Telemedicine and Use of Remote Monitoring in Cardiovascular Disease: A Systematic Review
Article Information
Umna Safdar Khan1, Babivigasan Gunasegaran2, Ann Mary Behanan2, Suganya Giri Ravindran3, Obianuju Efobi4, Nahid Sultana5*, Iffat Iqbal6, Srija Chowdary Vanka7, Deepkumar Patel8, Abiodun O Aboaba9, Olubukola Oloniyo10, Esosa Daniel Omoregie11, Stephen Dada10, Mayowa Stephen Apata10, Osahon David Omoregie11
1Dow International Medical College (DIMC), Dow University of Health Sciences (DUHS), Pakistan
2Caribbean Medical University, Willemstad Curacao
3Kanyakumari Government Medical College, India
4Danylo Halytsky Lviv National Medical University, Ukraine
5Shaheed Suhrawardy Medical College, Bangladesh
6Dow University of Health Sciences (DUHS), Pakistan
7Dr. Pinnamaneni Siddhartha Institute of Medical Sciences and Research Foundation, India
8Smt. B. K. Shah Medical Institute & Research Centre (SBKS), India
9Avalon University School of Medicine, Willemstad Curacao
10Windsor University School of Medicine, St. Kitts
11University of Benin, School of Medicine, Nigeria
*Corresponding author: Nahid Sultana, Shaheed Suhrawardy Medical College, Bangladesh
Received: 05 January 2022; Accepted: 14 January 2022; Published: 21 January 2022
Citation:
Umna Safdar Khan, Babivigasan Gunasegaran, Ann Mary Behanan, Suganya Giri Ravindran, Obianuju Efobi, Nahid Sultana, Iffat Iqbal, Srija Chowdary Vanka, Deepkumar Patel, Abiodun O Aboaba, Olubukola Oloniyo, Esosa Daniel Omoregie, Stephen Dada, Mayowa Stephen Apata, Osahon David Omoregie. Telemedicine and Use of Remote Monitoring in Cardiovascular Disease: A Systematic Review. Archives of Internal Medicine Research 5 (2022): 038-048.
View / Download Pdf Share at FacebookAbstract
Background: With the high prevalence of cardiovascular disease (CVD) across the globe, telehealth offers great potential for the management of rehabilitation and primary prevention. Lifestyle changes are also known to contribute to primary and secondary prevention strongly.
Aim: This study aimed to assess the effectiveness of telehealth intervention in the primary and secondary management of CVD.
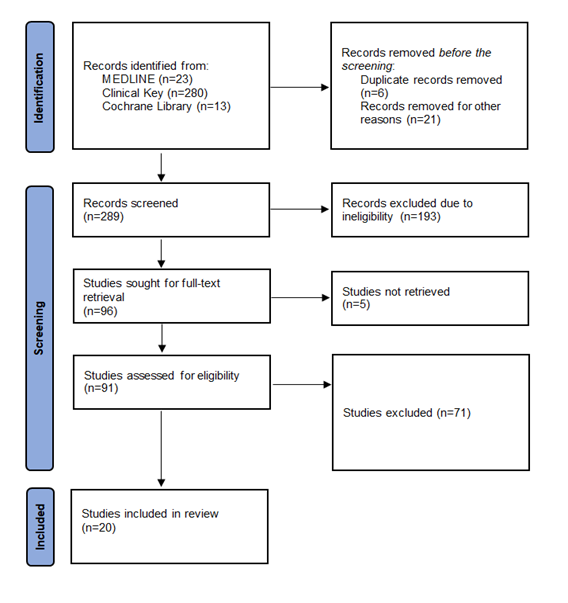
Method: The systematic review was performed as per the Cochrane methods. We searched relevant databases between 2010 and 2021. We chose studies as per the inclusion criteria and used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline.
Results: Twenty randomized controlled trials met the inclusion criteria. We used different telehealth methods with monitoring, including telephone calls, text messages, emails, online platforms, and remote monitoring of physiological parameters. Compared to routine care, we found moderate evidence of telehealth intervention efficacy.
