Surgical Approaches in Total Hip Arthroplasty
Article Information
Rajiv Supra1, Rajesh Supra2 and Devendra K Agrawal3*
1College of Osteopathic Medicine, Touro University, Henderson, Nevada, USA
2Georgetown University School of Medicine, Washington, DC, USA
3Department of Translational Research, College of Osteopathic Medicine of the Pacific, Pomona, California, USA
*Corresponding Author: Devendra K Agrawal, Department of Translational Research, College of Osteopathic Medicine of the Pacific, Pomona, California, USA.
Received: 04 May 2023; Accepted: 12 May 2023; Published: 15 May 2023
Citation:
Rajiv Supra, Rajesh Supra, Devendra K Agrawal. Surgical Approaches in Total Hip Arthroplasty. Journal of Orthopedics and Sports Medicine. 5 (2023): 232-240.
View / Download Pdf Share at FacebookAbstract
The Total Hip Arthroplasty (THA) has become one of the most reliable surgical interventions that has improved the quality of life in many patients. THA allows patients to have increased mobility, range of motion, and reduced pain in patients with degenerative hip joints. This surgical procedure has become an effective treatment option for several chronic conditions affecting the hip joint. Although this surgery has been shown to give promising results in patients with hip pathology, selecting the approach for THA is a critical step in pre-operative planning. The best approach for this surgical procedure depends on multiple factors and each present with their own challenges, success rates, and limitations. To further elucidate the advantages and disadvantages associated with different surgical approaches, we critically review each surgical approach along with the different causes of failure of the THA procedure.
Keywords
Anterolateral approach; Direct anterior approach; Direct lateral approach; Periprosthetic joint infection; Posterior approach; THA dislocation; Total hip arthroplasty
Osteopathic medicine articles Osteopathic medicine Research articles Osteopathic medicine review articles Osteopathic medicine PubMed articles Osteopathic medicine PubMed Central articles Osteopathic medicine 2023 articles Osteopathic medicine 2024 articles Osteopathic medicine Scopus articles Osteopathic medicine impact factor journals Osteopathic medicine Scopus journals Osteopathic medicine PubMed journals Osteopathic medicine medical journals Osteopathic medicine free journals Osteopathic medicine best journals Osteopathic medicine top journals Osteopathic medicine free medical journals Osteopathic medicine famous journals Osteopathic medicine Google Scholar indexed journals Total hip arthroplasty articles Total hip arthroplasty Research articles Total hip arthroplasty review articles Total hip arthroplasty PubMed articles Total hip arthroplasty PubMed Central articles Total hip arthroplasty 2023 articles Total hip arthroplasty 2024 articles Total hip arthroplasty Scopus articles Total hip arthroplasty impact factor journals Total hip arthroplasty Scopus journals Total hip arthroplasty PubMed journals Total hip arthroplasty medical journals Total hip arthroplasty free journals Total hip arthroplasty best journals Total hip arthroplasty top journals Total hip arthroplasty free medical journals Total hip arthroplasty famous journals Total hip arthroplasty Google Scholar indexed journals Hip osteoarthritis articles Hip osteoarthritis Research articles Hip osteoarthritis review articles Hip osteoarthritis PubMed articles Hip osteoarthritis PubMed Central articles Hip osteoarthritis 2023 articles Hip osteoarthritis 2024 articles Hip osteoarthritis Scopus articles Hip osteoarthritis impact factor journals Hip osteoarthritis Scopus journals Hip osteoarthritis PubMed journals Hip osteoarthritis medical journals Hip osteoarthritis free journals Hip osteoarthritis best journals Hip osteoarthritis top journals Hip osteoarthritis free medical journals Hip osteoarthritis famous journals Hip osteoarthritis Google Scholar indexed journals Femur articles Femur Research articles Femur review articles Femur PubMed articles Femur PubMed Central articles Femur 2023 articles Femur 2024 articles Femur Scopus articles Femur impact factor journals Femur Scopus journals Femur PubMed journals Femur medical journals Femur free journals Femur best journals Femur top journals Femur free medical journals Femur famous journals Femur Google Scholar indexed journals Acetabulum articles Acetabulum Research articles Acetabulum review articles Acetabulum PubMed articles Acetabulum PubMed Central articles Acetabulum 2023 articles Acetabulum 2024 articles Acetabulum Scopus articles Acetabulum impact factor journals Acetabulum Scopus journals Acetabulum PubMed journals Acetabulum medical journals Acetabulum free journals Acetabulum best journals Acetabulum top journals Acetabulum free medical journals Acetabulum famous journals Acetabulum Google Scholar indexed journals Periprosthetic fractures articles Periprosthetic fractures Research articles Periprosthetic fractures review articles Periprosthetic fractures PubMed articles Periprosthetic fractures PubMed Central articles Periprosthetic fractures 2023 articles Periprosthetic fractures 2024 articles Periprosthetic fractures Scopus articles Periprosthetic fractures impact factor journals Periprosthetic fractures Scopus journals Periprosthetic fractures PubMed journals Periprosthetic fractures medical journals Periprosthetic fractures free journals Periprosthetic fractures best journals Periprosthetic fractures top journals Periprosthetic fractures free medical journals Periprosthetic fractures famous journals Periprosthetic fractures Google Scholar indexed journals Lateral Femoral Cutaneous Nerve articles Lateral Femoral Cutaneous Nerve Research articles Lateral Femoral Cutaneous Nerve review articles Lateral Femoral Cutaneous Nerve PubMed articles Lateral Femoral Cutaneous Nerve PubMed Central articles Lateral Femoral Cutaneous Nerve 2023 articles Lateral Femoral Cutaneous Nerve 2024 articles Lateral Femoral Cutaneous Nerve Scopus articles Lateral Femoral Cutaneous Nerve impact factor journals Lateral Femoral Cutaneous Nerve Scopus journals Lateral