The 2021 Cholera Outbreak in West Africa: Epidemiology and Public Health Implications
Article Information
Vincent Dossou Sodjinou1*, Ambrose Talisuna2, Fiona Braka2, Phillipe Barboza3, Kathryn Alberti3, Ann FORTIN2, Walter Mulombo Kazadi4, Blanche-philomene Melanga Anya5, Mamoudou Harouna Djingarey6, Binta Fatoumata Diallo7, Adebola Olayinka4, Bienvenu Baruani5, Jean Paul Kimenyi2, Didier Tambwe5, Mory Keita1, Guy Mbayo2, Inès Gbedande Cica Tosse5, Nicole Mbarga8, Nannie Ishata Conteh2, Christian Emmanuel Douba Epee8, Geoffrey Namara4, Sonia Viviane Bedie6, Salam Abdou GUEYE2
1World Health Organization – Dakar Emergency Preparedness and Response Hub, BP 4039 Dakar, Senegal, West Africa
2World Health Organization Regional Office for Africa – Emergency Preparedness and Response cluster, BP06, Brazzaville, Congo, Central Africa
3World Health Organization-Head Quarter Cholera programme on behel of the Global Task Force on Cholera Control
4WHO country Office Nigeria, 910006 Abuja, Nigeria
5World Health Organization Country Office Niger, BP 10 739 Niamey, Niger, West Africa
6World Health Organization Country Office Benin, 01BP918 Cotonou, Benin, West Africa
7World Health Organization Country Office Togo, BP 1504, Lomé, Togo, West Africa
8World Health Organization Country Office, B.P. 155 Yaoundé, Cameroon
*Corresponding author: Vincent Dossou SODJINOU, World Health Organization – Dakar Emergency Preparedness and Response Hub, BP 4039 Dakar, Senegal.
Received: 28 February 2022; Accepted: 08 March 2022; Published: 16 March 2022
Citation:
Vincent Dossou Sodjinou, Ambrose Talisuna, Fiona Braka, Phillipe Barboza, Kathryn Alberti, Ann FORTIN, Walter Mulombo Kazadi, Blanche-philomene Melanga Anya, Mamoudou Harouna Djingarey, Binta Fatoumata Diallo, Adebola Olayinka, Bienvenu Baruani, Jean Paul Kimenyi, Didier Tambwe, Mory Keita, Guy Mbayo, Inès Gbedande Cica Tosse, Nicole Mbarga, Nannie Ishata Conteh, Christian Emmanuel Douba Epee, Geoffrey Namara, Sonia Viviane Bedie, Salam Abdou GUEYE. The 2021 cholera outbreak in West Africa: epidemiology and public health implications. Archives of Clinical and Biomedical Research 6 (2022): 296-307.
View / Download Pdf Share at FacebookAbstract
Introduction: Cholera is one of the most frequent public health emergencies in Sub Saharan Africa. The disease is targeted for elimination by the World Health Organization and the Global Task Force on Cholera Control.
Objective: This study describes the 2021 cholera outbreaks in West Africa and determines their public health implication.
Method: This was a descriptive cross-sectional study. Non-probability method and exhaustive choice of all countries affected by cholera outbreaks in West Africa in 2021 were performed. Data were collected using line-lists, situation reports, meeting and workshops reports.
