Systematic Review of the Effect of Upper Airway Surgery based on DISE findings in Adults with Obstructive Sleep Apnea
Article Information
Bertelsen JB1*, Ovesen T1,2, Zainali-Gill K1
1University Clinic for Balance, Flavour and Sleep, ENT Department, Godstrup Hospital, 7400 Herning, Denmark
2Department of Clinical Medicine, Aarhus University, Denmark
*Corresponding Author: Bertelsen JB, University Clinic for Balance, Flavour and Sleep, ENT Department, Godstrup Hospital, 7400 Herning, Denmark
Received: 07 November 2022; Accepted: 16 November 2022; Published: 09 March 2023
Citation: Bertelsen JB, Ovesen T, Zainali-Gill K. Systematic Review of The Effect of Upper Airway Surgery based on DISE findings in Adults with Obstructive Sleep Apnea. Journal of Surgery and Research. 6 (2023): 49-65.
View / Download Pdf Share at FacebookAbstract
Introduction: Obstructive sleep apnea (OSA) is common among adults worldwide and is associated with an increased risk of both cardiac, metabolic, and mental disease and an increased risk of traffic accidents. However, evidence of the different types of upper airway surgery to relieve OSA symptoms is sparse. Whether Drug induced sedation endoscopy (DISE) can improve the outcome of the various surgical techniques in the upper airways (UA) is uncertain. The objective of this review was to evaluate the effectiveness of UA surgery in adults with OSA by change in apnea-hypopnea index (AHI) with minimum three months follow-up in studies where DISE was used.
Methods: Cochrane, PubMed, CINAHL and Embase were systematically searched on March the 22nd 2022. Relevant studies were selected on abstracts and full texts were obtained for critical appraisal. Relevant data was extracted for data synthesis. The reference list of all studies selected for critical appraisal was screened for additional studies. Studies included were randomized controlled trials, prospective and retrospective studies, casecontrol studies and cohort studies of one or a combination of surgeries on the upper airways in adults diagnosed with OSA and obstruction verified by DISE before surgery published from January 1st 2000 to 31th of December 2021. AHI was reported prior to and minimum three months after surgery by polysomnography or home sleep apnea test and a minimum of 40 participants were included. Surgery in the upper airways such as soft tissue of the retropharyngeal space, velum, tonsils and base of tongue (BOT) were included. Cartilage and osseous surgery as septoplasty, turbinoplasty, mandibular advancement surgery, epiglottoplasty and tracheostomy were included plus studies of hypoglossal nerve stimulation implant insertion.
Results: Studies were
Keywords
Adults; apnea / hypopnea index, drug induced sedation endoscopy, obstructive sleep apnea, upper airway surgery
Adults articles; apnea / hypopnea index articles; drug induced sedation endoscopy articles; obstructive sleep apnea articles; upper airway surgery articles.
Adults articles Adults Research articles Adults review articles Adults PubMed articles Adults PubMed Central articles Adults 2023 articles Adults 2024 articles Adults Scopus articles Adults impact factor journals Adults Scopus journals Adults PubMed journals Adults medical journals Adults free journals Adults best journals Adults top journals Adults free medical journals Adults famous journals Adults Google Scholar indexed journals hypopnea index articles hypopnea index Research articles hypopnea index review articles hypopnea index PubMed articles hypopnea index PubMed Central articles hypopnea index 2023 articles hypopnea index 2024 articles hypopnea index Scopus articles hypopnea index impact factor journals hypopnea index Scopus journals hypopnea index PubMed journals hypopnea index medical journals hypopnea index free journals hypopnea index best journals hypopnea index top journals hypopnea index free medical journals hypopnea index famous journals hypopnea index Google Scholar indexed journals drug induced sedation endoscopy articles drug induced sedation endoscopy Research articles drug induced sedation endoscopy review articles drug induced sedation endoscopy PubMed articles drug induced sedation endoscopy PubMed Central articles drug induced sedation endoscopy 2023 articles drug induced sedation endoscopy 2024 articles drug induced sedation endoscopy Scopus articles drug induced sedation endoscopy impact factor journals drug induced sedation endoscopy Scopus journals drug induced sedation endoscopy PubMed journals drug induced sedation endoscopy medical journals drug induced sedation endoscopy free journals drug induced sedation endoscopy best journals drug induced sedation endoscopy top journals drug induced sedation endoscopy free medical journals drug induced sedation endoscopy famous journals drug induced sedation endoscopy Google Scholar indexed journals obstructive sleep apnea articles obstructive sleep apnea Research articles obstructive sleep apnea review articles obstructive sleep apnea PubMed articles obstructive sleep apnea PubMed Central articles obstructive sleep apnea 2023 articles obstructive sleep apnea 2024 articles obstructive sleep apnea Scopus articles obstructive sleep apnea impact factor journals obstructive sleep apnea Scopus journals obstructive sleep apnea PubMed journals obstructive sleep apnea medical journals obstructive sleep apnea free journals obstructive sleep apnea best journals obstructive sleep apnea top journals obstructive sleep apnea free medical journals obstructive sleep apnea famous journals obstructive sleep apnea Google Scholar indexed journals upper airway surgery articles upper airway surgery Research articles upper airway surgery review articles upper airway surgery PubMed articles upper airway surgery PubMed Central articles upper airway surgery 2023 articles upper airway surgery 2024 articles upper airway surgery Scopus articles upper airway surgery impact factor journals upper airway surgery Scopus journals upper airway surgery PubMed journals upper airway surgery medical journals upper airway surgery free journals upper airway surgery best journals upper airway surgery top journals upper airway surgery free medical journals upper airway surgery famous journals upper airway surgery Google Scholar indexed journals myofunctional therapy articles myofunctional therapy Research articles myofunctional therapy review articles myofunctional therapy PubMed articles myofunctional therapy PubMed Central articles myofunctional therapy 2023 articles myofunctional therapy 2024 articles myofunctional therapy Scopus articles myofunctional therapy impact factor journals myofunctional therapy Scopus journals myofunctional therapy PubMed journals myofunctional therapy medical journals myofunctional therapy free journals myofunctional therapy best journals myofunctional therapy top journals myofunctional therapy free medical journals myofunctional therapy famous journals myofunctional therapy Google Scholar indexed journals bariatric surgery articles bariatric surgery Research articles bariatric surgery