Femoral Cutaneous Nerve PubMed journals Lateral Femoral Cutaneous Nerve medical journals Lateral Femoral Cutaneous Nerve free journals Lateral Femoral Cutaneous Nerve best journals Lateral Femoral Cutaneous Nerve top journals Lateral Femoral Cutaneous Nerve free medical journals Lateral Femoral Cutaneous Nerve famous journals Lateral Femoral Cutaneous Nerve Google Scholar indexed journals Rectus fascia articles Rectus fascia Research articles Rectus fascia review articles Rectus fascia PubMed articles Rectus fascia PubMed Central articles Rectus fascia 2023 articles Rectus fascia 2024 articles Rectus fascia Scopus articles Rectus fascia impact factor journals Rectus fascia Scopus journals Rectus fascia PubMed journals Rectus fascia medical journals Rectus fascia free journals Rectus fascia best journals Rectus fascia top journals Rectus fascia free medical journals Rectus fascia famous journals Rectus fascia Google Scholar indexed journals Sartorius muscle articles Sartorius muscle Research articles Sartorius muscle review articles Sartorius muscle PubMed articles Sartorius muscle PubMed Central articles Sartorius muscle 2023 articles Sartorius muscle 2024 articles Sartorius muscle Scopus articles Sartorius muscle impact factor journals Sartorius muscle Scopus journals Sartorius muscle PubMed journals Sartorius muscle medical journals Sartorius muscle free journals Sartorius muscle best journals Sartorius muscle top journals Sartorius muscle free medical journals Sartorius muscle famous journals Sartorius muscle Google Scholar indexed journals Soft tissue articles Soft tissue Research articles Soft tissue review articles Soft tissue PubMed articles Soft tissue PubMed Central articles Soft tissue 2023 articles Soft tissue 2024 articles Soft tissue Scopus articles Soft tissue impact factor journals Soft tissue Scopus journals Soft tissue PubMed journals Soft tissue medical journals Soft tissue free journals Soft tissue best journals Soft tissue top journals Soft tissue free medical journals Soft tissue famous journals Soft tissue Google Scholar indexed journals Hip joint articles Hip joint Research articles Hip joint review articles Hip joint PubMed articles Hip joint PubMed Central articles Hip joint 2023 articles Hip joint 2024 articles Hip joint Scopus articles Hip joint impact factor journals Hip joint Scopus journals Hip joint PubMed journals Hip joint medical journals Hip joint free journals Hip joint best journals Hip joint top journals Hip joint free medical journals Hip joint famous journals Hip joint Google Scholar indexed journals Spine articles Spine Research articles Spine review articles Spine PubMed articles Spine PubMed Central articles Spine 2023 articles Spine 2024 articles Spine Scopus articles Spine impact factor journals Spine Scopus journals Spine PubMed journals Spine medical journals Spine free journals Spine best journals Spine top journals Spine free medical journals Spine famous journals Spine Google Scholar indexed journals Femoral articles Femoral Research articles Femoral review articles Femoral PubMed articles Femoral PubMed Central articles Femoral 2023 articles Femoral 2024 articles Femoral Scopus articles Femoral impact factor journals Femoral Scopus journals Femoral PubMed journals Femoral medical journals Femoral free journals Femoral best journals Femoral top journals Femoral free medical journals Femoral famous journals Femoral Google Scholar indexed journals Fracture articles Fracture Research articles Fracture review articles Fracture PubMed articles Fracture PubMed Central articles Fracture 2023 articles Fracture 2024 articles Fracture Scopus articles Fracture impact factor journals Fracture Scopus journals Fracture PubMed journals Fracture medical journals Fracture free journals Fracture best journals Fracture top journals Fracture free medical journals Fracture famous journals Fracture Google Scholar indexed journals Soft tissue articles Soft tissue Research articles Soft tissue review articles Soft tissue PubMed articles Soft tissue PubMed Central articles Soft tissue 2023 articles Soft tissue 2024 articles Soft tissue Scopus articles Soft tissue impact factor journals Soft tissue Scopus journals Soft tissue PubMed journals Soft tissue medical journals Soft tissue free journals Soft tissue best journals Soft tissue top journals Soft tissue free medical journals Soft tissue famous journals Soft tissue Google Scholar indexed journals
Article Details
1. Introduction
Total hip arthroplasty (THA) is a highly effective surgery for reducing pain and improving the quality of life in patients with hip osteoarthritis [1]. THA has been researched overtime and shown to have 10-year survivorship in more than 95% cases [2]. Over one million THA are performed every year and is projected to reach two million procedures a year by the year 2030 [1].
There are many surgical approaches when conducting this procedure such as the Direct Anterior Approach (DAA), Posterior Approach (PA), and Lateral Approach (LA), all of which have their respective advantages and pitfalls (Figure 1). The PA approach involves splitting the gluteus maximus muscle which allows exposure of the femur and acetabulum, avoiding disruption of the hip abductors all together [3]. However, this approach has an increased rate of dislocation when compared to the DAA or LA [4]. The LA begins with splitting the gluteus medius muscle to access the hip anterolaterally. This surgical approach has been documented to have the lowest risk of dislocation but is associated with superior gluteal nerve injury, impaired abductor function, and heterotopic ossification [3]. The DAA is different with its intermuscular and inter-nervous plane between the tensor facia latae and sartorius. Advantages with DAA is earlier recovery, lower dislocation rates, and shorter hospital stays [3]. Disadvantages include increased risk of periprosthetic fractures, increased learning curve, and higher risk of injuring the Lateral Femoral Cutaneous Nerve (LFCN) [5]. This article highlights the techniques for each surgical approach and a critical review of outcomes and complications.
