Surgical Treatment of Neovascular Glaucoma with Ex-PRESS Glaucoma Shunt
Article Information
Cenk Zeki Fikret, Nil Irem Ucgun
1Ankara City Hospital, Department of Ophthalmology, Ankara, Turkey
2University of Health Sciences, Ankara City Hospital, Department of Ophthalmology, Ankara, Turkey
*Corresponding author: Cenk Zeki Fikret, Ankara City Hospital, Department of Ophthalmology, Ankara, Turkey
Received: 08 April 2022; Accepted: 18 April 2022; Published: 25 April 2022
Citation: Cenk Zeki Fikret, Nil Irem Ucgun. Surgical Treatment of Neovascular Glaucoma with Ex-PRESS Glaucoma Shunt. Journal of Ophthalmology and Research 5 (2022): 66-73
View / Download Pdf Share at FacebookAbstract
Purpose: To compare the efficacy and safety profile of deep sclerectomy combined with Ex-PRESS shunt versus Ex-PRESS shunt surgery in eyes with neovascular glaucoma. Methods: Patients with neovascular glaucoma secondary to proliferative diabetic retinopathy who underwent Ex-PRESS glaucoma filtration surgery with or without deep sclerectomy were evaluated retrospectively. Twenty eyes with neovascular glaucoma secondary proliferative diabetic retinopathy were included in our study. Intravitreal bevacizumab injection and panretinal photocoag-ulation were applied to these eyes. Iris and angle neovascularization were achieved preoperatively. In spite of full antiglaucomatous treatment whose intraocular pressures were 21mm Hg and above were taken to surgery. Patients were randomly divided into two groups. Group A (10 patients) underwent deep sclerectomy combined with implantation of Ex-PRESS drainage device, group B (10 patients) underwent only Ex-PRESS glaucoma filtration surgery. Primary outcome measurements were intraocular pressure (IOP) and the number of antiglaucomatous medications at the first year follow up visit. Results: There was no difference in IOP between the groups at the first 2 months postoperatively (p>0.05). There was no need for antiglaucomatous medication in all groups in the first 2 months. Antiglaucomatous medication was administered to 2 patients in group A and to 4 patients in group B in the third month. IOP values were lower in group A than group B at the third and sixth months (p<0.05). At the end of the first year, ≤18 mm Hg IOP rate was found 80% in group A and 60% in group B without medication. Conclusions: Ex-PRESS shunt surgery demonstrated to be an effective treatment in eyes with neovascular glaucoma at the first year follow-up period. Ex-PRESS drainage device implantation with deep sclerectomy increased surgical success.
Keywords
Ex-PRESS shunt, deep sclerectomy, neovascular glaucoma, diabetic retinopathy
Ex-PRESS shunt articles, deep sclerectomy articles, neovascular glaucoma articles, diabetic retinopathy articles
Article Details
1. Introduction
Blindness in diabetic patients is a consequence of proliferative diabetic retinopathy, while neovascular glaucoma is responsible for approximately 5% of blindness in diabetics. When vascular proliferation occurs, it primarily appears at the pupillary border, but it can be seen first in the anterior chamber angle. Vessels run from the base of the iris and cover the ciliary body band, scleral spur, and finally the trabecular meshwork. This causes intraocular pressure (IOP) elevation commonly. Intraocular pressures may rise to 40-60 mm Hg. [1]
The Ex-PRESS P-50 model used in our study was 2.6 mm long with a 50 µm internal diameter. Ex-PRESS is a valveless, stainless steel glaucoma drainage device. Ex-PRESS glaucoma drainage device implantation supplies better postoperative perform-ance and is safer than trabeculectomy alone in neovascular glaucoma. The usage of adjuvant theraphy such as bevacizumab also affects the success of surgeries. [2-4]
Bevacizumab is a humanized monoclonal antibody and binds to all isoforms of vascular endothelial growth factor (VEGF)’s. VEGF causes proliferation in endothelial cells and this leads to formation of new blood vessels. Bevacizumab blocks the interaction between VEGF-A and its receptors on the surface of endothelial cells, which initiates the intercellular signaling pathway. It has been reported that iris neovascularization regresses after intravitreal bevacizumab injections. [5, 6]
In the literature, surgical success is higher in patients who underwent deep sclerectomy with Ex-PRESS shunt than those who only underwent Ex-PRESS shunt. [7] However, according to our reviews, results of deep sclerectomy with Ex-PRESS shunt in eyes with neovascular glaucoma have not been published in the literature. The aim of our study to evaluate the effects of deep sclerectomy with Ex-PRESS implantation in patients with neovascular glaucoma on surgical success.