review articles bariatric surgery PubMed articles bariatric surgery PubMed Central articles bariatric surgery 2023 articles bariatric surgery 2024 articles bariatric surgery Scopus articles bariatric surgery impact factor journals bariatric surgery Scopus journals bariatric surgery PubMed journals bariatric surgery medical journals bariatric surgery free journals bariatric surgery best journals bariatric surgery top journals bariatric surgery free medical journals bariatric surgery famous journals bariatric surgery Google Scholar indexed journals preoperative planning articles preoperative planning Research articles preoperative planning review articles preoperative planning PubMed articles preoperative planning PubMed Central articles preoperative planning 2023 articles preoperative planning 2024 articles preoperative planning Scopus articles preoperative planning impact factor journals preoperative planning Scopus journals preoperative planning PubMed journals preoperative planning medical journals preoperative planning free journals preoperative planning best journals preoperative planning top journals preoperative planning free medical journals preoperative planning famous journals preoperative planning Google Scholar indexed journals surgical approach articles surgical approach Research articles surgical approach review articles surgical approach PubMed articles surgical approach PubMed Central articles surgical approach 2023 articles surgical approach 2024 articles surgical approach Scopus articles surgical approach impact factor journals surgical approach Scopus journals surgical approach PubMed journals surgical approach medical journals surgical approach free journals surgical approach best journals surgical approach top journals surgical approach free medical journals surgical approach famous journals surgical approach Google Scholar indexed journals
Article Details
Introduction
Upper airway (UA) surgery to treat obstructive sleep apnea (OSA) have been performed for decades, however the outcomes of most operations for OSA are disappointing with mixed results and associated with morbidity. However, the development during the recent years may be in favor of UA surgery if patients are carefully selected. Drug induced sedation endoscopy (DISE), originally described in 1991 by Croft and Pringle [1], is a clinical evaluation of the individual upper airway anatomy during sleep. DISE has been validated to be relevant prior to sleep surgery [2-4]. Whether the introduction of DISE improves the outcome of the various surgical techniques including the evidence level of the executed studies is unknown.
OSA is a common condition among adults worldwide as 34% of men aged 30-70 years and 17% of women aged 30-70 years suffer from OSA [5]. The negative effects of OSA such as increased risk of cardiac and metabolic disease are well-documented [6]. Continuous positive airway pressure (CPAP) is considered first line treatment to prevent upper airway collapse and improve sleep, and to reduce daytime sleepiness. However, two systematic reviews found significant low levels of compliance reported as non-adherence levels to CPAP therapy of 34,3% [7] and from 29% to 83% [8]. Hence, alternatives for CPAP are explored as lifestyle changes, sleep position treatment, use of oral mandibular devices, bariatric surgery, and myofunctional therapy as well as different types of upper airway surgeries to relieve symptoms of OSA or to increase compliance to CPAP.
A preliminary search of PROSPERO, MEDLINE, Cochrane Database of Systematic Reviews, and JBI Database of Systematic Reviews and Implementation Reports was conducted and no current or underway systematic reviews on the topic were identified. A systematic review regarding hypoglossal nerve stimulation was identified [9]. Two systematic reviews regarding trans-oral robotic surgery (TORS) were identified [10,11].
A Cochrane review on the effect of UA surgery for OSA measured by change in AHI from 2005 found a limited number of trials assessing diverse surgical techniques. The effects reported across the trials were inconsistent. The evidence from the small studies did not support the use of surgery in patients with mild to moderate daytime sleepiness associated with OSA [12]. Based on a protocol from 2017, an updated Cochrane Review on surgical treatment of OSA was planned but it has not been published. This review seems to have a focus on change in AHI and in ESS but does not incorporate DISE prior to surgery [13]. The purpose of this review was to investigate the effectiveness of upper airway surgery in adults with OSA evaluated by change in AHI with a minimum of three months follow-up when DISE was included in the preoperative planning and choice of surgical approach.
Materials and Methods
Inclusion criteria
Participants
Inclusion criteria for this review were adult patients older than 18 years with diagnosed OSA either by polysomnography or by home sleep test. Follow-up time was 3 months or longer. Surgery was performed after DISE, and the surgery should address the obstruction site(s) in the UA confirmed by DISE. Exclusion criteria were case reports, reviews containing insufficient data and studies with less than 40 participants or studies that reported treatment with oral appliance therapy (OAT) / mandibular advancement devices (MAD), position trainer or bariatric surgery.
Outcomes
Primary outcomes in this review were changes in AHI, defined by the number of apnea and hypopnea events per hour of sleep, before and minimum three months after surgery. Surgical success and surgical response determined by Sher’s criteria [14] as the reduction of AHI > 50% and to a value of less than 20 events per hour were included. Changes in Epworth Sleepiness scale (ESS) were used to measure patient reported outcome. Secondary outcomes such as oxygen desaturation index (ODI), nadir peripheral oxygen saturation (SpO2), snoring scales, social and functional questionnaires, and other outcomes were described in the results if available.
Types of studies
The systematic review included English written randomized controlled trials, prospective and retrospective case-control studies, cohort studies on one or a combination of surgeries on the upper airways in adults diagnosed with OSA and obstruction verified by DISE before surgery. Sample size was minimum 40 participants. AHI should have been reported prior to and minimum three months after surgery by polysomnography or home sleep apnea test. Publications from January 1st 2000 to December 31th 2021 were included. Surgery of the upper airways, such as soft tissue of the retropharyngeal space, velum, tonsils, epiglottis, and base of tongue were incorporated. Septoplasty and turbinoplasty were also included as well as the novel implant techniques with hypoglossal nerve stimulation plus maxilla-mandibular advancement surgery and hyoid suspension surgery. This review excluded descriptive observational study designs such as case series, individual case reports and descriptive cross-sectional studies.
