbstract
Objective: To investigate the application of proximal splenic vein (SV) ligation in laparoscopic splenectomy plus pericardial devascularization (LSPD) surgery.
Methods: From January 2017 to December 2018, 31 patients with portal hypertension of liver cirrhosis in Zhejiang Provincial people’s Hospital were treated with LSPD surgery with the ligation of proximal SV.
Results: All the 31 patients were performed without any transfer to open operation. The operation time were 139.35 ± 19.48 min, blood loss were 138.06 ± 54.49 ml. Postoperative hospital stay (PHS) was 8.26 ± 1.59 days. There were 4 patients with postoperative portal vein thrombosis (PVT), among them 2 patients were degree I and 2 patients were degree II. There are no severe postoperative PVT cases. There were no abdominal infection, no pancreatic leakage, no abdominal hemorrhage, no liver failure or no upper gastrointestinal bleeding cases.
Conclusion: LSPD combined with ligation of proximal SV is safe and feasible, and short-term follow-up can effectively prevent the formation of PVT after operation.
Keywords
Proximal splenic vein ligation, Portal vein thrombosis, Laparoscopic splenectomy plus pericardial devascularizationl, Portal hypertension
Proximal splenic vein ligation articles, Portal vein thrombosis articles, Laparoscopic splenectomy plus pericardial devascularization articles, Portal hypertension articles
Proximal splenic vein ligation articles Proximal splenic vein ligation Research articles Proximal splenic vein ligation review articles Proximal splenic vein ligation PubMed articles Proximal splenic vein ligation PubMed Central articles Proximal splenic vein ligation 2023 articles Proximal splenic vein ligation 2024 articles Proximal splenic vein ligation Scopus articles Proximal splenic vein ligation impact factor journals Proximal splenic vein ligation Scopus journals Proximal splenic vein ligation PubMed journals Proximal splenic vein ligation medical journals Proximal splenic vein ligation free journals Proximal splenic vein ligation best journals Proximal splenic vein ligation top journals Proximal splenic vein ligation free medical journals Proximal splenic vein ligation famous journals Proximal splenic vein ligation Google Scholar indexed journals Portal vein thrombosis articles Portal vein thrombosis Research articles Portal vein thrombosis review articles Portal vein thrombosis PubMed articles Portal vein thrombosis PubMed Central articles Portal vein thrombosis 2023 articles Portal vein thrombosis 2024 articles Portal vein thrombosis Scopus articles Portal vein thrombosis impact factor journals Portal vein thrombosis Scopus journals Portal vein thrombosis PubMed journals Portal vein thrombosis medical journals Portal vein thrombosis free journals Portal vein thrombosis best journals Portal vein thrombosis top journals Portal vein thrombosis free medical journals Portal vein thrombosis famous journals Portal vein thrombosis Google Scholar indexed journals Laparoscopic splenectomy plus pericardial devascularizationl articles Laparoscopic splenectomy plus pericardial devascularizationl Research articles Laparoscopic splenectomy plus pericardial devascularizationl review articles Laparoscopic splenectomy plus pericardial devascularizationl PubMed articles Laparoscopic splenectomy plus pericardial devascularizationl PubMed Central articles Laparoscopic splenectomy plus pericardial devascularizationl 2023 articles Laparoscopic splenectomy plus pericardial devascularizationl 2024 articles Laparoscopic splenectomy plus pericardial devascularizationl Scopus articles Laparoscopic splenectomy plus pericardial devascularizationl impact factor journals Laparoscopic splenectomy plus pericardial devascularizationl Scopus journals Laparoscopic splenectomy plus pericardial devascularizationl PubMed journals Laparoscopic splenectomy plus pericardial devascularizationl medical journals Laparoscopic splenectomy plus pericardial devascularizationl free journals Laparoscopic splenectomy plus pericardial devascularizationl best journals Laparoscopic splenectomy plus pericardial devascularizationl top journals Laparoscopic splenectomy plus pericardial devascularizationl free medical journals Laparoscopic splenectomy plus pericardial devascularizationl famous journals Laparoscopic splenectomy plus pericardial devascularizationl Google Scholar indexed journals Portal hypertension articles Portal hypertension Research articles Portal hypertension review articles Portal hypertension PubMed articles Portal hypertension PubMed Central articles Portal hypertension 2023 articles Portal hypertension 2024 articles Portal hypertension Scopus articles Portal hypertension impact factor journals Portal hypertension Scopus journals Portal hypertension PubMed journals Portal hypertension medical