Conclusion: Our findings demonstrate positive outcomes for primary and secondary prevention of CVD. Telehealth can be incorporated as part of routine care to prevent and manage CVD.
Keywords
Telemedicine, Remote Monitoring, Cardiovascular Disease, Access, Healthcare
Telemedicine articles; Remote Monitoring articles; Cardiovascular Disease articles; Access articles; Healthcare articles
Article Details
1. Introduction
Telemedicine has been reintroduced within the modern era following the recent coronavirus disease 2019 (COVID-19) pandemic [1]. However, the concept of telemedicine was first introduced in the early 20th century, focusing on the transmission of images [2]. Over time, telemedicine was also being incorporated in remote patient monitoring. In the last two decades, there has been great progress with the simultaneous use of smartphone and broadband advances and capabilities [3]. The current healthcare model is presented with challenges to access healthcare by patients. The COVID-19 pandemic has resulted in a rapid shift in the healthcare delivery model with the adoption of telemedicine [4]. During the pandemic's peak, we adopted remote consultation and monitoring to support traditional face-to-face consultations between patients and healthcare workers [5]. Incorporating telemedicine within heal-thcare was not limited to high-income countries (HICs) but was also present in low- and middle-income countries (LMICs) [6]. Specifically consi-dering cardiovascular disease (CVD), we can easily monitor patients for their vitals and symptomatology remotely [7]. Typically, these telehealth technologies contain wearables such as watches or patches, which can prevent severe complications [8]. The following review focuses on the currently available data within the telemedicine technologies for CVD patients as preventive or interventional modalities. With the combined empirical evidence, we aim to integrate further and develop telemedicine-based healthcare in CVD patient care.
2. Methods
2.1 Search strategy and selection
We reviewed the following databases, including MEDLINE, Clinical Key, and Cochrane Library. Two reviewers screened the records. The first step was to examine the title and abstract, followed by full-text reviews. The third reviewer addressed discrepancies between the first two reviewers during every stage of the selection process. We selected only articles in English. There was no restriction on the search strategy. We included all articles from 2010 until November 24, 2021. The keywords including "cardiovascular disease, "CVD," "remote monitor-ing," and "telemedicine" were included. We included only relevant randomized controlled trials (RCTs). Further, a review of the reference list was also conducted of relevant articles as part of an umbrella review to ensure the inclusion of all relevant articles. Duplicates were removed using the software Endnote X9.
2.2 Objectives
The primary objective is to demarcate current evidence available for remote monitoring of patients with CVD. The secondary aim is to explore the feasibility of incorporating remote monitoring as part of the healthcare delivery model at a large scale.
2.3 Data analysis
Following the study inclusion, the studies were first assessed for quality. All three reviewers utilized the Newcastle-Ottawa Scale (NOS). Three reviewers extracted data on a customized datasheet in Excel. The following variables were tabulated for the included RCTs: author-year, country, target conditi-on, number of participants, proposed benefit, specific use of telemonitoring, and advantage. We conducted the qualitative analysis to identify currently available evidence regarding remote monitoring technologies for CVD patients.
3. Results
The search process is shown in Figure 1. The first phase of the screening yielded 316 results. After removing duplicates, we reviewed 310 results for titles and abstracts. In the second phase, we excluded 213 results as they did not meet the eligibility criteria. Twenty studies were finalized and included in the qualitative analysis during the third phase.
In total, six studies reported outcomes focusing on reducing all-cause readmission or all-cause mortality with telehealth interventions among patients with chronic heart failure (CHF). Among these trials, Gallagher et al. [9] did not identify any beneficial outcomes when focusing on adherence to medication with telephonic support. The other five trials identified a reduction in all-cause readmission and all-cause mortality with telehealth enabled intervene-tions, including self-care behavior with short mess-ages [10], monitoring of pulmonary artery pressure with a wireless hemodynamic monitoring system [11], electronic documenting of vitals [12], combined monitoring of the electrocardiogram, blood pressure, body weight, and oxygen saturation (SpO2) [13], communication about symptoms [14], and home-based exercise program [15].