Methods
This systematic review is conducted in accordance with the Joanna Briggs Institute methodology for systematic reviews of effectiveness evidence [15,16].
Search strategy
The electronic search strategy was designed and conducted by an experienced reference librarian based on input from the study investigators. An initial limited search of MEDLINE and CINAHL was undertaken to identify articles on the topic. The text words contained in the titles and abstracts of relevant articles, and the index terms used to describe the articles were used to develop a full search strategy for Cochrane, MEDLINE, CINAHL and Embase (see Appendix 1). The search strategy with all identified keywords and index terms, was adapted for each included information source. The reference list of all studies selected for critical appraisal was screened for additional studies. To identify eligible studies published in English, the electronic databases (MEDLINE, EMBASE, CINAHL and COCHRANE were searched for studies published from January 1st 2000 to December 31st 2021 cross-referenced with the key words obstructive sleep apnea, sleep apnea AND septoplasty, turbinoplasty, hyoid suspension, epiglottoplasty and tracheostomy, veloplasty, uvulopalatopharyngoplasty(UPPP), Laser-assisted Uvuloplasty (LAUP), palatal radiofrequency ablation (RFA), palatal implants, lateral expansion pharyngoplasty, expansion sphincter pharyngoplasty (ESP), Z-palatoplasty, tonsillectomy, tonsillotomy, adenoidectomy, RFA of tongue base, tongue base resection or reduction, mandibular advancement surgery, hypoglossal nerve stimulation (HNS) or upper airway stimulation (UAS).
Study selection
Following the search, all identified citations were collated and uploaded into Rayyan [17] and duplicates were removed. Titles and abstracts were afterwards screened by two independent reviewers with respect of the chosen inclusion criteria for the review.
Potentially relevant studies were retrieved in full and citation details imported into the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI) (Joanna Briggs Institute, Adelaide, Australia) [18].
The full texts of selected citations were assessed in detail by two independent reviewers. Reasons for exclusion were noted and reported. Any disagreements that occurred between the reviewers at each stage of the study selection process were resolved through discussion, or with a third reviewer. The results of the search were reported in full in the final systematic review and presented in a Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) flow diagram [19].
Assessment of methodological quality
Eligible studies were critically appraised by two independent reviewers at the study level. Authors of papers was contacted to request missing or additional data for clarification when required. Any disagreements that occurred was resolved through discussion, or with a third reviewer. Following critical appraisal, studies not meeting a certain quality regarding details on patient selection, intervention or data quality were excluded. The included studies are reported in tables 1 and 2.
Data extraction
Extracted data was included in the review using a standardized data extraction tool. The data included specific details about the populations, study methods, interventions, and outcomes of significance to the review objective.
Data synthesis
The meta-analysis was performed in a statistical software Cran-R-4.0.3 using the package 'metafor'. The estimates of pre- to post-operative changes and 95% confidence intervals were calculated using fixed effect model with inverse of the variance as weights. The data was divided into four groups, each specific for the level of obstruction addressed, either velum/oropharynx (soft palate), base of tongue (BOT), multilevel surgery or upper airway stimulation by hypoglossal nerve implant (UAS). Some specific studies investigated different techniques to address identical anatomical sites and therefore these studies are divided into several subgroups in the presentation of the meta-analysis for clarification purposes.
Soft palate surgery (Velum/Oropharynx)
Soft palate surgery aims to reduce and reconstruct the part of the soft palate which often collapses along with obstructive sleep apnea. A procedure initially known as classical uvulo-palato-pharyngo-plasty (UPPP), first described by Fujita involves removal of both tonsils, the posterior part of the soft palate and uvula, and closure of the tonsillar pillars [20]. Different techniques have evolved such as modified UPPP with removal of additional mucosa and submucosal adipose tissue [21]; expansion sphincter pharyngoplasty (ESP) described by Pang and Woodson [22]. The ESP involves transection of the palatopharyngeal muscle and rotation of the muscle superior-laterally for mobilization, and then suture it to the pterygomandibular raphe through a mucosal tunnel to create a broader widening of the pharyngeal space. Further techniques such as barbed wire stitch reposition pharyngoplasty (BRP) [23], use of radiofrequency ablation of the soft palate [24] or laser-assisted uvulopalatoplasty [25] are also well-known as treatment of retropharyngeal collapse. A thorough description of these techniques is not within the scope of this paper. However, it is noticed that some techniques are conducted in outpatient clinics, others require hospitalization; some techniques are performed as multilevel surgery, others as one-stage surgery.
Furthermore, some procedures are offered to patients with severe OSA where AHI is high, others in mild or moderate OSA. Clinical features such as comorbidity, BMI, tonsil size, position of the soft palate, narrowing of the pharyngeal wall, neck circumference, the degree of collapses of the upper airway observed during DISE are used, however not all available studies present these findings, nor do many studies follow a uniform standardized approach.
Base of tongue (BOT)
The variety of procedures designed to target the hypopharynx and BOT have been investigated. Procedures such as genioglossus advancement [26], radiofrequency tissue ablation of the tongue base [27], suturing of the tongue base and hyoid suspension are described [28], however, the studies are often case reports or retrospective studies with few subjects and a limited follow-up. The introduction of TORS and advancements in tongue base resections initially in cancer surgery has evolved to also include TORS in sleep surgery [29].
Multilevel surgery
OSA is often associated with multilevel collapse of the upper airways, hence multilevel surgery is commonly chosen as treatment opportunity. The benefits and disadvantages of single-step and multi-step surgical intervention is beyond the scope of this review. Some surgeons advocate that nasal surgery is performed prior to any direct approach towards the soft palate, lateral wall of the oropharynx or BOT is considered.
Upper Airway stimulation
Hypoglossal nerve stimulation by a unilateral stimulation lead attached to the branch of the hypoglossal nerve, thereby producing tongue protrusion synchronous with expiration during sleep, is termed upper airway stimulation (UAS) [30]. The impulse generator is implanted beneath the clavicle and a tunneled breathing sensing lead is placed between the external and intercostal muscles. One could advocate that UAS is a multilevel treatment modality, since postoperative DISE findings indicates improvements in the retropalatal obstruction as well. However, the treatment is indicated in OSA with a primarily retro-lingual obstruction. In this systematic review UAS is subcategorized as it affects the soft tissues in the upper airways indirectly by nerve stimulation.
