Surgical Stabilization in Unstable Vertebral Fractures
Article Information
Inaki Arrotegui*
Department of Neurosurgery, University General Hospital of Valencia, Valencia, Spain
*Corresponding Author: Inaki Arrotegui, Department of Neurosurgery, University General Hospital of Valencia, Avda Tres Cruces S/n. 46014-Valencia, Spain
Received: 04 May 2019; Accepted: 15 May 2019; Published: 17 May 2019
Keywords: Vertebral fracture; Thoracolumbar spine injuries; Trauma
Citation:
Inaki Arrotegui. Surgical Stabilization in Unstable Vertebral Fractures. Journal of Spine Research and Surgery 1 (2019): 029-032.
View / Download Pdf Share at FacebookKeywords
Vertebral fracture, Thoracolumbar spine injuries, Trauma
Vertebral fracture articles Vertebral fracture Research articles Vertebral fracture review articles Vertebral fracture PubMed articles Vertebral fracture PubMed Central articles Vertebral fracture 2023 articles Vertebral fracture 2024 articles Vertebral fracture Scopus articles Vertebral fracture impact factor journals Vertebral fracture Scopus journals Vertebral fracture PubMed journals Vertebral fracture medical journals Vertebral fracture free journals Vertebral fracture best journals Vertebral fracture top journals Vertebral fracture free medical journals Vertebral fracture famous journals Vertebral fracture Google Scholar indexed journals Thoracolumbar spine injuries articles Thoracolumbar spine injuries Research articles Thoracolumbar spine injuries review articles Thoracolumbar spine injuries PubMed articles Thoracolumbar spine injuries PubMed Central articles Thoracolumbar spine injuries 2023 articles Thoracolumbar spine injuries 2024 articles Thoracolumbar spine injuries Scopus articles Thoracolumbar spine injuries impact factor journals Thoracolumbar spine injuries Scopus journals Thoracolumbar spine injuries PubMed journals Thoracolumbar spine injuries medical journals Thoracolumbar spine injuries free journals Thoracolumbar spine injuries best journals Thoracolumbar spine injuries top journals Thoracolumbar spine injuries free medical journals Thoracolumbar spine injuries famous journals Thoracolumbar spine injuries Google Scholar indexed journals Trauma articles Trauma Research articles Trauma review articles Trauma PubMed articles Trauma PubMed Central articles Trauma 2023 articles Trauma 2024 articles Trauma Scopus articles Trauma impact factor journals Trauma Scopus journals Trauma PubMed journals Trauma medical journals Trauma free journals Trauma best journals Trauma top journals Trauma free medical journals Trauma famous journals Trauma Google Scholar indexed journals segmentaries articles segmentaries Research articles segmentaries review articles segmentaries PubMed articles segmentaries PubMed Central articles segmentaries 2023 articles segmentaries 2024 articles segmentaries Scopus articles segmentaries impact factor journals segmentaries Scopus journals segmentaries PubMed journals segmentaries medical journals segmentaries free journals segmentaries best journals segmentaries top journals segmentaries free medical journals segmentaries famous journals segmentaries Google Scholar indexed journals sublaminar wires articles sublaminar wires Research articles sublaminar wires review articles sublaminar wires PubMed articles sublaminar wires PubMed Central articles sublaminar wires 2023 articles sublaminar wires 2024 articles sublaminar wires Scopus articles sublaminar wires impact factor journals sublaminar wires Scopus journals sublaminar wires PubMed journals sublaminar wires medical journals sublaminar wires free journals sublaminar wires best journals sublaminar wires top journals sublaminar wires free medical journals sublaminar wires famous journals sublaminar wires Google Scholar indexed journals traumatic spinal injuries articles traumatic spinal injuries Research articles traumatic spinal injuries review articles traumatic spinal injuries PubMed articles traumatic spinal injuries PubMed Central articles traumatic spinal injuries 2023 articles traumatic spinal injuries 2024 articles traumatic spinal injuries Scopus articles traumatic spinal injuries impact factor journals traumatic spinal injuries Scopus journals traumatic spinal injuries PubMed journals traumatic spinal injuries medical journals traumatic spinal injuries free journals traumatic spinal injuries best journals traumatic spinal injuries top journals traumatic spinal injuries free medical journals traumatic spinal injuries famous journals traumatic spinal injuries Google Scholar indexed journals post-traumatic spinal cord articles post-traumatic spinal cord Research articles post-traumatic spinal cord review articles post-traumatic spinal cord PubMed articles post-traumatic spinal cord PubMed Central articles post-traumatic spinal cord 2023 articles post-traumatic spinal cord 2024 articles post-traumatic spinal cord Scopus articles post-traumatic spinal cord impact factor journals post-traumatic spinal cord