Investigators from one trial reported all-cause read-mission or mortality following percutaneous coronary intervention (PCI) for acute coronary syndrome (ACS). Investigators from another trial collected exercise and dietary habits of participants over online and smartphone platforms but that did not show any significant reduction in all-cause readmissions or mortality [16]. The second trial monitored dietary and exercise habits similarly and reported weight loss after telehealth monitoring [16]. Eleven trials supported self-rehabilitation following primary diag-nosis of CVD through sending text messages [17, 18], online platforms [19-21], telephone calls [22-25], and remote monitoring [26]. Two trials monitored primary prevention of CVD with tele-phone calls [27], emails [27], online platforms [27, 28]. Overall, the studies conducted telehealth inter-ventions and monitoring by sending text messages, telephone calls, telephone calls combined with messages, online programs, emails, and telemoni-toring. The major characteristics are summarized in Table 1.
ACS: Acute coronary syndrome; CVD: Cardiovascular disease; CHF: Chronic heart failure; CHD: Coronary heart disease; EHR: Electronic health record; ER: Emergency room; HF: Heart failure; LDL-C: low-density lipoprotein cholesterol; MI: Myocardial infarction; RCT: Randomized control trial; USA: United States of America.
Table 1: Summary of key findings of the included RCTs for telemonitoring in CVD management.
4. Discussion
This review summarizes data from 20 RCTs published in 2010-2020 reporting telehealth within CVD prevention and management. We aimed to examine the effects of telehealth compared to routine care for either primary or secondary prevention of CVD. In the qualitative analysis, we found efficacy with telehealth interventions focusing on secondary prevention. The present study's findings can be generalized as the data is obtained from RCTs globally. We noted that control of risk factors remains challenging with telehealth interventions, with certain studies reporting improvement compared to current standards of care. There may be various reasons that render telehealth interventions subop-timal. For instance, lifestyle changes are difficult to incorporate due to the lifelong fostering of these habits. Studies in our review show that telehealth interventions that focus on remote monitoring also offer some efficacy. However, we expect certain trials to perform better than others, probably due to differences in baseline characteristics.
CVD is the leading cause of mortality across the United States [30]. With the change in demographic patterns across industrialized nations, we may expect a higher burden of patients with CVD and its complications [31]. It is expected that by 2030, the prevalence of CVD is expected to increase rapidly. With the recent popularity of telehealth, it is pertinent to optimize telehealth interventions and monitoring for CVD [32]. Mobile applications are present within platforms that may collect information about patient physiological metrics, symptomatology, and disease education [33]. The collection of physiological data may also be present through smartphones. Recently, wearable devices have gained popularity as they may detect arrhythmias and act as portable sensors (e.g., Apple Watch) [33]. Other sensors may also detect heart rate, ECGs, and blood pressures. These technologies are present in industrialized nations and across developing nations such as India [34].
Another target for cardiac rehabilitation in heart failure patients is medication adherence [35]. While our study did not find any major improvement in medication adherence, it is an important target for cardiac telemonitoring. This could be particularly beneficial for older populations. There are numerous opportunities for streamlining programs that focus on singular outcomes such as patient education, self-monitoring, improving physical health, which falls within the arena of self-management [36]. Other aspects of telehealth include remote monitoring, which provides concrete information about patients with CVD [37]. We suggest further RCTs that focus on examining personal determinants of health, with aim to improve cardiac rehabilitation and prevention of CVD. Our study has a few limitations. There were differences in the outcomes of the studies that were included. Therefore, it was difficult to ascertain the objective benefits of each type of telehealth monitoring employed. We also did not find any clear follow-up period across the trials. Therefore, it was not possible to confirm whether the trials that had shown efficacy would also result in long-term improvement in the health status of the participants.