Results
Eighteen studies with a total of 1187 patients older than 18 years were included. Most patients suffered from moderate to severe OSA. Figure 1 showed the flow diagram for selecting studies.
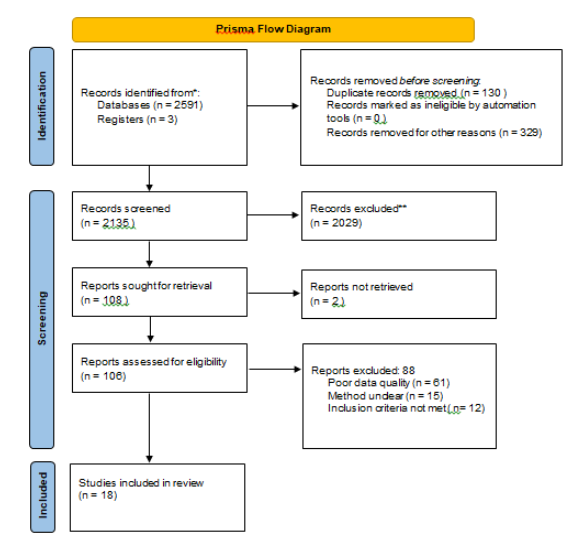
Figure 1: PRISMA 2020 flow diagram for new systematic reviews which included searches of databases and registers.
Due to the heterogeneity of the studies and different types of surgery, data was divided into four subcategories covering the site of obstruction addressed by surgery, hence velum and/or oropharyngeal surgery with six studies and a total of 401 patients (Plaza et al [31], Hong et al [32], Süslü et al [33], Amali et al [34], Elzayat et al [35], Babademez et al [36] one study of BOT surgery with 70 patients (Babademez et al [37], seven studies on multilevel surgery (387 patients) (Bahgat et al [38], Cammaroto et al [39], El-Anwar et al [40], Hwang et al [41], Thaler et al [42], Tsou et al [43], Turhan et al [44] and four studies on upper airway stimulation (329 patients) (Huntley et al [45], Mulholland et al [46], Steffen et al [47], Strollo et al [48]. A summary of the studies including level of evidence is presented in table 1.
[Insert table 1 here]
The changes in AHI in each study are presented in table 2. In velum/oropharynx the most frequent surgeries were ESP and BRP both with a percentage of surgical success based on Sher`s criteria of 84.9% to 91%. The multilevel surgery group was quite diverse with of different surgeries. In the UAS group the Sher`s criteria surgical success was around 90% (figure 1).
[Insert table 2 here]
Primary surgical outcomes were changes in AHI and ESS after surgery and meta-analysis of these results are presented in figures 2-9. Velum and oropharynx surgery led to a mean decrease in AHI of 14.0 events per hour (e/h), 95% CI (12.6; 15.4) (figure 2). ESS was reduced by a mean of 7.62, 95% (6.95; 8.30) (figure 3). In BOT surgery a mean reduction in AHI by 17.7 e/h, 95% CI (15.7; 19.7) (figure 4) and ESS was reduced by a mean of 7.90, 95% CI (7.15; 8.64) (figure 5). Multilevel surgery showed mean reduction in AHI by 25.0 e/h, 95% (22,8; 27.2) (figure 6) and mean ESS by 5.51, 95% (4.62; 6.39) (figure 7). Upper airway stimulation showed a mean decrease in AHI by 21.1 e/h, 95% CI (18.9, 23.3) (figure 8) and a mean reduction in ESS by 4.98, 95% CI (4.25; 5.71) (figure 9).
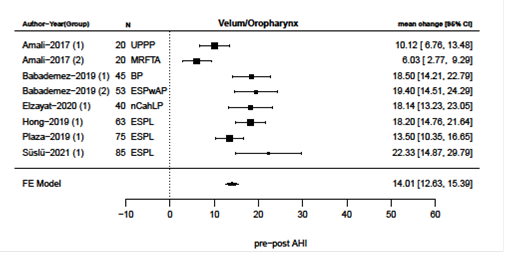
Figure 2: Reduction i AHI after surgery directed at velum/oropharynx
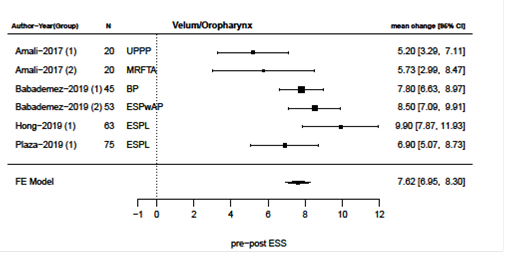
Figure 3: Reduction i ESS after surgery directed at velum/oropharynx
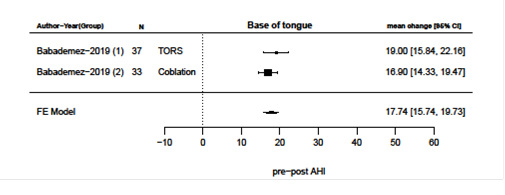
Figure 4: Reduction i AHI after surgery directed at base of tongue
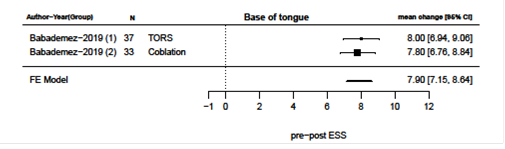
Figure 5: Reduction i ESS after surgery directed at base of tongue
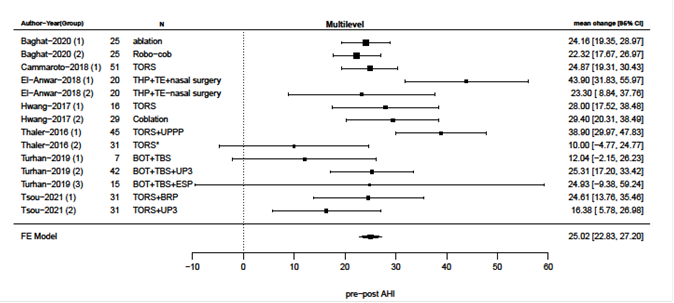
Figure 6: Reduction i AHI after multilevel surgery
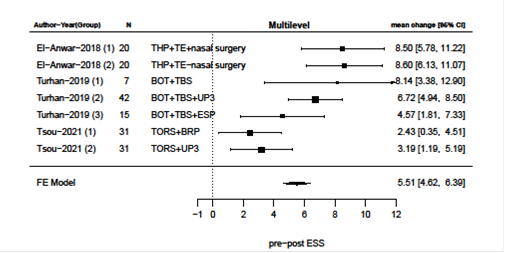
Figure 7: Reduction i ESS after multilevel surgery
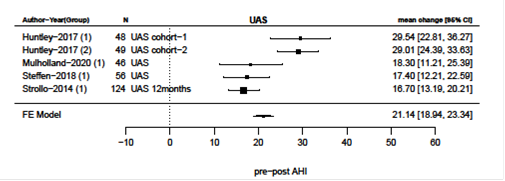
Figure 8: Reduction i AHI after upper airway stimulation
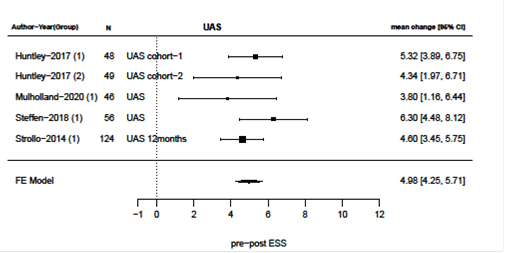
Figure 9: Reduction i ESS after upper airway stimulation
Discussion
Overall, the present systematic review of 18 studies comprised of retrospective case series, cohort studies, non-randomized and randomized prospective trials, found comparable improvements in AHI and ESS after surgery. The use of DISE in planning the surgical procedure was the main criterion for our review and based upon the level of surgery, the final included studies were divided into four groups: velum and oropharynx, BOT, multilevel surgery and UAS. The meta-analysis found statistically significant reductions of both AHI and ESS in all four groups after surgery. In studies where surgical success and surgical response were reported, these were in general acceptable. Sundaram et. al reviewed surgical treatment compared to CPAP treatment or non-surgical appliance therapy and did not find evidence that surgical intervention could improve OSA [12]. In comparison, our review indicates, that surgical intervention can improve both clinical and subjective OSA parameters such as AHI and ESS, when treatment is based upon DISE