Superior Sternal Cleft – A Rare Congenital Anomaly Associated with Atrial Septal Defect
Article Information
Dorathy Chinwe Obu1*, Obumneme Benaianh Ezeanosike1, Samuel Amechi Nwukor1, Onyinyechukwu Adaeze Arua2, Achike Ezeanwu2
1Department of Paediatrics, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria
2Department of Surgery, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria
*Corresponding Author: Dr. Dorathy Chinwe Obu, Department of Paediatrics, Alex Ekwueme Federal University Teaching Hospital Abakaliki, Ebonyi State, Nigeria
Received: 15 June 2020; Accepted: 29 July 2020; Published: 10 September 2020
Citation: Dorathy Chinwe Obu, Obumneme Benaianh Ezeanosike, Samuel Amechi Nwukor, Onyinyechukwu Adaeze Arua, Achike Ezeanwu. Superior Sternal Cleft – A Rare Congenital Anomaly Associated with Atrial Septal Defect. Archives of Clinical and Medical Case Reports 4 (2020): 853-858.
View / Download Pdf Share at FacebookAbstract
The sternal cleft is a rare anomaly occurring in 1 in 50, 000 – 100, 000 births. It results from either partial or total failure of sternal fusion early in embryological development. A few causes such as riboflavin deficiency, alcohol abuse during pregnancy, and disruption in the HOX-B4 gene have been postulated. Although asymptomatic, clinical diagnosis is easily made at birth due to the obvious chest defect and abnormal movements of the thorax. Surgery is indicated to prevent mediastinal injury, respiratory and hemodynamic sequelae, allow optimal growth of the chest, and cosmesis. We report a case of superior sternal cleft and skin defect associated with isolated ostium secundum type of atrial septal defect in an apparently healthy term female newborn. This is to create awareness among Paediatricians on this very rare type of congenital anomaly that should warrant further investigation for aetiologies and full evaluation in Nigeria. Also, to share the knowledge that will aid counseling of affected families because of possible environmental/social causes, and concerning recurrence in other siblings due to a genetic predisposition.
Keywords
Newborn; Sternum; Congenital malformation; Heart defect
Newborn articles, Sternum articles, Congenital malformation articles, Heart defect articles
Newborn articles Newborn Research articles Newborn review articles Newborn PubMed articles Newborn PubMed Central articles Newborn 2023 articles Newborn 2024 articles Newborn Scopus articles Newborn impact factor journals Newborn Scopus journals Newborn PubMed journals Newborn medical journals Newborn free journals Newborn best journals Newborn top journals Newborn free medical journals Newborn famous journals Newborn Google Scholar indexed journals Sternum articles Sternum Research articles Sternum review articles Sternum PubMed articles Sternum PubMed Central articles Sternum 2023 articles Sternum 2024 articles Sternum Scopus articles Sternum impact factor journals Sternum Scopus journals Sternum PubMed journals Sternum medical journals Sternum free journals Sternum best journals Sternum top journals Sternum free medical journals Sternum famous journals Sternum Google Scholar indexed journals Congenital malformation articles Congenital malformation Research articles Congenital malformation review articles Congenital malformation PubMed articles Congenital malformation PubMed Central articles Congenital malformation 2023 articles Congenital malformation 2024 articles Congenital malformation Scopus articles Congenital malformation impact factor journals Congenital malformation Scopus journals Congenital malformation PubMed journals Congenital malformation medical journals Congenital malformation free journals Congenital malformation best journals Congenital malformation top journals Congenital malformation free medical journals Congenital malformation famous journals Congenital malformation Google Scholar indexed journals tumor articles tumor Research articles tumor review articles tumor PubMed articles tumor PubMed Central articles tumor 2023 articles tumor 2024 articles tumor Scopus articles tumor impact factor journals tumor Scopus journals tumor PubMed journals tumor medical journals tumor free journals tumor best journals tumor top journals tumor free medical journals tumor famous journals tumor Google Scholar indexed journals Heart defect articles Heart defect Research articles Heart defect review articles Heart defect PubMed articles Heart defect PubMed Central articles Heart defect 2023 articles Heart defect 2024 articles Heart defect Scopus articles Heart defect impact factor journals Heart defect Scopus journals Heart defect PubMed journals Heart defect medical journals Heart defect free journals Heart defect best journals Heart defect top journals Heart defect free medical journals Heart defect famous journals Heart defect Google Scholar indexed journals treatment articles treatment Research articles treatment review articles treatment PubMed articles treatment PubMed Central articles treatment 2023 articles treatment 2024 articles treatment Scopus articles treatment impact factor journals treatment Scopus journals treatment PubMed journals treatment medical journals treatment