2. Patients and Methods
This study was performed in accordance with the Declaration of Helsinki and Lokal Ethics Committee approved the protocol for the study (E1-20-1382). Written informed consent was obtained from all patients. Twenty eyes of 20 diabetic patients with neovascular glaucoma secondary to proliferative diabetic retinopathy were included in our study. Argon laser panretinal photocoagulations were applied to the patients. An intravitreal injection of 0.05ml bevacizumab (Altuzan 100mg/4ml, Roche) was performed 7 days before the surgery. 0.3 mg / ml bimatoprost and 6.8 mg / ml timolol maleate drug combination, 10 mg / ml brinzolamide and 1.5 mg / ml brimonidine tartrate antiglaucomatous drugs were administered. Despite full antiglaucomatous treatment and iris, angle neovascularization regression whose intraocular pressures were 21 mm Hg and above were taken to surgery. Patients were randomly divided into two groups. Patients with ocular trauma history and other intraocular surgery were excluded to the study. All surgeries were performed by the same experienced surgeon (CZF). Ex-PRESS glaucoma drainage device implantation was performed with deep sclerectomy in some of the patients (Group A), and Ex-PRESS glaucoma drainage device implantation surgery without sclerectomy was performed in the other part (Group B).
Postoperative examinations were held in 1st week, 1st, 2nd, 3rd, 6th months and first year. Complete surgical success was determined as an eye with IOP ≤18 mm Hg but without medication. Partial surcical success was determined as IOP ≤18 mm Hg with decreased number of antiglaucomatous drugs needed. IOP below 7 mm Hg was accepted as failure criteria because of hypotonia. IOP was measured in the morning using applanation tonometry.
Deep sclerectomy with Ex-PRESS (Alcon Laboratories, Fort Worth, TX, USA) filtration device P-50 model implantation: Fornix-based conjunctiva and tenon's membrane dissection was performed. 5×5 mm2 in size one-third of the scleral thickness superficial scleral flap was dissected at 12 o'clock until the transparent cornea. Triangular sponge soaked with Mitomycin-C (MMC) (0.2 mg/mL) is placed under the superficial scleral flap for 2 minutes then irrigated by 20 ml balanced salt solution (BSS). Later, a 4×4-mm2 deep sclera flap is fashioned to create a trabeculodescemet membrane. The extent of the excision is up to the Schlemm’s canal. A 4 × 4 mm2 deep scleral flap is then shaped up to the Schlemm canal to create a trabeculodesemet membrane. The deep flap is excised. Schlemm’s canal outher wall was extracted and aqueous percolation ‘’oozing’’ occured. The anterior chamber is entered with a 25 G needle under the scleral flap parallel to the iris plane and an Ex-press drainage device (P50 model) is placed. The superficial scleral flap was sutured to the sclera with 10-0 nylon sutures at the two corners. After controlling the presence of flow by applying BSS to the anterior chamber, the tenon and conjunctiva were sutured continuously with 8-0 vicryl suture.
Ex-PRESS filtration device implantation: The surgical procedures are the same, only deep sclerectomy was not performed. A 25 gauge needle is inserted to the anterior chamber parallel to the iris plane at the center of the blue line. Ex-press drainage device (P50 model) was implanted from this point. All data were entered into SPSS ( version 17) Windows 15.0. Mann-Whitney U test was used for statistical analysis. All parameters used in our study is written as mean ± standard deviation (SD). Significance level was taken as p<0,05.
3. Results
Group A (Deep sclerectomy with Ex-PRESS filtration device implantation) consisted of 10 patients (4 males and 6 females), whereas group B (Ex-PRESS filtration device implantation) consisted of 10 patients (3 males and 7 females). The mean age was 59.5 ± 18.4 years in group A and 62.7 ± 15.2 years in group B (p=35). Preoperative and postoperative IOP values are shown in Table 1. At the second, third, sixth months and first year, IOP values were statistically lower in group A than in group B (p<0.05).
Table 1: Preoperative and postoperative IOP values, *p<0.05 value was considered statistically significant.