journals Portal hypertension free journals Portal hypertension best journals Portal hypertension top journals Portal hypertension free medical journals Portal hypertension famous journals Portal hypertension Google Scholar indexed journals portal hypertension articles portal hypertension Research articles portal hypertension review articles portal hypertension PubMed articles portal hypertension PubMed Central articles portal hypertension 2023 articles portal hypertension 2024 articles portal hypertension Scopus articles portal hypertension impact factor journals portal hypertension Scopus journals portal hypertension PubMed journals portal hypertension medical journals portal hypertension free journals portal hypertension best journals portal hypertension top journals portal hypertension free medical journals portal hypertension famous journals portal hypertension Google Scholar indexed journals liver cirrhosis articles liver cirrhosis Research articles liver cirrhosis review articles liver cirrhosis PubMed articles liver cirrhosis PubMed Central articles liver cirrhosis 2023 articles liver cirrhosis 2024 articles liver cirrhosis Scopus articles liver cirrhosis impact factor journals liver cirrhosis Scopus journals liver cirrhosis PubMed journals liver cirrhosis medical journals liver cirrhosis free journals liver cirrhosis best journals liver cirrhosis top journals liver cirrhosis free medical journals liver cirrhosis famous journals liver cirrhosis Google Scholar indexed journals splenic pedicle articles splenic pedicle Research articles splenic pedicle review articles splenic pedicle PubMed articles splenic pedicle PubMed Central articles splenic pedicle 2023 articles splenic pedicle 2024 articles splenic pedicle Scopus articles splenic pedicle impact factor journals splenic pedicle Scopus journals splenic pedicle PubMed journals splenic pedicle medical journals splenic pedicle free journals splenic pedicle best journals splenic pedicle top journals splenic pedicle free medical journals splenic pedicle famous journals splenic pedicle Google Scholar indexed journals Laparoscopic splenectomy articles Laparoscopic splenectomy Research articles Laparoscopic splenectomy review articles Laparoscopic splenectomy PubMed articles Laparoscopic splenectomy PubMed Central articles Laparoscopic splenectomy 2023 articles Laparoscopic splenectomy 2024 articles Laparoscopic splenectomy Scopus articles Laparoscopic splenectomy impact factor journals Laparoscopic splenectomy Scopus journals Laparoscopic splenectomy PubMed journals Laparoscopic splenectomy medical journals Laparoscopic splenectomy free journals Laparoscopic splenectomy best journals Laparoscopic splenectomy top journals Laparoscopic splenectomy free medical journals Laparoscopic splenectomy famous journals Laparoscopic splenectomy Google Scholar indexed journals Pericardial Devascularization Surgery articles Pericardial Devascularization Surgery Research articles Pericardial Devascularization Surgery review articles Pericardial Devascularization Surgery PubMed articles Pericardial Devascularization Surgery PubMed Central articles Pericardial Devascularization Surgery 2023 articles Pericardial Devascularization Surgery 2024 articles Pericardial Devascularization Surgery Scopus articles Pericardial Devascularization Surgery impact factor journals Pericardial Devascularization Surgery Scopus journals Pericardial Devascularization Surgery PubMed journals Pericardial Devascularization Surgery medical journals Pericardial Devascularization Surgery free journals Pericardial Devascularization Surgery best journals Pericardial Devascularization Surgery top journals Pericardial Devascularization Surgery free medical journals Pericardial Devascularization Surgery famous journals Pericardial Devascularization Surgery Google Scholar indexed journals
Article Details
1. Introduction
PVT is one of the most serious complication after LSPD [1, 2]. In patients with portal hypertension, most paper shows the incidence of PVT after LSPD is as high as 22.3% to 37.5%, some paper even reports the incidence rate of PVT after LSPD is higher than 50% [3, 4], which will cause a further increase in portal venous pressure, and will increase the rate of rebleeding of esophageal and gastric varices after LSPD surgery, and the difficulty of liver transplantation if necessary. Several systemic and local risk factors for PVT after LSPD have been identified. Systemic diseases include lymphoma [4], hemolytic disease [5, 6] and myeloproliferative disorders [5]. Local risk factors are mainly related to spleen characteristics such as splenomegaly [3, 4], preoperative SV diameter [2], splenic weight [2, 4-8], and splenic length [9], etc. However, the specific mechanisms of the development of PVT after splenectomy remain under investigation.