5. Conclusion
We found moderate-grade evidence of the beneficial effects of telehealth monitoring among CVD patients. Modifiying the lifestyle and habits of the participants was challenging, in both primary and secondary prevention of CVD. We expect telehealth to improve and widen the scope of cardiac monitoring and rehabilitation in the next few decades. With numer-ous trials underway for the management of CVD, patients may benefit from telehealth monitoring of their health status. Remote contact with healthcare providers also provides an assessment of functional capacity, attainment of cardiac rehabilitation, and potential of readmission to hospitals. These ongoing trials are important as they will develop the current understanding of cardiac telehealth and improve the existing burden.
References
- Hirko KA, Kerver JM, Ford S, et al. Telehealth in response to the COVID-19 pandemic: Implications for rural health disparities. J Am Med Informatics Assoc 27 (2020): 1816-1818.
- Nittari G, Khuman R, Baldoni S, et al. Telemedicine practice: review of the current ethical and legal challenges. Telemed e-Health 26 (2020): 1427-1437.
- Kim J, Campbell AS, de Ávila BE-F, et al. Wearable biosensors for healthcare monitoring. Nat Biotechnol 37 (2019): 389-406.
- Thomas EE, Haydon HM, Mehrotra A, et al. Building on the momentum: Sustaining telehealth beyond COVID-19. J Telemed Telecare (2020).
- Mobbs RJ, Ho D, Choy WJ, et al. COVID-19 is shifting the adoption of wearable monitoring and telemedicine (WearTel) in the delivery of healthcare: opinion piece. Ann Transl Med 8 (2020).
- Manenti L, Maggiore U, Fiaccadori E, et al. Reduced mortality in COVID-19 patients treated with colchicine: Results from a retrospective, observational study. PLoS One 16 (2021): e0248276.
- Bae YS, Kim KH, Choi SW, et al. Information technology-based management of clinically healthy COVID-19 patients: Lessons from a living and treatment support center operated by Seoul National University Hospital. J Med Internet Res 22 (2020): e19938.
- Guk K, Han G, Lim J, et al. Evolution of wearable devices with real-time disease monitoring for personalized healthcare. Nanomaterials 9 (2019): 813.
- Gallagher BD, Moise N, Haerizadeh M, et al. Telemonitoring adherence to medications in heart failure patients (TEAM-HF): a pilot randomized clinical trial. J Card Fail 23 (2017): 345-349.
- Chen C, Li X, Sun L, et al. Post-discharge short message service improves short-term clinical outcome and self-care behaviour in chronic heart failure. ESC Heart Fail 6 (2019): 164-173.
- Abraham WT, Adamson PB, Bourge RC, et al. Wireless pulmonary artery haemodynamic monitoring in chronic heart failure: A randomised controlled trial. Lancet 377 (2011): 658-666.
- Dendale P, De Keulenaer G, Troisfontaines P, et al. Effect of a telemonitoring-facilitated collaboration between general practitioner and heart failure clinic on mortality and rehospitalization rates in severe heart failure: the TEMA-HF 1 (TElemonitoring in the MAnagement of Heart Failure) study. Eur J Heart Fail 14 (2012): 333-340.
- Koehler F, Koehler K, Deckwart O, et al. efficacy of telemedical interventional management in patients with heart failure (TIM-HF2): a randomised, controlled, parallel-group, unmasked trial. Lancet 392 (2018): 1047-1057.
- Boyne JJJ, Vrijhoef HJM, Crijns HJGM, et al. Tailored telemonitoring in patients with heart failure: results of a multicentre randomized controlled trial. Eur J Heart Fail 14 (2012): 791-801.
- Peng X, Su Y, Hu Z, et al. Home-based telehealth exercise training program in Chinese patients with heart failure: a randomized controlled trial. Medicine (Baltimore) 97 (2018).
- Widmer RJ, Allison TG, Lennon R, et al. Digital health intervention during cardiac rehabilitation: a randomized controlled trial. Am Heart J 188 (2017): 65-72.
- Reid RD, Morrin LI, Beaton LJ, et al. Randomized trial of an internet-based computer-tailored expert system for physical activity in patients with heart disease. Eur J Prev Cardiol 19 (2012): 1357-1364.