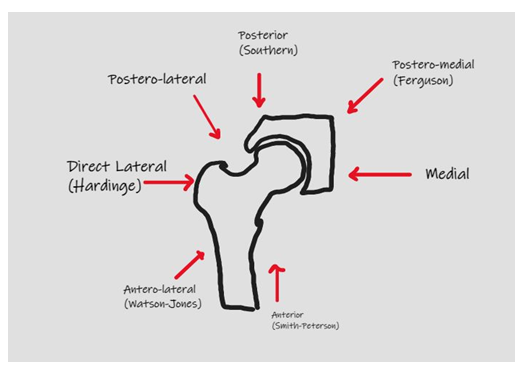
Figure 1: Surgical approaches to Total Hip Arthroplasty.
2. Approaches in Total Hip Arthroplasty
Direct Anterior Approach (DAA): The DAA enters the hip through an intermuscular plane between the tensor fasciae latae and gluteus medius laterally and medially through the sartorius muscle and rectus fascia [6]. The DAA is considered soft tissue sparing as it preserves the stability of the hip joint when compared to the posterior approach. Patients have been documented to experience a rapid recovery based on function and activity using the DAA making this approach potentially advantageous when compared with other approaches [6,7]. Additionally postoperative narcotic use is considerably lower in DDA compared to other surgical approaches [8]. The length of stay has been found to be shorter and more patients are being discharged home as opposed to transfer to post op care facilities [9]. Motor function recovery is faster and the time for ambulation without the use of assisted devices is also shorter. The average time to discontinue the use of walkers or canes was 21 days [10].
The DAA spares abductor muscles and the accuracy of the acetabular cup positioning has been shown to be better with less variation in cup angle when compared to the posterior approach [11,12]. Although there is a tendency for the insertion of the acetabular cup in an anteverted fashion, revision rates for acetabular cup failure were lower in DAA compared to the posterior approach [13]. Nerve injuries are also a risk with DAA. The LFCN has been reported to be among the most injured nerve with the DAA. The LFCN arises from the second and third lumbar nerves and is purely sensory. It courses along the psoas major muscle, crosses the iliacus, and runs below the anterior superior iliac spine [14].
The most important predisposing factor for LFCN injury is the branching pattern. A study described 4 major branching patterns identified as trifurcate, primary femoral, late, and classical. The late branch was found to be at highest risk for injury due to its perpendicular orientation to the incision line [15]. The branching pattern is difficult to predict prior to surgery and the best way to avoid nerve damage is to be cognizant of the various anatomical variations. The rate of injury of the LFCN associated with the DAA is variable between studies with reports ranging from 0.1% to 81% [16,17]. Fortunately, injury to the LFCN does not lead to major neurological deficits and patients report sensations of numbness or burning in the anterolateral region of the high at worst [18].
Early rates of THA failure have been reportedly increasing ranging from 24% to 50% within 5 years of the surgery due to femoral or acetabular prosthetic fracture, mal-alignment, or instability [19–21]. A study reported early femoral periprosthetic fractures and loosening were significantly higher in the DAA when compared to the LA and PA. Additionally, early femoral component loosening was higher with DAA than LA and PA [19,22]. Malalignment of the acetabular cup causes impingement, dislocation, and loosening of the acetabular component [23]. Femoral stem alignment and acetabular anteversion may differ among approaches but has been shown to be more difficult to implant the femoral stem in a neutral position through the anterolateral approach. This was due to elevating the proximal aspect of the femur in the anterolateral surgical approach which may also be true for DAA [20,24]. The tendency to insert the acetabular cup in a more anteverted orientation is seen with DAA and femoral stem anteversion may be mitigated by using the posterolateral approach [25].
Posterior Approach
The inception of the PA dates to 1874 with Bernhard Langenbeck who used this technique at the time to treat arthritis of the hip joint [26]. Later this technique was modified by detaching the short external rotator tendons and the gluteus maximus tendon from the femur to better visualize the hip joint [27]. PA has been reportedly the most used surgical approach for THA [28]. This surgical technique is performed by positioning the patient in lateral decubitus position. The pelvis is stabilized with a padded board placed anterior to the pubic symphysis and chest as well as posterior to the shoulder blades. Additionally, a padded roll should be placed under the contralateral chest wall to reduce incidence of brachial plexopathy. Incision begins 5 cm distal to the greater trochanter and near the center of the femoral diaphysis. The incision continues down and curves toward the superior iliac spine where the skin and subcutaneous fat are separated down to the fascia lata and Iliotibial Band (ITB). The ITB and fascia lata are separated longitudinally to split along the gluteus maximus. Retractors are then placed to split the gluteus maximus and better visualize the piriformis and short external rotators (SERs). The SER are then separated from the greater trochanter and reflected posteriorly to better visualize the posterior hip capsule [29].
Risk of dislocation
It has been noted, historically, that the PA has been associated with greater dislocation rates when compared to the LA. Studies revealed the occurrence of almost 10% dislocation rate after THA using PA compared to the anterolateral approach [30]. Similarly, a review of several studies examining over 10,000 THAs revealed the posterior approach group had a 6-fold higher dislocation rate than LA [29]. A critical factor of the PA was the enhanced soft tissue capsule repair at the end of the surgical procedure which helped diminish dislocation events [31]. A meta-analysis by Zhou et al. [32] revealed THAs with soft tissue capsular repair had lower dislocation rates than those without capsular repair. Kwon et al. [33] however, demonstrated that PA done with repair had higher rates of dislocation when compared to the LA. A prospective study by Meneghini et al. [34] showed that higher dislocation risk was not significantly associated with the PA Interestingly, a cohort study by Fessy et al. [35] revealed PA alone was not a risk factor for dislocation when compared to DAA and LA. Additionally, a randomized controlled trial compared DAA and PA regarding muscle damage. This trial measured inflammatory markers on post-operative days 1 to 4. Investigators concluded the DAA had less muscle damage as measured by inflammatory markers. However, no functional difference between the 2 groups were noticed when looking at 6-month Harris hip scores [35]. While the literature indicates different surgical approaches have variable muscle damage, most studies reveal equal outcomes around 6 weeks postoperatively and further research is warranted in this field [36].