Results: A total of 108,859 cases and 3,711 deaths (case fatality ratio of 3.4%) were reported from 4 January 2021 to 14 November 2021 in seven countries. The outbreak started on 12 December 2020 in Delta State, Nigeria and was reported later in Benin, Burkina Faso, Cameroon, Mali, Niger and Togo. The global attack rate was 355.7 per 1,000,000 inhabitants and was ranged to 527.2 per 1,000,000 inhabitants in Nigeria. Nigeria was the most affected country with 95% of cases followed by Niger Republic. The outbreak affected 89% of States in Nigeria, 88% of regions in Niger and 58% of departments in Benin. People above 15 years were the most affected (59%) while the under-five accounted for 26% of cases. The sex ratio Female / Male was 1.01 but more deaths were reported within male. The case fatality ratio ranged to 38.5% in Mali. Six countries out of 7 had a case fatality rate above 2%. Low access to safe water and proper sanitation, cross border movements and inadequate behaviors were the main predisposing factors. The magnitude of the outbreaks is unprecedented. The outbreaks were laboratory-confirmed in all the affected countries. Of the 1,086 stool samples col
Keywords
cholera; outbreak; West Africa
Article Details
1. Introduction
Cholera is an acute diarrheal infection caused by ingestion of food or water contaminated with the bacterium Vibrio cholerae of the serogroup O1 and O139 [1]. The World is experiencing the seventh pandemic that started in Indonesia in 1961 and reached Africa in 1970 [2]. Since then, recurrent cholera outbreaks are being reported in different subregions in Africa [3]. The burden of the disease is highest with 3,221,207 cases and 202,456 deaths reported from 1970 to 2011 [4]. Knowledge on the disease is being gradually improved and the main predisposing factors are being known. In African region, the cholera prone Member States have established cholera prevention and control programs and are coordinating the implementation of key interventions for the control of the disease. Despite these, the burden and impact of the disease is the highest especially in sub-Saharan part. At least, ten Member States are affected by cholera outbreaks each year in the World Health Organization (WHO) Region for Africa since decades [5]. West Africa countries are annually affected by cholera outbreaks. The disease is evolving on endemic mode in some settings and on epidemic mode in other settings. The occurrence of the disease is being driven by known predisposing factors. Cholera mostly affects poor communities with low socioeconomic status. The most vulnerable populations are those residing in overcrowded areas with limited safe water and sanitation services, including unplanned mass urbanization. Displacements due to conflicts, natural disasters and extreme climatic changes are other favorable conditions for cholera outbreaks in many settings across the globe [6]. In 2017, the Global task Force on Cholera Control (GTFCC) adopted the Ending cholera: A global roadmap to 2030 aiming at reducing the global cholera deaths by 90% and eliminate the disease in 20 countries by 2030 [7]. WHO is hosting the secretariat of the GTFCC and is fully committed to the cholera elimination. In 2018, the 71st session of the World Health Assembly adopted the Global Strategy for cholera prevention and control [8]. In line with this resolution, the WHO African Region Member States adopted in 2018 the Regional framework for the implementation of the global strategy for cholera prevention and control 2018-2030 [6]. This framework defines clear objectives, targets, milestones and interventions for cholera prevention and control in WHO African Region. In line with the elimination framework, West Africa countries are implementing planned interventions for cholera preparedness and response. Multisectorial collaboration is being strengthened as well as enhanced surveillance and cross border collaboration. Despite these efforts, new cholera outbreaks were reported in the subregion since December 2020. This study describes the epidemiology of these outbreaks and determines their public health implications for cholera elimination in WHO African Region.
2. Settings
The study was conducted on West Africa countries. This subregion is comprised of 16 countries with an estimated total number of 397 million inhabitants in the year 2021. The subregion is characterized by a high mobility of the population through major routes where intense population movements are daily reported. These routes include the corridor Abidjan Lagos (Nigeria, Benin, Togo, Ghana and Côte d’Ivoire), the corridor Niamey Dakar (Niger, Burkina Faso, Mali and Senegal) and the Lake Chad basin routes (Nigeria, Niger, Cameroon and Tchad). While Cameroon and Chad are not in West Africa geographical area, they were included in the study as they have regular and frequent links with cholera outbreaks in West Africa, especially in Nigeria. The subregion is affected by humanitarian crises in many countries including the northern part of Nigeria, the south eastern part of Nigeria (Bakasi peninsula), in Niger and Burkina Faso [9]. High malnutrition rate is registered in some places especially in Sahel [10].