findings. Although surgical intervention is limited to the procedures presented, this review found that surgical intervention is suitable for patients non-compliant to CPAP treatment if obstruction sites can be identified on DISE. Each study varies in preoperative and postoperative evaluation of every patient and inclusion criteria, exclusion criteria, surgical outcome, and patient follow-up time. Hence, heterogeneity exists between the included studies. However, mutual and comparable parameters were present, thus, surgical outcomes were primarily AHI and ESS, and terms such as surgical responders and surgical success were described with Sher’s criteria, providing a suitable comparison between the studies. DISE findings were essential, furthermore all studies used age, BMI, and the severity of OSA to screen patients before surgery. Some studies included clinical observations related to the Friedman staging system [49]. All studies presented in detail minor and severe adverse effects to surgery.
Weaver et al. showed that PSG parameters such as AHI does not correlate well to data on patient reported outcome (PRO) [50]. In sleep surgery, PRO is essential to address benefits of the surgical intervention. Most studies presented ESS data except for Elzayat, Süslü, Hwang, Baghat and Cammaroto. Thaler et al. reported ESS, however only 31 patients of 75 patients completed ESS measurements, hence the data was not included in the meta-analysis. Some studies included additional PRO measurement tools such as the Calgary Sleep Apnea Quality of Life Index (SAQLI) or Funtional Outcomes of Sleep Questionnaire (FOSQ) or merely Visual Analog Scale (VAS) snoring scale. This review found an overall statistically significant improvement in ESS. Lee et al. reported that ESS should not be used as a screening method in a population with sleep disorders since the method is unreliable [51]. However, this measurement of daytime sleepiness is frequently used among sleep surgeons and in CPAP therapy. Kendzerska et al. published in a systematic review evidence on the psychometric properties of ESS for describing the level of daytime sleepiness in adults and reported only high-quality studies on correlation between ESS and psychometric properties [52]. They suggested that ESS could be recommended for a group but not for individual-level comparisons. Our review found that ESS was comparable between the studies and that postoperative ESS improved. We suggest that other validated patient reported outcome questionnaires should be included in the evaluation of patients undergoing sleep surgery.
All studies included in this study reported mean values for AHI and ESS, as well for other secondary outcomes. However, the nature of surgical intervention compelled that each patient’s pre-operative and postoperative data were tested and if possible, reported individually. All studies except El-Anwar et al. and Thaler et al. reported true statistical analysis (paired-t-tests). The use of the arbitrary Sher’s criteria defined as reduction of AHI > 50% and to a value of less than 20 events per hour is the most used measurement of individual response of any sleep surgery regarding AHI. Plaza et al. [31] reported 90% surgical success when using Sher’s criteria, however only 33.3% were cured (AHI<5 events per hour) and patients with an AHI>5 were included. Furthermore, the authors found that seven patients failed surgical response and in two of these patients, AHI increased. In contrary, Thaler et al. [42] reported merely 45% surgical success using Sher’s criteria. Due to their study setup, patients with higher AHI values were included, hence mean preoperative AHI was high. A 50% reduction of AHI in patients with relatively low AHI (22.1 events per hour, Plaza et al.) compared to 50% reduction in AHI in patients with relatively high AHI (57.5 events per hour, Thaler et al.) is difficult to compare. However, the combination of PSG data, patient reported outcome, and use of Sher’s criteria can illustrate the influence of sleep surgery. Unfortunately, individual changes are not reported in these publications. We advocate that further research report individual changes regarding both PSG data and in data on patient reported outcome.