Lateral Approach
The first description of a lateral approach to THA was described as dissecting the interval between the gluteus minimus and medius tendons as well as the vastus lateralis [37]. This approach exposed the femoral head and in 1954, Osborne described a variation that involved placing the patient in a lateral decubitus position. This method involved removing the gluteus medius tendon from its attachment off the trochanter and conducting a subperiosteal dissection from the trochanter continuous with the vastus lateralis tendon [29,38]. The most well-known LA was described by Hardinge and involved splitting the gluteus medius and minimus tendons longitudinally and continuing distally into the vastus lateralis tendon [39]. Soon after, the anterolateral approach gained popularity and was well developed by Sir Watson-Jones. This approach involved the interval between the tensor fasciae latae and the gluteus medius tendon. The gluteus medius tendon was removed to allow for anterior dislocation of the hip joint [40]. Several modifications were created over the decades for the LA. Modifications were made such as removing the abductor muscles and repairing them in different variations. The Rottinger approach modified the LA by sparing detaching the abductor before exposing the joint capsule [41,42].
The LA also is now used in a minimally invasion approach. In the last decade, abductor sparing approaches have been used with early recovery in outpatient total hip programs. As up to 99% have been successfully discharged on the day of the THA using the minimally invasive anterolateral approach [43,44]. A randomized controlled trial compared 40 patients undergoing LA with patients using the DAA. The study examined several outcomes including the gait speed test, timed up and go test and concluded the DAA had better initial functional recovery up to 2 weeks post op. However, no difference was seen with respect to operative blood loss, procedure time, or length of stay in the hospital [45]. Furthermore, a study examined the LA and DAA while measuring damage with preop and postop lab values, muscle atrophy using MRI, and hip outcome scores. All preoperative demographics were equal amongst patients and lab values used to measure muscle damage included erythrocyte sedimentation rate, C-Reactive Protein (CRP), and acute inflammatory cytokines. Investigators revealed creatine kinase and CRP were higher in LA on postop day 4 and all lab values equalized 1 month post THA. Moreover, MRI 6 months post op showed increased gluteal fatty atrophy in LA [46,47].
Complications Using Different Approaches to THA
Regardless of the approach to performing a THA, post-surgical complications remain an issue for many patients. Advances in implant design, the use of advanced protocols for controlling infections, and the use of minimally invasive procedures have improved outcomes of THA [48]. However, possible causes of THA failure including periprosthetic joint infection, dislocation, iliopsoas impingement, and implant malalignment remain issues that must be addressed to improve outcomes of THA (Figure 2).
Dislocation
Dislocation has been one of the most common issues after a primary THA. Risk factors have been identified from several studies related to implant and surgical technique used. A meta-analysis revealed obesity as a risk factor associated with a higher risk of dislocation compared with non-obese patients [49]. Spinal fusion has also been shown to increase rates of dislocation [50]. Dislocation occurs when the forces on the implant head overcome resistance from soft tissues helping to prevent travel of the head. Selecting a larger sized head such as a 32 mm or 36 mm head is a simple option that can prevent dislocation [51,52]. Impingement can also occur leading to dislocation when bone-to-bone or implant-to-implant contact each other during hip motion [51]. Impingement results from malposition and residual osteophyte formation [53]. Other factors contributing to dislocation are lumbar fusion, posterior pelvic tilt, and conditions causing vertebral fusion [54,55]. Capsular repair also plays a critical role in dislocation. The posterior approach is associated with a higher risk of dislocation, however, studies revealed that capsular repair reduced the risk of dislocation [56].
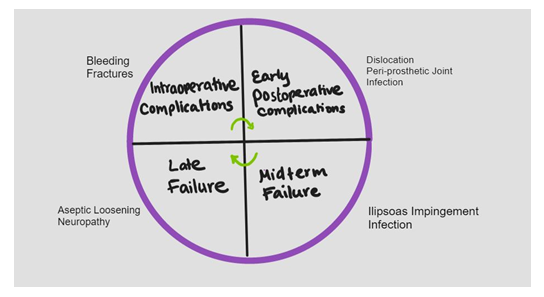
Figure 2: Potential causes of failure and complications following Total Hip Replacement.
Infection
Periprosthetic Joint Infection (PJI) can occur any time after the operation and is the most troublesome cause of failure after a hip replacement. A recent study of a registry database revealed that a mean 90-day revision rate for infection was 0.3% for THA and a meta-analysis of PJI found the overall incidence was 0.4% [57,58]. Risk factors for PJI include high body mass index, surgical site infection, diabetes mellitus, chronic pulmonary disease, cardiovascular disease, and allogenic blood transfusion [59,60]. Preoperative screening for risk factors is critical to reduce the incidence of infection in THA [61]. Perioperative antibiotic prophylaxis has also been researched to prevent PJI and data supports the use of cephalosporins [62]. Additionally, instead of using normal saline solution lavage, the data suggests povidone-iodine lavage for intraoperative irrigation [63]. Debridement and antibiotics for PJI in well-fixed implants is the first option for treatment. Critical factors for the success of this option involves early intervention, typically within seven days of onset, and replacing all modular components [64]. A recent meta-analysis revealed the use of rifampin in successfully treating PJI caused by any species of Cutibacterium, Streptococcus, and Staphylococcus. Results revealed combined use of agents with rifampin posed better outcomes than not using rifampin [65].
Nerve Impingement
Iliopsoas impingement causes pain upon active hip flexion and is a complication of THA [66]. A study reported the diagnosis of iliopsoas tendonitis was made at roughly 2.8 months post THA [67]. Symptoms of iliopsoas impingement appear after full recovery and do not appear immediately after surgery. Female sex increased acetabular to femoral head diameter, and female sex have been researched to be contributing factors for iliopsoas impingement [68]. In addition to iliopsoas tendonitis, the type of implant used for THA has been associated with higher rates of failure. For example, higher rates of failure were reported after use of large head and metal on metal bearings [69]. Furthermore, a severe post-op complication after THA is nerve palsy. Several nerves have been documented that can be potentially damaged during THA including the femoral and sciatic nerve [70]. Risk factors for nerve damage include revision arthroplasty, female sex, dysplastic osteoarthritis, and limb elongation [71]. Nerve damage leads to motor paralysis affecting patient activity and overall wellbeing post THA. Recovery of femoral nerve palsy has been shown to be more predictable than sciatic nerve injury [71].