3. Methods
This was a cross sectional descriptive study. The targeted populations were West Africa countries where cholera outbreaks were reported as well as the Lake Chad basin countries affected. The sampling method was non-probability; and all affected countries (exhaustive choice) were included. The data on cases and deaths have been collected using standardized tools developed for the outbreak. Each health facility, Cholera Treatment Unit (CTU) or Cholera Treatment Center (CTC) had to complete the tool on Excel format and shared with the national levels. The compilation of all line-list was performed in each country and the base was regularly updated. The data inputted in each line list were also collected through active case search at community level or through community-based surveillance mechanism. Information on sample collection and laboratory results were not systematically updated in the line lists. Data on predisposing factors especially water and sanitation were also collected through document review. The data analyzed were collected from 4 January 2021 to 14 November 2021. For laboratory confirmation, stool samples are collected systematically on any suspected cases before the outbreak for laboratory confirmation. In some settings, a Rapid Diagnostic Test (RDT) was performed locally on stool samples. If the sample tested negative, the case is discarded. If the sample tested positive for RDT, the sample was sent to laboratory for culture or Polymerase Chain Reaction (PCR) test. In other settings, samples are directly sent to laboratory for confirmation. Once an outbreak is confirmed in a given geographical area, the new suspected cases were not sampled systematically but a minimum number of samples were periodically collected as per WHO recommendation for laboratory confirmation during cholera outbreaks. The main data collection technique was the exploitation of documents. The sources of information were line-lists shared by national government, situational reports disseminated by national governments, information from other sources including internet and meetings reports available at the time of the study. Information on predisposing factors were collected from different sources including internet, meeting reports and countries presentations. The minimum set of variables in the line list included the general information (reporting date, epidemiological week), patient information (patient's name, sex, age), location information (name of health district, health facility or UTC or CTC name, residence place's name), clinical information (date of diarrhea onset, symptoms, health facility visit date), laboratory information (date of lab test, test performed, Lab results), final epidemiological classification (suspected disease/confirmed/not a case), outcome (alive, dead, unknown). The case was identified using case definition. The case and outbreak definitions were based on the GTFCC field manual – response to cholera [11]. Before the outbreak is confirmed in each country, any person aged 2 years or older presenting with acute watery diarrhea and severe dehydration or dying from acute watery diarrhea was considered as a suspected cholera case. After the confirmation of the outbreak, any person presenting with or dying from acute watery diarrhea was considered as suspected cholera case. In any case, a confirmed case was defined as a suspected case with Vibrio cholerae O1 or O139 confirmed by culture or PCR. The cholera outbreak was defined by the occurrence of at least one confirmed case of cholera and evidence of local transmission [11].
4. Results
4.1.Epidemiological data
Table 1 presents key figures of the cholera outbreaks per affected country from the epidemiological week 1 (4 to 10 January 2021) to the epidemiological week 45 (week ending 14 November 2021). From 4 January to 14 November 2021, a total of 108,859 cases and 3,711 deaths were reported from seven (7) countries. The overall Case Fatality Ratio (CFR) was 3.4% and was ranged to 38.5% in Mali. According to the outbreak case definition, Burkina Faso was not affected by cholera outbreak as the two documented cases were imported cases without proof of local transmission. The national Attack Rate (AR) ranged to 527 per 1,000,000 inhabitants in Nigeria. Figure 1 presents the attack rate per second administrative levels in affected countries. Nigeria was the first country to report the outbreak in Delta State on 12 December 2020. The index case in Niger, reported on 13 March 2021, had recent history of travel and living in Sokoto States, Nigeria where cholera outbreak was ongoing. The two cases reported in Burkina were two drivers that spend days in Niamey where cholera outbreak was ongoing. The first cholera-related death reported in Gao, Mali occurred in a family that received, two days before the death, visitors from Ayorou, Niger where cholera outbreak was ongoing. The first cases in South West region in Cameroon were reported from Nigerian fishermen in Bakasi area where intense movements across borders are reported. There was no link reported between Benin and Togo outbreaks with others. A timeline of the outbreaks in affected countries is presented in (Figure 2). Several waves of cholera outbreaks were reported in Benin and Cameroon.
Table 1: Cases, death, case fatality ratio and attack rate of cholera outbreaks in West Africa, 4 January to 14 November 2021.
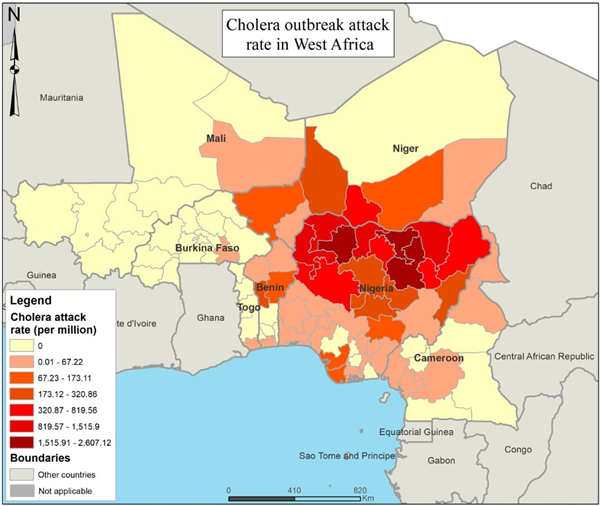
Figure 1: Map of cholera attack rate per second administrative levels in countries affected by cholera outbreaks in West Africa, 4 January 2021 to 14 November 2021.