- Chow CK, Redfern J, Hillis GS, et al. Effect of lifestyle-focused text messaging on risk factor modification in patients with coronary heart disease: a randomized clinical trial. Jama 314 (2015): 1255-1263.
- Vernooij JWP, Kaasjager HAH, Van Der Graaf Y, et al. Internet based vascular risk factor management for patients with clinically manifest vascular disease: randomised controlled trial. BMJ (2012).
- Dale LP, Whittaker R, Jiang Y, et al. Text message and internet support for coronary heart disease self-management: results from the Text4Heart randomized controlled trial. J Med Internet Res 17 (2015): e4944.
- Johnston N, Bodegard J, Jerström S, et al. Effects of interactive patient smartphone support app on drug adherence and lifestyle changes in myocardial infarction patients: a randomized study. Am Heart J 178 (2016): 85-94.
- Heron N, Kee F, Mant J, et al. Rehabilitation of patients after transient ischaemic attack or minor stroke: Pilot feasibility randomised trial of a home-based prevention programme. Br J Gen Pract 69 (2019): e706-714.
- Bosworth HB, Olsen MK, McCant F, et al. Telemedicine cardiovascular risk reduction in veterans: The CITIES trial. Am Heart J 199 (2018): 122-129.
- Hawkes AL, Patrao TA, Atherton J, et al. effect of a telephone-delivered coronary heart disease secondary prevention program (proactive heart) on quality of life and health behaviours: primary outcomes of a randomised controlled trial. Int J Behav Med 20 (2013): 413-424.
- Yan J, You L, Liu B, et al. The effect of a telephone follow-up intervention on illness perception and lifestyle after myocardial infarction in China: A randomized controlled trial. Int J Nurs Stud 51 (2014): 844-855.
- Karhula T, Vuorinen A-L, Rääpysjärvi K, et al. Telemonitoring and mobile phone-based health coaching among Finnish diabetic and heart disease patients: randomized controlled trial. J Med Internet Res 17 (2015): e153.
- Coorey G, Peiris D, Neubeck L, et al. A realist evaluation approach to explaining the role of context in the impact of a complex eHealth intervention for improving prevention of cardiovascular disease. BMC Health Serv Res 20 (2020): 1-13.
- Appel LJ, Clark JM, Yeh H-C, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med 365 (2011): 1959-1968.
- Assefa Y, Gilks CF, Van De Pas R, et al. Reimagining global health systems for the 21st century: lessons from the COVID-19 pandemic. BMJ Glob Heal 6 (2021): e004882.
- Roth GA, Johnson CO, Abate KH, et al. The burden of cardiovascular diseases among US states, 1990-2016. JAMA Cardiol 3 (2018): 375-389.
- Habib SH, Saha S. Burden of non-communicable disease: global overview. Diabetes Metab Syndr Clin Res Rev 4 (2010): 41-47.
- Barbosa W, Zhou K, Waddell E, et al. Improving Access to Care: Telemedicine Across Medical Domains. Annu Rev Public Health 42 (2021): 463-481.
- Bostrom J, Sweeney G, Whiteson J, et al. Mobile health and cardiac rehabilitation in older adults. Clin Cardiol 43 (2020): 118-126.
- Gasser U, Maclay CM, Palfrey JG. Working towards a deeper understanding of digital safety for children and young people in developing nations. Berkman Cent Res Publ (2010): 10-36.
- Rengo JL, Savage PD, Barrett T, et al. Cardiac rehabilitation participation rates and outcomes for patients with heart failure. J Cardiopulm Rehabil Prev 38 (2018): 38-42.
- Phillips SA, Ali M, Modrich C, et al. Advances in health technology use and implementation in the era of healthy living: implications for precision medicine. Prog Cardiovasc Dis 62 (2019): 44-49.
- Cruz-Martínez RR, Wentzel J, Asbjørnsen RA, et al. Supporting self-management of cardiovascular diseases through remote monitoring technologies: meta-ethnography review of frameworks, models, and theories used in research and development. J Med Internet Res 22 (2020): e16157.