Fractures
Other common post-operative complications after a THA include pain and periprosthetic fractures. A systematic review of 24 studies of postop pain after THA revealed causes of pain such as adhesions, trochanteric bursitis, heterotopic ossification, capsular fibrosis, and neuropathic pain. Of these, heterotopic ossification and bursitis were among the easiest to diagnose using imaging techniques and can be easily resolved through surgical management [72]. Additionally, periprosthetic fracture remains one of the most troublesome consequences post THA in older patients with osteoporosis [73]. This condition presents at any stage during a THA from intraoperatively to years after the surgery. A meta-analysis studying risk factors for periprosthetic factures revealed age greater than 80 and female sex as well as rheumatoid arthritis being most associated with post-operative fractures [74]. Risk assessment tools such as FRAX scores have been used to identify the risk of fractures post THA related to osteoporosis [75]. Several anti-osteoporosis drugs have been identified and used to prevent bone loss and fractures post THA, yet the clinical importance of such therapeutics has yet to be verified in an aging population [76,77].
Bone and Blood Loss
Extensive bleeding occurs during THA and in many cases requires blood transfusions during surgery which carries a risk of increased morbidity and mortality. A meta-analysis researched the effects of blood loss during THA and compared the DAA to the LA. The DAA was found to have less blood loss due to the intramuscular and inter-nervous approach [78]. Another study revealed the anterolateral approach had lowest rates of blood loss compared to the posterolateral approach which showed highest rates of blood loss [79]. These results were congruent with a separate study that showed the anterolateral approach having lower estimated levels of blood loss [80].
Bone loss is another potential complication following THA and must be considered when deciding an approach. Studies reveal that bone loss occurs at the proximal femur and greater trochanter which increases fracture rates around the implant. One study investigated the effects of using an anterolateral approach and direct lateral on periprosthetic bone loss in patients with femoral neck fracture. Bone loss was measured using bone mineral density and the study reported that at the 3 month follow up, higher rates of bone loss occurred in the patients using the direct lateral approach which subsequently increased at 6 months. Hence, surgical approach does have an influence on periprosthetic bone loss and surgical approaches must be considered to minimize bone loss [81].
Trendelenburg Sign
When a patient has weak hip abductors, the Trendelenburg sign can be observed. Different surgical approaches used in THA results in either the gluteus medius being split, retracted, or spared as mentioned above. The Trendelenburg gait is a well-known residual effect post THA, and the surgeons should choose an approach where these muscles are minimally affected. In a randomized controlled trial studying the DAA and the LA, patients who underwent the LA showed a positive Trendelenburg sign at higher rates [82]. If patients have not regained muscle strength at the 24-month mark, studies revealed they are unlikely to regain normal muscle strength. This was supported by other randomized controlled trials comparing the anterolateral and the LA which both showed high rates of Trendelenburg sign [83]. In a 6 year follow up study comparing PA and LA, the Trendelenburg sign was positive in most of the patients who undergone the LA whereas no signs were seen in those who were operated on using the PA [84]. Additionally, a systematic review revealed that the Trendelenburg sign was commonly seen with the LA than with the PA. Reinsertion, splitting, or retracting the gluteus medius can result in a positive Trendelenburg gait following THA. In the mentioned studies, the LA had higher rates of abnormal gait and the surgeon must be cautious when using this approach [85].
3. Conclusion
Total hip arthroplasty can be done using a wide range of surgical approaches. The DAA, LA, and PA are among the most common. Each approach comes with its own unique advantages and disadvantages. Even though the PA is the most common approach, all other methods fall short when considering infection rates, bone loss, and accessibility. Therefore, the surgeon should take caution when selecting a surgical approach.
Author Contributions:
Concept and design: Rajiv S, DKA; Literature Search: Rajiv S, RajeshS, DKA; Critical review and interpretation of the findings: RS, DKA; Drafting the article: RajivS, RajeshS; Revising and editing the manuscript: RS, DKA; Final approval of the article: RajivS, RajeshS, DKA.
Funding:
This work was supported by the research grants R01 HL144125 and R01HL147662 to DKA from the National Heart, Lung, and Blood Institute, National Institutes of Health, USA. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health.
Institutional Review Board Statement:
Not applicable.
Informed Consent Statement:
Not applicable
Data Availability Statement:
Not applicable since the information is gathered from published articles.
Acknowledgments:
None
Conflicts of Interest:
The authors declare no conflict of interest.
References
- Ackerman IN, Bohensky MA, Zomer E, et al. The projected burden of primary total knee and hip replacement for osteoarthritis in Australia to the year 2030. BMC Musculoskelet Disord 20 (2019): 90.
- Shan L, Shan B, Graham D, et al. Total hip replacement: a systematic review and meta-analysis on mid-term quality of life. Osteoarthritis Cartilage 22 (2014): 389-406.
- Talia AJ, Coetzee C, Tirosh O, et al. Comparison of outcome measures and complication rates following three different approaches for primary total hip arthroplasty: a pragmatic randomised controlled trial. Trials 19 (2018): 13.
- Docter S, Philpott HT, Godkin L, et al. Comparison of intra and post-operative complication rates among surgical approaches in Total Hip Arthroplasty: A systematic review and meta-analysis. J Orthop 20 (2020): 310-325.
- Hartford JM, Bellino MJ. The Learning Curve for the Direct Anterior Approach for Total Hip Arthroplasty: A Single Surgeon’s First 500 Cases. HIP International 27 (2017): 483-488.