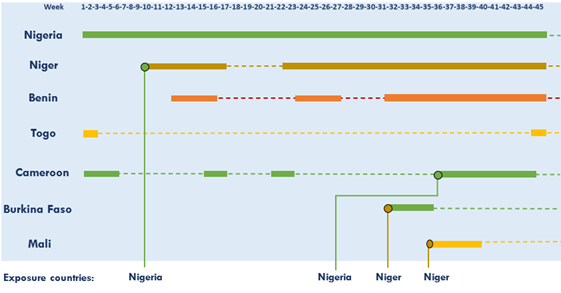
Figure 2: Timelines of cholera outbreaks in West Africa and exposure countries, Week 1 to Week 45, 2021
4.2. Lab confirmation
The outbreak was laboratory confirmed in affected second administrative level in each country. A total of 1,086 stool samples were collected and sent to reference laboratories for culture. This number represents 1.0% of reported cases. Of the samples collected, 617 tested positive leading to a positivity rate of 56.8%. The Vibrio cholerae serogroup O1 was identified in all the seven countries (Benin, Burkina Faso, Cameroon, Mali, Niger, Nigeria, Togo). The serotype Ogawa was identified in Burkina Faso, Niger and Togo while the serotype Inaba was identified in Cameroon.
4.3. Time, place, persons analysis
In terms of places, Niger and Nigeria had the highest proportion of regions / States and districts or Local Government Areas (LGA) affected (Table 1). A total of 33 States out of 37 (89%) were affected in Nigeria; seven regions out of eight (88%) were affected in Niger; eight departments out of 12 (58%) were affected in Benin, four regions in Cameroon and one region in Mali and Togo. Figure 1 presents the attack rate per States in Nigeria and per region or department in other countries. Figure 3 presents the weekly trend of cases during the outbreak. The global peak of the outbreak was reported in the week 33 (week ending 22 August 2021) with a cumulative number of 9,694 cases. The peak was reported the same week in Nigeria and Niger. The outbreaks in Benin, Cameroon and Togo were still increasing in the epidemiological week 45 and their peaks were not yet reached. Concerning the death, the overall peak was reported in the epidemiological week 30 (week ending 1st August 2021) with a total of 399 deaths. This was mainly driven by Nigeria who reported 395 deaths this week. The peak of the death in Niger was reported in week 33 (week ending 22 August 2021) with 46 deaths. The global sex ratio Female / Male in the subregion was 1.01. This ratio was 1.24 in Niger, 0.72 in Benin and Cameroon and 1.00 in Togo. Globally, females are slightly more affected than males. But, regarding deaths, the sex ratio Female / Male was 0.82. The number of deaths reported within male was higher than female. People above 15 years were the most affected (59%). This trend was reported in all affected countries. The under-five accounted for 26% of cases.
4.4. Predisposing factors
From the review of key documents on the outbreaks, low access to Water, Sanitation And Hygiene (WASH) was reported in all the affected countries as the main predisposing factors (Table 2). This included lack of potable water in rural areas and urban slums in all affected countries, low access to adequate sanitation, poor hygiene practices. The access to safe water was deprived in Lac district in Togo by the closing of potable water sources and by the contamination of water sources following floods in Niger and Nigeria. Inadequate community behaviours were also reported. These included low compliance with hygiene practices, intentional release of stool waste in run-off, reticence to the use of latrines and practices of large-scale opened defecation (Niger, Nigeria, Togo). The ongoing rainy seasons in Niger, Nigeria, Cameroon with heavy rains and floods, humanitarian situation and security issues in Cameroon, Mali, Niger and Nigeria; and overcrowded camps were also reported as predisposing factors. Cross-border movements and ongoing outbreaks in neighbouring countries were instrumental in the spread of the outbreak.
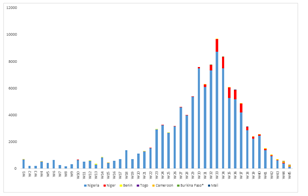
Figure 3: Cholera cases onset date weekly trend in affected countries in West Africa, week 1 to week 45 2021.