Among them, splenic vein thrombosis (SVT), which is an important factor leads to PVT. PVT is often attributed to the spread of SVT [6-7]. How to effectively prevent the forming of PVT after LSPD is the focus of clinical research [3-5]. The distal side of SV was blind after splenectomy, the blood flow velocity decreased sharply and formed turbulence, ligation and suture of splenic pedicle caused the injury of SV endomembrane, all of which will cause the SVT. The incidence of SVT is extremely high in clinical observation, and the occurance rate has been reported to be more than 90% in some paper [9-11]. How to block SVT to spread to superior mesenteric vein (SMV) or portal vein (PV) trunk may be a research direction to prevent PVT after LSPD operation. The authors carried out LSPD for more than 10 years. The number of cases were more than 200. The procedure was simplified and standardized, and the improved four-step method was summarized [12, 13]. In order to decrease the incidence of postoperative PVT, based on previous work, we have innovatively applied laparoscopic splenectomy with proximal SV ligation. We performed this technique in recent 31 cases of LSPD. The results of short-term follow-up have been satisfactory, and the report is as follows.
2. Data and Methods
2.1 Clinical data
General data from January 2017 to December 2018, 31 patients with posthepatitic cirrhosis associated with hypersplenism due to portal hypertension underwent LSPD with the ligation of proximal SV, all of whom 18 patients were male, 13 patients were female, aged 51.87 ± 7.11 years. Child-Pugh grade of liver function 21 pateints were grade A, 10 patients were grade B, no Child-Pugh grade C, preoperative ICG R15 were 15.68 ± 19.27. 24 cases with moderate hypersplenism and 7 cases with severe hypersplenism were assessed by CT or MR before operation. All patients and their families signed informed consent. Indications: Patients generally in good condition, no serious heart, kidney, lung and other important organic diseases. Preoperative diagnosis: cirrhosis, portal hypertension, severe esophageal and gastric varices, hypersplenism. Grade A or B of liver function. Any of the following is LSPD indication: (1) the portal hypertension caused by various causes and has a history of esophageal and gastric variceal bleeding, and there is portal blood flow to the liver; (2) there was no history of gastrointestinal bleeding, cirrhosis, but hypersplenism with severe varicose veins, positive red sign.
2.2 Operation method
- Anesthesia and posture: general anesthesia with endotracheal intubation, supine position, routine sterilized on abdominal skin.
- Incision and trocar placement: 1 cm incision was made on the navel, pneumoperitoneum (pneumoperitoneum pressure 10-14 mmHg) was established by pneumoperitoneum puncture, 10 mm Trocar was inserted as the observation hole. 30° laparoscopy was inserted to explore the whole abdominal cavity, and the reversed Trendelenburg position was setted, the head and left side were raised about 30° respectively. A 5 mm Trocar was inserted at the centerpoint of the xiphoid process and the umbilical cord under the direct vision. Another two trocars are placed at the upper left side of the abdomin.