Although many surgical approaches exist, only a few therapeutic interventions were included in this review. For soft palate surgery BRP, ESP, UPPP and MRFTA is reviewed and show promising results. MRFTA is suggested to treat mild OSA, while BRP, ESP and UPPP is suggested in patients with isolated lateral wall collapse of the oropharynx regardless of maximum AHI. Moffa et. al found five different approaches to address retropalatal airway collapse in a recently published systematic review [53]. Although primary outcomes were improved after surgery, heterogeneity was high and therefore the level of evidence for these procedures are low and further randomized studies are needed. For BOT, primarily two approaches were addressed. Either the reduction and removal of lingual tissue with the use of coblation or TORS. Although resection of BOT is widely investigated, most studies are biased with either small sample sizes or short follow-up. We found that the studies of Hwang et al. [41], Bahgat et al. [38] and Babademez et al. [37] showed large reduction in AHI without significant difference between TORS, coblation, and so-called Robot ablation respectively. This concurs with Tsou et al. [54] whom recently published a systematic review and found no differences in operation time, success rate or complication rate between TORS, coblation and UAS. Decline in AHI and ESS were also comparable. We found that more studies of higher level of evidence exists when it comes to UAS, especially with a longer follow-up time, and although Babademez et. al. show promising results as a single-step BOT intervention, it was the only single-step BOT study included in this review. Furthermore, Costantino et al. published a systematic review including twelve studies with 350 patients regarding UAS and found AHI and ESS improvements similar to this review [9].
The use of UAS and thereby protrusion of the entire tongue synchronous with expiration during sleep can be considered to affect the BOT but it also affects the velum. UAS show compelling results, not only because of the reported effects on AHI and ESS, but also based upon three different studies with long follow-up. Furthermore, the benefits of UAS are that the implant can be removed if compliance is not achievable, and that the implant is tailored to each patient individually and controlled by the patient.
Single step multilevel upper airway surgery is a heterogeneous entity and hence difficult to compare. Vroegop et al found in a cohort study of 1249 patients that single level collapse appeared in 31.8% of patients and multilevel collapse appeared in 68.2% of patients during DISE [55]. The discussion of single step vs. multi-step approach is beyond the scope of this review, however, the studies included in this review were single step multilevel approaches except for Thaler et al [42]. This review found seven multilevel studies suitable for review, although they vary greatly in study design and the surgical interventions used. Cammaroto et. al used tonsillectomy, ESP, TORS BOT surgery, and septo-turbinoplasty [39], El-Anwar et al. included hyoid suspension and a specific pharyngeal suture technique introduced by the first author [40], whereas Thaler et al. combined TORS with traditional UPPP [42]. All studies showed statistically significant reduction in AHI and in ESS, if ESS was reported. Secondary outcomes were also improved. Although the studies all included DISE, the specific findings were not reported. It is therefore critical not to compare the studies regarding the surgical approaches, but to consider the fact, that clinical screening and evaluation of the patient with the use of DISE is of utmost importance before surgical approach is selected. This results in a personal and individual approach to each patient, where single step multilevel surgery should be one of these modalities. In the multilevel group, mean preoperative AHI was among the highest compared to all the studies in this review. This illustrates, that severe OSA usually is comprised by several anatomical collapses, and a multilevel approach as either single or two-step procedure seemes beneficial. In the SAMs trial by Mackay et al. 101 patients with moderate to severe OSA was randomized to either modified UPPP + RFA tongue base in a single step procedure or to ongoing medical treatment. They found a statistically significant greater reduction in AHI after surgery [56]. The SAMS trial study was excluded from this review because DISE was not performed.
Limitations
Our inclusion criteria with preliminary DISE excluded many interesting studies. Especially the criteria of minimum 40 patients excluded many interesting, but smaller studies. Studies regarding maxillomandibular advancement (MMA) surgery were excluded due to small sample size (<40 patients) or due to no preliminary DISE, although MMA surgery in minor studies have shown a great and sustained reduction in AHI in a selected group of patients with OSA and maxillary or mandibular hypoplasia [57].
Selection bias occurs when UAS studies exclude patients with BMI>32 while remaining studies include patients with BMI < 35. Higher BMI corresponds with higher AHI and tendency to complex multilevel collapse [55]. It can also be discussed whether changes in AHI and ESS may represent a proper way to measure the effect of an intervention. Especially since Plaza et al. [31], Amali et al. [34] and Babademez et al. [36] included patients with AHI>5. This makes it more difficult to measure a statistically significant change in AHI after surgery. However, for now these parameters are the best way to objectively measure pre- and postoperative results, which the presented results indicate. In the synthesis of data, a zero correlation between the pre- and post-operative measurements were assumed and hence the reported 95% confidence intervals could be broader than their actual width, since the standard deviation for the mean change in preoperative AHI to postoperative AHI could not be calculated from the reported data.
The individual approach to OSA makes it more difficult to perform randomized prospective studies in the future and increases the risk of selection bias. The tendency to primarily publish studies with a positive or statistically significant result may represent a publication bias. Gouveia et al. recently described the overall trend in obstructive sleep apnea research [58]. They reported that although the number of published studies regarding OSA increased over time, the level of evidence in published studies remain stationary. Remarkably, majority of studies published are medical research of OSA and usually otolaryngology journal articles were less likely to be grant funded. However, the level of evidence did not differ between medical publications and otolaryngology publications. The process of this systematic review, illustrate that although many publications exist, only few were included in the final appraisal with a level of evidence two to four.
Conclusion
Our review found a statistically significant reduction in AHI and in ESS after surgery when DISE was incorporated in the preoperative evaluation of OSA patients to identify the level of obstruction in UA and to decide the proper upper airway surgery in each case. The literature was primarily comprised of case series containing a limited number of patients and we noticed a wide variety of approaches to pre-operative evaluation and post-operative follow up.
Declarations
Ethical Approval and Consent to participate
Not applicable
Consent for publication
Not applicable
Availability of supporting data
Can be provided upon request.
Competing interests
None
Funding
KZ received a grant from Fund for the advancement of health research in Central Denmark Region.