free journals treatment best journals treatment top journals treatment free medical journals treatment famous journals treatment Google Scholar indexed journals laparoscopy articles laparoscopy Research articles laparoscopy review articles laparoscopy PubMed articles laparoscopy PubMed Central articles laparoscopy 2023 articles laparoscopy 2024 articles laparoscopy Scopus articles laparoscopy impact factor journals laparoscopy Scopus journals laparoscopy PubMed journals laparoscopy medical journals laparoscopy free journals laparoscopy best journals laparoscopy top journals laparoscopy free medical journals laparoscopy famous journals laparoscopy Google Scholar indexed journals surgery articles surgery Research articles surgery review articles surgery PubMed articles surgery PubMed Central articles surgery 2023 articles surgery 2024 articles surgery Scopus articles surgery impact factor journals surgery Scopus journals surgery PubMed journals surgery medical journals surgery free journals surgery best journals surgery top journals surgery free medical journals surgery famous journals surgery Google Scholar indexed journals embryological articles embryological Research articles embryological review articles embryological PubMed articles embryological PubMed Central articles embryological 2023 articles embryological 2024 articles embryological Scopus articles embryological impact factor journals embryological Scopus journals embryological PubMed journals embryological medical journals embryological free journals embryological best journals embryological top journals embryological free medical journals embryological famous journals embryological Google Scholar indexed journals Electrocardiography articles Electrocardiography Research articles Electrocardiography review articles Electrocardiography PubMed articles Electrocardiography PubMed Central articles Electrocardiography 2023 articles Electrocardiography 2024 articles Electrocardiography Scopus articles Electrocardiography impact factor journals Electrocardiography Scopus journals Electrocardiography PubMed journals Electrocardiography medical journals Electrocardiography free journals Electrocardiography best journals Electrocardiography top journals Electrocardiography free medical journals Electrocardiography famous journals Electrocardiography Google Scholar indexed journals
Article Details
1. Introduction
The sternal cleft is a rare anomaly occurring in 1 in 50, 000 – 100, 000 births. Globally, it is a very rare chest wall deformity, with a dearth of such case reports from Africa [1]. It accounts for <1% of all chest wall deformities and corresponds to type 11 chest deformities from the Willital classification [2, 3]. Embryologically, the sternum is formed by the medial migration of cells from two bands of the lateral plate mesoderm present on either side of the developing chest wall with the process of fusion completing between 7th -10th week of intrauterine life. This starts cranially at the manubrium and finishes distally at the xiphoid process. A sternal cleft results from either partial or total failure of sternal fusion early in embryological development [4].
Depending on when the developmental process stopped, the sternal cleft may be partial or total. In total sternal cleft, the two halves of the sternum are entirely separated. The partial sternal cleft can be superior or inferior [5]. The superior cleft is often associated with malformations like facial haemangioma or abdominal raphe while the inferior cleft is associated with either ectopia cordis alone or as pentalogy of Cantrell [6]. A superior partial cleft is either a U-shaped defect with the cleft ending at the level of the fourth costal cartilage or a ‘V’–shaped defect if the sternum is cleft to the xiphoid process. Inferior clefts are rare and are usually associated with other abnormalities of midline fusion [1].
We present a case of term female neonate delivered with superior sternal cleft and skin defect with an incidental discovery of an atrial septal defect.
2. Case Report
A term female neonate was delivered to a 32-year-old now para 2 woman at a gestational age of 40 weeks through caesarian section (C/S) on account of a failed attempt at vaginal delivery. She had a history of one previous C/S. The baby cried well at birth with an Apgar score of 9 in one and 10 in five minutes. Her birth weight was 3.5kg while her head circumference and length were 35cm and 51cm respectively. Mother received antenatal care at Alex Ekwueme Federal University Teaching Hospital from the second trimester of pregnancy and was regular with her visits. She did not have a fever or rash in her first trimester of pregnancy. She was non-reactive to retroviral screening, hepatitis B surface antigen, and venereal disease research laboratory tests. She did not use any form of alcohol, cigarette, marijuana, or herbal medication during the index pregnancy. She took her iron, vitamin B complex, folic acid medications as prescribed and her pregnancy was uneventful. She had ultrasonography in the second trimester of pregnancy which did not reveal any fetal anomaly. She had a miscarriage at 3rd month of pregnancy.