|
Time |
Deep Sclerectomy+ Ex-PRESS IOP mm Hg, mean ±SD n=10 |
Ex-PRESS IOP mm Hg, mean ±SD n=10 |
P value* |
|
Preoperative |
33.4±9.7 |
31.7±8.6 |
0.25 |
|
Postoperative 1. week |
11.7±5.4 |
13.9±4.8 |
0.37 |
|
Postoperative 1. month |
9.7±4.4 |
10.6±4.1 |
0.26 |
|
Postoperative 2. month |
13.7±3.5 |
15.8±5.7 |
0.04 |
|
Postoperative 3. month |
14.9±4.8 |
17.9±4.6 |
0.03 |
|
Postoperative 6. month |
15.2±2.6 |
17.3±2.6 |
0.03 |
|
Postoperative 1. year |
16.5±1.1 |
17.8±2.1 |
0.02 |
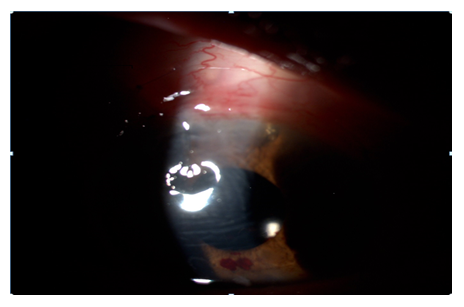
Complete success rate has been determined as 80% for group A and 60% for group B at the end of first year. Partial success rate is evaluated as 20% in group A and 40% in group B (p=0.04). Needling was applied to two patients in group B in the second month. In the third month, 10 mg / ml brinzolamide treatment was initiated in 2 patients in group A and 4 patients in group B, and IOP measurements were achieved to be 18 mm Hg and below. Following these postoperative additional treatments no failure was observed in either group at the end of first year. Shallow anterior chamber, hypotony, choroidal detachment, contact between the device and iris or corneal endothelium were not encountered after the surgery. Spontaneously absorbed grade 1 hyphema developed in one patient in each group (Figure 1).
4. Discussion
- The treatment of neovascular glaucoma requires immediate treatment of concomitant diseases such as proliferative diabetic retinopathy. It is difficult to control neovascular glaucoma. Regression of neovascularization in the iris and angle should be aimed with panretinal photocoagulation and intravitreal anti-VEGF injections. Topical β-blockers, topical α-agonists, topical and oral carbonic anhydrase inhibitors may be useful in IOP control by reducing aqueous production. Prostaglandin analogs act by increasing uvea-scleral outflow. However, their effects are limited in patients with neovascular glaucoma due to the fibrovascular structures at the angle. Surgical treatment is required in patients whose medical treatments are not sufficient. [1, 5] We also applied intravitreal bevacizumab injection and panretinal photocoagulation therapy for regression of iris and angle neovascularization in all eyes with neovascular glaucoma before surgery.
- Kawabata et al. performed Ahmed glaucoma valve implantation or trabeculectomy after intravitreal ranibizumab 7 days before surgery and found the success rate of both to be similar (52.2% vs 45.5%) [8]. Shen et al. reported that the success results of Ahmed glaucoma valve implantation and trabeculectomy with mitomycin C were similar (60% vs 55%) in neovascular glaucoma treatment at the end of 2 years [9].
- The success rates are low for both surgeries in eyes with neovascular glaucoma when glaucoma drainage devices were compared with cyclophotocoagulation. There was no difference between IOP lowering effects and failure rates. Light perception loss rate was lower in the glaucoma drainage device group [10]. Kawabata et al. found that, Ex-PRESS mini shunt surgery was less effective than trabeculectomy, but is a safer surgical aproach for neovascular glaucoma. Complications such as bleb leaks and hyphema were less common in patients treated with Ex-PRESS shunt device.[3]
- A number of studies have shown that the IOP lowering effect of Ex-PRESS shunt device surgery is similar to trabeculectomy, but the cause is not understood. However, complication rates were found lower in eyes with Ex-PRESS implantation. [11] In our study, grade 1 hyphema developed and that was absorbed spontaneously in one patient in each group. Apart from this, there was no preoperative or postoperative complication. EX-PRESS drainage device obtains predictable intraocular pressure reduction in the early postoperative period [12]. Ex-PRESS shunt is a safe method that enables us to obtain IOP below 18 mm Hg without causing hypotonia [13]. Post-operative hypotonia did not develop in our patients. Kato et al. found no difference in IOP reduction level, need for postoperative treatment and success rate of surgery between patients who underwent Ex-PRESS placement and trabeculectomy.
- The incidence of postoperative complications, especially hyphema rate was found lower in patients with Ex-PRESS glaucoma device. Regarding these findings, they suggest the implantation of Ex-PRESS in patients predisposed to bleeding or in eyes with neovascular glaucoma [14]. Puerto et.al. Compared non-penetrating deep sclerectomy and Ex-PRESS glaucoma shunt surgery. They reported that these tecniques had a nearly 25% IOP lowering effect and no difference in success rates [15].
- Kozobolis et al. investigated that the success rates of Ex-PRESS shunt device implantation with modified deep sclerectomy were higher than trabeculectomy in primary open angle glaucoma. (92.6% vs 68.2%) [16]. Fraczkiewicz-Skok et al. reported that deep sclerectomy increases surgical success in Ex-PRESS shunts implanted simultaneously with phacoemulsification. It has been explained that the intrascleral space created during this surgery can facilitate the outflow of the aqueous humor [7].