Scopus journals post-traumatic spinal cord PubMed journals post-traumatic spinal cord medical journals post-traumatic spinal cord free journals post-traumatic spinal cord best journals post-traumatic spinal cord top journals post-traumatic spinal cord free medical journals post-traumatic spinal cord famous journals post-traumatic spinal cord Google Scholar indexed journals prolonged spinal articles prolonged spinal Research articles prolonged spinal review articles prolonged spinal PubMed articles prolonged spinal PubMed Central articles prolonged spinal 2023 articles prolonged spinal 2024 articles prolonged spinal Scopus articles prolonged spinal impact factor journals prolonged spinal Scopus journals prolonged spinal PubMed journals prolonged spinal medical journals prolonged spinal free journals prolonged spinal best journals prolonged spinal top journals prolonged spinal free medical journals prolonged spinal famous journals prolonged spinal Google Scholar indexed journals root ischemia articles root ischemia Research articles root ischemia review articles root ischemia PubMed articles root ischemia PubMed Central articles root ischemia 2023 articles root ischemia 2024 articles root ischemia Scopus articles root ischemia impact factor journals root ischemia Scopus journals root ischemia PubMed journals root ischemia medical journals root ischemia free journals root ischemia best journals root ischemia top journals root ischemia free medical journals root ischemia famous journals root ischemia Google Scholar indexed journals
Article Details
1. Introduction
Spinal fractures of the thoracolumbar segment have experienced a high incidence in current medical practice, in the majority of patients it is due to falls in height, traffic accidents and direct traumatisms; affect young population groups in full physical and mental conditions [1-3]. In the developed countries that have reached great scientific and technical advances, the risky work of man has been replaced by machines, so that the frequency of falls of heights has diminished and car accidents predominate, this is not the case in the underdeveloped countries [4, 5]. Traumatic spinal injuries constitute a serious biosychosocial problem, because the trauma caused by this injury left the patient paraplegic, at the expense of the complications of bed rest and social support [6]. Due to the high morbidity of these lesions many scientists tried the knowledge and proper treatment. The causes of the irreversibility of the neurological lesion caused by this disease are unknown [7, 8]. In the 20th century, large sums of money were allocated for the study and treatment of these injuries. Large surgeons such as Harrintong, Luque, Roy Camile, among others, designed several surgical methods for the reduction and stabilization of these fractures, stabilization systems were created with bars, segmentaries, sublaminar wires and recently the transpedicular screws, with increasingly biocompatible materials like titanium, the latter extremely expensive and the acquisition by poor countries is impossible [9-13].
The latest studies have shown that the way to achieve some degree of neurological recovery is making a diagnosis and treatment as urgent as possible. Early decompression criteria in traumatic spinal injuries are well demonstrated, as well as surgical stabilization in unstable vertebral fractures. This allows to avoid post-traumatic spinal cord ascending edema and prolonged spinal or root ischemia, which causes dysfunction or blockage of motor or sensory transmissions through the medullary cords by vascular or neurochemical changes, which is known as secondary injuries of the trauma [12]. In addition, stabilizing the spine correcting as close as possible to its physiological curves, allows it to fulfill its load and spinal protection functions. The anatomical characteristics of the thoracolumbar vertebral segment, and the existence of a change from an area with little mobility to another with greater movement, make it more vulnerable to traumatic injuries. The highest incidence of vertebral involvement in this series was in T12-L1, which supports what has been said and also coincides with that reviewed in other articles [13, 14].
2. Clinical Case
Patient suffering vertebral fracture after precipitation in the MRI (Figure 1), you can see the occupation of the Lumbar spine of more than 80%. The patient did not present neurological focality. Under general anesthesia, a minimally invasive percutaneous surgery was performed. In the X-rays and CT-Scan (Figures 2, 3), the alignment of the spine can be observed, after the surgery the patient began walking, being discharged 5 days after the surgery.

Figure 1: RMI-It shows the vertebral fracture with the occupation of the Lumbar Spine.

Figure 2: X-rays The vertebral fixation is shown with minimally invasive surgery.
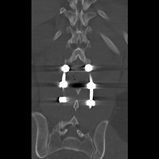
Figure 3: CT Scan: Perfect alignment of the lumbar spine.