Physical examination revealed a term female neonate with a 4 × 5cm ‘U’-shaped concave defect involving the upper two-thirds of the sternum. At the distal part of the defect are a spot of deficient skin and a subcutaneous wound covered only by a transparent epidermal layer of about 1cm in diameter and visible cardiac bulge and pulsation. While crying, the bulge of cardiac structures was noted over the defect (Figure 1b). Her heart rate was 144 beats/minute, respiratory rate was 58 breath/minute and the first and second heart sounds were heard, they were normal and there was no audible murmur. Other systemic examinations did not show any abnormalities.
The anteroposterior and lateral views of the chest radiograph showed increased interclavicular distance and deficiency of the superior part of the sternum sparing the distal ¼ of the sternum (Figure 2). Two-dimensional echocardiography revealed a normally located heart in its pericardium with an 11.4 mm ostium secundum ASD. The abdominal ultrasonography did not reveal any abnormality. The full blood count on the first day of life showed a total white cell count of 13 × 109/L, neutrophil of 68%, and lymphocyte of 30%, and blood film was normal. A primary diagnosis of the superior sternal cleft was made. The second diagnosis was the ostium secundum type of atrial septal defect. The baby was admitted and prophylactic intravenous antibiotics were given for the first three days because of the skin defect. The deficient skin was covered with sterilized gauze and the baby placed on SpO2 monitoring which showed normal reading. The baby remained stable and was discharged four days later for planned primary repair of the sternal cleft as soon as the parents are financially capable. Baby is well, being followed up and was last seen at the newborn clinic a week ago.
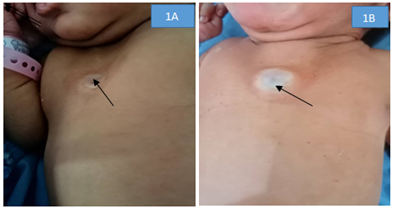
Figure 1: A- Retraction of soft parts in inspiration. B- Protruding soft parts in expiration.
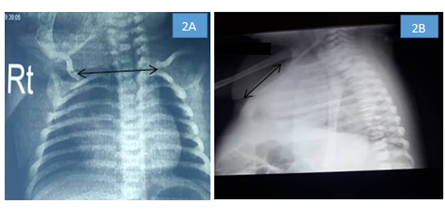
Figure 2: A- Widening of the interclavicular distance 2B- Deficiency of the superior part of the sternum sparing the distal ¼ of the sternum.
3. Discussion
A few causes such as methylcobalamin or riboflavin deficiency, alcohol abuse during pregnancy, and disruption in the HOX-B4 gene have been postulated in murine models [7]. An association with some syndromes have been observed. The acronym “PHACE” has been proposed to describe the association of posterior fossa malformation, hemangiomas, and arterial anomalies, coarctation of the aorta, eye abnormalities, and sternal nonunion [8]. Rare association with other malformations such as Cantrell’s pentalogy, gastroschisis, VACTERL syndrome, Dandy-Walker syndrome, pectus excavatum, and chest wall hamartoma have also been described [8]. We could not precisely identify the cause of this defect in our patient, although the mother may likely have riboflavin deficiency as she did not receive this drug during the first trimester of pregnancy. No syndrome complex was observed in the patient apart from the isolated ASD identified during echocardiography. Torre et al. [9] also reported a frequent association between sternal cleft and skin tags. However, the skin tag was not seen in the index patient.
Even though the condition is frequently diagnosed at birth, patients may present with this condition even in adolescence. This defect is usually asymptomatic and tends to have a predilection for the female gender. The absence of a skeleton in the front part of the chest wall gives rise to a severely paradoxical movement of this part of the thorax. Moreover, the pulsations of the heart and large vessels are visible because they are covered only by soft tissues [10]. The index patient was a female who was asymptomatic at birth apart from the presence of chest defect and had a visible bulge and pulsation of the heart especially while crying (Figure 1).
The condition can be diagnosed prenatally or at birth. At birth, diagnosis is largely clinical. Imaging modalities help in confirming the defects’ location, types, sizes, and other associated disorders. Computed tomography is the modality of choice to evaluate the anatomic detail of the sternum [11]. However, in resource-challenged environments or in situations where caregivers are low-income earners, this may not be obtainable. Hence, a chest radiograph will be necessary. A widened interclavicular distance on chest radiograph with other clinical findings on examination confirms the diagnosis. Echocardiography is needed to identify the intracardiac defects and shunts [12]. In the index patient, due to cost and limited availability of CT scan machines, a chest x-ray was used to confirm the absence of the superior part of the sternum. Echocardiography was further requested to identify any underlying cardiac anomaly which revealed an isolated atrial septal defect, a rare association that has also been reported by few researchers [9,12].