Authors' contributions
Jannik Buus Bertelsen (JBB) and Kasra Zainali-Gill (KZ) and Therese Ovesen (TO) have planned the study. JBB and KZ have screened and selected the titles and abstracts of relevant studies. JBB and KZ have read the full text of the selected studies to identify studies eligible for the systematic review. JBB, KZ and TO have all contributed to the writing of the systematic review.
Acknowledgements
Not applicable
References
- Croft CB, Pringle M. Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 16 (2009): 504-549.
- Soares D, Sinawe H, Folbe AJ, et al. Lateral Oropharyngeal Wall and Supraglottic Airway Collapse Associated With Failure in Sleep Apnea Surgery. Laryngoscope 122 (2012): 19687.
- Rabelo FAW, Braga A, Küpper DS, et al. Propofol-induced sleep: Polysomnographic evaluation of patients with obstructive sleep apnea and controls. Otolaryngol - Head Neck Surg 142 (2021): 218-224.
- Borek RC, Thaler ER, Kim C, et al. Quantitative airway analysis during drug-induced sleep endoscopy for evaluation of sleep apnea. Laryngoscope 122 (2011): 2592-2599.
- Peppard PE, Young T, Barnet JH, et al. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 177 (2013): 1006-1014.
- Heinzer R, Vat S, Marques-Vidal P, et al. Prevalence of sleep-disordered breathing in the general population: THE HypnoLaus study. Lancet Respir Med 3 (2015): 310-318.
- Rotenberg BW, Murariu D, Pang KP. Trends in CPAP adherence over twenty years of data collection: a flattened curve (2016).
- Rosenberg R, Doghramji P. Optimal treatment of obstructive sleep apnea and excessive sleepiness. Adv Ther 26 (2009): 295-312.
- Costantino A, Rinaldi V, Moffa A, et al. Hypoglossal nerve stimulation long-term clinical outcomes: a systematic review and meta-analysis. Sleep Breath 24 (2020): 399-411.
- Justin GA, Chang ET, Camacho M, et al. Transoral Robotic Surgery for Obstructive Sleep Apnea: A Systematic Review and Meta-Analysis. Otolaryngol Neck Surg 154 (2016): 835-846.
- Miller SC, Nguyen SA, Ong AA, et al. Transoral robotic base of tongue reduction for obstructive sleep apnea: A systematic review and meta-analysis. Laryngoscope 127 (2017): 258-265.
- Sundaram S, Lim J, Lasserson TJ. Surgery for obstructive sleep apnoea in adults. Cochrane Database Syst Rev (2005)
- Werz SM, Pfeifle M, Schrader F, et al. Surgery for obstructive sleep apnoea in adults. Cochrane Database Syst Rev (2017).
- Sher AE, Schechtman KB, Piccirillo JF. The efficacy of surgical modifications of the upper airway in adults with obstructive sleep apnea syndrome. Sleep 19 (1996): 156-177.
- Aromataris E MZ. JBI Manual for Evidence Synthesis (2020)
- Lockwood C, Porrit K, Munn Z, et al. JBI Manual for Evidence Synthesis (2020).
- Ouzzani M, Hammady H, Fedorowicz Z, et al. Rayyan-a web and mobile app for systematic reviews. Syst Rev 5 (2016): 210.
- Munn Z, Aromataris E, Tufanaru C, et al. The development of software to support multiple systematic review types: the Joanna Briggs Institute System for the Unified Management, Assessment and Review of Information (JBI SUMARI). JBI Evid Implement 17 (2019).
- Hutton B, Salanti G, Caldwell DM, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann Intern Med 162 (2015): 777-784.
- Fujita S. UPPP for sleep apnea and snoring. Ear Nose Throat J 63 (1984): 227-235.
- Browaldh N, Bring J, Friberg D. SKUP3: 6 and 24 months follow-up of changes in respiration and sleepiness after modified UPPP. Laryngoscope 128 (2018): 1238-1244.
- Pang KP, Woodson BT, Woodson B. Expansion sphincter pharyngoplasty: a new technique for the treatment of obstructive sleep apnea. Otolaryngol Head Neck Surg 137 (2007): 110-114.
- Vicini C, Hendawy E, Campanini A, et al. Barbed reposition pharyngoplasty (BRP) for OSAHS: a feasibility, safety, efficacy and teachability pilot study. “We are on the giant’s shoulders.” Eur Arch Oto-Rhino-Laryngology 272 (2015): 3065-3070.
- Powell NB, Riley RW, Troell RF, et al. clinical investigations Radiofrequency Volumetric Tissue Reduction of the Palate in Subjects With Sleep-Disordered Breathing 113 (1998): 6358.
- Wischhusen J, Qureshi U, Camacho M. Laser-assisted uvulopalatoplasty (LAUP) complications and side effects: A systematic review [Internet]. Vol. 11, Nature and Science of Sleep. Dove Medical Press Ltd 8 (2019): 59-67.
- Chang ET, Kwon YD, Jung J, et al. Genial tubercle position and genioglossus advancement in obstructive sleep apnea (OSA) treatment: a systematic review. Maxillofac Plast Reconstr Surg 41 (2021): 34.
- Powell N, Riley R, Guilleminault C. Radiofrequency tongue base reduction in sleep-disordered breathing: A pilot study. Otolaryngol Head Neck Surg 120 (1999): 656-664.
- Handler E, Hamans E, Goldberg AN, Mickelson S. Tongue suspension. Laryngoscope 14 (2014): 329-336.
- Vicini C, Dallan I, Canzi P, et al. Transoral robotic tongue base resection in obstructive sleep apnoea-hypopnoea syndrome: a preliminary report. ORL J Otorhinolaryngol Relat Spec 72 (2010): 22-27.
- Eisele DW, Smith PL, Alam DS, et al. Direct hypoglossal nerve stimulation in obstructive sleep apnea. Arch Otolaryngol Head Neck Surg 123 (1997): 57-61.
- Plaza G, Baptista P, O’Connor-Reina C, et al. Prospective multi-center study on expansion sphincter pharyngoplasty. Acta Otolaryngol 139 (2019): 219-222.
