Survey of the Level of Preparedness and Fears among Staff of the Department of Anaesthesia Regarding the Management of COVID-19 Patients in Zaria-Nigeria
Article Information
Yakubu SY*, Idris ME, Yakubu H, Muhammad ST, Yunus AA, Lawal II
Department of Anaesthesia, Ahmadu Bello University Teaching Hospital, Shika-Zaria, Nigeria
*Corresponding Author: Yakubu SY, Department of Anaesthesia, Ahmadu Bello University Teaching Hospital, Shika-Zaria, Nigeria.
Received: 04 December 2021; Accepted: 13 December 2021; Published: 15 December 2021
Citation: Yakubu SY, Idris ME, Yakubu H, Muhammad ST, Yunus AA, Lawal II. Survey of the Level of Preparedness and Fears among Staff of the Department of Anaesthesia Regarding the Management of COVID-19 Patients in Zaria-Nigeria. Anesthesia and Critical Care 3 (2021): 88-94.
View / Download Pdf Share at FacebookAbstract
Introduction
Coronavirus disease (COVID-19) is a respiratory infection caused by a novel coronavirus first observed in Wuhan China in December 2019. Some developed countries were caught unaware by the pandemic and faced a lack of intensive care unit (ICU) beds. The challenge was dire in Africa due to an inadequate number of health personnel, ICU, and ventilators. This survey was to determine the level of preparedness and fears among anaesthesia staff regarding the management of COVID-19 patients in Zaria.
Materials and Methods
In April 2020 structured questionnaires were sent out by WhatsApp to all anaesthesia staff. Demographic data, professional role, level of preparedness, availability of working materials/equipment, fear of COVID-19, perceived level of stress, stigmatization, and the willingness or otherwise to volunteer in the management of COVID-19 patients were collated. Ethics approval was waived and participants consented. Data were analyzed using SPSS version 21. The level of significance was set at p < 0.05.
Results
All 45 respondents had no life insurance. Forty-four (97.8%) lacked access to COVID-19 testing while 36 (80%) have not received any training on COVID-19 and the use of personal protective equipment. Twenty-eight of 43 staffs were not prepared to participate in the management of COVID-19 patients.
Conclusions
This survey showed that most staff had no life insurance, lacked access to COVID-19 testing and training. The fear of being infected with COVID-19 was high and two-thirds were not prepared to participate in the management of infected patients. However, only half became stressed up durin
Keywords
Level of preparedness, Fears, Anaesthesia, Staff, Management of COVID-19
Article Details
1. Introduction
Coronavirus disease 2019 (COVID-19) is a respiratory infection caused by a novel coronavirus first observed in Wuhan China in December 2019 [1]. Some developed countries were caught unaware by the disease and faced a lack of intensive care unit (ICU) beds among others [2]. The challenge was dire in Africa due to inadequate number of health personnel, intensive care units and ventilators. The high level of poverty, overcrowding and infectious diseases such as malaria, HIV and tuberculosis further complicated things [3]. The Johns Hopkins Center for Health Security publication reported Africa as least prepared among other continents to respond to health emergencies, provide treatment for the sick and protection for health personnel [4]. The fear being entertained by health workers in Nigeria concerning COVID-19 was because of shortage of protective equipment in hospitals and poor infection prevention and control policy [5]. Studies have shown that healthcare staff in COVID-19 treatment centres suffered stigmatization from friends and family members due to fear of contracting the disease [6, 7]. A study in Nigeria reported that “over 65% of healthcare workers strongly agreed that their willingness to go to work was affected by the COVID-19 pandemic”. They went further to state that “majority of participants 162 (54%) went to work four days in a week during the first wave of the pandemic in comparison to 226 (75.33%) who went to work for five days during the pre-Covid-19 period” [5]. This data was collected to determine the level of preparedness and fears among department of anaesthesia staff regarding the management of COVID-19 patients in a low resource tertiary hospital in Zaria, Nigeria. Study was restricted to these staff because they were more likely to get exposed to COVID-19 patients through their work in the ICU and operating theatres. Information obtained was used to request for missing equipment from the hospital management, address shortcomings and to allay the fears of staff during the first wave of COVID-19 pandemic.