3. Discussion
We agree with Cain, [13] in which confirmation of the diagnosis of these fractures is made with simple radiographs in A-P and lateral views, CT and nuclear magnetic resonance make it possible to specify details of this injury and include the degree of compression of the nerve structures. Thoracolumbar spinal fractures are clinically characterized by presenting a history of trauma, usually due to falls from heights, although occasionally they occur due to automobile accidents also of high intensity [13, 14]. The falls of fruit trees are observed very often, because our economy is mainly agricultural. Many authors state that patients go to the body of the guard, usually on stretchers, physical examination shows the ecchymosis and increased volume at the level of the injured vertebrae, spontaneous pain that is exacerbated by the movements and palpation, exquisite pain in the processes of said vertebrae may or may not radiate to one or both lower limbs [13]. Many authors report that when these fractures cause neurological damage by compression of the nervous structures they contain, they are added to the clinical picture. The most severe neurological defect is called paraplegia (grade A of the ASIA scale) [14, 15].
As documented in the literature reviewed, men [16] continue to contribute the most cases, which is due to the fact that they are more exposed to accidents due to the tasks they usually perform. In terms of age, the average figures are quite similar and are given to be the most active age of life [17, 18]. If urgent measures are not taken with these patients, that is to say, if the diagnosis is not made early and the vertebral fracture is unstable, it may reach a neurological injury due to a sudden movement. If there is, from the beginning, the diagnosis of the neurological lesion, the treatment must be intensive and early from the medical point of view as surgical, since the longer the nerve structures are compressed, the greater the tissue ischemia and the more irreversible the neurological damage [19, 20].
4. Conclusion
Surgeons defend the idea that in all unstable thoracolumbar spine injuries, although there are no neurological injuries, surgical treatment should be performed as soon as possible to avoid the complications of bedding and thus reduce their morbidity and mortality.
References
- Floman Y. Toracolumbar spine fractures. Philadelphia: Lippincott (1993).
- Errico BJ, Bauer RD, Waugh TR. Spinal trauma. Philadelphia: Lippincott (1991).
- Sansana ES, Mansilla MB. Fracturas del raquis toracolumbar tratadas mediante instrumentación pedicular. Rev Mapfre Med 10 (1999): 261-270.
- Benson DR, Burkus JK, Montesano PX. Unstable toracolumbar and lumbar burst fractures treated with the AO fixateaur interne. J Spinal Disord 5 (1999): 535-561.
- Baransky M, Kroczak S. Fractures of thoracic lumbar spine treatment and follow up. Ann Transplant 4 (2000): 3-4.
- Van Beek EJ. Upper thoracic spinal fractures. Injury 31 (2000): 219-223.
- Defino HL, Rodríguez-Fuente AE. Treatment of fractures of the thoracolumbar spine by combined anteroposterior fixation using the harms methods. Ear spine 7 (1998): 187-194.
- Ruan DK, Shen GB, Chui HX. Shen instrumentation for management of unstable thoracolumbarspinal fractures. Spine 23 (1999): 1324-1332.
- Watanabe T, Vaccaro AR, Welch WC. High inidence of occult nurogenic bladder dysfunction in neurologically intact patient with thoracolumbar spinal injuries. J Urol 159 (1999): 965-968.
- Rinsky L. Instrumentation of the lumbar spine. An overview. Clin Orthop 203 (2000): 209-218.
- Herdonm WA, Sullivan JA, Gross RH. Segmental spinal instrumentation with sublaminal wires. J Bone Joint Surg 69 (2000): 851-859.
- Bradford DS, Cook J. Result of spinal arthrodesis with pediele serew fixation. J Bone Joint Surg 73 (2001): 1179-1184.
- Cain JE, Dejong JT, Dinenberg AS. Pathomechanical analysis of thoracolumbar burst fractures reduction. Spine 18 (1999): 192-201.
- Garfin S, Nowery CJ. Confirmation of the posterolateral technique descompress and the thoracolumbar spine burst fractures. Spine 10 (2000): 218-226.
- Reid DC, Henderson LS, Miller JD. Etiology and clinical course of spinal fractures. J Trauma 27 (1999): 980-986.
- Sasso RC, Reuben JD. Posterior fixation of thoracolumbar spine fractures using pedicule serew. Spine 16 (2000): 134-142.
- Lindsey RW, Dick W. The fixation interne in the reduction and stabilization of thoracolumbar fractures. Clin Orthop 17 (2000): 161-166.
- Vacarro AR, Blan OG. Adult spine trauma. AM Acad Orth Surg 4 (2002): 593-608.
- Sandén B, Olerud C, Larson S. Hydroxyapatite Coating Improves Fixation of Pedicle Screws. J Bone Joint Surg 84 (2002): 387-391.
- Krepler P, Windhager R, Breschneider W, et al. Total vertebrectomy for primary malignant tumours of the spine. J Bone Joint Surg 84 (2002): 712-715.