- Hong SN, Kim HG, Han SY, et al. Indications for and outcomes of expansion sphincter pharyngoplasty to treat lateral pharyngeal collapse in patients with obstructive sleep apnea. JAMA Otolaryngol Neck Surg 145 (2019): 405-412.
- Süslü AE, Katar O, Külekçi Ç. Supine or non-supine apnea; which can be treated better with expansion sphincter pharyngoplasty? Auris Nasus Larynx 49 (2022): 431-436.
- Amali A, Motiee-Langroudi M, Saedi B, et al. A comparison of uvulopalatopharyngoplasty and modified radiofrequency tissue ablation in mild to moderate obstructive sleep apnea: A randomized clinical trial. J Clin Sleep Med 13 (2017): 5369.
- Elzayat S, El-Sobki A, El-Deeb ME, et al. Managing obstructive sleep apnea patients with CPAP failure with a novel Lateral Pharyngoplasty as a stand-alone procedure. Am J Otolaryngol - Head Neck Med Surg 41 (2020): 3698.
- Babademez MA, Gul F, Teleke YC. Barbed palatoplasty vs. expansion sphincter pharyngoplasty with anterior palatoplasty. Laryngoscope 130 (2020): 9568.
- Babademez MA, Gul F, Sancak M, et al. Prospective randomized comparison of tongue base resection techniques: Robotic vs coblation. Clin Otolaryngol 44 (2019): 989-996.
- Bahgat A, Bahgat Y, Alzahrani R, et al. Transoral Endoscopic Coblation Tongue Base Surgery in Obstructive Sleep Apnea: Resection versus Ablation. ORL 82 (2020): 201-208.
- Giovanni C, Giuseppe M, Matteo C, et al. Trans-Oral Robotic Tongue Reduction for OSA: Does Lingual Anatomy Influence the Surgical Outcome? J Clin Sleep Med 14 (2022): 1347-1351.
- El-Anwar MW, Amer HS, Askar SM, et al. Could Nasal Surgery Affect Multilevel Surgery Results for Obstructive Sleep Apnea? J Craniofac Surg 29 (2018): 1897-1899.
- Hwang CS, Kim JW, Kim JW, et al. Comparison of robotic and coblation tongue base resection for obstructive sleep apnoea. Clin Otolaryngol 43 (2018).
- Thaler ER, Rassekh CH, Lee JM, et al. Outcomes for multilevel surgery for sleep apnea: Obstructive sleep apnea, transoral robotic surgery, and uvulopalatopharyngoplasty. Laryngoscope 126 (2016): 266-269.
- Tsou YA, Hsu CC, Shih LC, et al. Combined transoral robotic tongue base surgery and palate surgery in obstructive sleep apnea syndrome: Modified uvulopalatopharyngoplasty versus barbed reposition pharyngoplasty. J Clin Med 10 (2021).
- Turhan M, Bostanci A. Robotic Tongue-Base Resection Combined With Tongue-Base Suspension for Obstructive Sleep Apnea. Laryngoscope 130 (2020).
- Huntley C, Kaffenberger T, Doghramji K, et al. Upper Airway Stimulation for Treatment of Obstructive Sleep Apnea: An Evaluation and Comparison of Outcomes at Two Academic Centers. J Clin Sleep Med 13 (2022): 1075-1079.
- Mulholland GB, Dedhia RC. Success of Hypoglossal Nerve Stimulation Using Mandibular Advancement During Sleep Endoscopy. Laryngoscope 130 (2020).
- Steffen A, Sommer JU, Hofauer B, et al. Outcome after one year of upper airway stimulation for obstructive sleep apnea in a multicenter German post-market study. Laryngoscope 128 (2018): 509-515.
- Strollo PJ, Soose RJ, Maurer JT, et al. Upper-Airway Stimulation for Obstructive Sleep Apnea. N Engl J Med 370 (2014):139-149.
- Friedman M, Salapatas AM, Bonzelaar LB. Updated Friedman Staging System for Obstructive Sleep Apnea. Adv Otorhinolaryngol 80 (2017): 41-48.
- Weaver EM, Woodson BT, Steward DL. Polysomnography indexes are discordant with quality of life, symptoms, and reaction times in sleep apnea patients. Otolaryngol neck Surg Off J Am Acad Otolaryngol Neck Surg 132 (2005): 255-262.
- Lee JL, Chung Y, Waters E, et al. The Epworth sleepiness scale: Reliably unreliable in a sleep clinic population. J Sleep Res 29 (2020): e13019.
- Kendzerska TB, Smith PM, Brignardello-Petersen R, et al. Evaluation of the measurement properties of the Epworth sleepiness scale: a systematic review. Sleep Med Rev 18 (2014): 321-331.
- Moffa A, Rinaldi V, Mantovani M, et al. Different barbed pharyngoplasty techniques for retropalatal collapse in obstructive sleep apnea patients: a systematic review. Sleep Breath 24 (2020): 1115-1127.
- Tsou YA, Chang WD. Comparison of transoral robotic surgery with other surgeries for obstructive sleep apnea. Sci Reports 10 (2020): 18163.
- Vroegop AV, Vanderveken OM, Boudewyns AN, et al. Drug-induced sleep endoscopy in sleep-disordered breathing: Report on 1,249 cases. Laryngoscope (2014).
- Carney AS, Antic NA, Catcheside PG, et al. Sleep Apnea Multilevel Surgery (SAMS) trial protocol: A multicenter randomized clinical trial of upper airway surgery for patients with obstructive sleep apnea who have failed continuous positive airway pressure. Sleep 42 (2019).
- Boyd SB, Walters AS, Waite P, et al. Long-Term Effectiveness and Safety of Maxillomandibular Advancement for Treatment of Obstructive Sleep Apnea. J Clin sleep Med JCSM Off Publ Am Acad Sleep Med 11 (2015): 699-708.
- Gouveia CJ, Zaghi S, Awad M, et al. Publication trends and levels of evidence in obstructive sleep apnea literature. Laryngoscope 128 (2018): 2193-2199.