Table 2: Status of key WaSH indicators in West African countries in 2020.
5. Discussion
Cholera is known as a major public health emergency in the WHO African Region and high burden cholera outbreaks were reported in the past [12-14]. However, the 2021 cholera is unprecedented in number of cases reported and geographic spread in terms of numbers of States and Regions affected in Niger and Nigeria [15 - 16]. This is the ever-biggest documented cholera outbreak in West Africa. The number of cases reported is closed to the total cumulative number of cholera cases reported in all West African countries from 1995 to 2005 during 124 outbreaks [2]. The scale of the outbreak was mainly driven by Nigeria figures that account for around 95 % of cases and deaths. The cases reported in Nigeria made up for close to the half of the total cumulative number of cholera cases reported in the country from 1970 to 2011 [4]. The 2021 outbreak is also unprecedented in number of deaths. The disease so far claimed more than 3,700 deaths and led to high CFR in all affected countries. This level of deaths was never documented in any single cholera outbreak in West Africa especially in Nigeria and Niger since 1991 [15, 16]. The magnitude of the outbreak can be explained by many factors. The already weak health systems of affected countries were overwhelmed by the ongoing covid-19 pandemic; The novelty and burden of Covid-19 mobilized political leaders and resources at the earlier stage of the response to these cholera outbreaks. Other competing outbreaks and emergencies were also ongoing in affected countries. These include Yellow fever in Nigeria, circulating vaccine-derived poliovirus outbreaks in both countries and humanitarian crises. All these public health events were to be managed by the same health system workforce with not enough additional manpower provided. On other hand, the level of preparation of countries to adequately and timely detect and respond to cholera outbreaks was insufficient. A readiness assessment conducted in seven countries (Burkina Faso, Cameroon, Côte d’Ivoire, Democratic Republic of Congo, Ghana, Kenya and Togo) in October 2021 reveals that the overall readiness rate was 54%. Only laboratory confirmation capacity reached the level of 80% while risk communication, surveillance, WASH and case management rates were below 50%. The magnitude and the spread of the outbreak can also be explained by the high susceptibility of affected communities to cholera in both countries. While cholera is endemic in some settings in Nigeria and Niger, the spread of the outbreak to non-endemic areas met cholera susceptible people. This susceptibility can explain the high attack rates reported in some settings [18]. Insufficient vaccination coverage in major hotspots could have contributed to this susceptibility. In fact, if oral cholera vaccines (OCV) campaigns were organized in targeted and geographically limited hotspots in response to outbreaks in West Africa [19-21], the limited availability of OCV in the stockpile as well as the delay in completing hotspot analysis and vaccines requests to GTFCC did not allow preventive vaccination in major hotspots before the outbreak. Despite the increased efforts in availing vaccines by GTFCC, the different cholera outbreaks reported across the World is regularly affecting the stock. Also, OCV is known to be more effective when campaigns are implemented in the situation of early outbreak detection and timely response. In these cases, rapid implementation of OCV campaign is instrumental in preventing further spread of the outbreak and quick control in a very limited geographical area. During the 2021 outbreaks in West Africa, huge delays were reported in the detection of the outbreak and especially in requesting vaccines from International coordination group or GTFCC. The community susceptibility was potentialized by known predisposing factors such as low access to WASH services [3, 22, 23] including inadequate hygiene practices [22, 24] and inadequate community behaviours that led to spread of the Vibrio cholerae.he overall CFR during the outbreak was too high. The Regional framework for the implementation of the global strategy for cholera prevention and control 2018-2030 targets a CFR below 1 % [6]. The high CFR reported was already found during previous cholera outbreaks including in Nigeria [13]. Late care seeking [25] and high proportion of malnutrition in some settings [10] were reported as contributing factors in different reports. This late care seeking was linked to the inadequate perception of the disease in some settings. In some communities by examples, some patients prefer to wait until night before going to health facilities for treatment. In the interim, their disease usually worsened and led to deaths. The large scale of the outbreak led also to management of severe cases in some health facilities. But the health workers were overwhelmed by competing emergencies (Covid-19, Yellow fever, circulating vaccine-derived poliovirus epidemics); coupled of known shortage of human resources, this could have led to weaknesses in case treatment and proper follow of severe cases. The absence of the community component in case management systems can also explain the high CFR. In fact, the establishment of oral rehydration places in community was extremely rare in all affected countries [26]. Despite these potential reasons, the number of reported deaths is concerning and need further deep investigation. In fact, there was no cholera deaths case definition used during these outbreaks. Then, the number of reported deaths could have included deaths related to other diseases associated to cholera. The outbreak was managed while covid-19 pandemic was ongoing. But, there was no mechanism in place to check if there was any potential association of covid-19 with cholera. On other hands, while females were the most affected gender, deaths were mainly reported within male. During the 2018 cholera outbreak in Nigeria, Elimian et Al. found that male gender was positively associated with cholera death [25]. This author also found other factors including older age, living in peri-urban areas or in flooded states, infection during the rainy season [25]. All these conditions were met during the current outbreak and can explain the high CFR reported.