2. Materials and Methods
During the period April 11-18, 2020 structured questionnaires were sent out by WhatsApp to all staff in the anaesthesia department of Ahmadu Bello University Teaching Hospital (ABUTH) Zaria, Nigeria. They included physician anaesthetists (doctors), nurse anaesthetists, intensive care nurses, biomedical engineers (anaesthetic technicians) and health assistants (support staff) and those who consented filled and returned the questionnaires. ABUTH Zaria is an 800 bedded tertiary healthcare centre in the North-West region of Nigeria. It has 5 ICU beds, 12 operating rooms and provides specialist training to various cadres of healthcare workers. Requirement for Ethics approval was waived by the Hospitals Ethics Committee to enable documentation of the situation of things in anaesthesia department during the first wave of COVID-19 pandemic. All participants of the survey consented to the filling of questionnaires and reporting of findings. Data obtained included age, gender, marital status, professional role, level of preparedness, availability of working materials/equipment, fear of COVID-19, perceived level of stress, stigmatization and the willingness or otherwise to volunteer in the management of COVID-19 patients. Information collected were analyzed using SPSS version 21. The level of significance was set at p < 0.05.
3. Results
Fifty questionnaires were sent out and 45 responses were received. The Mean Age± SD of participants was 40.25± 9.62. The demographic characteristics of respondents were as shown in Table 1. There were 22 (48.9%) females and 23 (51.1%) males. All 45 respondents stated that they were not having a life insurance. Forty four (97.8%) lacked access to COVID-19 testing while 36 (80%) have not received any training on COVID-19 and the use of personal protective equipment (PPE). In addition 35 (77.8%) of 45 participants said that elective operations were suspended while 38 (88.4%) of 43 respondents stated that emergency operations were continued during the first wave of COVID-19.
|
Characteristics |
Frequency |
Percent |
|
Female |
22 |
48.9 |
|
Male |
23 |
51.1 |
|
Total |
45 |
100 |
|
Marital Status |
||
|
Single |
11 |
24.4 |
|
Married |
34 |
75.6 |
|
Total |
45 |
100 |
|
Professional role |
||
|
Health Assistant |
5 |
11.1 |
|
Biomedical |
6 |
13.3 |
|
ICU Nurses |
11 |
24.4 |
|
Anaesthetic Nurses |
4 |
8.9 |
|
Registrar |
8 |
17.8 |
|
Senior Registrar |
7 |
15.6 |
|
Consultant |
1 |
2.2 |
|
Not indicated |
3 |
6.7 |
|
Total |
45 |
100 |
Table 1: Demographic characteristics of respondents
|
Frequency |
Percent |
|
|
Do you have hand sanitizers for use at work |
||
|
No |
13 |
28.9 |
|
Yes |
32 |
71.1 |
|
Total |
45 |
100 |
|
Do you have N95 masks for use during intubation |
||
|
No |
37 |
82.2 |
|
Yes |
8 |
17.8 |
|
Total |
45 |
100 |
|
Do you have other PPEs for use while on duty |
||
|
No |
43 |
95.6 |
|
Yes |
2 |
4.4 |
|
Total |
45 |
100 |
Table 2: Availability of working materials and personal protective equipment (PPEs)
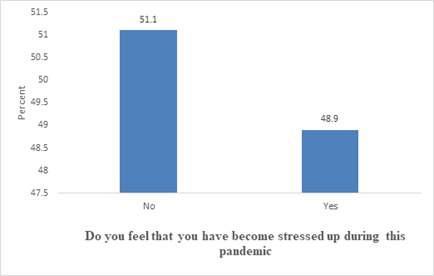
Table 2 above showed that while 32 (71.1%) of staff agreed that they had hand sanitizers for use at work; 43 (95.6%) indicated that other PPE’s for use while on duty were inadequate (p < 0.001). In addition, 90% of respondents said that there were no enough ventilators and other necessary equipment for the management of COVID-19 patients in the health facility. Regarding the fear of COVID-19 forty participants expressed the concern of being infected while on duty (p < 0.001) while 5 staff did not respond to the question. Furthermore, 28 of 30 staff that responded to the question on whether they fear transmission of infection to family members do so in the affirmative. Fifteen out of 45 participants answered the question on working hours becoming long during the pandemic. Ten (66.7%) of them agreed that their working hours have increased. On the issue of communication among staff in the department concerning COVID-19, forty four out of 45 staff commented. Twenty five (56.8%) stated that there was good communication among staff during this pandemic. However, only 7 (15.6%) participants indicated that they have a space for self-isolation for use if the need arises. Twenty three (51.1%) of staff stated that they became stressed up during the COVID-19 pandemic as shown in Figure 1.
Thirty two (71.1%) respondents reported that family members did not avoid associating with them because of fear of contracting the disease (p= 0.007). Twenty eight of 43 staff said that they were not prepared to participate in the management of COVID-19 patients.