- The left gastrocolonic ligament was amputated by ultrasonic knife to the splenogastric ligament.
- Open the lesser omentum sac and pull the gastric body to the upper right side with the catheter on the right side of the gastric coronal vein. exposing the pancreas surface and the superior edge.
- According to the pulsation of the splenic artery at the superior edge of the pancreas, the splenic artery was isolated and clamped with Hem-o-Lock (Figure 1).
- The splenic colon ligament, splenogastric ligament were cutted by ultrasonic knife and the splenic and renal ligaments were dissociated to establish the posterior splenic tunnel (Figure 2).
- A stapler (Endo-GIA) was placed through the tunnel to divide the secondary splenic pedicle (Figure 3) Then transfer the excised spleen to the pelvic cavity. Insert another stapler (Endo-GIA) to disconnect the gastric coronary venous mass (Figure 4), and use an ultrasound knife or LigaSure to disconnect the periesophageal vessels to the lower esophagus 6-8 cm.
- Cut the posterior peritoneum along the lower part of the neck of the pancreas, separate the posterior side of the neck of the pancreas, separate the SV and separate it to the right side to the confluence of the SV and the SMV, and use the 3-0 Vioryl suture knot at a certain distance from the left side of the confluence. (length of ligation point is 1/2 width of SV), SV is clipped with Hem-o-Lock on left side of ligation.
- Take out the spleen and place the drainage tube in the splenic fossa.
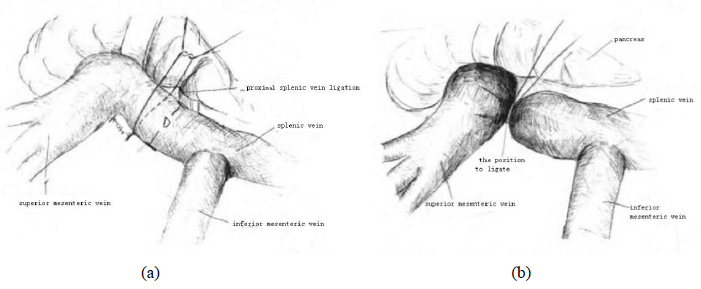
Figure 1: (a) and (b) The ligation position of proximal splenic vein.
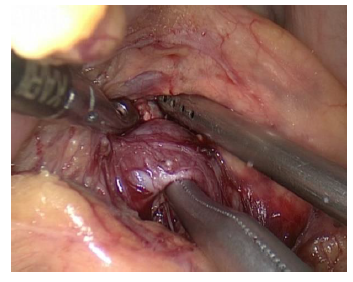
Figure 2: Free exposure of splenic vein (A: splenic vein).
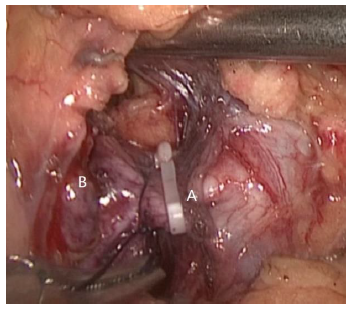
Figure 3: Ligation of splenic vein (A: splenic vein B: superior mesenteric vein).
2.3 Postoperative treatment
Absolute diet, gastrointestinal decompression, liver protection, infusion of plasma, albumin and diuretic treatment. No hemostatic. On the second day after operation, the gastric tube was removed, take liquid diet, the drainage volume and amylase value of the drainage fluid were monitored, and the changes of hemoglobin, platelet and liver function were monitored. Aspirin was taken 3 days after surgery (100 mg, once a day). All patients underwent a CT scan with contrast enhancement at POD 6 ± 1.