The 2021 cholera outbreak in West Africa highlights again the role of cross-border migration [3, 27] in outbreak spread as well as the role of specific populations such as travelers, migrants, truck drivers, fishermen in spreading the disease. The site of exposure of index cases, in 4 out the 7 countries, provides evidences on cross-border spread. Cholera outbreak is always reported in Niger Republic when ongoing in Nigeria. Vibrio cholerae O1 was the serogroup identified in all the affected countries. The serotype Ogawa was isolated by laboratories in six out of seven countries while the serotype Inaba was identified in Cameroon. Despites these findings, the absence of the vibrio sequencing does not allow formal establishment of links between affected countries. But, efforts are being made to systematize vibrio sequencing during future outbreaks. On other hands, a regional approach should quickly be established in responding to any cholera outbreak; this includes strengthened cross-border collaboration as well as rapid improvement of the readiness in at risk countries. The current outbreak is a huge bottleneck on the road to the achievement of the expected results of the regional framework for the implementation of the global roadmap for cholera prevention and control in the WHO African Region [6]. While one of the global roadmap objectives was to reduce by 90% the number of cholera related deaths, the figures reported during this outbreak is compromising the achievement of this objective. This applies also for the high CFR reported across affected countries. Countries are not yet fully committed to the implementation of the cholera elimination framework. None of the affected countries had long-term cholera elimination plan as per the global task force for cholera control recommendations before the outbreak. It is now urgent to WHO, Member States and partners to commit more to the implementation of the global roadmap and the African region cholera elimination framework. This is necessary to avoid new high burden cholera outbreaks with negative social and economic impacts; and to put the region on track for the elimination of cholera by 2030. The current study has reached the expected results. The epidemiology of the outbreaks was described. The potential limitations (under reporting, delay in reporting, low laboratory confirmation rate) does not affect the conclusion. It is obvious that data are under-estimated and further efforts are needed to ensure completeness and promptness of reporting during cholera outbreaks. However, the high-level commitment of all stakeholders involved in the management of the outbreaks need to be raised. The response to the outbreaks were taken seriously in all countries by political leaders and technical teams; adequate interventions implemented led to the quick control of the outbreaks in Burkina Faso, Mali and Togo. The trend of the outbreak has sharply decreased in Niger and Nigeria at the time of the study indicating possible control in the following weeks.
6. Conclusion
The high burden of the 2021 cholera outbreak shows that West Africa and all the WHO African region Member States are not yet on track to achieve the cholera elimination goal by 2030. Countries should quickly improve the implementation of the global roadmap and African region framework for cholera elimination by 2030. Strong and adequate measures are needed to improve country preparedness and readiness and enable early cholera outbreak detection and response. The deficit in term of access to WASH services is a mirror of the debilitating underinvestment in the sector over several years; if any successful intersectoral interventions are to be made to control or eliminate cholera in the region, improving WASH conditions should be prioritized effectively at all levels. Also, cross-border collaboration should be systematically strengthened at the earlier stage of any given outbreak and subregional response mechanism supported for adequate coordination of response and preparedness interventions. Cholera outbreaks need better and timely attention from government and partners at earlier stage to avoid their worsening especially when they occur at the same time with other emergencies.
References
- Kaper JB, Morris JG, Levine MM. Cholera. Clin Microbiol Rev 8 (1995): 48-86.
- Griffith DC, Kelly-Hope LA, Miller MA. Review of reported cholera outbreaks worldwide, 1995-2005. Am J Trop Med Hyg 75 (2006): 973-977.