- The main resistance to aqueous humor outflow is at the level of the trabecular meshwork in glaucoma, and the outflow can be significantly improved by surgically removing this resistance [17]. Ex-PRESS mini glaucoma shunt has been reported to be a less invasive surgical procedure compared to conventional trabeculectomy. Because of eliminating the need for iridectomy by providing adequate scleral fistula. It has been reported to be advantageous in neovascular glaucoma [18]. Although Ex-PRESS shunt surgery can be performed safely, there are limited publications regarding its usage in neovascular glaucoma. According to our study applying deep sclerectomy in Ex-PRESS drainage device implantation increased surgical success with low postoperative complication rates.
Conflict of Interest:
None of the authors has any conflict of interest.
Funding:
The authors do not have any funding support for the study.
Conflict of Interest:
None declared.
References
- Havens SJ & Gulati V. Neovascular Glaucoma. Dev Ophthalmol 55 (2016): 196–204.
- Shinohara Y, Akiyama H, Magori M, et al. Short-term outcomes after EX-PRESS implantation versus trabeculectomy alone in patients with neovascular glaucoma. Clinical Ophthalmology 11 (2017): 2207–2213.
- Kawabata K, Shobayashi K, Iwao K, et al. Efficacy and safety of Ex-PRESS® mini shunt surgery versus trabeculectomy for neovascular glaucoma: a retrospective comparative study. BMC Ophthalmology 19 (2019): 75.
- Yilmaz SG, Yildirim S, Degirmenci C, et al. Evaluation of Ex-PRESS mini glaucoma shunt implantation with preoperative intracameral bevacizumab injection in refractory neovascular glaucoma, Eur J Ophthalmol 26 (2016): 575-580.
- Bhagat PR, Agrawal KU,Tandel D. Study of the Effect of Injection Bevacizumab through Various Routes in Neovascular Glaucoma. Journal of Current Glaucoma Practice 10 (2016): 39-48.
- Beutel J, Peters S, Lüke M, et. al. Bevacizumab Study Group; Grisanti S. Bevacizumab as adjuvant for neovascular glaucoma. Acta Ophthalmologica 88 (2010): 103–109.
- Fra,czkiewicz-Skok M, Konopin´ska J, Mariak Z, Re,kas M. Comparison of Ex Press implantation and partial deep sclerectomy combined with ExPress implanttation and simultaneous phacoem-ulsification. Journal of Ophthalmology (2019): 7424376.
- Kawabata K, Shobayashi K, Iwao K, et al. Efficacy and safety of intravitreal ranibi-zumab with panretinal photocoagulation followed by trabeculectomy compared with Ahmed glaucoma valve implantation in neovascular glaucoma Int J Ophthalmol 10 (2017): 400-405.
- Shen CC, Salim S, Du H, et al. Trabeculectomy versus Ahmed Glaucoma Valve implantation in neovascular glau-coma. Clinical Ophthalmology 5 (2011): 281–286.
- Shchomak Z, Sousa DC, Leal I, et al. Surgical treatment of neovascular glaucoma: a systematic review and meta-analysis. Graefe's Archive for Clinical and Experi-mental Ophthalmology 257 (2019): 1079-1089.
- Shaarawy T, Goldberg I, Fechtner R. EX-PRESS glaucoma filtration device: Review of clinical experience and comparison with trabeculectomy. Survey of ophthalmology 60 (2015): 327 -345.
- Chan JE, Netland PA. EX-PRESS Glaucoma Filtration Device: efficacy, safety, and predictability. Medical Devices: Evidence and Research 8 (2015): 381–388.
- Rouse JM, Sarkisian Jr. SR. Mini-drainage devices: The Ex-Press mini-glaucoma device. In: Bettin P, Khaw PT, eds. Glaucoma Surgery. Dev Ophthalmol. Basel, Karger 50 (2012): 90–95
- Kato N, Takahashi G, Kumegawa1 K, et al. Indications and postoperative treatment for Ex-PRESS® insertion in Japanese patients with glaucoma: comparison with standard trabeculectomy. Clinical Ophthalmology 9 (2015): 1491–1498.
- Puerto B, Lo´pez-Caballero C, Sa´nchez-Sa´nchez C, et al. Clinical outcomes after Ex-PRESS glaucoma shunt versus non-penetrating deep sclerectomy: two-year follow-up. Int Ophthalmol 38 (2017): 2575-2584.
- Kozobolis V, Panos GD, Konstantinidis A, et al. Modified deep sclerectomy combined with Ex-PRESS filtration device versus trabeculectomy for primary open angle glaucoma. Int J Ophthalmology 10 (2017): 728-732.
- Roy S, Mermoud A. Deep Sclerectomy. In: Bettin P, Khaw PT, eds. Glaucoma Surgery. Dev Ophthalmol. Basel, Karger 50 (2012): 29–36
- Angmo D, Sobti A, Panda A. The Surgical Treatment of Neovascular Glaucoma with Ex-PRESS P-50 Miniature Glaucoma Shunt. J Curr Glaucoma Pract 6 (2012): 13-16.