- Su EP. Retraction: Post-operative neuropathy after total hip arthroplasty. Bone Joint J 99 (2017): 46-49.
- Jia F, Guo B, Xu F, et al. A comparison of clinical, radiographic, and surgical outcomes of total hip arthroplasty between direct anterior and posterior approaches: a systematic review and meta-analysis. HIP International 29 (2019): 584-596.
- Nistor DV, Caterev S, Bolboac? SD, et al. Transitioning to the direct anterior approach in total hip arthroplasty. Is it a true muscle sparing approach when performed by a low volume hip replacement surgeon? Int Orthop 41 (2017): 2245-2252.
- Nistor DV, Bota NC, Caterev S, et al. Are physical therapy pain levels affected by surgical approach in total hip arthroplasty? A randomized controlled trial. Orthop Rev (Pavia) 12 (2020).
- Rodriguez JA, Deshmukh AJ, Rathod PA, et al. Does the direct anterior approach in THA offer faster rehabilitation and comparable safety to the posterior approach? Clin Orthop Relat Res 472 (2014): 455-463.
- Meermans G, Konan S, Das R, et al. The direct anterior approach in total hip arthroplasty. Bone Joint J 99-B (2017): 732-740.
- Moerenhout K, Derome P, Laflamme GY, et al. Direct anterior versus posterior approach for total hip arthroplasty: a multicentre, prospective, randomized clinical trial. Canadian Journal of Surgery 63 (2020): E412-417.
- Bhaskar D, Rajpura A, Board T. Current Concepts in Acetabular Positioning in Total Hip Arthroplasty. Indian J Orthop 51 (2017): 386-396.
- Bartlett JD, Lawrence JE, Khanduja V. What Is the Risk Posed to the Lateral Femoral Cutaneous Nerve During the Use of the Anterior Portal of Supine Hip Arthroscopy and the Minimally Invasive Anterior Approach for Total Hip Arthroplasty? Arthroscopy: The Journal of Arthroscopic and Related Surgery 34 (2018): 1833-1840.
- Coffey R, Gupta V. Meralgia Paresthetica. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing 2023(2022).
- Gerry AS, Iturregui JM, Carlson BJ, et al. Increased Risk of Lateral Femoral Cutaneous Nerve Injury in Patients with Previous Hip Arthroscopy Who Underwent a Direct Anterior Approach Total Hip Arthroplasty. Arthrosc Sports Med Rehabil 5 (2023): e103-e108.
- Ukai T, Suyama K, Hayashi S, et al. The anatomical features of the lateral femoral cutaneous nerve with total hip arthroplasty: a comparative study of direct anterior and anterolateral supine approaches. BMC Musculoskelet Disord 23 (2022): 267.
- Gomez Y de la C, Remotti E, Momah DU, et al. Meralgia Paresthetica Review: Update on Presentation, Pathophysiology, and Treatment. Health Psychol Res 11 (2023).
- Lin B, Lan Y, Lu Z, et al. The compared study about femoral stem malalignment with or without the special curved rasp during DAA total hip arthroplasty. BMC Musculoskelet Disord 24 (2023): 319.
- Abe H, Sakai T, Takao M, et al. Difference in Stem Alignment Between the Direct Anterior Approach and the Posterolateral Approach in Total Hip Arthroplasty. J Arthroplasty 30 (2015): 1761-1766.
- Meneghini RM, Elston AS, Chen AF, et al. Direct Anterior Approach: Risk Factor for Early Femoral Failure of Cementless Total Hip Arthroplasty. Journal of Bone and Joint Surgery 99 (2017): 99-105.
- Kahhaleh E, Charles T, Collard X, et al. A low dislocation rate after revision total hip arthroplasty performed through the anterior approach. Arthroplasty 5 (2023): 4.
- Gautreaux M, Kautz S, Martin Z, et al. Acetabular Wall Weakening in Total Hip Arthroplasty: A Pilot Study. Pathophysiology 30 (2023): 83-91.
- Zhang B, Liu S, Liu Z, et al. Clinical and radiologic outcomes in patients undergoing primary total hip arthroplasty with Collum Femoris Preserving stems: a comparison between the direct anterior approach and the posterior approach. BMC Musculoskelet Disord 23 (2022): 77.
- Streck LE, Boettner F. Achieving Precise Cup Positioning in Direct Anterior Total Hip Arthroplasty: A Narrative Review. Medicina (Kaunas) 59 (2023).
- Gänsslen A, Grechenig S, Nerlich M, et al. Standard Approaches to the Acetabulum Part 1: Kocher-Langenbeck Approach. Acta Chir Orthop Traumatol Cech 83 (2016): 141-146.
- Gérard R, Savéan J, Lefèvre C. Minimally invasive posterolateral hip approach with SPARTAQUUS (Spare the Piriformis And Respect The Active QUadratus femoris and gluteus mediUS) technique. Orthopaedics and Traumatology: Surgery and Research 106 (2020): 1523-1526.
- Chechik O, Khashan M, Lador R, et al. Surgical approach and prosthesis fixation in hip arthroplasty worldwide. Arch Orthop Trauma Surg 133 (2013): 1595-1600.
- Moretti VM, Post ZD. Surgical Approaches for Total Hip Arthroplasty. Indian J Orthop 51 (2017): 368-376.
- Maratt JD, Gagnier JJ, Butler PD, et al. No Difference in Dislocation Seen in Anterior Vs. Posterior Approach Total Hip Arthroplasty. J Arthroplasty 31 (2016): 127-130.
- Jurkutat J, Zajonz D, Sommer G, et al. The impact of capsular repair on the risk for dislocation after revision total hip arthroplasty – a retrospective cohort-study of 259 cases. BMC Musculoskelet Disord 19 (2018): 314. .
- Zhou Y, Cao S, Li L, et al. Is soft tissue repair a right choice to avoid early dislocation after THA in posterior approach? BMC Surg 17 (2017): 60.