The absence of a sternum introduces multiple risks to the patient, including mediastinal injury, hypothermia, insensible fluid losses, respiratory and hemodynamic sequelae [9]. The indications for surgery are to prevent these complications, allow optimal growth of the chest, and cosmesis [13]. The consensus about the timing of sternal cleft repair is in the neonatal period as the flexibility of the thorax is maximum at this age leading to minimal compression of the underlying structures [10]. Primary closure is the preferred modality in infants under 3 months. After 3 months, sliding or rotating chondrotomies, autologous grafts such as costal cartilages, parietal skull, tibial periosteum, ribs and the use of prosthetic materials such as marlex, acrylic, silicone elastomer, Teflon and stainless steel mesh were described [14].
4. Conclusion
A sternal cleft is a rare congenital anomaly. Although usually asymptomatic, surgery is indicated to improve respiratory dynamics and protect the mediastinal structures from direct injuries, to allow a normal life as well as for cosmesis. Treatment in the neonatal period is most favorable, though other modalities are available in the later stages of life, it can be challenging. Adequate follow-up is necessary as these patients can develop chest wall deformities such as pectus excavatum. Counseling of affected families on possible environmental/social causes to prevent recurrence in other siblings is advocated.
Funding
None
Conflict of Interest
None.
Contribution of the Authors
DC and SA wrote the case summary, DC and OB did the literature review. All authors managed the case, read, and approved the final manuscript.
Acknowledgment
We thank the parents for their understanding and kind permission to take the patient’s pictures and de-identify them for use in this publication.
References
- Ashok RJ, Mathevan G, Ramasubramanianm P. Closing the cleft over a throbbing heart: neonatal sternal cleft. BMJ Case Rep (2014): 10.1136/bcr-2014-204529.
- Willital GH, Saxena AK, Schutze U, et al. Chest-deformities: A Proposal for a Classification. World J Pediatr 7 (2011): 118e23.
- Fokin AA. Cleft sternum and sternal foramen. Surg Clin North Am 10 (2000): 261-276.
- Firmin RK, Fragomeni LS, Lennox SC. Complete cleft sternum. Thorax 35 (1980): 303-306.
- Heron D, Lyonnet S, Iserin L, et al. Sternal cleft: case report and review of a series of nine patients. Am J Med Genet 59 (1995): 154e6.
- Dumitrescu A, Ryan AC, Green A. Sternal cleft malformation in a newborn. BMJ Case Rep (2017): 10.1136/bcr-2017-220237.
- Ramirez-Solis R, Zheng H, Whiting J, et al. Hox-4 (Hox-2.6) mutant mice show homeotic transformation of a cervical vertebra and defects in the cosure of the sternal rudiments. Cell 73 (1993): 279-294.
- Frieden IJ, Resse V, Cohen D. PHACE syndrome. The association of posterior fossa brain malformations, haemagiomas, arterial anomalies, coarctation of the aorta and cardiac defects and eye abnormalities. Arch Derm 132 (1996): 207-311.
- Kothari P, Gupta A, Patil PS, et al. Complete sternal cleft - A rare congenital malformation and its repair in a 3-month-old boy: A case report. J Indian Assoc Pediatr Surg 21 (2016): 78-80.
- Stark P, Jaramillo D. CT of the Sternum. Am J Roentgenol 147 (1986): 72-77.
- Olusoji OO, Sanni SB, Omodara OO, et al. Isolated sternal cleft in a patient with atrial septal defect: A rare sole association. Niger Postgrad Med J 24 (2017): 60-63.
- Torre M, Rapuzzi G, Carlucci M, et al. Phenotypic spectrum and management of sternal cleft: literature review and presentation of a new series. Eur J Cardiothorac Surg 41 (2012): 4-9.
- de Campos JR, Das-Neves-Pereira JC, MC V. Twenty seven-year experience with sternal cleft repair. Eur J Cardiothorac Surg 35 (2009): 539-541.
- Kohli V, Nooreyazdan S, Das BN, et al. Surgical reconstruction for absence of sternum and pericardium in a newborn. Indian J Pediatr 73 (2006): 367-368.