3. Results
All the 31 patients were successfully performed without hand assistant or converted to open laparotomy. The operation time were 139.35 ± 19.48 min, blood loss were 138.06 ± 54.49 ml. PHS was 8.26 ± 1.59 days. There were 4 patient occurred postoperative PVT, among them 2 patients were degree I and 2 patients were degree II. There are no severe postoperative PVT cases. There were no postoperative cases of abdominal infection, pancreatic leakage, abdominal hemorrhage, liver failure and upper gastrointestinal bleeding. At 1 and 6 months after operation, there were no PVT found by color Doppler ultrasonography and enhanced CT in the other 27 patients.
4. Discussion
Surgery is still the major method for the treatment of portal hypertension. Excision of pericardial blood vessels with giant spleen is one of the main methods. Laparoscopic technique has been widely used in portal hypertension surgery in recent years. The popularization and application of LSPD should do more studies in clinic. The author's team improved the technique of spleen subpedicle severance, which was summarized as improved four-step method [12], that is, the splenic artery was ligated in advance, the splenic pedicle tunnel was established, the splenic pedicle was cut off by the stapler, and the gastric coronal vein was cut off by the stapler. The success rate of operation was improved significantly, the blood loss was reduced, the postoperative recovery was accelerated, and the PHS was shortened.
Postoperative PVT is a common complication of LSPD, which seriously affects the prognosis of patients, and sometimes will be a major problem of liver transplantation. PVT was retrospectively graded according to the operative findings: Grade 1: <50% PVT minimal obstruction of the SMV; Grade 2: grade 1 but >50% PVT; Grade 3: complete PV and proximal SMV thrombosis; Grade 4: complete PV and entire SMV thrombosis. There were often no symptoms of PVT when PVT is grade 1 and grade 2. An unknown cause of fever (>38) or unexplained abdominal pain after the splenectomy was suspected of SVT. The wide and rapid formation of PVT including the SMV and the inferior mesenteric vein (IMV), may completely block the venous return, which may cause the mesenteric artery to contract and cramp, causing a life-threatening complication, including intestinal ischemia, intestinal infarction, peritonitis or with fulminant infections, blood stool, fever, acute ascites, metabolic acidosis and multiple organ failure.
The mechanism of the formation of the PVT is complicated. The present studies showed that the changes of platelet count, the changes of coagulation factors and the changes in portal and splenic venous blood flow may be associated with the formation of the PVT after splenectomy [1-2]. Among them, SVT, which is an important factor leads to PVT. PVT is often attributed to the spread of SVT [4-5, 14]. Johns Hopkins’ Broe [15] proposed that ligating SV at the left side of inferior mesenteric vein during splenectomy surgery could effectively reduce the formation of PVT. He thinks ligation at this point could reduce the length of the blind end of SV and may prevent the forming of SVT. We believe that the ligation at the left side of inferior mesenteric vein could cut off the spread of SVT at the blind end, but since there is only blood flow from the IMV, the blood flow in the proximal SV decreases dramatically, while the SV is much wider than IMV, and the velocity of the blood flow in the SV drops sharply. The formation of turbulence, can also cause thrombosis. We propose an operational method that ligation at the confluence of SV and SMV, the thrombosis from the blind end of SV can be isolated effectively. When we take this step, there is small collateral vessels at the proximal SV, so it is easy to dissociate SV at this point from the posterior of the pancreas, and laparoscopic operation has even more advantageous. Our clinical practice also showed that the procedure of ligation at the proximal of the SV only took 10 to 15 minutes, which was quite safe and feasible, without additional bleeding, pancreatic injury or other complications.
On the basis of routine operation of more than 200 cases of LSPD [12-13], we took this new technique on 31 cases of LSPD. Six months follow-up demonstrated that there were 4 patients with postoperative PVT, among them 2 patients were grade I and 2 patients were grade II. There were no grade III or grade IV postoperative PVT after surgery and there were no severe complications in those 4 cases. We think the key point of the operation is the proper ligation location. Too far away from the PV may cause some SV to become the new blind end and develop thrombosis. Our experience considered the length of the ligation point from the confluence is 1/2 the width of the SV. After ligation, the splenic venous wall becomes part of the portal venous wall, which could effectively reduce the distortion and stenosis of the PV (Figures 1-4). The application of proximal SV ligation could not only reduce the formation of PVT but also block the spread of SV, which could effectively reduce the incidence of PVT.