- Kwon MS, Kuskowski M, Mulhall KJ, et al. Does Surgical Approach Affect Total Hip Arthroplasty Dislocation Rates? Clin Orthop Relat Res 447 (2006): 34-38.
- Kyriakopoulos G, Poultsides L, Christofilopoulos P. Total hip arthroplasty through an anterior approach. EFORT Open Rev 3 (2018): 574-583.
- Fessy MH, Putman S, Viste A, et al. What are the risk factors for dislocation in primary total hip arthroplasty? A multicenter case-control study of 128 unstable and 438 stable hips. Orthopaedics and Traumatology: Surgery and Research 103 (2017): 663-668.
- Zhou Z, Li Y, Peng Y, et al. Clinical efficacy of direct anterior approach vs. other surgical approaches for total hip arthroplasty: A systematic review and meta-analysis based on RCTs. Front Surg 9 (2022).
- Carta S, Fortina M. ALDI (Anterior Lateral Decubitus Intermuscular) approach to the hip: Comprehensive description of the surgical technique with operative video. Orthopaedics and Traumatology: Surgery and Research 105 (2019): 923-930.
- Carro LP, Hernando MF, Cerezal L, et al. Deep gluteal space problems: piriformis syndrome, ischiofemoral impingement and sciatic nerve release. Muscles Ligaments Tendons J 6 (2016): 384-396.
- Goyal P, Lau A, McCalden R, et al. Accuracy of the modified Hardinge approach in acetabular positioning. Canadian Journal of Surgery 59 (2016): 247-253.
- Lepri AC, Villano M, Matassi F, et al. “Anterolateral” approach to the hip: a systematic review of the correct definition of terms. HIP International 30(2_suppl) (2020): 13-19.
- Bernasek TL, Thatimatla NK, Levering M, et al. Effect of Immediate Full Weight Bearing on Abductor Repair and Clinical Function After THA Through a Modified Hardinge Approach. Orthopedics 36 (2013).
- Delanois RE, Sultan AA, Albayar AA, et al. The Röttinger approach for total hip arthroplasty: technique, comparison to the direct lateral approach and review of literature. Ann Transl Med 5 (2017): S31-S31.
- Sheahan W. Elective Total Hip Arthroplasty: Which Surgical Approach Is Optimal? Federal Practitioner 39 (2022).
- Chen D, Berger RA. Outpatient minimally invasive total hip arthroplasty via a modified Watson-Jones approach: technique and results. Instr Course Lect 62 (2013): 229-236.
- Parvizi J, Restrepo C, Maltenfort MG. Total Hip Arthroplasty Performed Through Direct Anterior Approach Provides Superior Early Outcome. Orthopedic Clinics of North America 47 (2016): 497-504.
- Higgins BT, Barlow DR, Heagerty NE, et al. Anterior vs. Posterior Approach for Total Hip Arthroplasty, a Systematic Review and Meta-analysis. J Arthroplasty 30 (2015): 419-434.
- De Anta-Díaz B, Serralta-Gomis J, Lizaur-Utrilla A, et al. No differences between direct anterior and lateral approach for primary total hip arthroplasty related to muscle damage or functional outcome. Int Orthop 40 (2016): 2025-2030.
- Toci GR, Magnuson JA, DeSimone CA, et al. A Systematic Review and Meta-Analysis of Non-database Comparative Studies on Cemented Versus Uncemented Femoral Stems in Primary Elective Total Hip Arthroplasty. J Arthroplasty 37 (2022): 1888-1894.
- Kobayashi N, Kamono E, Kameda K, et al. Is there any clinical advantage of capsular repair over capsular resection for total hip arthroplasty? An updated systematic review and meta-analysis. Arch Orthop Trauma Surg 143 (2022): 1689-1697.
- Onggo JR, Nambiar M, Onggo JD, et al. Comparable dislocation and revision rates for patients undergoing total hip arthroplasty with subsequent or prior lumbar spinal fusion: a meta-analysis and systematic review. European Spine Journal 30 (2021): 63-70.
- Pituckanotai K, Arirachakaran A, Tuchinda H, et al. Risk of revision and dislocation in single, dual mobility and large femoral head total hip arthroplasty: systematic review and network meta-analysis. European Journal of Orthopaedic Surgery and Traumatology 28 (2018): 445-455.
- Hoskins W, Rainbird S, Holder C, et al. A Comparison of Revision Rates and Dislocation after Primary Total Hip Arthroplasty with 28, 32, and 36-mm Femoral Heads and Different Cup Sizes. Journal of Bone and Joint Surgery 104 (2022): 1462-1474.
- Shoji T, Ota Y, Saka H, et al. Factors affecting impingement and dislocation after total hip arthroplasty – Computer simulation analysis. Clinical Biomechanics 80 (2020): 105151.
- Stefl M, Lundergan W, Heckmann N, et al. Spinopelvic mobility and acetabular component position for total hip arthroplasty. Bone Joint J 99-B (1_Supple_A) (2017): 37-45.
- van der Gronde BATD, Schlösser TPC, van Erp JHJ, et al. Current Evidence for Spinopelvic Characteristics Influencing Total Hip Arthroplasty Dislocation Risk. JBJS Rev 10 (2022).
- Sun X, Zhu X, Zeng Y, et al. The effect of posterior capsule repair in total hip arthroplasty: a systematic review and meta-analysis. BMC Musculoskelet Disord 21 (2020): 263.
- Jin X, Gallego Luxan B, Hanly M, et al. Estimating incidence rates of periprosthetic joint infection after hip and knee arthroplasty for osteoarthritis using linked registry and administrative health data. Bone Joint J 104-B (2022): 10601066.
- Yoon BH, Ha YC, Lee YK, et al. Postoperative Deep Infection After Cemented Versus Cementless Total Hip Arthroplasty: A Meta-Analysis. J Arthroplasty 30 (2015): 1823-1827.