4. Discussion
This study found that no staff in the department had a life insurance and almost all lacked access to COVID-19 testing. Majority of staff had also not received training on the disease and the use of personal protective equipment as at the time of study. In a similar study by Ogolodom and co-workers on the Knowledge, Attitudes and Fears of Healthcare Workers towards the Corona Virus Disease pandemic in South-South, Nigeria; authors reported that 61% of healthcare workers saw themselves at the risk of being infected with COVID-19 while 62% of them indicated that there was inadequate safety in the hospital coupled with lack of insurance policy which posed a challenge to the efficient care of patients [5]. Our study involved the various staff of anaesthesia department in one institution while the work of Ogolodom and colleagues was multi-center that involved various categories of healthcare workers which added to the strength of their findings. The lack of testing was a challenge in most centres in Nigeria including the developed world during the first wave of COVID-19 disease [8]. In our hospital even elective operations were initially taken without testing patients for corona virus in order to know their status. Most of elective surgical procedures such as major tumour resections, urological surgeries and myomectomies were suspended in our centre but emergency operations like emergency caesarian section, laparatomy and trauma cases among others continued. The level of knowledge of a disease has been shown to affect ones understanding of the risk of contracting the disease [9]. The same situation applies to COVID-19. Receiving training on the disease by healthcare workers will assist in empowering them with the necessary skills of safety precautions to take while treating patients to avoid being infected. Majority of our staff had no PPE for use while on duty as at the time of study. The importance of provision of PPE’s for use while treating COVID-19 patients cannot be over emphasized. Many staff feared the transmission of infection to their family members as only few of them had a place for self isolation when the need arises. The importance of the availability of ventilators to manage critically ill patients cannot be taken for granted. The World Economic Forum reported in March 2020 that Africa had the lowest capacity to providing critical and intensive care in the world [10]. While working hours have increased for some staff members posted to the COVID-19 isolation centre, majority of staff in the department were not affected. In fact, some of our supporting staffs were asked to stay at home to help reduce traffic in the hospital. The communication among staff has been good particularly during this pandemic. This has served as an excellent means of delivering the best of care to our patients during this difficult period [11]. Half of the staffs reported being stressed up during the pandemic with only one third who witnessed stigmatization from family members. The reverse was the case in a study by Uvais et al on COVID-19 related stigma and perceived stress among dialysis staff. They documented that 54.6% of participants suffered significant stigma while 36.1% had stress. Their study had 335 respondents compared to ours that had only 45 participants [7]. Two thirds of staffs in anaesthesia department were not prepared to participate in the management of COVID-19 because of fear of infection and lack of safety, protection and working facilities. This situation cuts across various cadres of participants and was an indication that the hospital needed to be proactive in the provision of working materials and being ready for emergency situations such as COVID-19. This study is limited because the data obtained cannot be generalized to other hospitals. It only described the situation at the Ahmadu Bello University Teaching Hospital Zaria, Nigeria as at April 2020.
5. Conclusions
This survey showed that most staff had no life insurance, lacked access to COVID-19 testing and training. The fear of being infected with COVID-19 was high and two-thirds were not prepared to participate in the management of infected patients. However, only half became stressed up during the period.
Acknowledgements
We wish to thank all the participants of this survey and those who assisted in one way or the other with the study.
Competing interests
No conflicts of interest to declare
Funding
No funding was received for this survey
References
- Team NCPERE. Vital surveillances: the epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) - China. China CDC Weekly 2 (2020): 113-22.
- Rosenbaum L. Facing COVID-19 in Italy - ethics, logistics, and therapeutics on the epidemic’s front line. N Engl J Med 382 (2020): 1873-1875.
- Lucero-Prisno DE, Adebisi YA, Lin X. Current efforts and challenges facing responses to 2019-nCoV in Africa. Glob health res policy 5 (2020): 21.
- Johns Hopkins Center for Health Security. Global Health Security Index (2020).
- Ogolodom MP, Mbaba AN, Alazigha N, et al. Knowledge, attitudes and fears of healthcare workers towards the Corona Virus Disease (COVID-19) Pandemic in South-South. Nigeria. Health Sci J (2020): 1-12.
- Uvais NA, Shihabudheen P, Bishurul Hafi NA. Perceived stress and stigma among doctors working in COVID-19-designated hospitals in India. Prim Care Companion CNS Disord 22 (2020): 20-27.
- Uvais NA, Aziz F, Hafeeq B. COVID-19-related stigma and perceived stress among dialysis staff. J Nephrol (2020).
- Nguyen J. Who’s getting access to COVID-19 testing? Marketplace.
- Janjua NZ, Razaq M, Chandir S, Rozi S, et al. Poor knowledge- Predictor of nonadherence to universal precautions for blood borne pathogens at first level care facilities in Pakistan. BMC Infectious Diseases 7 (2007): 1-11.
- World Economic Forum (2020).
- Ratna H. The importance of effective communication in healthcare practice. Harvard Public Health Review (2019): 23.