- Ajayi A, Smith SI. Recurrent cholera epidemics in Africa: which way forward? A literature review. Infection 47 (2019): 341-349.
- Mengel MA, Delrieu I, Heyerdahl L, et al. Cholera outbreaks in Africa. Curr Top Microbiol Immunol 379 (2014): 117-144.
- World Health Organization. Cholera, 2019. Weekly Epidemiological Record 95 (2020): 441-448.
- Regional Committee for Africa 68. Regional framework for the implementation of the global strategy for cholera prevention and control, 2018–2030: Report of the Secretariat (2018).
- Global task force on cholera control. Ending cholera: A global roadmap to (2030).
- World Health Assembly 71. Cholera prevention and control (2018).
- Raleigh C, Nsaibia H, Dowd C. The Sahel crisis since 2012. African Affairs 120 (2021): 123-143.
- Heirman J, Rosenzweig MJ, Jenkins M. Leçons apprises grâce aux évaluations d’impact des programmes du PAM pour lutter contre la malnutrition aiguë moderee dans le Sahel (2020)
- Global Task Force on Cholera Control. GTFCC Manuel de terrain-Reponse à l’epidemie de choléra (2019).
- Bartels SA, Greenough PG, Tamar M, VanRooyen MJ. Investigation of a cholera outbreak in Ethiopia’s Oromiya Region. Disaster Med Public Health Prep 4 (2010): 312-317.
- Dalhat MM, Isa AN, Nguku P, et al. Descriptive characterization of the 2010 cholera outbreak in Nigeria. BMC Public Health 14 (2014): 1167.
- Noora CL, Issah K, Kenu E, et al. Large cholera outbreak in Brong Ahafo Region, Ghana. BMC Res Notes 10 (2017): 389.
- Elimian KO, Musah A, Mezue S, et al. Descriptive epidemiology of cholera outbreak in Nigeria, January-November, 2018: implications for the global roadmap strategy. BMC Public Health 19 (2019): 1264.
- World Health Organization. Cholera-Niger (2018).
- Denue BA, Akawu CB, Kwayabura SA, et al. Low case fatality during 2017 cholera outbreak in Borno State, North Eastern Nigeria. Ann Afr Med 17 (2018): 203-209.
- Onyango D, Karambu S, Abade A, et al. High case fatality cholera outbreak in Western Kenya, August 2010. Pan Afr Med J 15 (2013): 109.
- Msyamboza KP, M’bang’ombe M, Hausi H, et al. Feasibility and acceptability of oral cholera vaccine mass vaccination campaign in response to an outbreak and floods in Malawi. Pan Afr Med J 23 (2016).
- Amani A, Tatang CA, Bayiha CN, et al. A reactive vaccination campaign with single dose oral cholera vaccine (OCV) during a cholera outbreak in Cameroon. Vaccine 39 (2021): 1290-1296.
- Ngwa MC, Alemu W, Okudo I, et al. The reactive vaccination campaign against cholera emergency in camps for internally displaced persons, Borno, Nigeria, 2017: a two-stage cluster survey. BMJ Global Health 5 (2020): 002431.
- Elimian KO, Mezue S, Musah A, et al. What are the drivers of recurrent cholera transmission in Nigeria? Evidence from a scoping review. BMC Public Health 20 (2020): 432.
- Visa T, Emmanuel T, Mbodi F, et al. Risk factors associated with cholera outbreak in Mubi Adamawa state – Nigeria, 2018. International Journal of Infectious Diseases 101 (2020): 266.
- Gallandat K, Jeandron A, Ross I, et al. The impact of improved water supply on cholera and diarrhoeal diseases in Uvira, Democratic Republic of the Congo: a protocol for a pragmatic stepped-wedge cluster randomised trial and economic evaluation. Trials 22 (2021): 408.
- Elimian KO, Musah A, Ochu CL, et al. Identifying and quantifying the factors associated with cholera-related death during the 2018 outbreak in Nigeria. Pan Afr Med J 37 (2020): 368.
- Tappero JW, Tauxe RV. Lessons Learned during Public Health Response to Cholera Epidemic in Haiti and the Dominican Republic. Emerg Infect Dis 17 (2011): 2087-2093.
- Glass RI, Blake PA, Waldman RJ, et al. Cholera in Africa: lessons on transmission and control for Latin America. The Lancet 338 (1991): 791-795.