- Ren X, Ling L, Qi L, et al. Patients’ risk factors for periprosthetic joint infection in primary total hip arthroplasty: a meta-analysis of 40 studies. BMC Musculoskelet Disord 22 (2021): 776.
- Kim JL, Park JH, Han SB, et al. Allogeneic Blood Transfusion Is a Significant Risk Factor for Surgical-Site Infection Following Total Hip and Knee Arthroplasty: A Meta-Analysis. J Arthroplasty 32 (2017): 320-325.
- Johns WL, Layon D, Golladay GJ, et al. Preoperative Risk Factor Screening Protocols in Total Joint Arthroplasty: A Systematic Review. J Arthroplasty 35 (2020): 3353-3363.
- Siddiqi A, Forte SA, Docter S, et al. Perioperative Antibiotic Prophylaxis in Total Joint Arthroplasty. Journal of Bone and Joint Surgery 101 (2019): 828-842.
- Kobayashi N, Kamono E, Maeda K, et al. Effectiveness of diluted povidone-iodine lavage for preventing periprosthetic joint infection: an updated systematic review and meta-analysis. J Orthop Surg Res 16 (2021): 569.
- Tsang STJ, Ting J, Simpson AHRW, et al. Outcomes following debridement, antibiotics and implant retention in the management of periprosthetic infections of the hip. Bone Joint J 99-B (2017): 1458-1466.
- Kruse CC, Ekhtiari S, Oral I, et al. The Use of Rifampin in Total Joint Arthroplasty: A Systematic Review and Meta-Analysis of Comparative Studies. J Arthroplasty 37 (2022): 1650-1657.
- Hardwick-Morris M, Twiggs J, Miles B, et al. Iliopsoas tendonitis after total hip arthroplasty. Bone Jt Open 4 (2023): 3-12.
- Campbell A, Thompson K, Pham H, et al. The incidence and pattern of iliopsoas tendinitis following hip arthroscopy. HIP International 31 (2021): 542-547.
- Buller LT, Menken LG, Hawkins EJ, et al. Iliopsoas Impingement After Direct Anterior Approach Total Hip Arthroplasty: Epidemiology, Risk Factors, and Treatment Options. J Arthroplasty 36 (2021): 1772-1778.
- Haddad FS, Thakrar RR, Hart AJ, Skinner JA, Nargol AVF, Nolan JF, et al. Metal-on-metal bearings. J Bone Joint Surg Br. 2011 May;93-B(5):572–9.
- Hoshino C, Koga D, Koyano G, et al. Femoral nerve palsy following primary total hip arthroplasty with the direct anterior approach. PLoS One 14 (2019): e0217068.
- Kolanowska-Groma A, Synder M, Sibinski M, et al. Prognosis for Peripheral Nerve Injuries after Hip Joint Arthroplasty. Ortop Traumatol Rehabil 22 (2020): 323-332.
- Yucuma D, Riquelme I, Avellanal M. Painful Total Hip Arthroplasty: A Systematic Review and Proposal for an Algorithmic Management Approach. Pain Physician 24 (2021): 193-201.
- Karachalios TS, Koutalos AA, Komnos GA. Total hip arthroplasty in patients with osteoporosis. HIP International 30 (2020): 370-379.
- Deng Y, Kieser D, Wyatt M, et al. Risk factors for periprosthetic femoral fractures around total hip arthroplasty: a systematic review and meta-analysis. ANZ J Surg 90 (2020): 441-447.
- Wang Z, Tutaworn T, Wishman MD, et al. Fracture Risk Assessment Tool Scores and Radiographical Bone Measurements in Total Hip Arthroplasty Patients. J Arthroplasty 37 (2022): 2381-2386.
- Morita A, Kobayashi N, Choe H, et al. Effect of switching administration of alendronate after teriparatide for the prevention of BMD loss around the implant after total hip arthroplasty, 2-year follow-up: a randomized controlled trial. J Orthop Surg Res 15 (2020): 17.
- Kobayashi N, Inaba Y, Uchiyama M, et al. Teriparatide Versus Alendronate for the Preservation of Bone Mineral Density After Total Hip Arthroplasty – A randomized Controlled Trial. J Arthroplasty 31 (2016): 333-338.
- Wang Z, Wei BH, Zhao HJ. Direct anterior versus lateral approaches for clinical outcomes after total hip arthroplasty: a meta-analysis. J Orthop Surg Res 14 (2019): 63.
- Migliorini F, Trivellas A, Eschweiler J, et al. Hospitalization length, surgical duration, and blood lost among the approaches for total hip arthroplasty: a Bayesian network meta-analysis. Musculoskelet Surg 104 (2020): 257-266.
- Aggarwal VK, Elbuluk A, Dundon J, et al. Surgical approach significantly affects the complication rates associated with total hip arthroplasty. Bone Joint J 101-B (2019): 646-651.
- Ugland TO, Haugeberg G, Svenningsen S, et al. Less periprosthetic bone loss following the anterolateral approach to the hip compared with the direct lateral approach. Acta Orthop 89 (2018): 23-28.
- Mjaaland KE, Kivle K, Svenningsen S, et al. Do Postoperative Results Differ in a Randomized Trial Between a Direct Anterior and a Direct Lateral Approach in THA? Clin Orthop Relat Res 477 (2019): 145-155.
- Miller LE, Gondusky JS, Kamath AF, et al. Influence of surgical approach on complication risk in primary total hip arthroplasty. Acta Orthop 89 (2018): 289-294.
- Vicente JRN, Miyahara HS, Luzo CM, et al. Total hip arthroplasty using a posterior minimally invasive approach – results after six years. Revista Brasileira de Ortopedia (English Edition) 50 (2015): 77-82.
- Berstock J, Blom A, Beswick A. A systematic review and meta-analysis of complications following the posterior and lateral surgical approaches to total hip arthroplasty. The Annals of The Royal College of Surgeons of England 97 (2015): 11-16.