In conclusion, LSPD combined with proximal SV ligation is safe and feasible, and short-term follow-up showed this method could effectively prevent PVT after operation. We believe that this technique can be more applied in clinic. However, the number of cases is still accumulating, and the occurrence of PVT is related to many factors, the long-term effect needs to be further observed and more confirmation.
References
- Rattner DW, Ellman L, Warshaw AL. Portal vein thrombosis after elective splenectomy. An underappreciated, poten tially lethal syndrome. Arch Surg 128 (1993): 565-569.
- Danno K, Ikeda M, Sekimoto M, et al. Diameter of splenic vein is a risk factor for portal or splenic vein thrombosis after laparoscopic splenectomy. Surgery 145 (2009): 457-464.
- Ikeda M, Sekimoto M, Takiguchi S, et al. High incidence of thrombosis of the portal venous system after laparoscopic splenectomy: a prospective study with contrast-enhanced CT scan. Ann Surg 241 (2005): 208-216.
- De’Angelis N, Abdalla S, Lizzi V, et al. Incidence and predictors of portal and splenic vein thrombosis after pure laparoscopic splenectomy. Surgery 162 (2017): 1219-1230.
- Manouchehri N, Kaneva P, Seguin C, et al. Screening for thrombophilia does not identify patients at risk of portal or splenic vein thrombosis following laparoscopic splenectomy. Surg Endosc 30 (2016): 2119-2126.
- Bouvier A, Gout M, Audia S, et al. Routine screening of splenic or portal vein thrombosis after splenectomy. Rev Med Interne 38 (2017): 3-7.
- Romano F, Caprotti R, Conti M, et al. Thrombosis of the splenoportal axis after splenectomy. Langenbecks Arch Surg 391 (2006): 483-488.
- Lu Shaocheng, Gu Wanqing. Progress in Prevention and treatment of posterior Venous Thrombosis in patients with liver Cirrhosis after splenectomy [J]. Chinese Journal of Hepatobiliary surgery 21 (2015): 59-63.
- Kuroki T, Kitasato A, Tokunaga T, et al. Predictors of portal and splenic vein thrombosis after laparoscopic splenectomy: a retrospective analysis of a single-center experience. Surg Today 48 (2018): 804-809.
- Wang Mancai, Tian Bin, Wang Gennian, et al. Meta analysis of factors related to venous thrombosis after splenectomy for cirrhosis [J]. Chinese Journal of Hepatobiliary surgery 20 (2014): 855-861.
- Han Jianbo, Yi Yongxiang, Ding Hai, et al. Preoperative risk factors of portal vein thrombosis after splenectomy in patients with portal hypertension [J]. Chinese Journal of Hepatology 22 (2014): 739-743.
- Cheng Jian, Hong Defei, Shen Guoliang, et al. Optimization of laparoscopic splenectomy and pericardial devascularization [J]. Chinese Journal of General surgery 29 (2014): 165-167.
- Wu Wei Dingding, Hu Zhiming, Zhang Chengwu, et al. Application of left paraspinal anterior space approach in splenic preserving laparoscopic pancreatectomy [J]. Chinese Journal of Hepatobiliary surgery 20 (2014): 35-38.
- Zhang N, Yao Y, Xue W, et al. Early prophylactic anticoagulation for portal vein system thrombosis after splenectomy: a systemic review and meta-analysis. Biomed Rep 5 (2016): 483-490.
- Broe PJ, Conley CL, Cameron JL. Thrombosis of the portal vein following splenectomy for myeloid metaplasia [J]. Surg Gynecol Obstet 152 (1981): 488-492.
